Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
Analysis of Modifiable, Non-Modifiable, and Physiological Risk Factors of Non-Communicable Diseases in Indonesia: Evidence from the 2018 Indonesian Basic Health Research
Authors Arifin H , Chou KR , Ibrahim K , Fitri SUR , Pradipta RO , Rias YA , Sitorus N, Wiratama BS, Setiawan A, Setyowati S, Kuswanto H, Mediarti D, Rosnani R, Sulistini R, Pahria T
Received 13 July 2022
Accepted for publication 19 September 2022
Published 30 September 2022 Volume 2022:15 Pages 2203—2221
DOI https://doi.org/10.2147/JMDH.S382191
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hidayat Arifin,1,2 Kuei-Ru Chou,2 Kusman Ibrahim,1 Siti Ulfah Rifa’atul Fitri,1 Rifky Octavia Pradipta,3 Yohanes Andy Rias,4 Nikson Sitorus,5 Bayu Satria Wiratama,6 Agus Setiawan,7 Setyowati Setyowati,8 Heri Kuswanto,9 Devi Mediarti,10 Rosnani Rosnani,10 Rumentalia Sulistini,10 Tuti Pahria1
1Department of Medical and Surgical Nursing, Faculty of Nursing, Universitas Padjadjaran, Bandung, Indonesia; 2School of Nursing, College of Nursing, Taipei Medical University, Taipei, Taiwan, Republic of China; 3Department of Fundamental Nursing Care, Faculty of Nursing, Universitas Airlangga, Surabaya, Indonesia; 4Department of Medical and Surgical Nursing, Institut Ilmu Kesehatan Bhakti Wiyata Kediri, Kediri, Indonesia; 5Research Center for Public Health and Nutrition, National Research and Innovation Agency, Jakarta, Indonesia; 6Department of Biostatistics, Epidemiology, and Population Health, Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia; 7Department of Community Nursing, Faculty of Nursing, Universitas Indonesia, Depok, Indonesia; 8Department of Maternity Nursing, Faculty of Nursing, Universitas Indonesia, Depok, Indonesia; 9Department of Statistics, Institut Teknologi Sepuluh Nopember, Surabaya, Indonesia; 10Politeknik Kesehatan Kemenkes Palembang, Palembang, Indonesia
Correspondence: Hidayat Arifin, Department of Medical Surgical Nursing, Faculty of Nursing, Universitas Padjadjaran, Jl. Raya Bandung-Sumedang, KM. 21, Hegarmanah, Jatinangor, Sumedang, West Java, 45363, Indonesia, Tel +62 811 3194 433, Email [email protected]
Purpose: Indonesia is facing an increasing occurrence of non-communicable diseases (NCDs) every year. We assessed the modifiable, non-modifiable, and physiological risk factors of NCDs among the Indonesian population.
Methods: Secondary data was analyzed from the 2018 Indonesian basic health research (RISKESDAS). The national survey included participants aged 15– 54 years and obtained 514,351 responses. Linear systematic two-stage sampling was conducted by RISKESDAS. Furthermore, chi-square and binary logistic regression were utilized to explore the determinant of NCDs with a significance level of 95%.
Results: We found that almost 10% respondents in Indonesia had NCDs. We observed that depression has a higher odd (aOR: 2.343; 95% CI: 2.235– 2.456) contributed to NCDs and followed other factors such as no education (aOR: 1.049; 95% CI: 1.007– 1.092), passive smoking (aOR: 0.910; 95% CI: 0.878– 0.942), fatty food (aOR: 1.050; 95% CI: 1.029– 1.073), burnt food (aOR: 1.033; 95% CI: 1.005– 1.062), food with preservatives (aOR: 1.038; 95% CI: 1.002– 1.075), seasoned food (aOR: 1.057; 95% CI: 1.030– 1.084), soft drinks (aOR: 1.112; 95% CI: 1.057– 1.169), living in an urban area (aOR: 1.143; 95% CI: 1.119– 1.168), living in central Indonesia (1.243; 95% CI: 1.187– 1.302), being female (aOR: 1.235; 95% CI: 1.177– 1.25), and obese (aOR: 1.787; 95% CI: 1.686– 1.893). Conversely, people in Indonesia who undertook vigorous activity (aOR: 0.892; 95% CI: 0.864– 0.921), had employment (aOR: 0.814; 95% CI: 0.796– 0.834), had access to improved sources of drinking water (aOR: 0.910; 95% CI: 0.878– 0.942), and were aged 35– 44 years (aOR: 0.457; 95% CI: 0.446– 0.467) were less likely to develop NCDs.
Conclusion: Modifiable, non-modifiable, and physiological risk factors have a significant influence on NCDs in Indonesia. This finding can be valuable information for Indonesian Government to arrange a cross-collaboration between government, healthcare workers, and society through advocacy, partnership, health promotion, early detection, and management of NCDs.
Keywords: non-communicable diseases, NCDs, Indonesia, RISKESDAS
Corrigendum for this paper has been published.
Introduction
Non-communicable diseases (NCDs) are one of the biggest health challenges in the 21st century1 and have become a global concern in both developing and developed countries.2 NCDs are responsible for 41 million of 57 million deaths (71%) and consist of cardiovascular disease (44%), cancer (9%), chronic respiratory diseases (9%), diabetes (4%), and 75% of premature deaths (death at the age of 30–69 years) in the world.3 Data in Indonesia states that NCDs were the main cause of death in 2016. NCDs are responsible for 73% of deaths in Indonesia and the proportions are: cardiovascular disease (35%), cancer (12%), chronic respiratory diseases (6%), diabetes (6%), and the risk of premature death is more than 20%.1 This indicates that the incidence of NCDs should be a concern.
Indonesia is experiencing rapid technological development, environmental changes, and lifestyle shifts from a traditional to modern living. These developments and shifts have changed the pattern of disease in society, which is now dominated by NCDs.4 Changes in disease trends are also followed by shifts in disease patterns. Previously, NCDs were more commonly found among older people. Currently, the prevalence of disease is increasing among the 10–14-year-old age group, and the most common diseases are stroke, cardiovascular disease, and diabetes.5 If the trend of NCDs in children is not controlled, the government’s efforts to produce a healthy generation will be difficult to achieve, especially given that by 2030–2040, Indonesia is expected to face a demographic bonus where the productive age dominates the population.6 Thus, prevention plays an important role in reducing the risk of NCDs.
Most NCDs are caused by preventable and modifiable factors.7 The World Health Organization (WHO) made a target to reduce NCDs by controlling behavioral risk factors (consumption of alcohol, tobacco, salt, and physical activity) and metabolic risk factors (obesity and blood pressure).8 Meanwhile, the Indonesian government program to reduce the consumption of salt, sugar, fat, alcohol, and tobacco, increasing physical activity, and getting enough rest which were covered in the National Action Plan on NCDs control.9 Based on global and national policy, one of the important components in preventing NCDs is the control of modifiable and physiological risk factors.
The previous study mentioned that predictive, preventive, and personalized medicine (PPPM) can be a solution for NCDs.10 PPPM, a novel integrative concept in healthcare, allows for the prediction of a person’s propensity for a disease before it manifests, the provision of focused preventative interventions, and the development of individualized treatment algorithms for NCD patients.11 To stand the predictive of NCDs, we need the prognosis of treatment algorithm and efficiency, early diagnosis, risk assessment, and innovative screening. While, the preventive starts from improve the public health educational, targeted prevention of potential complication, and effective treatment management. Additionally, treatment algorithm tailored to the individual, personalized therapy monitoring and prognosis, and personalized patient profiling are needed to personalized medical care.10
One solution for NCD prevention is to control risk factors. Previous research has stated that the risk factors for NCDs are behavioral, metabolic, and socio-demographic.2,12–16 Unfortunately, these previous studies were only conducted at the city level,13,14 only involved adolescent respondents,16 and only examined DM as NCDs.12 The modernization of food in the Indonesian diet, such as the introduction of instant food and energy drinks,17 has not been studied. This study aimed to analyze the modifiable, non-modifiable, and physiological risk factors of NCDs in Indonesia. Researchers examined the risk factors for NCDs in the 15–54-year age group, used national data, examined risk factors that had not been studied in previous studies, and adopted the framework of the National Action Plan of Prevention and Handling of NCDs, Ministry of Health of the Republic of Indonesia.9 Information on the prevalence and risk factors of NCDs nationally can assist the Indonesian government in predicting and designing multisectoral policies so that NCDs risk factors can be controlled and the number of sufferers is reduced.
Materials and Methods
Study Design
A cross-sectional study was designed using secondary data from the 2018 Indonesian Basic Health Research (RISKESDAS) that was nationally conducted by the National Institute of Health Research and Development, Ministry of Health of the Republic of Indonesia. The 2018 RISKESDAS is integrated with The National Socio-Economic Survey (Susenas) and was conducted by Statistics Indonesia (BPS) in March 2018, in 34 provinces.18
Data Sources & Samples
Samples were taken from the 2018 RISKESDAS, which consisted of 30,000 census blocks (CBs) in urban and rural areas of Susenas with 300,000 household responses.18 The total survey included 565,592 individual observations obtained by linear systematics with two-stage sampling. The sampling was done in two stages: 1) Implicit stratification of all CBs from the 2010 population census based on welfare strata. Twenty-five percent of the total CBs were then systematically determined with the probability proportional to size (PPS) method to get 30,000 CBs. 2) A total of 10 households were chosen based on the highest level of education of the head of household to maintain the representativeness of the value diversity of household characteristics.18
RISKESDAS in determining the instrument components refers to the Sustainable Development Goals, National Mid-Term Development Plan, Strategic Plan, Minimum Service Standards, Community Health Development Index, Healthy Indonesia Program – Family Approach, and the Healthy Living Community Movement developed by the Government of Indonesia. The primary health indicators measured in RISKESDAS 2018 include morbidity (Non-Communicable Diseases and Infectious Diseases), disability, injury, environmental health (hygienic, sanitation, latrines, water and housing), knowledge and attitudes towards HIV, health behaviour (seeking treatment, tobacco use, drinking alcohol, physical activity, risky food consumption behaviour), various aspects of health services (access and health coverage) and nutritional status, as well as dental and oral health status. Then the questionnaire was tested for validity by RISKESDAS before being used.19
We included respondents aged 15–54 years and excluded missing responses from this study. Furthermore, the proportion of each region was calculated by weighting the observation based on the number of provinces in Indonesia. Out of 565,592 individual observations, approximately 51,241 observations were excluded from this study due to missing values for one or more variables. Finally, a total of 514,351 (245,234 males and 269,117 females) were recorded in this study.
Variables
In this study, we adopted and modified the framework of NCDs risk factors from the National Action Plan of Prevention and Handling of NCDs, Ministry of Health of the Republic of Indonesia.9 The framework consisted of modifiable risk factors (behavioral and environmental), non-modifiable risk factors, and physiological risk factors (Figure 1). Furthermore, we constructed independent variables consisting of: behavioral – modifiable risk factors (education level, smoking, level of activity, and the consumption of sweet food, fatty or fried food, burnt food, food containing preservatives, seasoned food, instant food, soft drinks, and energy drinks); environmental—modifiable risk factors (working status, residence, regional, time spent at a health facility, source of drinking water, and depression); non-modifiable risk factors (age and gender); and physiological risk factors (body mass index).
 |
Figure 1 Framework of modifiable, non-modifiable, and physiological risk factors. |
Behavioral – modifiable risk factors: Level of education was categorized into high education, secondary education, primary education, and no education.20 Smoking was organized into no, passive smoker, and active smoker. Level of activity was categorized into gentle, moderate, and vigorous.21 The consumption of sweet food, fatty or fried food, burnt food, food containing preservatives, seasoned food, instant food, soft drinks, and energy drinks were classified into < 3 times/week and ≥ 3 times/week.22
Environmental – modifiable risk factors: Working status and residence were classified into yes/no and rural/urban respectively. Regional areas were classified based on time differences in Indonesia, namely Eastern Indonesia, Central Indonesia, and Western Indonesia.23 Time spent to health facility was organized into fast (≤ 8 minutes) and slow (> 8 minutes).24 Source of drinking water was classified into bottled water, improved (refill water, tap water, retail/purchase tap water, drill/pump well, protected dug well, and protected spring), and not improved (unprotected dug wells, unprotected springs, rainwater storage, and surface water (rivers/ lakes/ irrigation)). We introduced the bottled water category because the prevalence of bottled water usage has increased in Indonesia.25 Additionally, depression was categorized into no and yes based on questionnaire developed by RISKESDAS with mean as the cut of point.
Non-modifiable risk factors: We classified age into four categories (15–24 years, 25–34 years, 35–44 years, and 45–54 years).26 Gender was classified into male and female categories.
Physiological risk factors: Body mass index (BMI) was classified into underweight (under 18.5 kg/m^2), normal (greater than or equal to 18.5 to 24.9 kg/m^2), overweight (greater than or equal to 25 to 29.9 kg/m^2), and obese (greater than or equal to 30 kg/m^2).27
The dependent variable in this study was NCDs. It was composed of seven diseases: stroke, cardiovascular disease, diabetes mellitus, cancer, hypertension, renal disease, and asthma. All the NCDs were declared and diagnosed by medical doctor and recorded in patient’s medical records. The seven selected diseases were identified as the most common diseases in Indonesia.28 If the respondents had one or more of the seven diseases, the variables of NCDs were categorized as NCDs and organized into yes and no.
Data Analysis
This study was written using the strengthening the reporting of observational studies in epidemiology (STROBE) statement as a guideline, and all of the methodologies were carried out to conform to the appropriate standards and regulations.29 STATA version 16.1 was used to carry out the data analysis. We used univariate analysis to present the weighted percentages of independent and dependent variables. We also used the chi-square test to investigate the association between each variable. The factors associated with NCDs in Indonesia were examined using binary logistic regression. The adjusted odds ratio (aOR) was presented in the study, along with a 95% confidence interval (CI) and a p-value of 0.05. Since the nationwide survey was used, we performed STATA’s “svy” survey commands to account for clustering effects, and sample weight due to multi-stage cluster random sampling was used in the data collection.
Ethical Consideration
Ethical considerations were considered and approved by the Health Research Ethics Committee and the National Institute of Health Research and Development in accordance with the Helsinki Declaration30 with number LB.02.01/2/KE.024/2018. We have received an approval to use the data with number IR.03.01/4/5388/2021 from the National Institute of Health Research and Development, Ministry of Health of the Republic of Indonesia. Written informed consent for each individual was obtained by the 2018 Indonesian Basic Health Research.
Results
National survey data representing Indonesia are presented in this study. We presented risk factors of NCDs into behavioral – modifiable risk factors, environmental – modifiable risk factors, non-modifiable risk factors, and physiological risk factors.
Behavioral – Modifiable Risk Factors
In a total of 514,351 respondents, it was found that almost half had a primary level of education. The majority of the respondents were found to be non-smokers (62.6%) and more than 50% of the activity level results were in the moderate category. The results for consuming food and beverages revealed that burnt food (86.17%), food with preservatives (89.14%), instant food (71.06), soft drinks (94.27%), and energy drinks (95.70%) were consumed ≤ 3 times per week. Additionally, sweet food (60.31%), fatty or fried food (64.57%), and seasoned food (84.69%) were consumed ≥ 3 times per week (Table 1).
 |  |  | 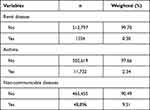 |
Table 1 Respondents’ Characteristic, Demographic, and Distribution of Non-Communicable Diseases (n = 514,351) |
Environment – Modifiable Risk Factors
We found that the majority (73.15%) are employed, and more than half of the total respondents live in urban areas. The survey showed that the majority of participants are from Western Indonesia (79.17%). The majority of time spent at health facilities was categorized as slow (92.55%), the majority of drinking water sources were categorized as improved and 11.65% consume bottled water. Additionally, the majority of respondents were found to be not depressed (Table 1).
Non-Modifiable Risk Factors
From the survey, the age range of 15–54 years was evenly distributed (>20%). As many as 50.1% are male and the rest are female (Table 1).
Physiological Risk Factors
A total of 51.39% of the total survey respondents had a normal Body Mass Index (BMI) (Table 1).
From the NCD data in Table 1, it is known that the prevalence of stroke is 0.41%, cardiovascular disease (1.25%), diabetes mellitus (1.16%), cancer (0.19%), hypertension (4.81%), renal disease (0.30%), asthma (2.34%), and had NCDs (9.51%).
The results of the bivariate analysis regarding the determinants of non-communicable diseases in Indonesia are presented in Table 2. It is known that age, gender, education level, working status, residence, regional, time spent at a health facility, water, smoking, level of activity, BMI, depression, and the consumption of sweet food, fatty or fried food, food containing preservatives, instant food, soft drinks, and energy drinks have a correlation with NCDs in Indonesia (p < 0.05). Additionally, burnt food and seasoned food have no significant correlation with NCDs in Indonesia (p > 0.05).
 |  |  |
Table 2 Bivariate Analysis of Determinants of Non-Communicable Diseases in Indonesia |
The results of the logistic regression analysis are presented in Table 3. From behavior-modifiable risk factors, we found that respondents with no education were 1.049 times more likely to have NCDs rather than those with a higher education (p = 0.020; aOR: 1.049; 95% CI: 1.007–1.092). Passive smokers are 1.185 times more likely to have NCDs compared with smokers (p < 0.001; aOR: 0.910; 95% CI: 0.878–0.942). Respondents with moderate levels of activity are 0.892 times less likely to have NCDs than those who do a gentle level of activity (p < 0.001; aOR: 0.892; 95% CI: 0.864–0.921). In food and beverage consumption, we found that respondents who consume fatty or fried food (p < 0.001, aOR: 1.050; 95% CI: 1.029–1.073), burnt food (p = 0.020, aOR: 1.033; 95% CI: 1.005–1.062), food containing preservatives (p = 0.034, aOR: 1.038; 95% CI: 1.002–1.075); seasoned food (p < 0.001, aOR: 1.057; 95% CI: 1.030–1.084); and soft drinks (p < 0.001, aOR: 1.112; 95% CI: 1.057–1.169) for ≥ 3 times per week are more likely to have NCDs compared with the group who consumed these foods and drinks ≤ 3 times per week.
 |  |  |
Table 3 Binary Regression Analysis of Determinants of Non-Communicable Diseases in Indonesia |
Environmental – modifiable risk factors show that the respondents who have a working status are 0.814 times less likely to have NCDs than people who did not have working status (p < 0.001; aOR: 0.814; 95% CI: 0.796–0.834). People from urban areas were 1.143 times more likely to have NCDs compared with respondents who live in rural areas (p < 0.001; aOR: 1.143; 95% CI: 1.119–1.168). Regional disparities in Indonesia show that people from Central Indonesia are 1.243 times more likely to contract NCDs compared with Eastern Indonesia (p < 0.001; aOR: 1.243; 95% CI: 1.187–1.302). Respondents who consumed water from improved sources are 0.910 times less likely to have NCDs compared with those who consume bottled water (p < 0.001; aOR: 0.910; 95% CI: 0.878–0.942). Additionally, respondents with depression are 2.343 times more likely to have NCDs compared with those who did not have depression (p < 0.001; aOR: 2.343; 95% CI: 2.235–2.456) (Table 3).
For the non-modifiable risk factors, we learned that respondents aged 35–44 years are 0.457 times less likely to have NCDs than respondents aged 45–54 years (p < 0.001; aOR: 0.457; 95% CI: 0.446–0.467). In this study, females were 1.235 times more likely to have NCDs compared with males (p < 0.001; aOR: 1.235; 95% CI: 1.177–1.25). Physiological risk factors indicated that respondents in the obese category were 1.787 times more likely to have NCDs than respondents who were underweight (p < 0.001; aOR: 1.787; 95% CI: 1.686–1.893) (Table 3).
Discussion
In this study, we found that behavioral (modifiable risk factors), environment (modifiable risk factors), non-modifiable risk factors, and physiological risk factors significantly contribute to NCDs in Indonesia. These risk factors can enhance the likelihood of developing NCDs and can be characterized in a variety of ways.31 Thus, management of NCD risk factors should be initiated by understanding the characteristics of each risk factor.
Behavioral – Modifiable Risk Factors
In this study, respondents with no education were more likely to contract NCDs compared with those with a higher education level. It is important to note that education level is a predictor of the incidence of NCDs. This finding is in line with previous studies.32,33 Society needs basic information on the maintenance of a healthy lifestyle to prevent NDCs.34 It is assumed that people with a higher education level could receive and understand the information regarding a healthy lifestyle and implement it in their daily lives.35 By optimizing education levels, correct and easily understood information can be widely distributed to decrease the prevalence of NCDs.35,36 However, in Indonesia, we are challenged by cultural and belief barriers that sometimes contradict information regarding NCDs. Thus, for further strategic programs, healthcare workers, such as nurses, need to collaborate with local authorities to share information regarding the management, control, and prevention of NCDs.
Another behavioral – modifiable risk factor is smoking. We found that passive smokers are more likely to contract NCDs. This is supported by previous studies.37,38 Passive smoking is more dangerous than active smoking because it can increase the risk of respiratory illnesses, including asthma, bronchitis, and pneumonia.39–42 Exposure to tobacco smoke will contribute to a change in metabolism, gene mutation, and deoxyribonucleic acid (DNA) damage that will affect the seriousness of NCDs, such as cancer.42–44 The most challenging task is changing the beliefs and behavior of smokers who believe that smoking cigarettes does not cause NCDs. Thus, a comprehensive approach is needed to solve this problem.
In this study, respondents with vigorous activity levels had a lower likelihood of contracting NCDs in Indonesia. Increased physical activity can have a positive impact on the body’s metabolic system and can reduce metabolic syndrome in patients with NCDs.45–47 Physical activity released dopamine and glucoregulatory hormones to reduce stress.48–50 Thus, a regular program of increased activity levels should be promoted and initiated at the government, company, and societal levels.
We found that fatty food, burnt food, food containing preservatives, seasoned food, and soft drinks consumed more than three times per week had a significant contribution to NCDs. Fatty food increases cholesterol blood levels and causes hypertension and cardiovascular diseases;51 burnt food has become a predictor and derived carcinogen of cancer;52,53 and preservatives, seasoned food, and soft drink will affect metabolism, gene mutation, and bone mineral density that leads to NCDs.53–56 However, a European study found that seasoning food with herbs can prevent NCDs.50 Clear information regarding healthy food and drinks is important and should be delivered to communities through health education programs. Additionally, collaborations between healthcare workers and the government on the distribution of risky food should be initiated.
Environmental - Modifiable Risk Factors
In this study, the respondents that have working status were less likely to have NCDs than people who did not have working status. This is because people who work have more activities, which can prevent a sedentary lifestyle.57 In addition, people who have jobs and earn money can better regulate their lifestyle by eating healthy foods, such as fruits and vegetables. Conversely, people who do not work are at risk of experiencing stress because they do not have an income. The combination of stress and a sedentary lifestyle can trigger the emergence of NCD diseases such as stroke and diabetes mellitus.58,59
People living in urban areas are more likely to have NCDs than people living in rural areas. Previous studies have shown that urban societies that have greater access to processed, high calorie, high fat, and salty foods can easily develop NCDs.60 Also, urban societies that are supported by easy access to public facilities can develop sedentary lifestyles, which can lead to lower levels of physical activity.61 Socioeconomic status among the urban population can shape people’s behavior to choose an unhealthy lifestyle. Lack of physical activity and exercise, lack of intake of nutritious foods such as fruits and vegetables, consuming foods that are high in fat, calories, and sodium, alcoholic beverages, and smoking habits can significantly increase the incidence of NCDs. The results of the study also indicated that people who live in Central and Western Indonesia are more likely to have NCDs compared with those in Eastern Indonesia. Central and Western Indonesians are in the urban category, where people’s lifestyles are often sedentary, in contrast to Eastern Indonesia, which is included in the rural area. People in rural areas tend to adhere to a simple culture with a natural environment and informal social life.
Respondents who consumed water from improved sources are less likely to have NCDs compared with those who consume bottled water. Health problems can occur because chemical substances that can harm the body have been found in some bottled water. A previous study in Malawi found that from 12 samples of bottled water, 10 brands did not comply with the Malawi Standards (MS) 699 (2004) turbidity standard (1 Nephelometric Turbidity Units (NTU)), and the pH of one of the brands was below the minimum MS 699 (2004) standard of 6.50.62 Also, all the brands had bottle labeling errors and discrepancies in chemical composition. Another study found the presence of microplastics in bottled water that led to contamination that partially came from the packaging and/or the bottling process itself.63,64 Contaminated water in bottles can trigger cancer because microplastic can enter and be absorbed into the body. Repeated use of drinking water bottles should also be avoided because plastic bottles are intended for single use only.
Our study found that people who have depression are more likely to have NCDs compared with those who did not have depression. Depression in a person can be caused by physical or psychological factors. Prolonged depression makes a person disabled, and it can interfere with health. Previous research has shown that depression can be a precursor to disease and a double burden for an NCD sufferer.65 Depression and NCDs are interrelated and can be mutually exclusive. In accordance with previous research that states that someone who has an NCD requires adjustment to their condition. Living with pain, disability, and social and economic problems is what triggers depression.66,67 Another study also stated that depression was twice as common in patients with NCDs and is prevalent in 40% of diabetic patients, 37% of cancer patients, 38% of hypertension patients, and 39% of stroke patients.68 Indirectly, depression can increase the morbidity and mortality of NCDs.69
Non – Modifiable Risk Factors
This study found that respondents aged 35–44 years are less likely to have NDCs than respondents aged 45–54 years. This is related to the previous study that conducted in Southern India indicated by the correlation of NCDs with increasing age.70,71 As they get older, many people are exposed to risk factors for longer periods, then difficulties can arise and NCD clinical syndromes develop.72 In this study, the prevalence of NCDs similarly increased with age. The frequency of NCDs increased the most in a very young age group (30–49 years). These findings point to the population’s early development of NCDs, which must be addressed.
Females are more likely to have NCDs compared with males. This finding is related to biological risk factors, including being overweight or obese, as well as elevated blood pressure, glucose, and cholesterol, which are seen in a higher percentage of women in older age groups.73 In developing countries, such as Indonesia, the prevalence of selected behavioral and clinical risk factors was higher among women than men.74 Treatment-seeking behavior is slightly better among men than women.75 The government should take the vulnerability of women into account while designing and implementing programs to prevent and control NCDs.
Physiological Risk Factor
The physiological risk factors in this study were measured from BMI. We found that obese respondents had more susceptibility to NCDs in Indonesia. Obesity, in particular, affects nearly every facet of health, from reproductive and pulmonary function to cognition and mood. Obesity raises the risk of a variety of severe and fatal diseases, including diabetes, heart disease, and some malignancies.76,77 Thus, weight-loss management is important for a healthy life. Obesity prevention, starting at a young age and continuing throughout one’s life has the potential to greatly enhance individual and public health, as well as reduce the chance of suffering from NCDs.
Strength and Limitations
The study presents the data regarding risk factors of NCDs nationally. This study covered respondents from younger to older age and presented Indonesian population data that can represent the characteristics of respondents. Additionally, this study uses a framework that has been developed by the Ministry of Health of the Republic of Indonesia, which has been adapted to the characteristics of the Indonesian population. Thus, these findings can be used as a reference and source of information for the Indonesian government to determine policies for the management and control of NCDs. However, the data presented by RISKESDAS is still limited and does not provide data related to beliefs and culture that can be used for the proper handling of NCDs using a local approach. The gender and urban-rural disparity analysis will present rich information like the previous study in Kerala, India.78
Conclusion
The Indonesian government should pay attention to the prevention and handling of NCDs. Modifiable, non-modifiable, and physiological risk factors are the most significant causes of NCDs in Indonesia and need to be addressed. The utilization of healthcare and cross-collaboration among healthcare workers, government, and society should be provided through advocacy, partnerships, health promotion, steps for early detection, and management of NCDs. However, the program should take local culture, beliefs, and regional differences into consideration. Healthcare workers, especially nurses, should collaborate with local public authorities to educate the target population to optimize the screening, control, and NCDs management and treatment. Furthermore, the results of this study will be valuable as essential information for further policies and interventions to promote PPPM as a new suggestion on NCDs.
Acknowledgments
We acknowledge to Ministry of Health of Republic of Indonesia and RISKESDAS who supported and provided the data for this study.
Disclosure
The authors have declared no conflicts of interest in relation to this work.
References
1. World Health Organization. Noncommunicable Diseases Country Profiles 2018. World Health Organization; 2018.
2. Dahal S, Sah RB, Niraula SR, Karkee R, Chakravartty A. Prevalence and determinants of non-communicable disease risk factors among adult population of Kathmandu. PLoS One. 2021;16(9):e0257037–e0257037. doi:10.1371/journal.pone.0257037
3. World Health Organization. Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016. World Health Organization; 2018.
4. Purnamasari D. The emergence of non-communicable disease in Indonesia. Acta Med Indones. 2018;50(4):273–274.
5. Ministry of Health. Kolaborasi pusat dan daerah dalam penguatan yankes menuju cakupan kesehatan semesta [Central and regional collaboration in strengthening health care services towards universal health coverage]. 2019. Indonesian
6. Widyawati Widyawati. Penyakit tidak menular kini ancam usia muda [Non-communicable diseases are now threatening young people]. 2021. Indonesian
7. World Health Organization. Fact Sheets on Sustainable Development Goals: Health Targets; 2017.
8. World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. World Health Organization; 2017.
9. Indonesia KKR. Rencana Aksi Nasional Pencegahan dan Pengendalian Penyakit Tidak Menular [National Action Plan for Prevention and Control of Non-Communicable Diseases]. Kementerian Kesehatan Republik Indonesia; 2017.
10. Wang W, Yan Y, Guo Z, et al. All around suboptimal health — a joint position paper of the Suboptimal Health Study Consortium and European Association for Predictive, Preventive and Personalised Medicine. EPMA J. 2021;12(4):403–433. doi:10.1007/s13167-021-00253-2
11. Chaari L. Digital Health in Focus of Predictive, Preventive and Personalised Medicine. Springer Cham; 2020.
12. Kristanti D, Rahajeng E, Sulistiowati E, Kusumawardani N, Dany F. Determinants of diabetes comorbidities in Indonesia: a cohort study of non-communicable disease risk factor. Universa Medicina. 2021;40(1):3–13. doi:10.18051/UnivMed.2021.v40.3-13
13. Rosdewi NN, Trisnowati H, Yuningrum H. Risk factors for non-communicable diseases among adolescents in The City Yogyakarta. Int Proc. 2020;2020:666–676.
14. Sudayasa IP, Rahman MF, Eso A, et al. Deteksi Dini Faktor Risiko Penyakit Tidak Menular Pada Masyarakat Desa Andepali Kecamatan Sampara Kabupaten Konawe [Early Detection of Non-Communicable Disease Risk Factors in the Andepali Village Community, Sampara District, Konawe Regency]. J Commun Engage Health. 2020;3(1):60–66. doi:10.30994/jceh.v3i1.37
15. Wekesah FM, Nyanjau L, Kibachio J, et al. Individual and household level factors associated with presence of multiple non-communicable disease risk factors in Kenyan adults. BMC Public Health. 2018;18(S3):1220. doi:10.1186/s12889-018-6055-8
16. Yuningrum H, Trisnowati H, Rosdewi NN. Faktor Risiko Penyakit Tidak Menular (PTM) pada Remaja: Studi Kasus pada SMA Negeri dan Swasta di Kota Yogyakarta [Risk Factors for Non-Communicable Diseases (NCD) in Adolescents: A Case Study in Public and Private Senior High Schools in Yogyakarta]. Jurnal Formil. 2021;6(1):41. doi:10.35842/formil.v6i1.343
17. Umberger WJ, Rupa JA, Zeng D. Understanding food westernisation and other contemporary drivers of adult, adolescent and child nutrition quality in urban Vietnam. Public Health Nutr. 2020;23(14):2571–2583. doi:10.1017/S1368980020001354
18. Ri K. Laporan Nasional RISKESDAS 2018. 2018.
19. Balitbangkes TL. RISKESDAS Tahun 2018 [RISKESDAS 2018]. Kemenkes; 2022. Available from: https://labmandat.litbang.kemkes.go.id/riset-badan-litbangkes/menu-riskesnas/menu-riskesdas/426-rkd-2018.
20. Kemendikbud. UU No. 20 Tahun 2003 Tentang Sistem Pendidikan Nasional [UU no. 20 of 2003 concerning the National Education System]. Indonesia: Kementerian Pendidikan dan Kebudayaan; 2003:1–38.
21. World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour. World Health Organization; 2020.
22. Feng BJ, Jalbout M, Ayoub WB, et al. Dietary risk factors for nasopharyngeal carcinoma in Maghrebian countries. Int J Cancer. 2007;121(7):1550–1555. doi:10.1002/ijc.22813
23. Windi R, Efendi F, Qona’ah A, Adnani QES, Ramadhan K, Almutairi WM. Determinants of acute respiratory infection among children under-five years in Indonesia. J Pediatr Nurs. 2021;60:e54–e59. doi:10.1016/j.pedn.2021.03.010
24. Nainggolan O, Hapsari D, Indrawati L. Pengaruh Akses ke Fasilitas Kesehatan terhadap Kelengkapan Imunisasi Baduta (Analisis Riskesdas 2013) [Effect of Access to Health Facilities on Completeness of Baduta Immunization (Analysis of Riskesdas 2013)]. Media Penelitian Dan Pengembangan Kesehatan. 2016;6(1):15–28. doi:10.22435/mpk.v26i1.4900.15-28
25. Lestari L. Konsumsi Air Kemasan Indonesia [Indonesian Bottled Water Consumption]. Jurnal Litbang Sukowati. 2021;4(2):110–119. doi:10.32630/sukowati.v4i2.210
26. Arifin H, Ibrahim K, Rahayuwati L, et al. HIV-related knowledge, information, and their contribution to stigmatization attitudes among females aged 15–24 years: regional disparities in Indonesia. BMC Public Health. 2022;22(1):637. doi:10.1186/s12889-022-13046-7
27. Weir CB, Jan A. BMI Classification Percentile and Cut off Points. StatPearls Publishing; 2021.
28. Riskesdas. Riset Kesehatan Dasar 2018 [Basic Health Research 2018]. Kementrian Kesehatan Republik Indonesia; 2018:1–100.
29. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296–e296. doi:10.1371/journal.pmed.0040296
30. World Medical Association. World Medical Association declaration of Helsinki. JAMA. 2013;310(20):2191. doi:10.1001/jama.2013.281053
31. Budreviciute A, Damiati S, Sabir DK, et al. Management and prevention strategies for Non-communicable Diseases (NCDs) and their risk factors. Review. Front Public Health. 2020;8. doi:10.3389/fpubh.2020.574111
32. Oshio T, Kan M. Educational level as a predictor of the incidences of non-communicable diseases among middle-aged Japanese: a hazards-model analysis. BMC Public Health. 2019;19(1):852. doi:10.1186/s12889-019-7182-6
33. Sommer I, Griebler U, Mahlknecht P, et al. Socioeconomic inequalities in non-communicable diseases and their risk factors: an overview of systematic reviews. BMC Public Health. 2015;15(1):914. doi:10.1186/s12889-015-2227-y
34. Arena R, Guazzi M, Lianov L, et al. Healthy lifestyle interventions to combat noncommunicable disease—a novel nonhierarchical connectivity model for key stakeholders: a policy statement from the American Heart Association, European Society of Cardiology, European Association for Cardiovascular Prevention and Rehabilitation, and American College of Preventive Medicine. Eur Heart J. 2015;36(31):2097–2109. doi:10.1093/eurheartj/ehv207
35. Irani F, Coquoz E, von Wolff M, Bitterlich N, Stute P. Awareness of non-communicable diseases in women: a cross-sectional study. Arch Gynecol Obstet. 2022;306:801–810. doi:10.1007/s00404-022-06546-9
36. Castillo-Carandang NT, Buenaventura RD, Chia Y-C, et al. Moving towards optimized noncommunicable disease management in the ASEAN region: recommendations from a review and multidisciplinary expert panel. Risk Manag Healthc Policy. 2020;13:803–819. doi:10.2147/RMHP.S256165
37. Hashemi-Aghdam MR, Shafiee G, Ebrahimi M, et al. Trend of passive smoking and associated factors in Iranian children and adolescents: the CASPIAN studies. BMC Public Health. 2022;22(1):603. doi:10.1186/s12889-022-13045-8
38. Kelishadi R, Noori A, Qorbani M, et al. Are active and passive smoking associated with cardiometabolic risk factors in adolescents? The CASPIAN-III study. Paediatr Int Child Health. 2016;36(3):181–188. doi:10.1179/2046905515y.0000000039
39. Wang A, Kubo J, Luo J, et al. Active and passive smoking in relation to lung cancer incidence in the Women’s Health Initiative Observational Study prospective cohort†. Ann Oncol. 2015;26(1):221–230. doi:10.1093/annonc/mdu470
40. Poirier AE, Ruan Y, Grevers X, et al. Estimates of the current and future burden of cancer attributable to active and passive tobacco smoking in Canada. Prev Med. 2019;122:9–19. doi:10.1016/j.ypmed.2019.03.015
41. Pan A, Wang Y, Talaei M, Hu FB, Wu T. Relation of active, passive, and quitting smoking with incident type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015;3(12):958–967. doi:10.1016/S2213-8587(15)00316-2
42. Feng S, Cummings O, McIntire G. Nicotine and cotinine in oral fluid: passive exposure vs active smoking. Pract Lab Med. 2018;12:e00104. doi:10.1016/j.plabm.2018.e00104
43. Walser T, Cui X, Yanagawa J, et al. Smoking and lung cancer: the role of inflammation. Proc Am Thorac Soc. 2008;5(8):811–815. doi:10.1513/pats.200809-100TH
44. Ma Y, Li MD. Establishment of a strong link between smoking and cancer pathogenesis through DNA methylation analysis. Sci Rep. 2017;7(1):1811. doi:10.1038/s41598-017-01856-4
45. Myers J, Kokkinos P, Nyelin E. Physical activity, cardiorespiratory fitness, and the metabolic syndrome. Nutrients. 2019;11(7):1652. doi:10.3390/nu11071652
46. Lee J, Kim Y, Jeon JY. Association between physical activity and the prevalence of metabolic syndrome: from the Korean National Health and Nutrition Examination Survey, 1999–2012. SpringerPlus. 2016;5(1):1870. doi:10.1186/s40064-016-3514-5
47. Park SK, Larson JL. The relationship between physical activity and metabolic syndrome in people with chronic obstructive pulmonary disease. J Cardiovasc Nurs. 2014;29(6):499–507. doi:10.1097/JCN.0000000000000096
48. Sellami M, Bragazzi NL, Slimani M, et al. The effect of exercise on glucoregulatory hormones: a countermeasure to human aging: insights from a comprehensive review of the literature. Int J Environ Res Public Health. 2019;16(10):1709. doi:10.3390/ijerph16101709
49. McGonical K. Five surprising ways exercise changes your brain. The Greater Good Science Center at the University of California. Available from: https://greatergood.berkeley.edu/article/item/five_surprising_ways_exercise_changes_your_brain.
50. Iriti M, Varoni EM, Vitalini S. Healthy diets and modifiable risk factors for non-communicable diseases—the European perspective. Foods. 2020;9(7):940. doi:10.3390/foods9070940
51. Soliman GA. Dietary cholesterol and the lack of evidence in cardiovascular disease. Nutrients. 2018;10(6):780. doi:10.3390/nu10060780
52. Anderson KE, Mongin SJ, Sinha R, et al. Pancreatic cancer risk: associations with meat-derived carcinogen intake in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial (PLCO) cohort. Mol Carcinog. 2012;51(1):128–137. doi:10.1002/mc.20794
53. Chiavarini M, Bertarelli G, Minelli L, Fabiani R. Dietary intake of meat cooking-related mutagens (HCAs) and risk of colorectal adenoma and cancer: a systematic review and meta-analysis. Nutrients. 2017;9(5):514. doi:10.3390/nu9050514
54. Köncke F, Toledo C, Berón C, et al. Estimation of intake of critical nutrients associated with noncommunicable diseases according to the PAHO/WHO criteria in the diet of school-age children in Montevideo, Uruguay. Nutrients. 2022;14(3):528. doi:10.3390/nu14030528
55. Wanjohi MN, Thow AM, Abdool Karim S, et al. Nutrition-related non-communicable disease and sugar-sweetened beverage policies: a landscape analysis in Kenya. Glob Health Action. 2021;14(1):1902659. doi:10.1080/16549716.2021.1902659
56. Chen L, Liu R, Zhao Y, Shi Z. High consumption of soft drinks is associated with an increased risk of fracture: a 7-year follow-up study. Nutrients. 2020;12(2):530. doi:10.3390/nu12020530
57. Dhungana RR, Thapa P, Devkota S, et al. Prevalence of cardiovascular disease risk factors: a community-based cross-sectional study in a peri-urban community of Kathmandu, Nepal. Indian Heart J. 2018;70:S20–S27. doi:10.1016/j.ihj.2018.03.003
58. Ge F, Li Y, Yuan M, Zhang J, Zhang W. Identifying predictors of probable posttraumatic stress disorder in children and adolescents with earthquake exposure: a longitudinal study using a machine learning approach. J Affect Disord. 2020;264:483–493. doi:10.1016/j.jad.2019.11.079
59. Kusnanto K, Rohmah FA, Wahyudi AS, Arifin H. Mental workload and stress with blood glucose level: a correlational study among lecturers who are structural officers at the university. Article. Syst Rev Pharmacy. 2020;11(7):253–257. doi:10.31838/srp.2020.7.40
60. Tumas N, Rodríguez López S, Bilal U, Ortigoza AF, Diez Roux AV. Urban social determinants of non-communicable diseases risk factors in Argentina. Health Place. 2021;102611. doi:10.1016/j.healthplace.2021.102611
61. Ruel MT, Garrett J, Yosef S, Olivier M. Urbanization, food security and nutrition. In: de Pee S, Taren D, Bloem MW, editors. Nutrition and Health in a Developing World. Springer International Publishing; 2017:705–735.
62. Chidya RCG, Singano L, Chitedze I, Mourad KA. Standards compliance and health implications of bottled water in Malawi. Int J Environ Res Public Health. 2019;16(6):951. doi:10.3390/ijerph16060951
63. Kosuth M, Mason SA, Wattenberg EV. Anthropogenic contamination of tap water, beer, and sea salt. PLoS One. 2018;13(4):e0194970. doi:10.1371/journal.pone.0194970
64. Mason SA, Welch VG, Neratko J. Synthetic polymer contamination in bottled water. Original research. Front Chem. 2018;6. doi:10.3389/fchem.2018.00407
65. Anwar N, Kuppili P, Balhara Y. Depression and physical noncommunicable diseases: the need for an integrated approach. Perspective. WHO South-East Asia J Public Health. 2017;6(1):12–17. doi:10.4103/2224-3151.206158
66. Stein DJ, Benjet C, Gureje O, et al. Integrating mental health with other non-communicable diseases. BMJ. 2019;364:l295. doi:10.1136/bmj.l295
67. Thakur J, Prinja S, Garg C, Mendis S, Menabde N. Social and economic implications of noncommunicable diseases in India. Review article. Indian J Commun Med. 2011;36(5):13–22. doi:10.4103/0970-0218.94704
68. Uphoff EP, Newbould L, Walker I, et al. A systematic review and meta-analysis of the prevalence of common mental disorders in people with non-communicable diseases in Bangladesh, India, and Pakistan. J Glob Health. 2019;9(2):020417. doi:10.7189/jogh.09.020417
69. Padhy SK, Sarkar S, Davuluri T, Malhotra N. Depression as a risk factor for cardiac illness – what do we know about? J Indian Coll Cardiol. 2015;5(2):123–130. doi:10.1016/j.jicc.2015.02.004
70. Syed MA, Alnuaimi AS, Zainel AJ, A/Qotba HA. Prevalence of non-communicable diseases by age, gender and nationality in publicly funded primary care settings in Qatar. BMJ Nutr Prev Health. 2019;2(1):20–29. doi:10.1136/bmjnph-2018-000014
71. Doddamani A, Ballala ABK, Madhyastha SP, Kamath A, Kulkarni MM. A cross-sectional study to identify the determinants of non-communicable diseases among fishermen in Southern India. BMC Public Health. 2021;21(1):414. doi:10.1186/s12889-021-10376-w
72. Abebe SM, Andargie G, Shimeka A, et al. The prevalence of non-communicable diseases in northwest Ethiopia: survey of Dabat Health and Demographic Surveillance System. BMJ Open. 2017;7(10):e015496. doi:10.1136/bmjopen-2016-015496
73. World Health Organization. New data from WHO/Europe shows links between gender and noncommunicable diseases. World Health Organization; 2022. Available from: https://www.euro.who.int/en/health-topics/health-determinants/gender/news/news/2020/12/new-data-from-whoeurope-shows-links-between-gender-and-noncommunicable-diseases.
74. Defianna SR, Santosa A, Probandari A, Dewi FST. Gender differences in prevalence and risk factors for hypertension among adult populations: a cross-sectional study in Indonesia. Int J Environ Res Public Health. 2021;18(12):6259. doi:10.3390/ijerph18126259
75. Mridha M, Hasan M, Khan S, Hossain M, Sutradhar I. Women are more vulnerable to non-communicable diseases in rural and urban Bangladesh (P18-082-19). Curr Dev Nutr. 2019;3(Supplement_1). doi:10.1093/cdn/nzz039.P18-082-19
76. Donkor N, Farrell K, Ocho O, et al. Correlates of obesity indices and cardiovascular disease risk factors among Trinidadian nurses. Int J Africa Nurs Sci. 2020;12:100194. doi:10.1016/j.ijans.2020.100194
77. Chiang C-F, Villaverde C, Chang W-C, Fascetti AJ, Larsen JA. Prevalence, risk factors, and disease associations of overweight and obesity in dogs that visited the veterinary medical teaching hospital at the University of California, Davis from January 2006 to December 2015. Top Companion Anim Med. 2022;48:100640. doi:10.1016/j.tcam.2022.100640
78. Sarma PS, Sadanandan R, Thulaseedharan JV, et al. Prevalence of risk factors of non-communicable diseases in Kerala, India: results of a cross-sectional study. BMJ open. 2019;9(11):e027880–e027880. doi:10.1136/bmjopen-2018-027880
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
