Back to Journals » Psoriasis: Targets and Therapy » Volume 13
Analysis of Drug Utilization in Patients with Psoriasis: A Real-World Retrospective Study Among the Italian Population
Authors Perrone V, Losi S, Sabatino S, Mezzetti M, Dovizio M, Sangiorgi D , Degli Esposti L
Received 3 November 2022
Accepted for publication 15 February 2023
Published 2 March 2023 Volume 2023:13 Pages 1—9
DOI https://doi.org/10.2147/PTT.S396003
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Uwe Wollina
Valentina Perrone,1 Serena Losi,2 Silvia Sabatino,2 Maurizio Mezzetti,3 Melania Dovizio,1 Diego Sangiorgi,1 Luca Degli Esposti1
1CliCon S.r.l., Società Benefit-Health Economics and Outcomes Research, Bologna, 40137, Italy; 2Eli Lilly Italy S.p.A, Sesto Fiorentino, Italy; 3Eli Lilly Italy S.p.A, Rome, Italy
Correspondence: Valentina Perrone, CliCon S.r.l., Società Benefit-Health Economics and Outcomes Research, Via Murri 9, Bologna, 40137, Italy, Tel +39 544 38393, Fax +39 544 212699, Email [email protected]
Purpose: An Italian real-world retrospective study was conducted in patients with psoriasis (PSO) to evaluate their characteristics, treatment patterns, and biological/targeted synthetic disease-modifying antirheumatic drug (b/tsDMARD) drug utilization.
Patients and Methods: The retrospective analysis was carried out on real-world data collected from administrative databases of selected Italian health-departments; the dataset covered approximately 22% of the Italian population. PSO patients (identified by PSO hospitalization, and/or active exemption code and/or a topical anti-psoriatic medication prescription) were included. In prevalent patients identified during 2017– 2018-2019-2020, baseline characteristics and treatment patterns were investigated. Moreover, b/tsDMARD drug utilization (focusing on persistence, monthly dosage, and mean duration between prescriptions) was evaluated in bionaïve patients included during 2015 and 2018.
Results: PSO was diagnosed in 241,552 (in 2017), 269,856 (in 2018), 293,905 (in 2019) and 301,639 (in 2020) patients. At the index date, almost 50% of patients had not received systemic medications, and 2% had received biological treatment. Among the b/tsDMARD-treated patients, a decrease in the use of tumour necrosis factor (TNF) inhibitors (60.0– 36.4%, from 2017 to 2020) and an increase in the use of interleukin (IL) inhibitors (36.3– 50.6%, from 2017 to 2020) were observed. In 2018, the persistence rates of TNF inhibitors and IL inhibitors in bionaïve patients ranged from 60.8– 79.7% and 83.3– 87.9%, respectively.
Conclusion: This real-world study of PSO drug utilization in Italy showed that a significant number of patients were not treated with systemic medications and only 2% of patients were treated with biologics. An increase in the use of IL inhibitors and a decrease in the prescription of TNF inhibitors over years were found. Patients treated with biologics were highly persistent with treatment. These data provide insight into routine clinical practice for PSO patients in Italy, suggesting that the optimization of treatment for PSO still represents an unmet medical need.
Keywords: psoriasis systemic medications, psoriasis biological drugs, TNF inhibitors, IL inhibitors, treatment optimization, real world evidence
Introduction
Psoriasis (PSO) is a chronic inflammatory skin disease with a strong genetic predisposition and pathogenic autoimmune mechanisms. The worldwide prevalence is approximately 2% but varies according to region, reaching up to 11% among Caucasian and Scandinavian populations.1 The prevalence of PSO among the Italian population is estimated to vary from 1.8% to 3.1%.2 The dermatologic manifestations of PSO vary; the most prevalent is psoriasis vulgaris, also called plaque-type psoriasis. It is characterized by erythematous, often pruritic plaques covered with silvery scales. While PSO can occur at any age, two peaks of disease onset have been described: the first between 20 and 30 years, and the second between 50 and 60 years, affecting men and women equally.3 Depending on the severity and localization of the psoriatic lesions, patients may suffer from physical and psychological discomfort and significant disability, which negatively affects the patient’s quality of life.4,5
PSO typically affects the skin but may also affect the joints and has been associated with a number of other inflammatory diseases, such as psoriatic arthritis (PsA). Skin manifestations generally precede PsA, which shares the inflammatory chronicity of PSO and requires systemic therapy due to potential destructive progression. PsA develops in up to 40% of PSO patients,6–9 and its incidence increases with time after PSO onset, reaching up to 20% after 30 years.10,11 In addition, PSO patients have an increased incidence of metabolic syndrome manifestations12 and cardiovascular disease (CVD).13 Treatment options available to manage psoriatic disease include topical therapy, phototherapy, oral treatment, and biologic therapy.14 The choice of treatment is largely based on disease severity, the presence of comorbid conditions, such as PsA, and patients’ treatment history.15
The Italian guidelines for the treatment of plaque PSO state that topical therapy (ie, corticosteroids, vitamin D3 analogues) alone is indicated in mild PSO. While in patients with moderate-to-severe PSO, topical agents remain useful when combined with systemic treatments.16 Systemic therapy available for PSO comprises phototherapy, conventional treatments (ie, cyclosporine, methotrexate, acitretin), and biological (b)/synthetic target(ts) disease-modifying antirheumatic drugs [DMARDs, such as tumor necrosis factor (TNF)-A blockers, interleukin (IL) inhibitors and phosphodiesterase 4 (PDE)-inhibitors].16 Biologics represent established and efficacious treatments in patients for whom traditional systemic therapies failed to achieve an adequate response, were not tolerated owing to adverse effects, or were unsuitable owing to comorbidities.14
According to Italian PSO guidelines, no single sequence in which biologics should be initiated or switched has been suggested.16 The choice of therapy depends on the characteristics of the disease (eg, severity, location, PsA manifestation), patient-related features and the characteristics of the treatments.16 Moreover, despite standard approved dosing regimens of biologic agents have been established, in real-world setting of PSO management, alternative dosing regimens have been frequently observed.17–19
Moreover, it has been reported that despite several therapeutic options and the high number of patients experiencing biologics, some of them could manifest multiple therapeutic failure of the management of multi-resistant patients represent an important challenge for the clinician.20,21
Despite several therapeutic options, PSO remains an underdiagnosed and undertreated disease;22 thus, a better understanding of the disease and the available treatment options would help to optimize the therapeutic management of PSO patients.
In this study, a retrospective analysis of administrative datasets of PSO patients was carried out to evaluate patient characteristics and treatment patterns of b/tsDMARD, across the most recent years. Moreover, b/tsDMARD drug use (in terms of treatment persistence and dosage regimen) was evaluated, in a real-world Italian setting.
Methods
Data Source
A retrospective observational study based on data extracted from the administrative databases of geographically distributed Italian health departments, covering approximately 22% of the Italian population, was carried out. Within the administrative flows, an anonymous univocal numeric code was assigned to each patient to electronically link all subjects’ records across databases. Administrative databases among the Italian National Health System (NHS) contain data for the health-care services reimbursement purpose, and include data on drug prescriptions, hospitalizations and outpatient specialist visits/diagnostic tests. For the current study, Italian Entities database was selected by their geographical distribution across Italy, by data completeness, and by the high-quality linked datasets. Specifically, data from the following databases were extracted (S1 Methods): i) demographic database, ii) the pharmaceutical database, iii) the hospitalization database, iv) the diagnostic test and specialist visit database, and v) the payment exemption database. The anonymous univocal numeric code guaranteed total compliance with the European General Data Protection Regulation (GDPR) (2016/679). The integration of administrative datasets enables to represent the patient’s entire clinical history and not just individual prescriptions. The analyses were conducted using exclusively anonymized data in full compliance with privacy regulations. The results were exclusively in aggregated form which cannot be attributed to a single institution, department, doctor, individual, or individual prescribing behaviour. The analysis was conducted in full compliance with current legislation for retrospective studies. Based on the Data Privacy Guarantor Authority (General Authorization for personal data treatment for scientific research purposes – n.9/2014), informed consent was not required, as its collection would be impossible for organizational reasons. According to Italian law on observational studies, the ethics committee of each participating entity was notified and approved the analysis (Table S1).
Identification of PSO Patients: Baseline Characteristics and Treatment Pattern
Among 2017–2018-2019 and 2020, PSO patients were identified by the presence of i) at least one hospitalization with a primary or secondary discharge diagnosis of PSO (ICD-9-CM code 696.1) and/or ii) at least one active PSO exemption code (code 045.696.1), and/or iii) at least a prescription of a topical antipsoriatic drug (ATC code: D05A) (diagnosis by proxy). The distribution of patients across the years was not mutually exclusive, and in each calendar year prevalent patients with PSO diagnosis was analysed. The index-date was defined as the date of the first fulfilment of the inclusion criteria for each calendar year.
Baseline demographic characteristics (age and sex) were evaluated at the index-date, while the presence of clinical manifestations related to PSO and comorbidities21,22 were assessed considering all available periods before the index-date (details are reported in the Supplementary Material).
Treatment pattern was evaluated during the first year of follow-up, and by considering the presence of at least one prescription among medications indicated for PSO: b/tsDMARDs [TNF inhibitors (adalimumab, etanercept, infliximab); IL inhibitors, IL-12/-23 inhibitor (ustekinumab), IL-23 inhibitors (risankizumab, tildrakizumab, guselkumab), IL-17 inhibitors (brodalumab, ixekizumab, secukinumab); phosphodiesterase-4 (PDE)-inhibitor (apremilast)], nonsteroidal anti-inflammatory drugs (NSAIDs), and conventional therapies [cyclosporine, methotrexate, acitretin, and dimethyl fumarate] (Supplementary Material). Patients were defined untreated if they were not prescribed with any of the above reported systemic medications during the first year of follow-up. Based on the presence or absence of b/tsDMARD prescriptions during the total period before the index date, patients were defined as bioexperienced or bionaïve, respectively.
Drug Utilization Analysis in b/tsDMARD-Treated Patients
Drug utilization analysis in b/tsDMARD-treated patients was carried out by evaluating treatment persistence and the mean monthly dosage in bionaïve patients who received initial first-line b/tsDMARD treatment during 2015 or during 2018, to report a snapshot in b/tsDMARD use one-year before and one-year after the introduction of the most recent drug class in 2017, ie, anti IL-17. For drug utilization analysis, the index-date was the date of the first b/tsDMARD prescription across 2015 or 2018. Treatment persistence was defined as the percentage of patients prescribed with the index-medication during the last quarter of the one-year follow-up. During the treatment maintenance phase, over 12-months follow-up, the mean monthly dosage prescribed and the spacing (in weeks) between prescriptions were estimated.
Statistical Analysis
All analyses were descriptive. Continuous variables are reported as the mean ± standard deviation (SD); categorical variables are expressed as numbers and percentages. In all the analyses, the unit of analysis was the patient. Following the “Opinion 05/2014 on Anonymization Techniques” drafted by the “European Commission Article 29 Working Party”, the results of analyses involving fewer than 3 patients were not reported, as they potentially may be traceable to single individuals. Therefore, the results referring to ≤3 patients were reported as NI (not issuable). All analyses were performed using STATA SE version 17.0 (StataCorp LLC, College Station, TX, USA).
Results
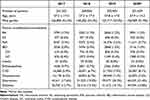
Across the study period, 241,552 (in 2017, 52.2% male), 269,856 (in 2018, 52.0% male), 293,905 (in 2019, 52.0% male) and 301,639 (in 2020, 51.9% male) PSO patients were identified (Table 1). The enrolled PSO population was a predominantly adult population (with a quote of non-adult patients ranging 0.03–0.04%) with average age of 57.0±17.0 years (in 2017), 57.3±17.0 years (in 2018), 57.8 ± 17.0 years (in 2019), and 57.9 ± 14.3 years (in 2020). The most frequent comorbid conditions related to PSO, identified by disease-related hospitalizations or exemption codes, are reported in Table 1.
The evaluation of treatment patterns during the first year of follow-up (index date included) revealed that across the study period, 47.8% (N = 115,397 in 2017) to 56.8% (N = 68,336 in 2020) of PSO patients did not receive systemic medications (untreated patients), 50.3% (N = 121,459, in 2017) to 41.0% (49,398, in 2020) received conventional therapies, while, 1.9% (N = 4696, in 2017) to 2.2% (2629, in 2020) of PSO patients received at least one prescription of b/tsDMARDs (Figure 1). Among b/tsDMARD users, 33.2–44.9% received monotherapy (Table S2), 15.5–14.7% received b/tsDMARDs plus topical agents, 19.3–17.8% received b/tsDMARDs plus NSAIDs, and 5.9–5.2% received cotreatment with b/tsDMARDs and other systemic conventional treatments (Table S2). Although NSAID use is not recommended for the treatment of PSO, it can be prescribed to patients with concomitant PsA,18 in fact it has been recently reported that almost 20% of naïve biologic-treated PSO patients had a concomitant PsA diagnosis.11
AAmong all PSO patients from 2017 to 2020, a decreasing tendency in TNF inhibitors (60.0–36.4%) and an increase in IL inhibitors (36.3–50.6%) and tsDMARD use (3.7–13.0%) were observed (Figure 2A). A comparable trend was found among bioexperienced patients, with 65.1% (in 2017) and 36.5% (in 2020) of patients prescribed TNF inhibitors and 33.9% (in 2017) and 52.2% (in 2020) of PSO patients prescribed IL inhibitors. The proportion of patients prescribed tsDMARD accounted for an average 1.0% in 2017 up to 11.3% in 2020 (Figure 2B). In bionaïve patients, the use of TNF inhibitors and IL inhibitors ranged from 42.2% (in 2017) to 35.9% (in 2020) and from 44.8% (in 2017) to 36.0% (in 2020), respectively. Moreover, a tendency toward an increase in tsDMARD prescriptions was found, from 12.9% in 2017 to 28.5% in 2020 (Figure 2C). In Table 2, the stratification of b/tsDMARD-treated patients based on the molecule prescribed at the index date is reported. Across the study period, 28.0% (in 2017) – 19.9% (in 2020) of patients were prescribed adalimumab; 26.5–15.3% of patients were prescribed etanercept; 21.9–18.8% were prescribed ustekinumab, 13.8–18.6% were prescribed secukinumab, 3.7–13.0% were prescribed apremilast, 5.4–1.2% were prescribed infliximab, and 0.6–8.1% were prescribed ixekizumab (Table 2).
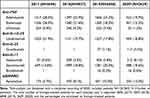 |
Table 2 Stratification of PSO Patients Based on the Type of b/tsDMARD Prescribed at Inclusion. Data are Given as Numbers and Percentages in Brackets |
Two time-frame snapshots of drug utilization in b/tsDMARD-treated patients were performed by considering bionaïve PSO patients during 2015 and 2018. As reported in Table 3, in 2015, 76.4–82.2% of patients were persistent to TNF inhibitors, and 83.3% of patients were persistent to IL-12/-23 inhibitors treatment. During 2018, the persistence rates of those using TNF inhibitors ranged from 60.8% to 79.7% and that for IL-17 inhibitors ranged from 86.3% to 87.9%; in addition, the IL-12/-23 inhibitor persistence rate was 83.3%, and 64.3% of PSO patients persistently used tsDMARDs (Table 3). In Table 4, the monthly dosages and the durations between prescriptions are reported in weeks. In patients included during 2015, the prescribed monthly dosages for TNF inhibitors and IL-12/-23 inhibitors were comparable to the label recommendations. The same pattern between the monthly dosage prescribed and the recommendations was found in patients included during 2018 (Table 4). During 2015 and 2018, dosage increases were not observed, except for ustekinumab (45 mg), with 7% and 7.9% increases, respectively (not shown). The durations between prescriptions in 2015 and 2018 averaged 8.3 and 8.0 weeks for adalimumab, 8.1 and 6.8 weeks for etanercept, 7.6 and 5.6 weeks for infliximab, 12.6 and 11.5 weeks for ustekinumab, respectively; the durations in only 2018 were 8.7 weeks for ixekizumab and 7.3 weeks for secukinumab (Table 4).
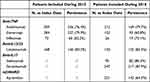 |
Table 3 Treatment Persistence During the First Year of Follow-Up in Bionaïve PSO Patients Included During 2015 and 2018. Persistent Patients are Reported as Numbers and Percentages in Brackets |
Discussion
This study reported Italian real-world data on PSO in terms of patient characteristics, treatment patterns across the most recent years, and drug utilization of biological medications considering two time periods, 2015 and 2018, to better discriminate biological use data based on the marketing access of anti-IL-17 biological class, which represent, one of the most recent class introduced.
Across 2017–2020, baseline characteristics of the enrolled PSO population were comparable to those reported in real-world studies and surveys among Italian PSO patients.23–25 In our research, less than 4% of PSO patients had a concomitant diagnosis of PsA. The prevalence rates of PsA in PSO patients range from 6% to 41%,6–9 and its incidence increases with time after PSO onset, reaching up to 20% after 30 years.10,11 In a recent noninterventional, retrospective analysis in the German population, the cumulative percentage of patients with existing PSO who developed concomitant PsA during the four-year study period was 3.44%.23 In addition, approximately 15% of PSO patients are thought to have undiagnosed PsA.24 Moreover, since multiple immune-mediated comorbidities have been associated with psoriasis26 their frequency was evaluated in PSO patients at baseline: almost 1.2% of rheumatoid arthritis (RA), 0.2% of ankylosing spondylitis (AS), 1% of inflammatory bowel disease (IBD) diagnoses were identified among the included patients.
Across 2017–2020, the analysis of treatment pattern showed that almost 50% of PSO patients had not received systemic medications (conventional treatments/biologicals), during the first year of follow-up. In accordance with our findings, a recent retrospective study among the Italian population found that in PSO patients who received prescription therapy, almost 40% received non-DMARDs.25 Data from a Belgian cross-sectional study confirmed that undertreatment represents a challenge in PSO management; the results showed that almost 40% of patients with moderate-to-severe PSO were not treated with any systemic therapy (or with any therapy at all, including topical drugs) despite the disease severity.27
Biologics were used by 2% of the entire PSO population, with more than half of the patients receiving TNF inhibitors, less than half prescribed IL inhibitors, and up to 13% prescribed tsDMARDs. Across the study period, 2017–2020, TNF inhibitor use decreased, while the use of IL inhibitors, especially in bioexperienced patients, increased. This tendency could, among other factors, be attributable to a shift in the treatment goal paradigm in PSO, as stated in the Italian guidelines,16 with the ultimate goal of achieving complete or almost complete PSO clearance; evidence from head-to-head trials and metanalyses have shown that this therapeutic goal is more easily achievable with IL inhibitors.28–31
In the drug utilization analysis, in bio-naïve patients included during 2018, a high rate of treatment persistence for TNF inhibitors, IL-12/-23 inhibitor and IL-17 inhibitors was found, with the persistence rate to IL inhibitors being more than 80%; moreover, the monthly dosage regimens were commensurate with the label recommendations. These results regarding biologic treatment persistence, despite being derived from a small sample of patients, are in line with those of previous national and international observational reports, which have shown a trend of higher persistence rate in patients under IL-17 inhibitors or IL-12/23 inhibitors.32–35 The high persistence rate among PSO patients treated with biologics, in addition to improving clinical patients’ conditions, could translate into a lower economic burden on these patients.36 The response to biologics could be impacted by the previous exposure to the drug: in fact bio-naïve PSO patients, respect to bio-experienced, could be characterized by a higher and shorter clinical response to biologics.21,37
The limitations of the present study are related to its retrospective observational nature and the use of anonymized data derived from administrative databases. Regional/local health unit administrative databases progressively improve the quality of collected data. Nevertheless, some information may be missing; if the necessary information was missing for a given patient, that patient was excluded from the analysis. Other limitations are related to the fact that primary care data were not collected and there was a lack or limited clinical information on comorbidities, the disease severity and duration, and other potential confounders that could have influenced the present results. Since the comorbidities analyzed were addressed based on proxy of diagnosis, there might be incomplete capture or over/under estimation of these variables among patients. Data on pharmacological treatments were captured from medical prescription and dispensing information; thus, the reason for non-persistence was not retrievable from the dataset. The use of some medications such as NSAID could account by the out-of-pocket procedure, thus being not retrievable from the dataset. Therefore, limitations are related to the small sample size of some patient subgroups and to the partial data availability for 2020. In the present analysis, a non-canonical classification of PSO-related medications was approached, but since the main objective was to investigate the use of biologics among PSO patients and that the main results were reported as descriptive analyses among patients stratified per single molecule, the subgrouping does not have an impact on the main results of the present manuscript.
Conclusion
This real-world study outlined some of the clinical practices for PSO in Italy. Almost one-half of patients were not treated with systemic medications among the study periods, and a quote of 2% were under biologics, which may encompass moderate-to-severe PSO patients. Over the study period, the use of IL inhibitors increased, while the use of TNF inhibitors decreased. In addition, a trend of IL inhibitors higher persistence rate in bionaïve PSO patients across the years was observed. These results suggest that the management of PSO remains an unmet medical need and that treatment optimization in routine clinical practice should be addressed.
Acknowledgments
Eli Lilly purchased the study report, which is the basis for this manuscript. This manuscript was developed with Eli Lilly and CliCon S.r.l. Società Benefit. The agreement signed by CliCon S.r.l. Società Benefit and Eli Lilly & Company does not create any entity-ship, joint venture or any similar relationship between the parties. CliCon S.r.l. Società Benefit is an independent company. Neither CliCon S.r.l.- Società Benefit nor any of their representatives are employees of Eli Lilly & Company for any purpose.
Disclosure
VP, MD, DS, and LDE are affiliated with CliCon S.r.l. Società Benfit. SL, SS and MM are employees of Eli Lilly S.p.A Italy. SL is a stockholder of Eli Lilly S.p.A Italy. The authors report no other conflicts of interest in this work.
References
1. Rendon A, Schäkel K. Psoriasis pathogenesis and treatment. Int J Mol Sci. 2019;20(6):1475. doi:10.3390/ijms20061475
2. Prignano F, Rogai V, Cavallucci E, Bitossi A, Hammen V, Cantini F. Epidemiology of psoriasis and psoriatic arthritis in Italy-a systematic review. Curr Rheumatol Rep. 2018;20(7):43. doi:10.1007/s11926-018-0753-1
3. Armstrong AW. Psoriasis. JAMA Dermatol. 2017;153(9):956. doi:10.1001/jamadermatol.2017.2103
4. Mease PJ, Menter MA. Quality-of-life issues in psoriasis and psoriatic arthritis: outcome measures and therapies from a dermatological perspective. J Am Acad Dermatol. 2006;54(4):685–704. doi:10.1016/j.jaad.2005.10.008
5. Mukhtar R, Choi J, Koo JY. Quality-of-life issues in psoriasis. Dermatol Clin. 2004;22(4):389–viii. doi:10.1016/j.det.2004.03.016
6. Ogdie A, Langan S, Love T, et al. Prevalence and treatment patterns of psoriatic arthritis in the UK. Rheumatology. 2013;52(3):568–575. doi:10.1093/rheumatology/kes324
7. Li R, Sun J, Ren LM, et al. Epidemiology of eight common rheumatic diseases in China: a large-scale cross-sectional survey in Beijing. Rheumatology. 2012;51(4):721–729. doi:10.1093/rheumatology/ker370
8. Carneiro JN, Paula AP, Martins GA. Psoriatic arthritis in patients with psoriasis: evaluation of clinical and epidemiological features in 133 patients followed at the University Hospital of Brasília. An Bras Dermatol. 2012;87(4):539–544. doi:10.1590/s0365-05962012000400003
9. Haroon M, Kirby B, FitzGerald O. High prevalence of psoriatic arthritis in patients with severe psoriasis with suboptimal performance of screening questionnaires. Ann Rheum Dis. 2013;72(5):736–740. doi:10.1136/annrheumdis-2012-201706
10. Zabotti A, Tinazzi I, Aydin SZ, McGonagle D. From psoriasis to psoriatic arthritis: insights from imaging on the transition to psoriatic arthritis and implications for arthritis prevention. Curr Rheumatol Rep. 2020;22(6):24. doi:10.1007/s11926-020-00891-x
11. Seneschal J, Lacour JP, Bewley A, et al. A multinational, prospective, observational study to estimate complete skin clearance in patients with moderate-to-severe plaque PSOriasis treated with BIOlogics in a REAL world setting (PSO-BIO-REAL). J Eur Acad Dermatol Venereol. 2020;34(11):2566–2573. doi:10.1111/jdv.16568
12. Sommer DM, Jenisch S, Suchan M, Christophers E, Weichenthal M. Increased prevalence of the metabolic syndrome in patients with moderate to severe psoriasis. Arch Dermatol Res. 2006;298(7):321–328. doi:10.1007/s00403-006-0703-z
13. Prodanovich S, Kirsner RS, Kravetz JD, Ma F, Martinez L, Federman DG. Association of psoriasis with coronary artery, cerebrovascular, and peripheral vascular diseases and mortality. Arch Dermatol. 2009;145(6):700–703. doi:10.1001/archdermatol.2009.94
14. Menter A, Strober BE, Kaplan DH, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol. 2019;80(4):1029–1072. doi:10.1016/j.jaad.2018.11.057
15. Martin G, Young M, Aldredge L. Recommendations for initiating systemic therapy in patients with psoriasis. J Clin Aesthet Dermatol. 2019;12(4):13–26.
16. Gisondi P, Altomare G, Ayala F, et al. Italian guidelines on the systemic treatments of moderate-to-severe plaque psoriasis. J Eur Acad Dermatol Venereol. 2017;31(5):774–790. doi:10.1111/jdv.14114
17. Carrascosa JM, Garcia-Doval I, Pérez-Zafrilla B, et al. Use of off-label doses is frequent in biologic therapy for moderate to severe psoriasis: a cross-sectional study in clinical practice. J Dermatolog Treat. 2015;26(6):502–506. doi:10.3109/09546634.2015.1034070
18. Iskandar IYK, Ashcroft DM, Warren RB, et al. Patterns of biologic therapy use in the management of psoriasis: cohort study from the British Association of Dermatologists Biologic Interventions Register (BADBIR). Br J Dermatol. 2017;176(5):1297–1307. doi:10.1111/bjd.15027
19. Esposito M, Gisondi P, Conti A, et al. Dose adjustment of biologic therapies for psoriasis in dermatological practice: a retrospective study. J Eur Acad Dermatol Venereol. 2017;31(5):863–869. doi:10.1111/jdv.14145
20. Mastorino L, Roccuzzo G, Dapavo P, et al. Patients with psoriasis resistant to multiple biological therapies: characteristics and definition of a difficult-to-treat population. Br J Dermatol. 2022;187(2):263–265. doi:10.1111/bjd.21048
21. Cariti C, Dapavo P, Mastorino L, et al. Comparison of Secukinumab and Ixekizumab in psoriasis: a real-life cohort study on the efficacy and drug survival of 445 patients. J Eur Acad Dermatol Venereol. 2022;36(3):e233–e235. doi:10.1111/jdv.17766
22. Wu JJ. Contemporary management of moderate to severe plaque psoriasis. Am J Manag Care. 2017;23(21 Suppl):S403–S416.
23. Reich K, Krüger K, Mössner R, Augustin M. Epidemiology and clinical pattern of psoriatic arthritis in Germany: a prospective interdisciplinary epidemiological study of 1511 patients with plaque-type psoriasis. Br J Dermatol. 2009;160(5):1040–1047. doi:10.1111/j.1365-2133.2008.09023.x
24. Villani AP, Rouzaud M, Sevrain M, et al. Prevalence of undiagnosed psoriatic arthritis among psoriasis patients: systematic review and meta-analysis. J Am Acad Dermatol. 2015;73(2):242–248. doi:10.1016/j.jaad.2015.05.001
25. Ingrasciotta Y, Isgrò V, Ientile V, Tari M, Trifirò G, Guarneri C. Are patients with psoriasis and psoriatic arthritis undertreated? A population-based study from Southern Italy. J Clin Med. 2021;10(15):3431. doi:10.3390/jcm10153431
26. Vanaclocha F, Crespo-Erchiga V, Jiménez-Puya R, et al. Immune-mediated inflammatory diseases and other comorbidities in patients with psoriasis: baseline characteristics of patients in the AQUILES study. Actas Dermosifiliogr. 2015;106(1):35–43. doi:10.1016/j.ad.2014.06.003
27. Lambert J, Ghislain PD, Lambert J, Cauwe B, Van den Enden M. Treatment patterns in moderate-to-severe plaque psoriasis: results from a Belgian cross-sectional study (DISCOVER). J Dermatolog Treat. 2017;28(5):394–400. doi:10.1080/09546634.2016.1255304
28. Reich K, Pinter A, Lacour JP, et al. Comparison of ixekizumab with ustekinumab in moderate-to-severe psoriasis: 24-week results from IXORA-S, a Phase III study. Br J Dermatol. 2017;177(4):1014–1023. doi:10.1111/bjd.15666
29. Griffiths CE, Reich K, Lebwohl M, et al. Comparison of ixekizumab with etanercept or placebo in moderate-to-severe psoriasis (UNCOVER-2 and UNCOVER-3): results from two Phase 3 randomised trials. Lancet. 2015;386(9993):541–551. doi:10.1016/S0140-6736(15
30. Thaçi D, Blauvelt A, Reich K, et al. Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate to severe plaque psoriasis: CLEAR, a randomized controlled trial. J Am Acad Dermatol. 2015;73(3):400–409. doi:10.1016/j.jaad.2015.05.013
31. Langley RG, Elewski BE, Lebwohl M, et al. Secukinumab in plaque psoriasis--results of two phase 3 trials. N Engl J Med. 2014;371(4):326–338. doi:10.1056/NEJMoa1314258
32. Zagni E, Colombo D, Fiocchi M, et al. Pharmaco-utilization of biologic drugs in patients affected by psoriasis, psoriatic arthritis and ankylosing spondylitis in an Italian real-world setting. Expert Rev Pharmacoecon Outcomes Res. 2020;20(5):491–497. doi:10.1080/14737167.2020.1800456
33. Lockshin B, Cronin A, Harrison RW, et al. Drug survival of ixekizumab, TNF inhibitors, and other IL-17 inhibitors in real-world patients with psoriasis: the corrona psoriasis registry. Dermatol Ther. 2021;34(2):e14808. doi:10.1111/dth.14808
34. Schmitt-Egenolf M, Freilich J, Stelmaszuk-Zadykowicz NM, Apol E, Hansen JB, Levin LÅ. Drug persistence of biologic treatments in psoriasis: a Swedish national population study. Dermatol Ther. 2021;11(6):2107–2121. doi:10.1007/s13555-021-00616-7
35. Sewerin P, Borchert K, Meise D, Schneider M, Mahlich J. Real-world treatment persistence with biologic disease-modifying antirheumatic drugs among German patients with psoriatic arthritis-A retrospective database study. Rheumatol Ther. 2021;8(1):483–497. doi:10.1007/s40744-021-00286-z
36. Lee S, Xie L, Wang Y, Vaidya N, Baser O. Evaluating the effect of treatment persistence on the economic burden of moderate to severe psoriasis and/or psoriatic arthritis patients in the U.S. Department of defense population. J Manag Care Spec Pharm. 2018;24(7):654–663. doi:10.18553/jmcp.2018.24.7.654
37. Mastorino L, Castelli F, Stroppiana E, et al. Risankizumab shows faster response in bio naïve than in bio-experienced psoriatic patients. J Eur Acad Dermatol Venereol. 2022;36(10):e838–e841. doi:10.1111/jdv.18314
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.