Back to Journals » Clinical Optometry » Volume 12
Analysis of Alphabet Patterns of Deviations Found in Patients Without Strabismus in Primary Position
Authors Gantz L , Millodot M, Roth GL
Received 5 December 2019
Accepted for publication 21 February 2020
Published 20 March 2020 Volume 2020:12 Pages 49—56
DOI https://doi.org/10.2147/OPTO.S197783
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Liat Gantz,1 Michel Millodot,2 Gary Lewis Roth1
1Department of Optometry and Vision Science, Hadassah Academic College, Jerusalem, Israel; 2School of Optometry and Vision Sciences, Cardiff University, Cardiff, UK
Correspondence: Liat Gantz
Department of Optometry and Vision Science, Hadassah Academic College, 37 Haneviim St., Jerusalem 91010, Israel
Tel +972-2-629-1959
Fax +972-54-723-5511
Email [email protected]
Aim: To detect alphabet patterns in a group of patients without strabismus and to determine whether they induced any convergence insufficiency type symptoms.
Methods: Data on subjective refraction, distance and near heterophoria, distance and near positive fusional vergence (BO), near point of convergence (NPC), measurements of upgaze and downgaze made 45° above and below the primary position with alternate cover test and a prism bar at a distance of 37.5 cm, were collected from participants of two clinics. Symptoms were assessed using the 15-item Convergence Insufficiency Symptoms Survey (CISS) to determine a symptom score. Association between alphabet patterns and the other variables was analyzed using parametric and non-parametric tests.
Results: Out of 122 patients, 14 were found to present an alphabet pattern. Defining a V pattern exophoria ≥ 15–prism dioptre or ≥ 10–prism dioptre deviation, three patients (2.5%) and 12 patients (9.8%) were identified, respectively. In addition, one case resembled an X pattern and another a diamond pattern. The refraction, distance and near heterophoria, positive fusional vergence and CISS scores were not significantly different in the participants with V pattern compared to those without V pattern.
Conclusion: Alphabet patterns, especially V type, were demonstrated in approximately 11.5% of a sample of 122 non-strabismus patients. These alphabet patterns were found not to be associated with convergence insufficiency-like symptoms.
Keywords: binocular vision anomalies, incomitant deviations, alphabet patterns, V pattern; heterophoria
Introduction
Incomitant heterotropia describes an anomaly of binocular vision in which the angle of deviation varies depending on which eye is fixing, with deviation typically greater when the habitually deviated eye fixates.1 Incomitant heterophoria describes a varying angle of deviation at varying directions of gaze when there is no demand for binocular fusion in patients with normal binocular vision.2–4 Incomitance is present in 13% of heterotropia cases but much less common in heterophoria.2,4 Incomitance in heterotropia is usually secondary to physical damage to muscle tissue;3,5-7 or muscle dysfunction associated with innervational deficiencies;8–11 or congenital due to a developmental anomaly of the motor system.12 Treatment options for heterotropia include extraocular muscle surgery, yoked vertical prisms (with or without additional base-in horizontal prisms), and visual therapy/vision training.3
Heterophoria is typically measured clinically in primary gaze position (straight-ahead) for both distance and near fixation, though normal daily activities involve head and eye positions that vary from primary position.4
Horizontal deviations can present as incomitant deviations called alphabet patterns, commonly A and V patterns in which a significant increase or decrease in the angle of deviation is noted between an upgaze and downgaze. Occasionally, alphabet patterns may exist without a primary angle deviation.
In V pattern there is a marked increase in divergence on upgaze (more exotropia) and a marked increase in convergence on downgaze (less exotropia). In A pattern there is a marked increase in convergence on upgaze (more esotropia) and a marked increase in divergence on downgaze (less esotropia). Although some incomitant heterophorias could be regarded as a normal physiological deviation, A patterns are considered abnormal physiological variants by some,3 and their existence (physiological or not) can be associated with abnormal head postures3,7 and/or symptoms.3 There are other forms of alphabet patterns such as X pattern in which there is increase in divergence in both up- and downgaze;13 diamond pattern in which there is an increase in convergence in up- and downgaze; Y pattern in which there is an increase in divergence on upgaze and no significant difference between the primary position and downgaze;9 and arrow pattern in which there is an increase in divergence on downgaze and no significant difference between the primary position and upgaze,11 although these last two forms may be variants of the classic A and V patterns.11,14 A V pattern is defined as a difference between upgaze and downgaze that is equal or greater than 15 prism diopters (pd), whereas an A pattern is defined as a difference equal or greater than 10 pd.3,11 The higher criterion adopted for the V pattern stems from the fact that there is a physiological tendency for the eyes to diverge in upgaze.14 It must be noted that these values are arbitrary and in fact it has been suggested that a V pattern exists when the difference is 10 pd in heterophoric3 and heterotropic15 patients.
A and V patterns are most common in patients with heterotropia, with a reported prevalence between 12% and 50%.16,17 They are also common in Duane’s retraction syndrome and in Brown’s syndrome.14 Asthenopia and diplopia are the most common symptoms of those with incomitant strabismic deviations3,18 and patients may present with mongoloid features3 or compensatory head posture.
However, to the best of our knowledge, the relationship between incomitant deviation in elevation and depression in patients without strabismus, and symptoms has not been investigated. Therefore, the aim of this study was to determine and analyze cases of alphabet patterns in a cohort of patients without heterotropia presenting to the optometry department clinics or community- based practice and to test whether the alphabet patterns are in any way related to symptoms.
Methods
Study Population
This study was conducted in the Optometry Clinic of Hadassah Academic College and at Rachel Roth community-based Eye Clinic, both in Jerusalem, Israel between June 2015 and September 2016. Both clinics are routine refraction clinics and not clinics that specialize in heterotropia. Patients with systemic or ocular diseases and any history of eye surgery, amblyopia, constant heterotropia, partial low vision (best-corrected distance and near visual acuity of less than 6/9), nystagmus, trauma, visual field loss, or unable to complete the questionnaire were not included in the study. Patients unable to exhibit reliable retinoscopic or subjective refractive results, or those with inadequate fixation during the cover test were also excluded. Of the 129 volunteers, seven were excluded because they did not meet inclusion criteria. Therefore, 122 patients (53 men, 69 women, mean age: 37 ± 16 years, range: 14–75) were included in the analysis. Of these, 60 patients were seen at Hadassah Academic College and 62 at Rachel Roth clinic. The study was approved by the Ethics Committee of Hadassah Academic College and was conducted in accordance with the Declaration of Helsinki. An explanation was given to patients attending the clinic and those who volunteered signed a statement of informed consent. For participants younger than 18 years (eight participants), a parent also signed the consent form.
Questionnaire
Prior to the eye examination patients were asked to complete a Convergence Insufficiency Symptoms Survey (CISS) questionnaire.19–21 The questionnaire was designed to quantify the severity of symptoms and to monitor these before and after convergence insufficiency (CI).19 It has been shown to be reliable and valid in distinguishing symptomatic patients with CI from those with normal binocular vision.19,21,22 It has been shown not to be specific for CI23 and has been used previously to assess visual symptoms not specifically associated with CI. For example, it has been used to assess symptoms associated with general binocular vision anomalies,24 to assess eyestrain during prolonged viewing of smartphones,25 to assess symptoms after viewing stereoscopic displays,26 and to assess symptoms associated with Parkinson’s Disease.27 The questionnaire comprises 15 questions to which the patient must respond with one of four answers (infrequent, sometimes, fairly often, always) and from which a total score is established.
Procedures
All measurements were performed by the same examiner (GR). Testing included distance Snellen visual acuity, near point of convergence (NPC) break and recovery with a tip of a pen, distance and near heterophorias using prism-neutralized cover testing, and positive fusional vergences (BO) (blur, break and recovery). The refractive status of each eye was then determined with non-cycloplegic retinoscopy and standard subjective techniques including binocular balance method with alternatives such as polaroid, Humphriss Immediate Contrast test, and alternate occlusion (in that order), as needed. If a patient wore a near correction, the preliminary tests were performed with the correction in place.
A modified Royal Air Force (RAF) rule with colored stickers affixed to a vertical bar as targets ensured that the exact angle for gaze testing was achieved and maintained. Three positions of gaze were measured, at a near testing distance, and without correction in order to eliminate prismatic effects of viewing through spectacle correction. The three directions included upgaze, primary gaze (straight-ahead) and downgaze with a prism bar or loose prisms. The upgaze and downgaze positions were measured at 45 degrees from the primary position. This angle was chosen to maximize possible changes in heterophoria as was done in several studies.3,28,29 Two measurements were made at each gaze position and the findings were averaged. The entire examination duration was approximately 45 mins.
Data Analysis
Data were entered into an excel spreadsheet for subsequent analysis. Data were analyzed for the entire group (all ages), and as two separate age groups (young group: 14–39 years old, and presbyopic group: 42–75). When analyzed as one data set, normality was assessed using the Anderson–Darling test. Normally distributed data were analyzed using Student’s t-tests and Pearson correlation coefficients. For variables that were not normally distributed, non-parametric tests such as the Mann–Whitney U-test and Spearman rank correlation test were used. When analyzed as two separate age groups, an ANOVA test was used with one factor (age) and a Chi Square was applied (examining prevalence of V-pattern exophoria as a binary measure). Excel and SPSS software were used for the statistical analysis. Values of p<0.05 were considered significant.
Results
The data from 60 patients from the Hadassah Academic College clinics and 62 patients from the Rachel Roth clinics were compared with regard to the difference in the values of heterophoria during upgaze versus downgaze, heterophorias (distance and near) and CISS scores, and were not found to be significantly different (see Table 1). Hence, the data from both clinics were analyzed as one sample.
 |
Table 1 Characteristics of Outcome Measures at Rachel Roth (RR) and Hadassah Academic College (HAC) Clinics |
Of the sample of 122 patients, 75 were 14 to 39 years of age (mean age: 25 ± 6) and 47 were 42 to 75 years of age (mean age: 55±8). Because the prevalence of Vxp is a binary variable, a ChiSquare test was performed to examine the relationship between age and prevalence of Vxp. The relationship between these variables was not significant (X2(1, N=122)= 1.03, p=0.31) indicating no difference between the presbyopic and non-presbyopic groups. Additionally, the difference between the heterophoria value at upward and downward gaze (used to determine the alphabet pattern) between the presbyopic and non-presbyopic groups was not significantly different (Mann–Whitney U-test, p=0.13). The only variable that was significantly different between the young and presbyopic populations was the near heterophoria (mean difference: 3.35 pd; 95% Confidence Interval, −5.4 to 1.27; p = 0.002). This is consistent with other studies who report that near heterophoria becomes more exophoric with age in presbyopes.30 Therefore, the data from non-presbyopic and presbyopic populations were also analyzed as one sample.
None of the patients presented noticeable head tilt, craniofacial or neuromuscular abnormalities. Of the 122 patients, 12 (9.8%) presented with a Vxp ≥10 pd of which three had Vxp pattern of ≥15pd (2.5%) and nine had a Vxp of 10–14pd. In addition, one case resembled an X pattern and another resembled a diamond pattern (See Appendix A). Another 10 were considered Vxp suspect because of a measured upgaze vs downgaze heterophoria difference ≥8 and one was a diamond suspect. The suspect cases were not included in the analysis nor were the two odd alphabet patterns. Interestingly, no case of A pattern was detected. Hence, all data of Vxp were analyzed as one sample. The Vxp values of the 12 cases (Table 2) were not significantly correlated with either the distance or near heterophoria (Spearman’s r = 0.24, 95% Confidence Interval −0.37 to 0.71; p =0.45 and r = 0.243, 95% Confidence Interval −0.38 to 0.72 p = 0.45, respectively) or the CISS scores (Spearman’s r = 0.19, 95% Confidence Interval −0.42 to 0.68; p = 0.56). The near heterophoria was not significantly different from the primary gaze heterophoria measurement for patients without Vxp (mean difference: 0.90 pd, 95% Confidence Interval of the difference in means −0.53 to 2.32, p = 0.25) and for Vxp patients (mean difference: 2.58 pd, 95% Confidence Interval of the difference in means −3.20 to 7.30, p = 0.43).
 |
Table 2 Comparison Between Patients With and Without Vxp |
There was no significant correlation between the upgaze-downgaze values of the 108 patients without Vxp and their CISS scores (r =0.02, 95% Confidence Interval −0.016 to 0.21; p = 0.82). Comparing the non-Vxp and Vxp groups using the multiple comparison Bonferroni correction to the 14 variables only p-values <0.003 were considered significant. As such, there was no significant difference between the non-Vxp and Vxp groups in the refraction, distance and near heterophoria, NPC, distance and near BO values and CISS scores (Table 3). As expected, the mean difference between the heterophoria measured in upgaze vs downgaze of the non-Vxp and Vxp groups was significantly different. Only one patient with a Vxp pattern had a remote NPC but a normal CISS score although the exophoria at near exceeded that at distance by 5.5 pd, and four non-Vxp patients had NPC ≥10 cm but normal CISS and near heterophoria values. Although the mean CISS value was higher in the Vxp than in the non-Vxp (14.57 vs 11.00 (mean difference 3.60, 95% Confidence Interval −1.70 to 8.90) the difference was not significant (p = 0.19).
 |
Table 3 Comparison Between the Non-Vxp and Vxp Patients |
Discussion
It is well documented that alphabet patterns are present in horizontal strabismus at the primary position.18 The percentage varies between 12% and 50%,16,17,31,32 but on average it is reported to occur in about 25% of patients with strabismus.15,17 In patients with strabismus at primary position, the most common pattern is V pattern esotropia.17 However, the present study demonstrates the existence of alphabet patterns, especially V pattern exophoria, in a group of patients free of strabismus in primary position. Although it had been noted anecdotally by some12 and reported by others2,29 this is, to the best of our knowledge, the first systematic determination of Vxp that examines symptomology in such a group of patients. Table 4 summarizes two previous research studies as well as the present study reporting alphabetical patterns in samples of patients without strabismus at primary gaze. It is important to note that the definitions of alphabetical deviations used by the studies are not uniform thus it is difficult to compare directly. For example, Stuart & Burian2 reported all differences between upgaze and downgaze at 20 and 40 degrees that were greater than 1 pd without reporting raw values that would allow to adopt the same definition as the present study (deviations greater than 10 pd). Magee29 did not specify the angle of the gaze and the testing distance.
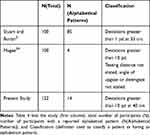 |
Table 4 Reported Prevalence of Alphabetical Deviations in Patients Without Strabismus at Primary Position |
Our results are not negligible; out of 122 patients, three presented a Vxp of 15 pd or more and another nine with a difference of ≥10 pd. In addition, one patient showed a clear resemblance to a diamond pattern and another patient, an X pattern. These results are similar to a study in which out of 100 non-strabismus patients several patients had Vxp deviations of up to 18 pd in near fixation (33cm) and at 40° upgaze and downgaze,2 as well as in another study in which three cases were found with Vxp ≥10 pd of which two ≥15 pd in 100 non-strabismus patients.29 There is no criterion value regarded as diagnostic of these conditions. Most authors regard a difference of 15 pd or greater as diagnostic of a V pattern. Other studies have suggested a difference of 10 pd but this figure is actually arbitrary.3,15 On the basis of 15 pd, our results show a proportion of 2.5%, but if the results include 10 pd, it becomes 9.8%. When all alphabetical patterns measured in extreme positions of gaze are considered the prevalence increases to 11.5%.
The reason why we detected many cases of alphabet patterns can be related to the extreme angle of measurement of the up and downgaze (45°) compared to the commonly used angle of 25–30°,18 although 40° was previously used by Stuart & Burian2 in a sample of patients without strabismus at primary gaze. Greater angles could lead to artificial deviations or pseudodeviations.29 In strabismus patients, it has been shown that measuring at extreme angles such as 45° in upgaze and 55° in downgaze results in a mean increase of 5 pd in V pattern compared to measurements made at 25°.30 Similarly, a study examining heterophoria of six patients at primary gaze, 20 degrees upgaze, and 20, 40, and 60 degrees downgaze found that the heterophoria varies by approximately 4 pd with gaze position.32 This result was confirmed in another study in which the mean increase was 4 pd.28 Differences in the range of 4 pd are much lower than values that can be considered alphabetical patterns. This could explain why Jampolsky33 suggested that the diagnosis of A and V patterns should be based on extreme angles of gaze positions. Still, there is no study to establish which angle of measurement is best for strabismus management but surgical correction of a known large pattern would likely provide fusion in more positions of gaze.29
The extreme up-gaze and down-gaze angles in combination with the myopic refractive error could have also impacted our findings. Specifically, a long axial length of the globe that encounters the curved orbital wall in extreme gazes could impact the gaze deviation. However, as seen in Table 3, the spherical equivalent refractive error of the right and left eyes of the 12 Vxp patients was not significantly different than the non-Vxp patients, both being myopic, and differing by less than a Diopter. Therefore, the globe axial length is not likely to account for our findings, though cannot be precluded without ocular biometry measurements.
The aetiology of V patterns in strabismus is uncertain, although it has been suggested to be due to an overaction of the inferior oblique muscles, accompanied by overaction of the superior rectus muscles which partially abduct the eyes in upgaze,34 and of the lateral rectus muscles which contribute to elevation in upgaze.31 It is worth noting that there does not appear to be a proven mechanism and it is alternatively possible that the alphabet patterns are iatrogenic and induced by strabismus surgery. However, overaction of the inferior oblique is consistent with extorsion typically seen in a patient with a V pattern.18 It is not known whether the same process occurs in patients without strabismus at primary gaze, but it is plausible that a mild aspect of the aforementioned aetiology prevails in Vxp patients free of strabismus like the patients of the present study.
Only one patient with an alphabet pattern presented with convergence insufficiency as would be detected by the following four signs:19 Convergence Insufficiency Symptoms Survey (CISS) score above 21, near point of convergence farther than 6 cm, exophoria at near at least 4 prism diopters larger than the exophoria at distance and BO break lower than 15 prism Diopters. Moreover, there was no significant correlation between the Vxp values and CISS scores in the group of 12 patients with the Vxp pattern. In fact, all but one of the patients with an alphabet pattern had a CISS score <21 which is considered asymptomatic of convergence insufficiency in individuals older than 18 years of age.19
None of the patients with Vxp assumed a chin-up head posture, but this is not surprising since only a small percentage of patients with strabismus with a V pattern assume an abnormal head position (9% according to Kushner).34 Additionally, the patients with Vxp did not report blur or diplopia when reading. Hence, it is inferred that the detected heterophoria may be considered compensated.
There are limitations to this study. The proportion of patients found with an alphabet pattern cannot necessarily be regarded as a prevalence of the general population but only of that existing in this sample of patients who were seen in two optometric practices and were not recruited randomly since they volunteered. Indeed, some of the patients had shown an indication of an incomitant deviation with the cover test during routine examination and were asked to volunteer. However, as mentioned in the study methods, these clinics are routine refraction clinics and not clinics that specialize in strabismus. It may be inferred that the Vxp determined in this study may not reflect reality because it was measured without the patient’s correction, as was actually performed by others.2,4 However, these measurements were made at near and adjusting spectacles is not only cumbersome but may induce prismatic or optical distortions and at near the target is magnified and the effect of blur is thus mitigated. The difference with and without correction in up- and downgaze is likely to be very small since there was no significant difference in the primary gaze position. Nevertheless, more research is needed to evaluate this possible discrepancy.
Another possible limitation of the study is that the inclusion criteria did not include extraocular motility testing, stereopsis, suppression, or double Maddox rod testing that would preclude binocular vision anomalies. However, cover-uncover testing, fusional vergence ranges and NPC tests were carried out. As such, suppression would have been detected in the fusional vergence ranges and NPC testing. The cover-uncover testing would have detected strabismus. Brown’s Syndrome which is typically noticeable with adduction and upward gaze35 would have been diagnosed with NPC testing as well as on upgaze with the RAF rule with covering of the fellow eye. Similarly, Duane’s retraction syndrome also would have been diagnosed with adduction during NPC testing.36 We are therefore confident that the participants of the study did not have strabismic extraocular muscle abnormalities which would have appeared during fusional vergence range or NPC testing. Finally, we did not assess the accommodative amplitude of the patients and cannot rule out that the symptoms reported are associated with accommodative anomalies. In fact, 22 of the non-Vxp subjects had CISS scores higher than 21 and only one patient with Vxp indicating that perhaps symptomatology is more frequent in the non-Vxp patients. In the future, the experiment can be repeated on a cohort of non-presbyopes with accommodative amplitudes within their age-dependent norms.
An additional possible limitation may be the inclusion of a wide range of ages in the sample. It could be argued that younger populations can accommodate and this can affect their heterophoria value.30,37,38 Of the 12 Vxp patients, five were presbyopic. However, there was no significant difference between the presbyopic and non-presbyopic groups as stated in the results section.
In conclusion, this study shows that in a small cohort of 122 patients free of strabismus at primary gaze, a V pattern is the most common type of alphabet pattern, albeit to a much smaller extent than in patients with strabismus, confirming the results of other similar studies.2,7,39 It also demonstrates that the V pattern heterophoria is not associated with symptoms of convergence insufficiency.
Data Sharing Statement
The data used to support the findings of this study are included in the https://www.dovepress.com/get_supplementary_file.php?f=197783.xlsx.
Acknowledgment
This project was supported by a Grant from the Research Fund of Hadassah Academic College.
Disclosure
The authors have no conflicts of interest to declare.
References
1. Economides JR, Adams DL, Horton JC. Variability of ocular deviation in strabismus. JAMA Ophthalmol. 2016;134(1):63–69. doi:10.1001/jamaophthalmol.2015.4486
2. Stuart JA, Burian HM. Changes in horizontal heterophoria. Am J Ophthalmol. 1962;53:274–279. doi:10.1016/0002-9394(62)91175-3
3. Nizza A, Dufeck D. The’A’and’V’pattern syndromes. J Am Optom Assoc. 1985;56(2):133–140.
4. Osuobeni EP, Al‐amir OM. Gaze‐related near heterophoria incomitance. Clin Exp Optom. 1996;79(2):76–81. doi:10.1111/j.1444-0938.1996.tb04979.x
5. Ansons AM, Davis H. Alphabet patterns. In: Diagnosis and Management of Ocular Motility Disorders. Oxford,UK: Wiley Blackwell; 2014:431–450.
6. Oh SY, Clark RA, Velez F, Rosenbaum AL, Demer JL. Incomitant strabismus associated with instability of rectus pulleys. Invest Ophthalmol Vis Sci. 2002;43(7):2169–2178.
7. Parks MM, Mitchell PR. Chapter 16: a and V Patterns. In: Twj EA, editor. Duane’s Ophthalmology on CD-ROM. Philadelphia, PA, USA: Lippincott Williams & Wilkins; 2006.
8. Clark RA, Miller JM, Rosenbaum AL, Demer JL. Heterotopic muscle pulleys or oblique muscle dysfunction? J AAPOS. 1998;2(1):17–25. doi:10.1016/S1091-8531(98)90105-7
9. Coats DK, Paysse EA, Stager DR. Surgical management of V-pattern strabismus and oblique dysfunction in craniofacial dysostosis. J AAPOS. 2000;4(6):338–342. doi:10.1067/mpa.2000.110337
10. Guyton DL. Sensory torsion as the cause of primary oblique muscle overaction/underaction and A-and V-pattern strabismus. Binocul Vis Eye Muscle Surg Q. 1994;9:209–236.
11. Wright KW. Alphabet patterns and oblique muscle dysfunctions. In: Wright KW, Spiegel PH, Thompson L, editors. Handbook of Pediatric Strabismus and Amblyopia. New York, NY, USA; 2006:284–322.
12. Evans BJW. Pickwell’s Binocular Vision.
13. Kekunnaya R, Shenoy HB, Gupta A, Sachdeva V. Biomechanical analysis of X-pattern exotropia. Am J Ophthalmol. 2011;152(5):881. doi:10.1016/j.ajo.2011.08.002
14. Rowe F. Clinical Orthoptics.
15. Knapp P. “A” and “V” patterns. In: Symposium on Strabismus: Transactions of the New Orleans Academy of Ophthalmology. St. Louis, MO, USA: Mosby; 1971:242–254.
16. Rosenbaum AL, Santiago AP. Pattern strabismus. In: Rosenbaum AL, Santiago AP, editors. Clinical Strabismus Management. Philadelphia, PA, USA: WB Saunders; 1999:202–215.
17. Costenbader F. Introduction in symposium: the A and V patterns in strabismus. Trans Am Acad Ophthalmol Otolaryngol. 1964;68:354–355.
18. Kushner BJ. A, V and other alphabet pattern strabismus. In: Taylor D, Hoyt GS, editors. Pediatric Ophthalmology and Strabismus.
19. Rouse MW, Borsting EJ, Lynn mitchell G, et al. Validity and reliability of the revised convergence insufficiency symptom survey in adults. Ophthal Physiol Opt. 2004;24(5):384–390. doi:10.1111/opo.2004.24.issue-5
20. Group CITTI. Validity of the convergence insufficiency symptom survey: a confirmatory study. Optom Vis Sci. 2009;86(4):357. doi:10.1097/OPX.0b013e3181989252
21. Scheiman M, Mitchell GL, Cotter S, et al. The convergence insufficiency treatment trial: design, methods, and baseline data. Ophthalmic Epidemiol. 2008;15(1):24–36.
22. Borsting E, Rouse MW, Deland PN, et al. Association of symptoms and convergence and accommodative insufficiency in school-age children. Optometry. 2003;74(1):25–34.
23. Horan L, Ticho BH, Allen M. Is the convergence insufficiency symptoms survey specific for convergence insufficiency? J AAPOS. 2013;17(1):e17. doi:10.1016/j.jaapos.2012.12.061
24. Liu C, Chase C, Drew S, et al. Tonic accommodation correlates with accommodative amplitude-scaled facility test for symptomatic graduate students. Invest Ophthalmol Vis Sci. 2013;54(15):4259.
25. Long J, Cheung R, Duong S, Paynter R, Asper L. Viewing distance and eyestrain symptoms with prolonged viewing of smartphones. Clin Exp Optom. 2017;100(2):133–137. doi:10.1111/cxo.2017.100.issue-2
26. Fortuin MF, Lambooij MT, IJsselsteijn WA, Heynderickx I, Edgar DF, Evans BJ. An exploration of the initial effects of stereoscopic displays on optometric parameters. Ophthal Physiol Opt. 2011;31(1):33–44. doi:10.1111/opo.2010.31.issue-1
27. Law C, Chriqui E, Kergoat M-J, et al. Prevalence of convergence insufficiency-type symptomatology in Parkinson’s disease. Can J Neurol Sci. 2017;44(5):562–566. doi:10.1017/cjn.2017.39
28. Procianoy E, Procianoy L. Prevalence of horizontal deviation pattern changes with measurements in extreme gazes. Eye. 2008;22(2):229. doi:10.1038/sj.eye.6702588
29. Magee AJ. Minimal values for the A and V syndromes. Am J Ophthalmol. 1960;50(5):753–756. doi:10.1016/0002-9394(60)90108-2
30. Spierer A, Hefetz L. Normal heterophoric changes: 20 years’ follow-up. Graefes Arch Clin Exp Ophthalmol. 1997;235(6):345–348. doi:10.1007/BF00937281
31. Urist MJ. The etiology of the so-called A and V syndromes. Am J Ophthalmol. 1958;46(6):835–844. doi:10.1016/0002-9394(58)90995-4
32. Mon-williams M, Plooy A, Burgess-limerick R, Wann J. Gaze angle: a possible mechanism of visual stress in virtual reality headsets. Ergonomics. 1998;41(3):280–285. doi:10.1080/001401398187035
33. Jampolsky A. Transactions of the new orleans academy of ophthalmology; 1978.
34. Kushner BJ. Ocular causes of abnormal head postures. Ophthalmology. 1979;86(12):2115–2125. doi:10.1016/S0161-6420(79)35301-5
35. Brown HW. True and simulated superior oblique tendon sheath syndromes. Doc Ophthalmol. 1973;34(1):123–136. doi:10.1007/BF00151801
36. Tasman W, Jaeger EA. Duane’s Clinical Ophthalmology. Vol. 1. Philadelphia,PA,USA: Williams and Wilkins Lippincott; 1994.
37. Goss DA, Rainey BB. Relationship of accommodative response and nearpoint phoria in a sample of myopic children. Optom Vis Sci. 1999;76(5):292–294. doi:10.1097/00006324-199905000-00016
38. Howarth PA, Heron G. Repeated measures of horizontal heterophoria. Optom Vis Sci. 2000;77(11):616–619. doi:10.1097/00006324-200011000-00013
39. Kushner BJ. Torsion and pattern strabismus: potential conflicts in treatment. JAMA Ophthalmol. 2013;131(2):190–193. doi:10.1001/2013.jamaophthalmol.199
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
