Back to Journals » Infection and Drug Resistance » Volume 14
Analysis of Bacterial Biofilm Formation in Patients with Malignancy Undergoing Double J Stent Indwelling and Its Influencing Factors
Authors Zeng K, Zhang JM, Li XB, Peng SX, Zhang SC, Xie WX, Xi CF, Cao CJ
Received 9 August 2021
Accepted for publication 3 November 2021
Published 7 December 2021 Volume 2021:14 Pages 5209—5217
DOI https://doi.org/10.2147/IDR.S333421
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Ke Zeng,1,* Jia-Mo Zhang,2,* Xiao-Bin Li,1 Sheng-Xian Peng,3 Su-Chuan Zhang,4 Wen-Xian Xie,5 Chun-Fang Xi,1 Cheng-Jian Cao6
1Department of Urology, First People’s Hospital of Zigong City, Zigong, People’s Republic of China; 2Department of Urology, YongChuan Hospital Chongqing Medical University, Chongqing, People’s Republic of China; 3Scientific Research Department, First People’s Hospital of Zigong City, Zigong, People’s Republic of China; 4Laboratory Department, First People’s Hospital of Zigong City, Zigong, People’s Republic of China; 5Department of Basic Medicine, Sichuan Vocational College of Health and Rehabilitation, Zigong, People’s Republic of China; 6Zigong Academy of Medical Sciences, First People’s Hospital of Zigong City, Zigong, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Cheng-Jian Cao
Zigong Academy of Medical Sciences, First People’s Hospital of Zigong City, Zigong, People’s Republic of China
Email [email protected]
Objective: To analyze the bacterial biofilm (BF) formation in patients with malignancy undergoing double J stent indwelling and its influencing factors.
Methods: A total of 167 patients with malignant tumors who received double J stent indwelling in the hospital from January 2018 to January 2021 were included in the study. The urine and double J stent samples were collected for bacterial identification and observed for BF formation on the surface of the urinary catheter under a scanning electron microscope (SEM). Univariate and multivariate logistic regression analyses were used to analyze the influencing factors of BF.
Results: The BF formation rate was 34.73% (58/167). The BF formation rate of positive specimens cultured in urine and double J stent was significantly higher than that of negative ones (P< 0.05). Staphylococcus was the main BF bacteria in double J stent and urine culture specimens, followed by Enterococcus, Pseudomonas, Enterobacter, and Acinetobacter. Compared with the non-BF group, the number of viable bacteria in the double J stent and urine and the catheterization time in the BF group rose markedly (P< 0.05). Advanced age, chemotherapy, anemia, indwelling time ≥ 90d, and urinary tract infection were risk factors for BF formation in patients with malignancy undergoing double J stent indwelling (P< 0.05).
Conclusion: There is a high rate of BF formation in patients with malignancy undergoing double J stent indwelling, with Staphylococcus as the dominant species. Treatment requires enhanced urinary catheter management and nutritional status to inhibit BF formation and lower the rate of urinary catheter-related infections.
Keywords: malignant tumor, double J stent indwelling, biofilm, catheter-related infection, etiology, influence factor
Introduction
Double J ureteral stent, frequently used for indwelling ureter, can effectively relieve ureteral obstruction and prevent ureteral stenosis.1 Consequently, preoperative or intraoperative indwelling double J stent is a common measure to prevent ureteral injury2 as well as postoperative upper urinary tract obstruction due to surgery or metastasis of tumor in patients with malignant tumors, especially gynecological and urinary malignant tumors.3 However, its therapeutic effect is undermined by complications, such as urinary tract infection and urinary sepsis in severe cases, which threatens the life and health of patients.4 It has been confirmed by relevant research that bacteria biofilm (BF) formation, membrane-like substances formed by bacteria adhering to the surface, can enable bacteria to develop drug resistance against antimicrobial agents.5 As a result, it is considered that the formation of BF may be a key contributory factor to the relapse and intractability of urinary tract infections.6 Therefore, the analysis of BF formation in patients with malignancy undergoing double J stent indwelling and the exploration of factors affecting urinary tract infection in patients are of great significance for clinical treatment. The results are reported as follows.
Data and Methods
Clinical Data
A total of 167 patients with malignant tumors who received double J stent indwelling in the hospital from January 2018 to January 2021 were included in the study. Inclusion criteria: ① 18–80 years old; ② malignant tumors confirmed by pathology; ③ the double J stent was indwelling for the first time, with the indwelling time no less than 30 d; ④ COOK(UFH-626, USI-626-CE-B) double J stent was used; ⑤Estimated survival time ≥6 months. Exclusion criteria: ①urinary tract infection existed before the double J stent indwelling; ②double J stent indwelling contradiction; ③ failure in double J stent indwelling; ④Infection occurred due to other reasons after operation; ⑤ urological tumors such as epithelial tumors of the upper urinary tract. The study was approved by the Hospital Ethics Committee of First people’s hospital of Zigong city and the patients signed an informed consent form. The study was in accordance with the Helsinki Declaration as revised in 2013 for experiments involving humans.
Methods
General Information Collection
General information, including the patients’ age, gender, height, weight, highest educational level, hypertension, diabetes mellitus, hormone therapy, chemotherapy, radiotherapy, tumor clinical stage, tumor type, anemia, double J stent indwelling time, the presence of urinary tract infection, and the type of urinary tract infection was recorded. Body Mass Index (BMI)= Weight (kg) divided by the square of Height (m).
Specimen Collection
After routine disinfection, draping, and local anesthesia, 3 mL of urine was collected by a disposable sterile syringe by urethral catheterization, and the double J stent was removed under a cystoscopy or ureteroscopy. The bladder pelvis segment was divided into two segments for observation, each about 3 cm long. One segment was observed under Scanning Electron Microscope (SEM) on the BF morphology on the surface of the double J stent. The other section of the double J tube was placed in the inoculation bottle, added with 30 mL of physiological saline, and eluted by the vortex shaker at 3000 R/min for 1 minute. Subsequently, the precipitate was inoculated into blood agar plate medium and MacConkey agar medium, and placed in a constant temperature incubator at 37°C for 16 to 24 hours. The formation of sterile colonies was observed, and the bacterial species and drug sensitivity were identified.
Observation on BF Morphology on Double J Stent Surface and Counting of Viable Bacteria Colony
In the groups of 30–60 days, 61–90 days, 91–120 days, 121–150 days, and more than 150 days, 5 specimens of double J stent were selected from each group by random number table method. The double J stent was rinsed with PBS solution three times, 10 min each. The samples were fixed with osmic acid for 1 h and rinsed with PBS solution three times, 10 min each. The dehydration was carried out in gradient with 30%, 50%, 70%, 80%, 90%, and 100% trimethyl methanol, respectively, and repeated for three times. After drying with a high-vacuum coating apparatus for 20–30 min, the specimens of double J stent were scanned by a SEM (S3000N, Hitachi, Japan) after gold spraying, and six fields of 100 μm were randomly selected for each specimen. The formation of BF on the surface of the double J stent was observed and photographed, and the viable bacterial colonies were counted. It is defined as BF if meeting the following morphological characteristics: water channel, three-dimensional structure, spherical or elliptical corpuscle coated with matrix.
Viable Bacteria Counting and Bacterial Identification
1 mL each of clean urine and double J stent rinsing fluid were collected, and viable bacteria counts were analyzed with a UF-1000i automatic urine analyzer from SYSMEX. Urine specimens and double J stent specimens were inoculated on blood agar plates (Zhengzhou Antu Company). All the specimens were identified in accordance with the national clinical inspection operating procedures. Vitek 2 compact automatic bacteria identification drug susceptibility instrument (Mérieux Company, France) was used to identify the bacteria, and the reagents were the matching GN, GP identification cards and GN13, GP67 drug susceptibility cards.7
Diagnosis Criteria8
The occurrence of urinary infection within 48 h after indwelling or removal of double J stent was considered as urinary infection associated with double J stent. Urinary infection was diagnosed with urine bacterial culture containing Gram-positive cocci ≥104CFU/mL and Gram-negative bacilli ≥105CFU/mL.
Statistical Methods
SPSS20.0 software was used for statistical analysis. Measurement data conforming to normal distribution were expressed as ( ±s). Independent sample t-test was used for comparison between groups, paired sample t-test for intra-group comparison, one-way analysis of variance for comparison among groups, and Sink-q test for pairwise comparison. The enumeration data were expressed by frequency or ratio and analyzed using the Karman non-correction method, with the total cases no less than 40 and the minimum theoretical frequency over 5. Logistic regression was used to analyze the risk factors. P < 0.05 indicated that the difference was statistically significant.
±s). Independent sample t-test was used for comparison between groups, paired sample t-test for intra-group comparison, one-way analysis of variance for comparison among groups, and Sink-q test for pairwise comparison. The enumeration data were expressed by frequency or ratio and analyzed using the Karman non-correction method, with the total cases no less than 40 and the minimum theoretical frequency over 5. Logistic regression was used to analyze the risk factors. P < 0.05 indicated that the difference was statistically significant.
Results
General Information About Double J Stent Indwelling Patients with Malignant Tumors
Patients’ general information is presented in Table 1.
 |
Table 1 General Data of Malignant Tumor Patients with Indwelling Double J Stent (n=167) |
Formation of BF of Urine and Double J Stent Specimens
The BF formation rate in 167 malignant tumor patients with double J stent indwelling was 34.73% (58/167). Positive specimens cultured in urine and double J stent showed a remarkably higher formation rate of BF than those negative specimens (P < 0.05). See Table 2.
 |
Table 2 Formation of Urinary Stent BF in Double J Stent Indwelling Patients with Malignant Tumors |
The Changes of Double J Tube Electron Microscope Monitoring of Patients in Each Group
BF formation is observed on various surfaces. After 30 days, the bacteria on the surface of the double J stent were few and scattered, and covered by a large number of fibrous membranes. Inconsistent amounts of inflammatory attachments and crystals were observed on the surface of the double J stent (Figure 1A). At 90 days, piles of colonies on the surface of the double J stent were observed, and most were cocci (Figure 1B). The number of bacterial colonies in the ducts was (1.73±0.59), (2.26±1. 19), (4. 68±1.31), (5.71±1.06), (7.76±1.37) CFU/cm2 in each group, respectively (P<0.05). It shows that bacterial colonies, inflammatory attachments, crystals, and bacterial biofilm on the surface of the double J stent increase with the extend of the double J tube indwelling time.
Bacterial Identification of BF in Double J Stent of Patients
A total of 58 strains of biofilm-positive bacteria were screened out from 78 positive specimens cultured in a double J stent. The results showed that Staphylococcus was the main type of bacteria in double J stent, followed by Enterococcus, Pseudomonas, Enterobacter, and Acinetobacter. See Table 3.
 |
Table 3 Bacterial Identification of BF in Double J Stent of Patients |
Bacterial Identification of BF in the Urine of Patients
Eleven strains of biofilm-positive bacteria were screened out from 45 positive urine-cultured specimens. After identifying the bacterial genus, it was found that the biofilm bacteria in the urine were mainly Staphylococcus, followed by Enterococcus, Pseudomonas, and Enterobacter, Acinetobacter, see Table 4.
 |
Table 4 Bacterial Identification of Urine BF in Patients |
Comparison of Viable Counts of Bacteria - In Double J Stent and Urine of Patients in the BF-Forming Group and Non-BF-Forming Group
The viable count of bacteria in the double J stent and urine of patients of the BF-forming group exceeded that of the non-BF-forming group (P < 0.05). See Table 5.
 |
Table 5 Comparison of Viable Counts of BF in Double J Stent and in Urine of Patients Between the BF Forming Group and the Non BF Forming Group (Cells/μL, |
Comparison of Double J Stent Indwelling Time Between Groups with and without BF Formation
A markedly longer double J stent indwelling time was recorded with patients in the BF-forming group in comparison with the non-BF-forming group (P < 0.05). See Table 6.
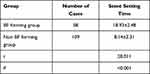 |
Table 6 Comparison of Double J Stent Time of Patients in the BF Forming Group and Non BF Forming Group (d, |
Comparison of Viable Counts Of Bacteria in Double J Stent and Urine of Patients with Different Double J Stent Indwelling Time
As the stenting duration increased, the viable count of bacteria in the double J stent and urine grew significantly (P < 0.05). See Table 7.
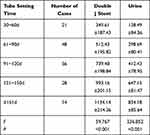 |
Table 7 Comparison of Viable Counts of Biofilm in Double J Stent and Urine of Patients with Different Double J Stent Duration (Cells/μL, |
Analysis of the Influencing Factors BF Formation in Malignant Tumor Patients with Double J Stent Indwelling
Patients with an age of ≥60 years, female, diabetes, hormonal therapy, chemotherapy, anemia, long duration of tube indwelling, and urinary tract infection had significantly increased rates of ureteral BF formation (P < 0.05). See Table 8.
 |
Table 8 Analysis of Urinary Catheter BF Formation in Malignant Tumor Patients with Double J Stent Indwelling |
Logistic Regression Analysis for Multiple Factors of Urinary Catheter BF Formation in Malignant Tumor Patients with Double J Stent Indwelling
Advanced age, chemotherapy, anemia, indwelling time ≥90 d, and urinary tract infection were risk factors for BF formation in patients with malignancy undergoing double J stent indwelling (P < 0.05). See Table 9.
 |
Table 9 Multi-Factor Logistic Regression Analysis of Urinary Catheter BF Formation in Malignant Tumor Patients with Double J Stent Indwelling |
Discussion
Indwelling double J stent is a significant step to prevent upper urinary tract obstruction after malignant tumor surgery to achieve better quality of life.9 Relevant evidence suggests that the rate of catheter-associated urinary tract infections remains at a high level in recent years, which requires sufficient attention.10 The application of double J stent mainly plays a role in fixedly supporting the ureter, relieving the obstruction caused by ureteral edema and inflammation, and preventing postoperative anastomotic leakage and ureteral stenosis,11 which ensures a shorter bed rest and a better rehabilitation effect with no limitation and discomfort from the external drainage stent.12 However, it has been found that the presence of double J stent predisposes to urinary reflux in the ureter, resulting in a rise in the retrograde infection rate of the kidney.13 Zhou Honghui et al14 reported that the rate of urinary tract infection in patients with double J stent indwelling for early radical cervical cancer was about 22.95%. The rate of BF formation in this study (34.73%) was slightly higher than that reported by others14 and was related to the inclusion of gastrointestinal and urinary malignancies in this study. The high molecular materials such as polyurethane used in the double J stent facilitate the adherence of bacteria to its surface and the subsequent formation of BF. Prior research demonstrated that the formation of bacterial BF can increase its resistance by more than 1000 times15 and inhibit its antigenic expression to generate immune escape.16 In addition, under appropriate conditions, the bacteria in BF can diffuse and free from the membrane, causing re-infection.17
In this study, urine and double J stent specimens were collected from patients, respectively, and SEM observation revealed that BF formation was found in 39 of 45 positive urine culture specimens, which was consistent with the results of previous studies, and BF formation was found in 13 other negative urine culture specimens, which may be related to the fact that urine bacteria are mostly planktonic, thereby leading to false-negative results; however, the influence of native bacteria on the results was not excluded, which requires further analysis.18 Moreover, BF formation was found in 58 of 78 positive double J stent culture specimens, and no BF formation was found in negative double J stent culture specimens. These results suggest that the rate of BF formation is higher in patients with malignancy undergoing double J stent indwelling, and double J stent culture more accurately responds to bacterial colonization and BF formation in the urinary catheter than urine culture. The results of bacterial identification showed that Staphylococcus was the dominant type of bacteria in the double J stent and urine culture samples, followed by Enterococcus, Pseudomonas, Enterobacter, and Acinetobacter, which was basically in line with the previous research results.8,14 This suggested that, compared with other types of bacteria, Staphylococcus might be more prone to produce biofilm bacteria, which provides a reference for the selection of clinical antibacterial drugs.
Moreover, this study found that the viable count of bacteria in both double J stent and urine rose sharply with the increase of stenting duration, indicating that the risk of BF formation grew with the increase of stenting duration, which was confirmed by the results of electron microscope scan. In clinical practice, the application of indwelling double J stent requires strict management to reduce unnecessary use. To reduce the formation of BF, Double J stent requires regular replacement or the periodical evaluation of double J stent removal in a timely manner. Analysis of factors influencing the formation of BF in the urinary catheter in patients with malignancy undergoing double J stent indwelling found that patients with an age of ≥60 years, female, diabetes, hormonal therapy, chemotherapy, anemia, long duration of tube indwelling, and urinary tract infection had significantly increased rates of ureteral BF formation, and advanced age, chemotherapy, anemia, indwelling time ≥90 d, and urinary tract infection were risk factors for BF formation in patients with malignancy undergoing double J stent indwelling. It indicated that enhanced nutritional management for elderly patients, urethral care for female patients, and strict control of blood glucose levels in diabetic patients are warranted to reduce the rate of urinary catheter-related infections.
In conclusion, there is a high rate of BF formation in patients with malignancy undergoing double J stent indwelling, with Staphylococcus as the dominant species. Treatment requires enhanced urinary catheter management and nutritional status to inhibit BF formation and lower the rate of urinary catheter-related infections. The shortcoming of this study lies in the absence of characterization analysis of the isolates,19 which limits the determination of treatment protocols and will be explored in further studies.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sundaramurthy S, Thomas RJ, Herle K, et al. Double J stent removal in paediatric patients by Vellore Catheter Snare technique: a randomised control trial. J Pediatr Urol. 2019;15(6):661–668. doi:10.1016/j.jpurol.2019.08.009
2. Haitao Y, Wei Z, Chunhong N. Comparison and analysis of ureteral stricture caused by malignant tumor treated by conventional surgery and minimally invasive double J stent retrograde insertion. Chin Basic Med. 2021;28(2):203–207.
3. He JW, Shu G, Songtao X, et al. Analysis of clinical data of 96 cases of ureteral obstruction caused by gynecological malignant tumor. Chin J Endoscopy. 2020;26(2):65–69.
4. Dengjun H, Yong L, Chan A, et al. Effect of pre-set double J stents on complications of flexible ureteroscopic lithotripsy in kidney calculi. Med J Qilu. 2017;155(5):87–89.
5. Rajput A, Thakur A, Sharma S, et al. aBiofilm: a resource of anti-biofilm agents and their potential implications in targeting antibiotic drug resistance. Nucleic Acids Res. 2018;46(D1):894–900. doi:10.1093/nar/gkx1157
6. Betschart P, Zumstein V, Buhmann MT, et al. Symptoms associated with long-term double-J ureteral stenting and influence of biofilms. Urology. 2019;134(4):72–78. doi:10.1016/j.urology.2019.08.028
7. Hong S, Yushan W, Ziyu S. National operating procedures for clinical examination. People’s Health Publishing House; 2015.
8. Yuncai Y, Junlin Z, Jianming C. Characteristics and drug resistance of pathogens causing catheter-related urinary tract infection. Chin J Disinfect. 2017;34(10):986–988.
9. AI-ling Z, Qiong-feng X, Fang-lei X, et al. Analysis of influencing factors of time of indwelling catheter for patients with benign prostatic hyperplasia and malignant tumor after operation. Chin J Mod Nurs. 2017;23(13):1718–1723.
10. Mingrong S, Wenzhi H, Quanhui W. Investigation on prevalence rate of catheter-related urinary tract infection from 2012 to 2018. Chin J Nosocomiol. 2020;30(15):91–95.
11. Alnadhari I, Alwan MA, Salah MA, et al. Treatment of retained encrusted ureteral double-J stent. Arch Ital Urol Androl. 2019;90(4):265–269. doi:10.4081/aiua.2018.4.265
12. Wuxue LI, Zhao X, Changbao XU, et al. Clinical observation of time of double J stent indwelling in treatment of complex ureteral calculi with ureteroscope. J Pract Med. 2017;33(2):256–258.
13. Shi ZJ, Qiong Z, Lixin J, et al. Analysis of clinical characteristics of double J stent urinary system infection. J Wuhan Univ. 2020;41(3):109–113.
14. Zhou HH, Wang N, Ding JJ. Etiological characteristics and influencing factors of urinary tract infection in patients with double J stents indwelling in radical hysterectomy for early cervical cancer. Chin J Nosocomiol. 2019;29(18):2839–2842.
15. Goswami S, Sarkar R, Saha P, et al. Effect of human placental extract in the management of biofilm mediated drug resistance - A focus on wound management. Microb Pathog. 2017;111(34):307–315. doi:10.1016/j.micpath.2017.08.041
16. Jia L, Sun L, Wei L, et al. A nuclease from Streptococcus mutans facilitates biofilm dispersal and escape from killing by neutrophil extracellular traps. Front Cell Infect Microbiol. 2017;28(7):97–99.
17. Heim CE, Bosch ME, Yamada KJ, et al. Lactate production by Staphylococcus aureus biofilm inhibits HDAC11 to reprogramme the host immune response during persistent infection. Nat Microbiol. 2020;5(10):1271–1284. doi:10.1038/s41564-020-0756-3
18. Zhang JZ. Exploration on related factors and preventive measures of indwelling urethral catheterization in urinary system infection of hospital. Contemp Med. 2017;23(6):116–117.
19. Gajdács M, Kárpáti K, Stájer A, et al. Insights on carbapenem-resistant Pseudomonas aeruginosa: phenotypic characterization of relevant isolates. Acta Biologica Szegediensis. 2021;65(1):105–112. doi:10.14232/abs.2021.1.105-112
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




