Back to Journals » Open Access Emergency Medicine » Volume 12
Analysis of Symptoms of COVID-19 Positive Patients and Potential Effects on Initial Assessment
Authors Korell F , Giannitsis E , Merle U , Kihm LP
Received 11 August 2020
Accepted for publication 27 October 2020
Published 3 December 2020 Volume 2020:12 Pages 451—457
DOI https://doi.org/10.2147/OAEM.S275983
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Hans-Christoph Pape
Felix Korell,1,2 Evangelos Giannitsis,3 Uta Merle,4 Lars Philipp Kihm1,5
1Casualty Department, University Hospital Heidelberg, Heidelberg, Germany; 2Department of Internal Medicine V, University Hospital Heidelberg, Heidelberg, Germany; 3Department of Internal Medicine III, University Hospital Heidelberg, Heidelberg, Germany; 4Department of Internal Medicine IV, University Hospital Heidelberg, Heidelberg, Germany; 5Department of Internal Medicine I, University Hospital Heidelberg, Heidelberg, Germany
Correspondence: Felix Korell
University Hospital Heidelberg, Im Neuenheimer Feld 410, 69120 Heidelberg, Germany
Tel +49 6221567989
Email [email protected]
Background: SARS-CoV-2 is a highly contagious virus, significantly impacting Germany among other countries since its emergence. Because of heterogeneous symptoms and a subset of patients even being asymptomatic at presentation, fast identification of infected patients remains challenging.
Objective: The goal of this study is the evaluation of different patient groups with a focus on symptoms and pre-existing illness at admission, as this is important for initial assessment and adequate emergency care.
Methods: COVID-19 positive patients at the University Hospital Heidelberg were retrospectively analyzed for disease history and symptoms at the initial presentation as well as mortality. The authors obtained institutional review board (IRB) approval by the Ethics Committee (Medical Faculty of Heidelberg University) prior to commencing the study.
Results: Dyspnea was more common in patients admitted to intermediate care/intensive care units (48 vs 13%, P< 0.001) and showed a significantly higher percentage in the deceased (91 vs 48%, P=0.004). The symptoms of all presenting patients were highly variable, and many manifestations commonly associated with COVID-19 like cough, fever, and sore throat were only detected in a subset of patients, 60%, 43%, and 33%, respectively.
Conclusion: Dyspnea was present significantly more often in patients dying of COVID-19 compared to all patients admitted to the IMC/ICU, necessitating adequate observation and monitoring. In all presenting patients, initial symptoms showed large variation; therefore, COVID should be considered as a main differential diagnosis at every patient presentation, and patients with high pre-test probability should, if possible, be isolated until testing results are known.
Keywords: COVID-19, dyspnea, mortality, triage
Introduction
The novel coronavirus, severe acute respiratory syndrome–coronavirus 2 (SARS-CoV-2), was first reported in Wuhan, China in December 2019.1–3 It has spread rapidly and globally ever since.4,5 In March 2020, it was recognized as a pandemic by the World Health Organization (WHO) and since then has had a considerable impact on the global economy and national health systems. Germany has been greatly affected by the virus. As of October 10, it ranked 22nd in numbers of infected patients worldwide (320.495), with 9.599 individuals having died of the disease (mortality rate of 3.0%).6
In the beginning, coronavirus disease 2019 (COVID-19) infection was suspected in symptomatic patients with either a travel history to a risk area or contact with an infected individual. With the increasing penetration of COVID-infection in the population, more emphasis was put on the triage of patients by clinical presentation.7 When comparing countries and regions, local differences in symptoms and death rates were found.8–11 These discrepancies, as well as varying symptoms at initial presentation, complicate and often delay the diagnosis. Therefore, a thorough investigation of every presenting patient is necessary.
In this report, data from more than 3,000 screenings and all thereof positive tested patients were analyzed. A particular focus was placed on the usefulness of a standardized emergency medical triage for COVID-19, as well as symptoms that may indicate increased mortality.
Investigation was centered on questions regarding 1) testing results, with admission rates (both hospitalization to a general ward and to an intermediate or intensive care unit (IMC/ICU)) as a primary outcome; 2) patients characteristics; 3) risk stratification evaluating potential stays in risk area(s) and chain of infection; 4) initial symptoms at presentation; 5) comorbidity; and 6) mortality analysis (secondary outcome).
Methods and Materials
Testing, Setting, and Selection
Included in the analysis were patients diagnosed and treated between February 25 and April 7, 2020. Different testing facilities for COVID-19 at the University Hospital Heidelberg were implemented: The Emergency Department began testing of patients on February 25. In an inaugural phase, both with expected organizational difficulties as well as many anticipated patients, an ambulatory COVID-19 testing center was launched for a span of 25 days, ranging from March 2 to March 27. With increasing patient numbers across the country, a dedicated Corona Emergency Department that provided case isolation was established and ambulatory testing was moved to drive-ins and primary care physicians. All patients presenting for SARS-CoV-2 testing were evaluated, and follow-up was performed until April 18.
All presenting patients were tested and included in the analysis. The patients’ naso- and oropharyngeal swabs was processed in the virology laboratory and examined by means of reverse transcriptase polymerase chain reaction (RT-PCR) to SARS-CoV-2. Testing was processed with LightMix® Modular SARS-CoV (TIB MOLBIOL GmbH; Berlin, Germany), using base stratifications set by the Virology Department Charité, Berlin, which developed the test.12 In addition, Allplex™ 2019-nCoV Assay (Seegene, inc.) was used.
Symptoms and Prior Diseases
All patients testing positive were evaluated for symptoms at admission. By percentage of occurrence these were divided into main (>10% mean in all patients) and less common (<10%) symptoms.
Additionally, all patients were screened for comorbidities such as previous cardiovascular and/or lung diseases, previous or active cancer, diabetes mellitus or other metabolic diseases, hypertension, chronic kidney failure, and others.
Patient Information
Standard demographic characteristics such as age or gender were registered.
Additionally, this evaluation includes examination of baseline characteristics and symptoms of selected groups: patient admitted to IMC/ICU and those succumbing to COVID-19.
Data Collection, Study Design, and Public Involvement
According to the Declaration of Helsinki, written informed consent for all patients was obtained and data collection and analysis had been approved by the Ethics Committee (Medical Faculty of Heidelberg University, reference number: S-148/2020). A quality control program for standardized data collection (including using medical patients records by manual review) was implemented and the study was designed as a retrospective, non-randomized analysis. The abstractor was blinded to outcomes when assessing symptoms. The same applies for the study personnel, as they were blinded from symptoms when evaluating patient outcome. No funds or time were allocated for patients or public involvement. Therefore, patients were not involved in writing or editing of the research.
Data Analysis
Continuous variables were tested for normal distribution using Kolmogorov-Smirnoff test for normality. A student´s T-test was carried out if values were normally distributed, otherwise a Wilcoxon test was carried out. Qualitative variables were compared using Chi-square test or Fisher´s exact test for small sample size. For all tests, 95%-confidence interval was calculated (denoted as CI; percentages displayed on a scale of 0–1) and a P-value<0.05 was considered to be statistically significant and indicated as follows: *P<0.05, **P<0.01, ***P<0.001. For analysis, IBM SPSS 20 for Windows (IBM Corp. Armonk, NY, USA) was used.
Results
Testing Results
In total, 3,015 tests were administered from February 25 until April 7, 2020 in the departments of internal medicine, of which a total of 352 were positive. Of these patients, 13 (3%) were initially administered for a hospital stay, while 59 (17%) had to be treated in intermediate care (IMC) or intensive care units (ICU). Two hundred and eightly patients (80%) were not admitted for stationary treatment and released after testing.
Among the patients tested, age ranged from 1 month to 91 years, with a median of 38 years. More female (56%) than male presentations were registered. Of those tested for SARS-CoV-2, admission proportion for hospital stay (0.4%) or IMC/ICU (0.2%) was low.
Patients Characteristics
Overall, of the positive patients, 55% (CI=0.48–0.61) were male. A difference was detected comparing all these patients to those admitted to the IMC/ICU (n=59), where the number of male patients rose up to 63% (CI=0.57–0.68; P=0.2). Age and gender distribution of all patients and the respective subgroups is shown in Table 1A. The age of patients without a hospital admission (median=41, range=10–77 years, CI=0.39–0.43) was significantly lower than the median age of patients admitted to the IMC/ICU (64, range=21–88 years; CI=0.59–0.67; P<0.001).
Seven patients (7%) were below age 18, none of these patients required hospitalization. Body mass index (BMI) of patients admitted to the general ward (26.1, range=18.1–31.0, CI=0.21–0.32) was comparable to those in need of IMC/ICU care (26.9, range=21.7–48.1, CI=0.24–0.31; P=0.1).
Risk Stratification
Stay in a Risk Area
The 289 patients testing positive at the COVID-19 testing center were examined for stays in risk areas, as defined by the Robert-Koch-Institute (RKI) and shown in Table 1B. While more than half of patients (52%) had no such travels, 28% had a travel history to Austria. Travel history to Italy (9%) could also be identified.
Chain of Infection
One hundred and fifty-seven of the 289 patients who tested positive were also identified to have had contact with a positive tested person (54%), according to the RKI and local authorities (Health department Rhein-Neckar). Of these patients, 110 (70%) had not been to an RKI-declared risk area.
Symptom Analysis
Figure 1 displays the main symptoms of COVID-19 positive patients. Coughing (60%) and fever (43%) were detected to be the two most prevalent symptoms in all patients. In between the analyzed subgroups however, significant differences regarding presenting symptoms were found across subgroups. While patients who were discharged after testing often experienced symptoms like sore throat (39%) and headache (30%), these symptoms were observed less frequently in patients admitted to the IMC/ICU. In contrast, dyspnea and exhaustion where far more common in patients admitted to the IMC/ICU than in discharged patients (48% (CI=0.34–0.60) vs 5% (CI=0.03–0.08), P<0.001 and 37% (CI=0.25–0.50) vs. 15% (CI=0.11–0.19), P<0.001; respectively). In addition, fever (78% (CI=0.67–0.89) vs 34% (CI=0.28–0.40), P<0.001) was also seen more often in hospitalized patients.
No symptoms at presentation were registered in 8% of patients. Pediatric patients showed no significant differences in presenting symptoms compared to the adult cohort.
Supplementary Table S1 shows the distribution of less common symptoms, while a more detailed overview and subgroup comparison of main and less common symptoms is displayed in Supplementary Tables S2 and S3.
Comorbidities
Patients were analyzed for pre-existing medical conditions and comorbidities. Regarding presumed main risk factors to a COVID-19 infection, 4% patients were identified to have a history of cardiovascular disease, and 2% had a history of lung disease, while 5% had cancer, or received immunosuppressive medication at the time of presentation. Regarding major cardiovascular risk factors, 7% had arterial hypertension, 2% diabetes mellitus, and 1% were obese. Another 6% showed metabolic diseases other than diabetes (eg, hypothyroidism), 4% gastroenterological, 3% orthopedic, and 2% neurological diseases. Very rare were renal disease (2%), skin disorders (2%), and ear/throat (1%) diseases.
The seven pediatric patients had no known comorbidities, while no significant differences in comparison to the adult cohort were seen due to the small pediatric sample size.
Supplementary Tables S4 and S5 display a detailed overview with comparison of comorbidities and distribution of past medical conditions in all subgroups, respectively.
Mortality
A total of 11 patients (3%) died from COVID-19 infection, as of 18 April. These patients, all from the adult cohort, were treated for a median of 4 (range=1–11) days until their deaths, while the median age was 82 (range=42–91) years. Of the deceased, 82% (CI=0.70–0.93) were male (vs 63% in all patients receiving intensive care; CI=0.55–0.73; P=0.1). Among the non-survivors, the age of two patients was younger than 70 years, whereas all other deceased were 75 or older. No significant differences were seen regarding the patients BMI (26.8, range=24.8–37.2, CI=0.23–0.32) compared to all other patients admitted to the general ward or IMC/ICU (26.9, range=18.1–48.1, CI=0.19–0.46, P=0.2).
Dyspnea (91%), coughing (82%), and fever (73%) were the most prevalent symptoms at initial presentation, with an overview of symptoms of all patients in need of intensive care and those later deceased displayed in Figure 2. While the latter two showed no differences to the group of all IMC/ICU patients, percentages for dyspnea were significantly higher (91% (CI=0.73–1.0) vs 48% (CI=0.34–0.60), P=0.004). Analyzing pre-existing diseases and comorbidities, 55% showed cardiovascular and 36% lung disease, while hypertension was seen in 27%. The first-mentioned (CI=0.41–0.70) was seen significantly higher compared to all IMC/ICU patients (27%, CI=0.16–0.39; P=0.04).
Discussion
In all positive tested patients, age (median 45, range=10–91 years) and gender ratio were comparable with data shown from the RKI and other publications.13,14 Primary outcome (hospital admission) was reached in 20%, while 3% died from COVID-19 (secondary outcome).
Overall, cough and fever were the most prevalent symptoms in all evaluated patients and rates were consistent with data reported from the RKI on symptoms of positive tested individuals in the German population.11,15 In other evaluations, however, there were differences regarding the frequency of observed symptoms.8–12,16 This could be due to the differences in number of cases, different population groups, or examination of groups with different stages of disease severity in these aforementioned publications.
On the contrary, dyspnea was seen more frequently in patients with severe or critical disease requiring intensive care treatment compared to patients who were not admitted (48% (CI=0.34–0.60) vs 5% (CI=0.03–0.08), P<0.001). Additionally, an even more drastic difference could be shown in deceased patients, as percentages of dyspnea at presentation were almost twice as high as in all IMC/ICU (91% (CI=0.73–1.0) vs 48% (CI=0.34–0.60), P=0.004). Supporting these findings, dyspnea had been described, in prior studies, as a potential marker for severe disease.10,17,18 As no other symptoms showed a significant difference between deceased and all other IMC/ICU patients, dyspnea needs to be closely monitored in all presenting patients because of its potential risk estimation for higher mortality.
Additional to testing of COVID-19 suspicious patients with symptoms, detection of risk areas and contact persons are indispensable components of infection control. Of the positive tested patients, 54% had contact with a positive tested person, but 70% had not been to an RKI-declared risk area. Therefore, if these patients had not developed any symptoms, they would potentially not have been tested and subsequently might have contributed to a further spread of the virus. In addition, a recent study suggests the number of people distributing the virus while still asymptomatic/pre-symptomatic to be higher than previously expected.19
Nine months since COVID-19 has been declared as a pandemic disease, detection and treatment of infection with SARS-CoV-2 remains challenging, as is management of positive tested patients. A sequential model was implemented at our institution for adequate testing while at the same time adjusting capacities for possibly rapidly increasing numbers of cases. In the Corona testing Center, many patients with mild or absent symptoms, presenting after having traveled to a risk area or had contact with a positive tested person, could be tested simultaneously. After the initial wave of infected patients, mostly returning from risk areas in Italy or Tyrolia (Austria), the newly established Corona Emergency Department took over for a more individualized check-up on potential COVID-19 positive patients. Additionally, a “corona taxi” was initiated for regular assessment of positive tested patients not admitted to hospital.20
In summary, when analyzing all patients presenting, symptoms showed to be inconsistent, with symptoms varying heavily from patients with COVID-19 suspicious symptoms – like cough, fever, and sore throat – to patients with little (like rhinitis), unspecific (like epigastric pain or fainting), or no symptoms. Respiratory symptoms were the most common findings in this analysis as well as in other studies.21,22 With this and more knowledge about the distribution of SARS-CoV-2 through asymptomatic/pre-symptomatic patients, a change in selection and triage might be needful. Additionally, fever was found in less than half of all patients and only in a third of the patients not admitted. In this context, a fever measurement alone or facilities such as special fever clinics appear to be of little use to adequately quantify a risk for infection. Therefore, most or at least those patients with high pre-test probability should be treated like a suspected COVID-19 issue.21 Because of this, sufficient protective measures as well as thorough laboratory, radiological, and other symptom-specific diagnostic investigations can be provided, leading to a reduction of infection or missed cases.22 These measures should be maintained until a negative test result on COVID-19 is obtained. This can potentially contribute to containment with return to the situation at the beginning of the pandemic – individual cases, where a detailed analysis for suspects and whereabouts as well as sufficient medical care at all times is possible again. Infection control by stringent quarantine of symptomatic patients and rigorous contact tracing have so far been the most effective measures.22
Limitations of this analysis include small sample size in some evaluated patient groups like patients admitted to a general ward as well as the relatively small number of deceased patients with regards to all patients. In addition, not all findings may be applicable to the general public due to the character of a single center report and relative short time frame. Therefore, while some findings may be concerning regarding the differences in symptoms at presentation, there is caution needed in the interpretation of these findings due to the small number of cases (59 patients in intensive care and 11 deceased) and its data being collected retrospectively. There is likely confounding between the symptoms at presentation and the disposition of the patient, as patients with fever and dyspnea are more likely to be admitted to the hospital/ICU, which may limit the interpretation. Furthermore, not enough data on sensitivity and specificity of the SARS-CoV-2 PCR testing is available yet, leaving questions to whether there is a clear and complete picture on COVID-19 and its effects.
Conclusion
The unspecific nature of symptoms of patients with COVID-19 infection prohibits a proper preselection of patients that require isolation in order to reduce contamination. Dyspnea indicates a more severe disease stage and may predict a fatal outcome with a more than 2-fold higher risk in comparison to all IMC/ICU patients. However, while this warrants close monitoring during stationary treatment, dyspnea itself remains unspecific. Additionally, at times when COVID-19 infection cannot be suspected by a travel history to a risk area, triage of patients to a regular emergency department or chest-pain unit versus a dedicated isolation ward is increasingly challenging as COVID-19 spreads within the population. Therefore, every patient presentation should feature COVID as a main differential diagnosis, and patients with high pre-test probability should be, if possible, isolated until testing results are known.
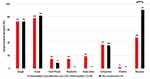 |
Figure 2 Main symptoms at presentation for all intensive care patients and those later deceased. **P<0.01. |
Acknowledgments
The authors have nothing to acknowledge.
Author Contributions
FK and LPK designed the research project. FK acquired and analyzed the data. FK, LPK, EG, and UM discussed the data and the organization of the manuscript. FK wrote the manuscript. All authors critically reviewed the manuscript, FK, LPK, and EG edited the manuscript. LPK supervised the work. FK and LPK undertook recruitment of participating patients and managed the data, including quality control. FK, EG, and LPK provided statistical advice on the study design and analyzed the data. LPK chaired the data oversight committee. All authors contributed (as listed above) to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
Evangelos Giannitsis reports personal fees from AstraZeneca, grants from Roche Diagnostics, Daiichi Sankyo, and Brahms Thermo Fisher. The authors report no other potential conflicts of interest for this work.
References
1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506.
2. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi:10.1056/NEJMoa2001017
3. WHO. Novel coronavirus – China. January 12, 2020. Available from: http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/.
4. Taylor DB. A timeline of the coronavirus. The New York Times. February 13, 2020. Available from: https://www.nytimes.com/2020/02/13/world/coronavirus-timeline.html.
5. CDC. 2019 Novel Coronavirus (2019-nCoV) situation summary. Centers for Disease Control and Prevention. February 11, 2020. Available from: https://www.cdc.gov/coronavirus/2019-ncov/summary.html.
6. Johns-Hopkins University & Medicine Coronavirus Resource Center.
7. Zhang J, Zhou L, Yang Y, et al. Therapeutic and triage strategies for 2019 novel coronavirus disease in fever clinics. Lancet Respir Med. 2020;8(3):e11–e12. doi:10.1016/S2213-2600(20)30071-0
8. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). March, 2020. Available from: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdfDisease.2020.
9. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi:10.1016/S2213-2600(20)30079-5
10. Wu J, Liu J, Zhao X, et al. Clinical characteristics of imported cases of COVID-19 in Jiangsu province: a multicenter descriptive study. Clin Infect Dis. 2020. doi:10.1093/cid/ciaa199
11. Robert-Koch Institute. SARS-CoV-2 fact sheet for Coronavirus Disease-2019 (COVID-19). Available from: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Steckbrief.html.
12. Corman VM, Landt O, Kaiser M, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25(3):2000045. doi:10.2807/1560-7917.ES.2020.25.3.2000045
13. Daily report of the RKI (Robert-Koch Institute) on Coronavirus Disease-2019 (COVID-19), as of 05. 03.2020 - (original text: täglicher lagebericht des RKI (Robert-Koch Institute) zur coronavirus-krankheit-2019 (COVID-19)).
14. Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720.
15. Lake MA. What we know so far: COVID-19 current clinical knowledge and research. Clin Med (Lond). 2020;20(2):124–127. doi:10.7861/clinmed.2019-coron
16. Zhu J, Ji P, Pang J, et al. Clinical characteristics of 3062 COVID‐19 patients: a meta‐analysis. J Med Virol. 2020. doi:10.1002/jmv.25884
17. Yang W, Cao Q, Qin L, et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): a multi-center study in Wenzhou city, Zhejiang, China. J Infect. 2020;80(2020):388–393. doi:10.1016/j.jinf.2020.02.016
18. Chen J, Qi T, Liu L, et al. Clinical progression of patients with COVID-19 in Shanghai, China. J Infect. 2020;80(5):e1–e6. doi:10.1016/j.jinf.2020.03.004
19. He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020. doi:10.1038/s41591-020-0869-5
20. A German Exception? Why the country’s coronavirus death rate is low, NY Times, April 4, 2020.
21. Sahu KK, Mishra AK, Lal A. COVID-2019: update on epidemiology, disease spread and management. Monaldi Arch Chest Dis. 2020;90(1). doi:10.4081/monaldi.2020.1292
22. Mishra AK, Sahu KK, George AA, et al. A review of cardiac manifestations and predictors of outcome in patients with COVID-19. Heart Lung. 2020:
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


