Back to Journals » Clinical Ophthalmology » Volume 15
Analysis of the Refractive Profile of Children with Oculocutaneous Albinism versus an Age-Matched Non-Albino Group
Authors Sayed KM , Abdellah MM , Kamel AG
Received 10 October 2020
Accepted for publication 8 December 2020
Published 8 January 2021 Volume 2021:15 Pages 73—78
DOI https://doi.org/10.2147/OPTH.S286126
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Khulood Muhammad Sayed, Marwa Mahmoud Abdellah, Ahmad Gad Kamel
The Department of Ophthalmology, Sohag Faculty of Medicine, Sohag University, Sohag, Egypt
Correspondence: Marwa Mahmoud Abdellah
The Department of Ophthalmology, Sohag Faculty of Medicine, Sohag University, Sohag 82524, Egypt
Tel +2010071291010
Email [email protected]
Purpose: To find out and analyze the points of difference in the refractive profile between children with complete oculocutaneous albinism (OCA) and an age-matched, non-albino group seeking paediatric ophthalmic examination.
Methods: A cross-sectional study was conducted on 164 infants and young children in Paediatric Ophthalmology Center, Sohag City, Egypt. Informed consent was obtained from the participants’ guardians. The study divided the population into 2 equal groups: albino group = 82 eyes, non-albino group = 82 eyes. Cycloplegic refraction and average keratometric measurements using the hand-held autokeratometer were taken for the study groups.
Results: In the albino group, astigmatism and hypermetropia were the most common refractive errors, 100% and 62% respectively, with significant difference between both groups. Mean total (TA), corneal (CA) and lenticular astigmatism (LA) were significantly higher in albino group (P< 0.05). All albino eyes were high astigmats (≥ 1.25 D).
Conclusion: This study is novel in being comparative and includes the largest sample size ever reported for albino eyes of infants and children. High WTR astigmatism is the most prevalent refractive error in albinos with an overall bias toward hyperopia, but extreme errors (>− 11.00D myopia or >+10.00D hyperopia) are not common. Albino eyes have a significantly higher degree of LA which compensates for the high CA to decrease the amount of TA. The study emphasizes the importance of refraction examination and visual rehabilitation for OCA children as early as possible to reduce eye morbidity-associated low vision.
Keywords: refractive error, albinism, young children, autorefractometer, non-albinos
Introduction
Albinism is an inherited disorder involving a defective synthesis of melanin from tyrosine resulting from mutation of one or more associated genes.1 This results in a reduction in or absence of melanin in various parts of the body, particularly hair, skin and eyes. Albinism is universal, although unevenly distributed.2
Albinism is more common in black people, and its transmission is autosomal recessive in most cases3 with no sex difference and with an estimated incidence of approximately one in 20,000.4
During the development of the optic system, melanin deficiency causes clinical manifestations such as foveal hypoplasia, strabismus, nystagmus, photophobia, and refractive errors. This explains the low visual acuity that presents from birth.2
Some authors5,6 studied ophthalmic disorders in all types of albinos between 2001–2007 in Douala, Cameroon. Here, the study focuses only on refractive errors in patients diagnosed with complete OCA.
Published refractive profiles for patients with OCA are generally abnormal, with high refractive errors, being frequently encountered.7,8 However, there are discrepancies between studies in the overall bias in refractive errors, with both hyperopia7,8 and myopia2,6 being reported. This study included a larger number of albino patients than ever reported to compare the results with other previous studies and with an age-matched group and to clarify such inter-study differences.
As the process of normal emmetropization was documented to be impaired in albino patients, partly due to foveal hypoplasia and partly due to high refractive error,3 the present study aims to make a complete analysis of the refractive status of albino children as young as possible. The study also compares the results with an age-matched, non-albino control group; such study – to the best of the authors’ knowledge – has not been done before. The study aims also to focus on the importance of refraction examination of any child with OCA as young as possible to allow for early refractive correction, visual rehabilitation and less impairment of the process of emmetropization.
Methods
This study was performed in Paediatric Ophthalmology Center, Sohag City, Egypt. Ethics committee approval was granted for the study. The study adheres to the guidelines of the Declaration of Helsinki. Included in the study were 164 children, one eye was included for each child. Albino group included 82 eyes and the non-albino age-matched control group included another 82 eyes, this control group involved any non-albino apparently normal children who came to paediatric clinics for fundus and refraction examination.
Diagnosis of OCA was based on the presence of iris transillumination, foveal hypoplasia, and retinal hypopigmentation in association with depigmentation of the skin, hair, and nails. Cycloplegic automatic refraction and keratometric readings was performed using Nidek ARK-30 hand-held autorefractometer (Nidek Co. Ltd., Hiroishi, Japan). Cycloplegia was achieved with 1% cyclopentolate (Colircusi Cicloplejico, Alcon, El Masnou, Barcelona, Spain); a drop was instilled alternately at 30 minutes intervals. A total of 3 instillations were made. Automatic refraction was performed for 1.5–2 hours after the 1st instillation. To avoid excessive systemic absorption, finger pressure was applied on the lacrimal sac for 1–2 minutes following application of the eye drops.
Inclusion Criteria
All children with OCA were included. Age-matched, non-albino children were included.
Exclusion Criteria
Children who had an eye disease that may affect automatic refraction measurement like cataract, cornea pathology, vitreous opacity or retina diseases were excluded. Any child who had a prior eye operation for any reason was also excluded from the study.
Examination
Detailed ophthalmic examination of the anterior and posterior segments in addition to the automatic cycloplegic refraction and K readings using the hand-held autokeratometer (Nidek Co. Ltd.) were done for all eyes. No measurements were taken except when the eye became completely centralized. All measurements were repeated at least 3 times and the most stable results were recorded in order to be used in the study.
Age, sex, spherical error, total cylindrical, cylindrical axis, Average k-readings and corneal astigmatism values were collected.
Statistical Analysis
Age and measurement values obtained from the study groups are presented as averages ± standard deviation. Bivariate relationships were examined using Pearson correlation test or by Spearman correlation test. Multivariable stepwise logistic regression analysis was performed for each dependent variable.
Definitions
The study defines Low myopia to be (<-3.00), moderate myopia (−3.00 to −6.00D) and high myopia (>-6.00D).9 Regarding hyperopia, low hyperopia consists of an error of ≤ +2.00 D, moderate hyperopia includes a range of error from +2.25 to +5.00 D and high hyperopia consists of an error > +5.00 D.10
The study defined high astigmatism to be total cylinder ≥1.00 and normal astigmatism total cylinder ≤ 0.75 D.11
With the rule, astigmatism was defined as cylinder axes from 1° to 15° or 165 ° to 180°, and ATR astigmatism as cylinder axes from 75° to 105°. Oblique astigmatism was defined as cylinder axes from 16° to 74° or 106° to 164°.
Lenticular astigmatism was calculated as the difference between the refractive (total) and corneal astigmatic components.
Results
This cross-sectional study included 164 children, one eye of each child was included in the study. Children were divided into 2 groups: albino group= 82 eyes and non-albino, age-matched control group = 82 eyes.
Mean age was 5.16 ys ±3.4 and 4.95 ys ±1.89 for albino and non-albino groups, respectively with no significant difference between both groups (P=0.309). Age ranged from 3 to 312 months and from 42 to 132 months for albino and non-albino groups, respectively.
Regarding refractive errors; Myopic eyes significantly predominate in non-albino than in albino group (n=29, 35.8%) vs (n=14, 17.3%) (P=0.00758). No significant difference between both groups was found in different degrees of Myopia.
On the other hand, hyperopic eyes significantly predominate in albino group (n=62, 76.5%) vs (n=32, 39.5%) in non-albino group (P=0.000); this significant difference is noticed with high hyperopia (n=21, 26%) vs (n=7, 8.6%) (P= 0.00362) but not with low or moderate hyperopia (p>0.05) (Table 1, Figure 1).
 |
Table 1 Comparison Between Both Groups in Different Parameters |
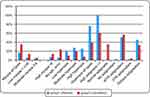 |
Figure 1 Comparison between both groups (albinos and non-albinos) in different parameters. |
Eyes with no spherical refractive error significantly predominate in non-albino (n=20, 24.7%) than in albino group (n=5, 6.2%) (P=0.001).
Astigmatism was predominantly WTR in both groups with no significant difference between the percentage of eyes with WTA in both groups.
All eyes in albino group were high astigmats (n=82, 100%), in contrast to only (n=50, 61.7%) of high astigmatism in non-albino group (P=0.00)
There was a significantly higher mean total, corneal and lenticular astigmatism in albino than in non-albino group (P<0.05) (Figure 2).
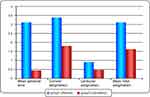 |
Figure 2 Comparison between both groups (albinos and non-albinos) in mean spherical and astigmatic errors. |
Range of spherical error was −9.75 to +9.00D in albino vs −16.75 to +16.25D in non-albinos.
Range of astigmatic error was −6.00 to −1.25 D in albino vs −4.75 to 0.00 D in non-albinos.
Range of corneal astigmatism was −6.88 to −1.00 D in albino vs −6.25 to 0.00 D in non-albinos.
LA ranged from 0–4.25D in albino and 0–1.50D in non-albinos.
Correlations
When considering the absolute values of astigmatism, there was a moderate correlation between CA and TA (r=0.531) in albino group, whereas this correlation was strong in group 2 (r=0.858) (P=0.001, P= 0.000 respectively)
There was also a moderate correlation between CA and Average K reading (r=0.406) in albino group, this correlation was not found in non-albinos.
No correlations were found between refractive error and age.
Discussion
Albinism refers to a congenital disorder characterized by a group of conditions that are inherited as a recessive genetic trait.12–14 Individuals with albinism will always have some form of vision difficulty, which mainly include nystagmus and high values refractive errors.2
This cross-sectional study included analysis of the refractive error of 164 eyes of 164 children: 82 were albino children and 82 were non-albino, age-matched control group referred for fundus and cycloplegic refraction examination.
There are no previous published reports in the medical literature either about detailed analysis of the refractive profile in young albino children nor comparing them with an age-matched, non-albino control group.
Regarding refractive errors, several studies have reported that albinism is associated with high spherical and astigmatic refractive errors.15–19
There are discrepancies between studies with both myopia7,20 and hyperopia8,21 being reported. Although myopic astigmatism and myopia were reported to be the most common for albinos,2 the opposite trend was seen in the present study, with hyperopia being significantly more common than myopia (P=0.00). A similar result is evident in a related study by Dickerson and Abadi7 and also by Yahalom et al’s study.22
The study found astigmatism to be the most common refractive error in albinos (100%) followed by hyperopia (62%) with significant difference between albino and non-albino group.
This is comparable to the results reported by Yahalom et al22 who reported astigmatism and hypermetropia as the most common refractive errors.
But is contrary to other studies5,18 in which myopic astigmatism of albino patients was the most common.
In this study, the difference in hyperopia between both groups is highly significant with high hyperopic eyes representing 26% vs 8.6% for albino and non-albino groups, respectively (P=0.000)
Wildsoet et al reported a range of refractive error in OCA patients from −10.50 D to +9.13D2 and from −11.00D to +7.00D23 in Bhari et al study. These data are comparable with the findings of the current study that a range of −9.75 to +9.00D in albino children was reported. As the study is comparative in nature, the range of refractive error appeared to be much wider in non-albino group (−16.75 to +16.25D), which is in agreement with previous reports on 614 non-albino children eyes with a range of −16.88 to +16.00 D.11
From these observations, one can conclude that although high hyperopia is significantly more common in albinos than non-albino group, severe refractive errors (>−11.00D myopia or >+10.00D hyperopia) are not common and has not been reported for OCA patients. This is in contrast to high astigmatic error which is a character of albino patients; the range was −6.00 to −1.25 D for albino versus −4.75 to 0.00 D in non-albino group.
Astigmatism in albino patients is generally classified as with-the-rule and of high-power;24,25 results of the current study are comparable with these reports. One hundred percent of the albino group were high astigmatic (> −1.25D) and 52% were WTR. This is in agreement with Wildsoet et al2 who found refractive astigmatism in all but one albino subject. But in contrast to Bhari et al23 who found astigmatism in only 2/3 (68%) of albino people.
The reported high astigmatism in OCA was mainly corneal in origin (as refractive astigmatism correlated highly with corneal astigmatism) and mostly with-the-rule in nature.
In this study, WTR astigmatism accounts for 51.9%, followed by Oblique astigmatism (45.7%) and ATR astigmatism (2.5%) with no significant difference between albino and non-albino groups in the distribution of these types of astigmatism. This is in agreement with Khanal et al18 who found 58% of all participants had with-the-rule astigmatism, but not in agreement with Wildsoet et al2 who found refractive astigmatism of OCA eyes was almost always with-the-rule. This discrepancy between studies may be due to age difference in different study populations as this study included a younger age group (5.16 years±3.4) in comparison to a range of 3 to 51 years in Wildsoet et al study.2 It may also be due to different definitions of the axis of different types of astigmatism or the use of retinoscope18 rather than autorefractometer.
WTR astigmatism is also characteristic of idiopathic nystagmus.7,25 Grosvenor26 suggested that corneal molding by the lids might give rise to astigmatism and is a potential explanation here, if the effect of the accompanying nystagmus is to lower corneal rigidity, thereby rendering it more moldable.
Corneal astigmatism generally exceeded refractive astigmatism (TA) in both albino and non-albino groups. These results are suggestive of the presence of compensatory effect of the lenticular astigmatism on CA to decrease the amount of TA. As the CA and TA are significantly higher in albino than non-albino group; LA was also significantly higher in albino group (0.89±0.86) vs (0.47±0.37 D) P=0.016 to allow much more compensation for the significantly higher corneal stigmatism. Albinos also have a much wider range of LA (0–4.25D) than in non-albinos (0–1.50D). An association between LA and hyperopia was previously reported.11 Albinos are mostly hyperopes.
The accuracy of the results of this study is due to the following reasons: large sample size of albino eyes; refraction examination was done under the effect of cycloplegia, the use of autorefractometer rather than retinoscope for determination of accurate axis of astigmatism and the study being comparative.
Study limitations are absence of axial length measurements and analysis of its correlation with the refractive profile in albino children. The importance of axial length was previously documented.2
In conclusion, high astigmatism is the most common refractive error. The refractive profile of albino subjects – in contrast to many previous studies – has an overall bias toward hyperopia especially high degrees (+5.00 to +9.00) but extreme degrees of refractive errors (>−11.00D myopia or >+10.00D hyperopia) are not common in albinos.
High astigmatism is universal in all albino children (100%) with predominance of WTR type followed by oblique and ATR astigmatism. Lenticular astigmatism is significantly of higher degrees to compensate for the high CA to decrease the amount of TA.
The study also stresses the importance of cycloplegic refraction examination for albinos as early as possible to allow early visual rehabilitation and less impairment of the process of emmetropization.
Funding
The authors have not received grant support or research funding.
Disclosure
None of the authors have any financial, consultant, institutional or any other conflicts of interest to disclose for this work.
References
1. Summers CG. Albinism: classification clinical characteristic and recent findings. Optom Vis Sci. 2009;86:659–662.
2. Wildsoet CF, Oswald PJ, Clark S. Albinism: its implications for refractive development. Invest Ophthalmol Vis Sci. 2000;41:1–7.
3. Goddé-Jolly D, Dufier JL. Ophtalmologie Pédiatrique. [Paediatric Ophthalmology]. Paris, France: Masson; 1992:425–429.
4. Gronskov K, Brondum-Nielsen K. Oculocutaneous albinism. Orphanet J Rare Dis. 2007;2:43.
5. Mvogo CE, Bella-Hiag AL, Ellong A, et al. Visual problems in albinos: a hospital study carried out at the Douala General Hospital. Sante. 1999;9(2):89–91.
6. Ebana CM, Eballé AO, Ebana SR, et al. Anomalies oculaires des albinismes oculo-cutanés en milieu camerounais. [Ocular anomalies of oculo-cutaneous albinism in Cameroon]. Revue Soao. 2011;2:7–12.
7. Dickerson CM, Abadi RV. Corneal topography of humans with congenital nystagmus. Ophthal Physiol Opt. 1984;4:3–13.
8. Stark N. Refractive errors in visually handicapped children. Klin Monatsbl Augenheilkd. 1987;191:397–402.
9. Grosvenor T. A review and a suggested classification system for myopia on the basis of age-related prevalence and age of onset. Am J Optom Physiol Opt. 1987;64:545–554.
10. Augsburger AR. Hyperopia. In: Amos JF, editor. Diagnosis and Management in Vision Care. Boston: Butterworths; 1987:101–119.
11. Sayed KM. Analysis of components of total astigmatism in infants and young children. Int Ophthalmol. 2017;37:125–129.
12. Oetting WS, Fryer JP, Shriram S, et al. Oculocutaneous albinism type 1: the last 100 years. Pigment Cell Res. 2003;16:307–311.
13. Hagen EAH, Houston GC, Hoffmann MB, et al. Retinal abnormalities in human albinism translate into a reduction of grey matter in the occipital cortex. Eur J Neurosci. 2005;22:2475–2480.
14. Hagen EAH, Houston GC, Hoffmann MB, et al. Pigmentation predicts the shift in the line of decussation in humans with albinism. Eur J Neurosci. 2007;25:503–511.
15. Eballé AO, Mvogo CE, Noche C, et al. Refractive errors in Cameroonians diagnosed with complete oculocutaneous albinism. Clin Ophthalmol. 2013;7:1491–1495.
16. Carden SM, Boissy RE, Schoettker PJ, et al. Albinism: modern molecular diagnosis. Br J Ophthalmol. 1998;82:189–195.
17. Mohamed AF, El-Sayed NS, Seifeldin NS. Clinico-epidemiologic features of oculocutaneous albinism in northeast section of Cairo – Egypt. Egypt J Med Hum Genet. 2010;11:167–172.
18. Khanal S, Pokhrel A, Kandel H. Visual deficits in Nepalese patients with oculocutaneous albinism. J Optom. 2016;9:103–109.
19. Silver J. Low vision aids in the management of visual handicap. Br J Physiol Opt. 1977;31:47–87.
20. Spedick MJ, Beauchamp GR. Retinal vascular and optic nerve abnormalities in albinism. J Pediatr Ophthalmol Strabismus. 1986;23:58–63.
21. Nathan J, Kiely PM, Crewther SG, et al. Disease-associated visual image degradation and spherical refractive errors in children. Am J Optom Physiol Opt. 1985;62:680–688.
22. Yahalom C, Tzur V, Blumenfeld A, et al. Refractive profile in oculocutaneous albinism and its correlation with final visual outcome. Br J Ophthalmol. 2012;96(4):537–539.
23. Bhari AM, Bajracharya K, Thapa HB, et al. Effectiveness of refractive error correction for people with oculocutaneous albinism in Nepal. Asian J Med Sci. 2017;8:30–34.
24. Orlow SJ. Albinism. An update. Semin Cutan Med Surg. 1997;16:24–29.
25. Nathan J, Kiely PM, Crewther SG, et al. Astigmatism occurring in association with pediatric eye disease. Am J Optom Physiol Opt. 1986;6:497–504.
26. Grosvenor T. Etiology of astigmatism. Am J Optom Physiol Opt. 1978;55:214–218.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
