Back to Journals » Clinical Interventions in Aging » Volume 15
Analysis of the Degree of Acceptance of Illness Among Patients After a Stroke: An Observational Study
Authors Guzek Z, Kowalska J
Received 17 June 2020
Accepted for publication 16 September 2020
Published 2 November 2020 Volume 2020:15 Pages 2063—2072
DOI https://doi.org/10.2147/CIA.S268095
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Zbigniew Guzek,1 Joanna Kowalska2
1Department of Neurological Rehabilitation, University Hospital in Zielona Góra, Zielona Góra, Poland; 2Department of Physiotherapy, University School of Physical Education, Wroclaw, Poland
Correspondence: Joanna Kowalska Department of Physiotherapy
University School of Physical Education, Paderewskiego 35 Street, Wrocław 51-612, Poland
Tel +48 71 347-35-22
Fax +48 71 347-30-81
Email [email protected]
Introduction: The aim of this study was to analyse the level of illness and disability acceptance in stroke patients undergoing regular rehabilitation at two time points, before rehabilitation and after 3 weeks, and to answer the following questions: What is the functional and emotional status of stroke patients, characterized by a lower and higher level of illness acceptance before and after the 3-week rehabilitation period? What factors, including clinical, sociodemographic, functional and emotional, are associated with the degree of illness acceptance in patients who have suffered a first stroke?
Sample and Methods: The study included 64 patients after first stroke, aged 50– 87 years. The following tests were used: Acceptance of Illness Scale, Geriatric Depression Scale, Rivermead Mobility Index and Barthel Index. Tests were conducted at two time points, the first before rehabilitation and the second after 3 weeks of regular rehabilitation.
Results: The study group had an average level of acceptance of their illness and disability, both before and after 3 weeks of rehabilitation. After rehabilitation process, statistically significant improvements were achieved in acceptance of illness, mood disorders, functional status, mobility and locomotion. Low levels of illness acceptance were observed in stroke patients with a poorer functional condition, with mood disorders, with primary and vocational education.
Conclusion: The results suggest that the level of illness acceptance may be an important factor in the rehabilitation of stroke patients; however, further studies are necessary.
Keywords: stroke, older adults, rehabilitation, acceptance of illness, symptoms of depression, functional status
Introduction
Studies conducted to date have confirmed that the level of self-acceptance of illness and disability is an important factor in the rehabilitation and recovery of patients of different ages and illnesses.1–6 According to Painter, self-acceptance of the illness may be the element that activates the patient. Moreover, improvement in functional status and sustained physical activity are conducive to better illness acceptance.7–9 Therefore, this factor may influence the effectiveness of rehabilitation, which, according to the holistic model, should care for the patient not only physically but also mentally. This is extremely important, especially for people suffering from illnesses involving a disability and loss of independence. Unfortunately, the studies carried out so far indicate that the older the patient and the poorer their functional condition, the lower the degree of acceptance.10,11 This applies to residents of nursing homes, among others.1,11 The lowest degree of illness acceptance has been observed in stroke patients.1,8 This is also indicated by other studies, although only a few have focussed on this particular group of patients.12–14 The clinical symptoms, complications and consequences of the underlying disease lead to a partial or total reduction in the patient’s fitness and independence. The majority of patients who have suffered a stroke experience difficulty in adapting to their surrounding social environment, living conditions, everyday life and, above all, difficulty in accepting the sudden onset of their new disability.12
The relationship between functional status and the level of illness acceptance is multidirectional, as proposed in previous studies, and acceptance plays an important role in the process of early and comprehensive rehabilitation of stroke patients. The ability to function independently facilitates the acceptance of the consequences of stroke, while the acceptance of one’s own illness and disability at a given time forms the basis for adopting a proactive attitude during the rehabilitation process.13,15 Therefore, the aim of this study was to analyse the level of illness and disability acceptance in stroke patients undergoing regular rehabilitation at two time points, before rehabilitation (T1) and after 3 weeks (T2), using the data and factors that were already known at the time of admission to the post-stroke rehabilitation ward, ie, sociodemographic, clinical (eg, effected hemisphere, type of stroke, and time since stroke), as well as functional and emotional status of the patients. Taking into account the above factors, the following research questions were put forward: What is the functional and emotional state of patients following a stroke, characterized by a lower and higher level of illness acceptance before and after the 3-week rehabilitation period? What clinical, sociodemographic, functional and emotional factors are associated with the degree of illness acceptance in patients who have suffered a first stroke?
Sample and Methods
Studied Group
This observational study was conducted at the Neurological Rehabilitation Unit of the Department of Rehabilitation of the University Hospital in Zielona Góra, Poland, with the consent of the head of the department and under the ethical and legal supervision of the Department of Physiotherapy of the University School of Physical Education (6/11/2006). This study was conducted in accordance with the Declaration of Helsinki.
The study group consisted of patients who were successively admitted to the rehabilitation ward in the period from July 2017 to February 2018, who satisfied the following criteria for inclusion: written informed consent to participate in the study, first stroke incident, patients admitted up to 2 weeks following a discharge from the hospital, satisfactory cognitive function (no dementia, Mini Mental State Examination, MMSE >23). Exclusion criteria were also established: occurrence of aphasia, refusal to participate at any stage of the study, and the presence of serious mental disorders (eg, consciousness disorders or mental disorders) in the medical records or at the time of the study.
The data used for statistical analysis were only from subjects who after meeting the inclusion criteria, were regularly involved in rehabilitation for a period of 3 weeks (Figure 1).
 |
Figure 1 Recruitment process for the study group. |
Finally, the analysed data covered 64 patients aged 50–87 years, with a mean age of 68.5 (±8.7) years, of whom 29 were women and 35 were men. The majority of patients in the studied group had suffered ischaemic stroke (80%). Detailed patient characteristics are presented in Table 1.
 |
Table 1 Characteristics of Patients (n = 64) |
Measurement Tools
Patients who were included in the study were assessed using the following measurement scales: Acceptance of Illness Scale (AIS), Geriatric Depression Scale (GDS), Rivermead Mobility Index (RMI), and Barthel Index (BI). Additionally, a patient’s medical file was completed, containing sociodemographic and clinical data, collected on the basis of an interview and their previous medical records.
The AIS examines the degree of acceptance of illness and disability. It consists of eight statements that describe the difficulties and limitations that are subjectively experienced by the patient due to their illness. The scale of disease acceptance ranges from 8 to 40 points. The higher the final score (after adding up the points), the better the patient’s acceptance of their own illness. The following interpretation of the results was adopted: 8–19 low, 20–30 average and 31–40 high level of illness acceptance.16 The Cronbach’s reliability index was determined to be 0.85 for studies that use the Polish version.17
The GDS-15 is a screening tool to assess the prevalence of depressive symptoms in older people. It is also recommended for the examination of people who have suffered a stroke.18 The patient responds to questions regarding the past 2 weeks of their life with “yes” or “no” answers. A score between 0 and 5 points indicates no depression, while a score of 6 points or higher indicates depression of increasing severity. The Cronbach’s reliability coefficient of the GDS is 0.94, and the sensitivity and specificity are 84% and 95%, respectively.19
The Rivermead Mobility Index (RMI) is used to assess mobility and locomotion. The respondent performs 13 tasks (from very simple ones, such as sitting down without the use of support, to more complex ones, such as jumping on a paretic limb, repeated five times). For each correctly performed task, the patient receives 1 point, with a possible total score of 13 points. The higher the score, the better the functional status of the patient.20
The Barthel Index (BI) assesses the patient’s performance of 10 basic everyday activities. The maximum a patient can obtain is 100 points. Scores from 0 to 21 indicate a severe condition, 21–85 a medium-heavy condition, and between 86 and 100 the patient’s condition is described as mild. The psychometric properties of the BI scale are considered very good.21
The above tests were performed at two measurement points: T1, the initial assessment prior to the commencement of rehabilitation, on the first day of patient admission to the ward; T2, the final assessment after 3 weeks of regular rehabilitation. The rehabilitation programme was carried out in accordance with doctor’s instructions with a specified frequency and duration, performed from Monday to Friday for about 150 minutes per day and 90 minutes on Saturday. This programme was dependent on the functional status of the patient and included individual exercises with a physiotherapist (120 minutes) and activities with the aim of learning and improving gait (30 minutes, eg, walking on a flat and uneven surface, walking on a special learning track and learning to walk up and down stairs).
Prior to admission to the rehabilitation ward, all patients were subjected to early poststroke rehabilitation at the hospital ward.
Data Analysis
Descriptive statistics were generated, including the mean, standard deviation, minimum and maximum values, numbers and percentages. The Kolmogorov–Smirnov test was used to check for normal distribution of the data. Following confirmation of a normal distribution, the following parametric tests were performed: Student’s t-test to compare two dependent groups and Student’s t-test to compare two independent groups. In the case of Student’s t-test, the Bonferroni correction was applied. For comparison of more than two groups, one-way ANOVA was used. In the case of qualitative variables, a chi-square (χ2) test was used. The Pearson’s correlation analysis for selected pairs of variables was used. Statistical tests were performed at a significance level of p < 0.05 and p<0.025 in the case of Student’s t-test results with Bonferroni correction.
Results
The mean illness acceptance score in the initial assessment (AIS1) was 23.6 (±8.7). On admission to the ward, more than 34% (n = 22) of patients had a low level of illness acceptance, 41% (n = 26) had an average level, and 25% (n = 16) had a high level of acceptance of their illness.
The initial functional status of the respondents was measured using the BI and RMI scales, with mean values of 56.8 (±29.5) and 5.6 (±3.2), respectively, while the mean GDS score was 5.4 (±3.9). Twenty-eight patients (44%) had depressive symptoms (GDS >5).
The lowest level of illness acceptance at the commencement of the study (AIS1) and after 3 weeks of rehabilitation (AIS2) was found in patients with mood disorders and in those with primary and vocational education. There were no statistically significant differences in terms of gender, marital status, economic situation, place of residence, type of stroke, lesion location and initial functional status (Table 2).
 |
Table 2 The Level of Illness Acceptance by Patients at the Initial and Final Assessments (Student’s t-Test for Independent Groups and One-Way ANOVA) |
A comparative analysis of two groups of stroke patients with a low (AIS1 scores 8–19) and high (AIS1 scores 31–40) levels of acceptance of illness at T1 showed statistically significant differences for the following variables: RMI1, RMI2, BI2, GDS1, GDS2, AIS2, and time elapsed since the stroke. Thus, the group of patients with a low AIS1 score had a worse functional status, symptoms of depression, longer time elapsed since the stroke and a low level of illness acceptance after rehabilitation. With the application of Bonferroni correction to the Student’s t-test, statistical significance was observed in the following: RMI 2, GDS 1, GDS 2 and AIS 2 (Table 3). In this group of patients, significantly more cases of depressive disorders were reported than in the group with a high level of illness acceptance before rehabilitation (14 vs 2; χ2 test, p = 0.0016).
 |
Table 3 Comparison of Selected Factors Between Patients with a Low or High Level of Illness Acceptance Before Rehabilitation (Student’s t-Test for Independent Groups) |
After 3 weeks of rehabilitation, statistically significant improvements were achieved in whole study group in the following: acceptance of illness (AIS), mood disorders (GDS), functional status (BI), and mobility and locomotion (RMI) (Table 4). The number of patients with depressive symptoms decreased to 28% following 3 weeks of rehabilitation. The number of stroke patients with a low level of acceptance of illness also decreased to 20% (n = 13).
 |
Table 4 Mean Values for the Tested Parameters in the Initial and Final Assessments in Whole Study Group (Student’s t-Test for Dependent Groups) |
It is worth emphasizing, that patients with low AIS 1 significantly improved their functional as well as emotional status following 3 weeks of rehabilitation. Nevertheless, the mean GDS remained at 6.1± 3.8, which indicates the presence of depressive symptoms. Statistically, the level of illness acceptance in this group of patients also increased significantly; however, it was in the lower values of the average level of illness acceptance (20.1± 7.3) (Table 5).
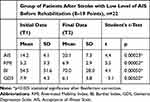 |
Table 5 Mean Values in the Initial and Final Assessments in Group of Patients with Low Level of Illness Acceptance Before Rehabilitation (Student’s t-Test for Dependent Groups) |
A comparative analysis of two groups of stroke patients with low (AIS2 scores 8–19) and high (AIS2 scores 31–40) levels of acceptance of illness at T2 showed statistically significant differences for the following variables: RMI1, RMI2, BI1, BI2, GDS1, GDS2, and AIS1. Thus, the group of patients with a low AIS2 score after rehabilitation had a poorer functional status, symptoms of depression and a low level of illness acceptance before the rehabilitation (Table 6). Significantly more cases of depressive disorders were observed in this group of patients than in the group with a high level of illness acceptance before rehabilitation (9 vs 1; χ2 test, p = 0.00002). Patients with high and secondary education had a higher level of illness acceptance than those with primary and vocational education (χ2 test, p = 0.0219).
 |
Table 6 Comparison of Selected Factors Between Patients with a Low or High Level of Illness Acceptance After 3 Weeks of Rehabilitation (Student’s t-Test for Independent Groups) |
There were no statistically significant differences between groups for the remaining variables (gender, age, BMI, number of comorbidities, marital status, time since stroke, type of stroke and lesion location) at both T1 and T2.
Correlation analyses showed a statistically significant positive relationship of AIS with BI and RMI scores and a significant negative relationship between AIS and GDS scores (Table 7).
 |
Table 7 Results of Pearson’s Correlation Analysis for Selected Pairs of Variables in the Study Group |
Discussion
Among the many factors influencing the effectiveness of rehabilitation are those of psychological nature, one of which is the level of acceptance of one’s own illness.
In the present study, similar to research by Kobylańska et al and Kowalska et al, the study group was described as having an average level of illness acceptance at the time of admission to the ward.8,9 An average level of illness acceptance was also observed by Kurpas et al in patients with chronic diseases, in a study by Chrobak-Bień et al that looked at patients with Leśniewski-Crohn’s disease, and also in patients with colorectal cancer undergoing chemotherapy in studies by Kapela et al.22–24 Different research results were recorded by Kowalska et al in 2016 and 2019, in which stroke patients had a low level of illness acceptance.1,14 Divergent results in this group may be associated with the disease course and differences in the functional status of patients, often associated with a loss of independence, and thus, difficulties in accepting the disease and its implications. However, the limited number of studies focused on stroke patients makes it difficult to compare our results to those of other authors.
The findings presented here reveal that the lowest values of illness acceptance after a stroke in the whole study group both before and after rehabilitation were recorded in patients with depressive symptoms and in those with primary and vocational education. This is also confirmed by the correlation results, which indicate a strong link between the level of illness acceptance and the mood of stroke patients, as well as the comparative analysis of groups of patients with low and high AIS scores before and after the 3-week rehabilitation programme. Based on these results, it can be seen that before commencing rehabilitation, the group of stroke patients with low AIS included those individuals in a poorer functional and emotional condition and those who began rehabilitation a longer period of time after the onset of the disease. This group also achieved significantly lower AIS values after 3 weeks of rehabilitation compared to the group of patients with higher initial AIS levels. Similar relationships between AIS and functional status have been reported in previous studies. The relationship between the level of illness acceptance and mood is also evident, as previously confirmed by Kobylańska et al, Kowalska et al, and Uchmanowicz et al.1,9,25 From these results, it is suggested that the worse the mood and severity of depression symptoms, the lower the level of acceptance of one’s illness and disability.
After 3 weeks of systematic rehabilitation, the functional and emotional status and level of illness acceptance in stroke patients were improved, indicating the effectiveness of the therapy. The patients were described as having an average degree of illness acceptance, as in the initial assessment. However, 20% of the group still had a low level of illness acceptance. A comparative analysis of the final results showed that the group of patients with a low level of AIS included subjects in a worse functional and emotional status, with primary and vocational education, and those who had lower AIS values at the beginning of rehabilitation.
The additional analysis of initial and final results in the group of patients with low AIS at the beginning of rehabilitation indicates a significant improvement of both functional and emotional state, however, the final results still indicate the presence of depressive symptoms and low values of average illness acceptance level.
Therefore, it is this group of stroke patients that should be monitored and subjected to prophylactic interventions to help them adapt to the implications of their disease, so that they gain independence and autonomy during the rehabilitation process. This is necessary to increase the effectiveness of rehabilitation and for patients to adapt more quickly to the physical and psychosocial consequences of disease and disability.26
There were no significant correlations between AIS values and gender, stroke type, brain hemisphere affected, number of coexisting diseases, marital status, economic situation and place of residence. Similar results have been reported by other researchers,11,27,28 in contrast to the results of Kobylańska et al, who observed lower AIS values in patients who were single and who had suffered a haemorrhagic stroke, or the results of studies by Kazimierska-Zając et al, in which women showed poorer acceptance of their illness than men.9,29 On the other hand, in a study by Majda and Józefowska on patients with chronic obstructive pulmonary disease, women achieved a higher rate of acceptance of their illness compared to men.30
The above results indicate that the level of illness acceptance is an important factor in the rehabilitation process of stroke patients. Therefore, in addition to standard examinations performed in the ward, it is advisable to also include tests concerning illness acceptance in order to help the patient adapt to the psychophysical effects of stroke at the earliest possible stage of the disease.
It appears interesting, that in patients with low AIS 1 (before rehabilitation) were subjects who had longer time since stroke compared to those with high AIS1. However, this result was not confirmed by the Bonferroni correction or the additionally performed correlation analysis. The period of 3 weeks is a period of intensive changes, as demonstrated by the results, however, too short to confirm a correlation between the time since stroke and the level of illness acceptance. This is a limitation of the study, as recognized by the authors. Clinical observations show that the functional status of stroke patients stabilizes over time and the effects of rehabilitation are not always so spectacular. This can affect the assessment and acceptance of the disease by the patient. This research requires continuation and duration extension.
Some further limitations of this study need to be addressed. The tests performed, especially those on depressive disorders, are screening in nature and the results are not equivalent to making a diagnosis. The tests were performed in one rehabilitation unit; therefore, the results presented should not be generalised. We emphasize that the group did not belong to the geriatric population only and the assessment concerned only a narrowed group of stroke patients without dementia (MMSE>23). However, there is a need to continue the studies on a larger number of stroke patients in order to confirm or rule out the relationships presented here. Taking into account the numerous factors influencing the level of illness acceptance, the observation period should probably be extended, as 3 weeks is quite a short time to adapt to new conditions of staying in a rehabilitation ward and too short a time for patients to fully accept their constantly changing functional status. Nevertheless, this is a good time for providing specific support to stroke patients with low level of illness acceptance, who are starting rehabilitation.
Conclusions
- The studied stroke patients had an average level of acceptance of their illness and disability, both before and after 3 weeks of rehabilitation.
- Low levels of illness acceptance were observed in stroke patients with a poorer functional condition, with mood disorders, with primary and vocational education and with a longer time elapsed since the stroke when they began rehabilitation.
- A significant relationship was observed between the level of illness acceptance upon admission to the post-stroke rehabilitation unit and the functional and emotional status of stroke patients.
- The level of illness acceptance may be an important factor in the rehabilitation of stroke patients; however, further studies are necessary.
Acknowledgments
The authors would like to thank Ms Aneta Lubczyńska and Ms Paulina Niedziółka for preparing data for statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kowalska J, Mazurek J, Rymaszewska J. Analysis of the degree of acceptance of illness among older adults living in a nursing home undergoing rehabilitation – an observational study. Clin Interv Aging. 2019;14:925–933. doi:10.2147/CIA.S199975
2. Mazurek J, Lurbiecki J. Acceptance of illness scale and its clinical impact. Pol Merk Lek. 2014;36(212):106–108.
3. Niedzielski A, Humeniuk E, Błaziak P, Fedoruk D. The level of approval in selected chronic diseases. Wiad Lek. 2007;60(5–6):224–227.
4. Rusin-Pawelek E, Uchmanowicz I, Jankowska-Polańska B, Panaszek B, Fal AM. Acceptance of illness of patients with bronchial asthma and asthma control. Alergologia Info. 2012;7:61–67.
5. Kurowska I, Kasprzyk A. Disease acceptance and the ways of coping with stress in patients on dialysis. Psychiatr Psychol Klin. 2013;13:99–107.
6. Marmurowska-Michałowska H, Dubas-Slemp A, Kozak A, Dolecki W, Kochański A. Przystosowanie do choroby w grupie osób z rozpoznaniem schizofrenii paranoidalnej – doniesienie wstępne. Badania Nad Schizofrenia. 2004;5:324–329.
7. Painter P. Physical functioning in end-stage renal disease patients: update 2005. Hemodial Int. 2005;9:218–235. doi:10.1111/j.1492-7535.2005.01136.x
8. Kowalska J, Wolny K, Kobylańska M, Wójcik B. The degree of acceptance of illness and functional status among elderly people staying in the rehabilitation centre. Geriatria. 2015;9:3–9.
9. Kobylańska M, Kowalska J, Neustein J, et al. The role of biopsychosocial factors in the rehabilitation process of individuals with a stroke. Work. 2018;61(4):523–535. doi:0.3233/WOR-162823
10. Kaczmarczyk M. The level of acceptance of illness among elderly people living In different environments. Studenterraad Med. 2008;12:29–33.
11. Cybulski M, Cybulski Ł, Krajewska-Kułak E, Cwalina U. Illness acceptance, pain perception and expectations for physicians of elderly in Poland. BMC Geriatr. 2017;17(1):46. doi:10.1186/s12877-017-0441-4
12. Kamusińska E, Rojowska A. Acceptance of disability for people after stroke. Studenterraad Med. 2012;25(1):37–42.
13. Stelmach A, Lorencowicz R, Jasik J, Turowski K. Factors determining the assessment of quality of life made by patients who have had a stroke. J Neurol Neurosurg Nurs. 2016;5(4):136–143. doi:10.15225/PNN.2016.5.4.2
14. Kowalska J, Bojko E, Szczepańska-Gieracha J, Rymaszewska J, Rożek-Piechura K. Occurrence of depressive symptoms among older adults after a stroke in the nursing home facility. Rehabil Nurs. 2016;41:112–119. doi:10.1002/rnj.203
15. Szczepańska-Gieracha J, Kowalska J, Pawik M, Rymaszewska J. Evaluation of a short-term group psychotherapy used as part of the rehabilitation process in nursing home patients. Disabil Rehabil. 2014;36(12):1027–1032. doi:10.3109/09638288.2013.825331
16. Nowicki A, Ostrowska Ż. Disease acceptance in patients after surgery from breast cancer during supplementary treatment. Pol Merk Lek. 2008;XXIV(143):403–407.
17. Juczyński Z. Measurement tools in health promotion and psychology (second edition). Warsaw: Laboratory of Psychological Tests of the Polish. [Narzędzia Pomiaru w Promocji I Psychologii Zdrowia.drugie wydanie. Warszawa: Pracownia Testów PsychologicznychPolskiego Towarzystwa Psychologicznego]; 2011.
18. Albiński R, Kleszczewska-Albińska A, Bedyńska S. Geriatric depression scale (GDS). Validity and reliability of different versions of the scale-review. Polish Psychiatry. 2011;XLV(4):555–562.
19. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: A preliminary report. J Psychiatr Res. 1983;17:37–49. doi:10.1016/0022-3956(82)90033-4
20. Collin D, Wade D. Assessing motor impairment after stroke: a pilot reliability study. J Neurol Neurosurg Psychiatry. 1990;53:575–579. doi:10.1136/jnnp.53.7.576
21. Mahoney F, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61.
22. Kurpas D, Mroczek B, Bielska D. The correlation between quality of life, acceptance of illness and health behaviors of advanced age patients. Arch Gerontol Geriatr. 2013;56:448–456. doi:10.1016/j.archger.2012.12.010
23. Chrobak-Bień J, Gawor A, Paplaczyk M, Gąsiorowska A. The impact of sociodemographic and clinical factors on the degree of acceptance of the disease in people with Crohn’s disease. Pielegniarstwo I Zdrowie Publiczne. 2018;8(1):47–53. doi:10.17219/pzp/76713
24. Kapela I, Bąk E, Krzemińska S, Foltyn A. Evaluation of the level of acceptance of the disease and of the satisfaction with life in patients with colorectal cancer treated with chemotherapy. Pielegniarstwo I Zdrowie Publiczne. 2017;26(1):53–61. doi:10.17219/pzp/64689
25. Uchmanowicz I, Jankowska-Polańska B, Motowidlo U, Uchmanowicz B, Chabowski M. Assessment of illness acceptance by patients with COPD and the prevalence of depression and anxiety in COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:963–970. doi:10.2147/COPD.17
26. Chiu SY, Livneh H, Tsao LL, Tsai TY. Acceptance of disability and its predictors among stroke patients in Taiwan. BMC Neurol. 2013;13:175. doi:10.1186/1471-2377-13-175
27. Rolka H, Pilecka E, Kowalewska B, et al. Acceptance evaluation of disease and quality of life of patients with pacemaker. Piel Zdr Publ. 2012;2(3):183–192.
28. Bąk E, Marcisz C, Krzemińska S, Dobrzyn-Matusiak D, Foltyn A, Drosdzol-Cop A. Relationships of sexual dysfunction with depression and acceptance of illness in women and men with type 2 diabetes mellitus. Int J Environ Res Public Health. 2017;14(9):1073. doi:10.3390/ijerph14091073
29. Kazimierska-Zając M, Dymarek R, Rosińczuk J. Quality of life and the degree of disease acceptance in patients with spinocerebellar ataxia. JNNN. 2018;7(1):12–21.
30. Majda A, Józefowska H. Psychological status of patients with chronic obstructive pulmonary disease. Nurs Topics. 2009;17(4):283–293.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
