Back to Journals » Medical Devices: Evidence and Research » Volume 16
An Innovative Design for the Vaginal Speculum
Authors Bouquet JM , Naji R, Armas CA, Roldan V, Selkhi S, Bentley CZ, Zapata I, Fisher J
Received 8 April 2023
Accepted for publication 31 August 2023
Published 25 September 2023 Volume 2023:16 Pages 211—218
DOI https://doi.org/10.2147/MDER.S415558
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Jean M Bouquet,1 Rayyan Naji,2 Carlos A Armas,2 Valentina Roldan,2 Shadi Selkhi,2 Camille Z Bentley,1 Isain Zapata,3 Jensen Fisher4
1Department of Family Medicine, Rocky Vista University College of Osteopathic Medicine, Englewood, CO, 80112, USA; 2Department of Biomedical Engineering, College of Engineering and Computing, Florida International University, Miami, FL, 33174, USA; 3Department of Biomedical Sciences, Rocky Vista University College of Osteopathic Medicine, Englewood, CO, 80112, USA; 4Medical Humanities Department, Rocky Vista University College of Osteopathic Medicine, Englewood, CO, 80112, USA
Correspondence: Jean M Bouquet, Department of Family Medicine, Rocky Vista University College of Osteopathic Medicine, 8401, S. Chambers, Englewood, CO, 80112, USA, Email [email protected]
Introduction: The main objective of this study is to evaluate the effectiveness of a newly designed vaginal speculum, the Bouquet Speculum, in-vitro. The setting of this study was at Florida International University and involved four senior students in the Department of Biomedical Engineering.
Methods: A phantom vaginal model was used to test three variables of the Bouquet Speculum (Visibility, Pressure and Gynecologic Tools tests). As this was bench-lab testing with simulated models, no human participants were involved in this study.
Results: The results of this in-vitro study are as follows: The visibility test demonstrated statistically better visualization of the cervix and the cervical os (sampling area for pap tests) with the Bouquet Speculum over the existing 2-bladed speculum at all intrapelvic pressures; The pressure test demonstrated an equal radial distribution of force, without breakage, across the Bouquet Speculum; The gynecologic tools test demonstrated that the Bouquet Speculum is compatible with the existing speculum and standard gynecologic tools in terms of retrieving samples and accessing the cervical os and entire cervix during gynecologic procedures and screening.
Conclusion: The gynecologic screening and procedural value of this innovative change in the design of the vaginal speculum could save hundreds of thousands of lives every year, provide a more comfortable exam for the patient, and result in a more efficient and user-friendly provider experience.
Keywords: medical device, vaginal speculum, public health, gynecology
Background
Cervical cancer kills over 342,000 women every year.1 It is the second most common cancer affecting women in developing countries and results in significant morbidity and mortality as well as negatively impacting these communities in many ways.2 Human Papilloma Virus (HPV) is the single most important risk factor for cervical cancer and pre-cancers, responsible for 99.7% of the incidence.3 Routine gynecological screenings effectively detect and prevent cervical cancer, with a high cure rate with early detection.4 Unfortunately, there is a significant lack of screening in developing countries and certain vulnerable and marginalized populations in the United States for a variety of reasons. Some of the reasons include lack of knowledge and awareness about cervical cancer and dysplasia, inaccessibility to health clinics and female providers, and the fear of embarrassment, pain, and discomfort from the pap test or procedure involving a vaginal speculum.5 In some instances, the existing speculum creates an additional barrier to effective screening and gynecologic procedures by failing to provide full cervical visibility due to anatomical variation or lateral vaginal wall collapse and causing patient discomfort and anxiety.6–8
Limitations of the Traditional Speculum
The traditional, two-bladed vaginal speculum is the oldest instrument in the history of obstetrics and gynecology. Its design goes back to 79 AD when a 2-bladed bronzed speculum was found preserved in the ashes of Pompeii when Mt. Vesuvius erupted.9 This traditional two-bladed vaginal speculum has three apparent limitations. First, in some women, such as multiparous and obese patients with a cervix, where there is vaginal wall laxity, the 2-bladed design allows for lateral vaginal wall collapse, thus impeding the view of the cervix and making the diagnosis of cancer or dysplasia challenging. Additionally, this creates challenges to procedures such as cervical cancer and pre-cancer treatment, intrauterine device (IUD) insertion and removal, and artificial insemination. Even experienced clinicians have difficulty with lateral vaginal wall collapse that may obscure the view of the cervix. This usually results in using larger-sized specula with a condom or the cut- out finger from an exam glove around the blades to hold the walls back from collapsing, which can cause pain for the patient and may result in breakage of the plastic speculum.10 Second, patients with a cervix may have anatomic differences such as ante and retroversion or flexion (tipped uteri) present. This presents another challenge to the existing two- bladed speculum. This adds to both the patient’s and provider’s stress during the exam. The often-necessary repositioning of the speculum and the patient usually results in an extended, uncomfortable, and frustrating exam. Finally, the current 2-bladed speculum opens in a predominately vertical fashion, creating forces only in an anterior-posterior direction.11 This results in a wide dilation of the distal vagina with resultant pain and occasional breakage of the speculum. The speculum-free inserter was invented to self-screen for cervical cancer and pre-cancers. However, it does not allow for instrumentation or procedures of the cervix.6
The Bouquet Speculum, is FDA-Cleared and May Offer an Improvement to the Existing 2-Bladed Traditional Speculum
The Bouquet Speculum provides a novel design that will allow health-care providers to detect and subsequently treat cervical cancer and pre-cancers and perform other gynecologic procedures more efficiently and accurately while improving the patient experience. The Bouquet Speculum is a newly designed, 5-petaled, disposable, fully recyclable, plastic vaginal speculum that claims to overcome these limitations of the existing, traditional speculum. The 5-petals open as the dilator is advanced, and the ends of the petals lightly cup the cervix, ensuring that only the cervix is visualized, without vaginal wall collapse. The radial opening of this newly designed, 5-petaled speculum distributes the forces symmetrically and evenly, reducing the discomfort experienced by the vertical forces of the existing speculum. This may result in a more efficient and comfortable vaginal speculum exam (Figure 1).
 |
Figure 1 The Bouquet Speculum. |
Methods
Vaginal Phantom Model
A vaginal phantom model was designed and fabricated to simulate the female reproductive system’s uterus, fallopian tubes, ovaries, cervix, and vaginal wall opening (SynDaver Labs, Tampa, FL). The vaginal phantom is composed of a vaginal organ model placed in a plastic container with an opening on the side corresponding to the vaginal opening and suspended for testing. The uterus model is held by a supporting wire to simulate a natural biological system (Figure 2A). The plastic container was filled with ultrasonic gel at different heights to simulate different pressures (Figure 2B).
 |
Figure 2 Synthetic vaginal model in a sealed acrylic case (A) with the addition of gel to simulate intravaginal pressures (B). |
Pressure Evaluation
Different gel heights represent different pressures as given by the formula:
The speculum was inserted in a closed position and was opened once inside the phantom vaginal model to test that it would fully open (and remain open as needed) and withstand these pressures without failure (breaking/bending). Material failure, in this case, of a 3-D printed plastic prototype was tested using a von Mises nodal stress test. This test was repeated at increasing pressures to ensure that the breaking point of the speculum petals was above the known average vaginal wall pressures.12 Additionally, the von Mises nodal stress test images demonstrate radial force distribution across the speculum. It can be extrapolated that the forces within the vagina are similarly distributed (Figure 3).
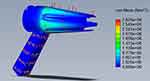 |
Figure 3 Pressure test-static nodal stress test. Stress applied = 18 cm H2O (1765 Pa) (maximum recorded vaginal pressure). |
Gynecological Tools Test
The speculum was inserted into the phantom vaginal model (closed, then opened), where an 8-inch cotton-tipped applicator was inserted into the speculum. The applicator was inserted inside the opened speculum and manipulated with different movements to ensure that it could efficiently perform regular gynecologic functions (ie, obtain a sample or access the cervical os and cervix for cancer and precancer treatments or for IUD insertion or insemination) (Figure 4).
 |
Figure 4 Gynecological tools test- retrieving samples and accessing the cervical os during gynecologic procedures and screening. |
Visibility Test
The visibility area of the cervix was observed by inserting the speculum in the phantom vaginal model in the same way as for the pressure test (closed, then opened), and a camera was placed at the opening of the speculum to take photos of the cervical region. The area was calculated from the percent visual area (PVA) given by:
This was also observed at different gel heights to quantify how the visibility varies with different pressures.
Results
The visibility test, using PVA, demonstrated better visualization of the cervix and the cervical os (sampling area for pap tests) with the Bouquet Speculum than the existing 2-bladed speculum at normal, heavy, and extreme pressures (Figure 5A–L).
Statistical analysis using an independent t-test showed that the mean PVA for the Bouquet Speculum was statistically higher (better) than the existing plastic 2-bladed speculum (p<0.05) at 4, 8, 12 and 18 cm/H20 pressure (Table 1).
 |
Table 1 Vaginal Phantom Visualization Test-Results |
The pressure test, using von Mises nodal stress test, demonstrated an equal radial distribution of force across the Bouquet Speculum without breakage or bending of the five petals at extreme simulated intrapelvic pressures of 18 cm/H2O (2.826e+06 N/m2 [von Mises]) (Figure 3). Further testing is needed in human subjects to determine if this translates to less discomfort during an exam.
The gynecologic tools test demonstrated that the Bouquet Speculum is compatible with the existing speculum and accommodates an 8” large cotton-tipped applicator for instrumentation (Figure 4). This was done using a pass/fail criterion over 10 consecutive trials. The test is considered satisfactory if all trials are successful. All trials demonstrated sample retrieval from cervical os. This demonstrates that the Bouquet Speculum is compatible with the existing speculum and standard gynecologic tools in terms of retrieving samples and accessing the cervix during gynecologic procedures and screening. Further testing is needed in human subjects to see if this translates to the efficacy of gynecologic tools in vivo.
Discussion
The Bouquet Speculum is an innovative redesign of the traditional 2-bladed speculum whose design has not changed in almost 2000 years. The redesign of the vaginal speculum was necessitated due to complaints about the limitations of the existing speculum and the barriers to care it created.
This in-vitro evaluation found that the novel 5-petaled Bouquet Speculum was better at visualizing the cervix than the existing 2-bladed speculum. Additionally, as the speculum was dilated within the phantom vaginal model at increasing vaginal pressures, the speculum remained intact without breakage, and the forces were evenly distributed around the five petals. Finally, the gynecologic tool compatibility test demonstrated that the Bouquet Speculum was able to accept and obtain samples from the cervical os with an 8” cotton-tipped, large applicator on 10/10 attempts.
Potential Benefits of This Innovation
The future scope of the project will focus on moving forward with the preferred mass manufacturing method (injection molding) and finding health-care providers interested in implementing this design nationally and internationally.13 The Bouquet Speculum has reached the international market with its first order in July 2023. A formal comparison of the Bouquet speculum versus the 2-bladed, traditional speculum has been completed with 100 patients in Pakistan. The results are promising in terms of visualizing the cervix, ease-of-use for the provider and less discomfort for the patient. Additional clinical studies are being discussed for Planned Parenthood in the United States.
Strengths and Limitations
The strength of this in-vitro study is the quantifiable and reproducible assessment of visualization of the cervix, pressures exerted across the speculum and ability to instrument the cervix in the phantom vaginal model. The limitations of this in-vitro study are the translatability to in-vivo assessments via subjective measurements (surveys) of the same variables. A recent clinical trial study was conducted in Pakistan in June 2023 with 100 patients and the preliminary data suggest statistical improvement in visualization of the cervix and ease-of-use with no statistical difference in comfort level for the patients.
Ethics Approval
Protocol #2022-098 - An Innovative Design for the Vaginal Speculum. Rocky Vista University IRB granted approval of the project as it is considered exempt from full IRB oversight because it does not involve interaction or intervention with human subjects.
Author Contributions
The authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public, commercial or nonprofit sector. However, the Bouquet Speculum was donated to the researchers by Viospex. The phantom vaginal model was purchased from SynDaver Labs and donated to the researchers by Cure Cervical Cancer, Inc. (CCC is a 501 (c)(3) non-profit). There is no award or grant number from CCC. The views presented in this paper are the author’s own and do not necessarily represent the official views of Viospex, SynDaver Labs, and Cure Cervical Cancer, Inc.
Disclosure
Dr. JM Bouquet is the owner and CEO of Viospex, the makers of the Bouquet Speculum. He designed, patented (US and Canadian patents), and FDA-cleared the Bouquet Speculum. He is also the President and Chairman of the Board of Cure Cervical Cancer, Inc. (CCC), a nonprofit that donates the Bouquet Speculum to low-resource countries to screen and treat cervical cancer clinics. The authors report no other conflicts of interest in this work.
References
1. Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R. Cancer of the cervix uteri: 2021 update. Int J Gynecol Obstet. 2021;155(Suppl 1):28–44. doi:10.1002/ijgo.13865
2. Hull R, Mbele M, Makhafola T, et al. Cervical cancer in low and middle-income countries. Oncol Lett. 2020;20(3):2058–2074. doi:10.3892/ol.2020.11754
3. Okunade KS. Human papillomavirus and cervical cancer. J Obstet Gynaecol. 2020;40(5):602–608. doi:10.1080/01443615.2019.1634030
4. Carneiro SR, Fagundes MA, Do Rosário PJO, et al. Five-year survival and associated factors in women treated for cervical cancer at a reference hospital in the Brazilian Amazon. PLoS One. 2017;12(11):e0187579. doi:10.1371/journal.pone.0187579
5. Seng LM, Rosman AN, Khan A, et al. Awareness of cervical cancer among women in Malaysia. Int J Health Sci. 2018;12(4):42–48.
6. Asiedu MN, Agudogo J, Krieger MS, et al. Design and preliminary analysis of a vaginal inserter for speculum-free cervical cancer screening. PLoS One. 2017;12(5):e0177782. doi:10.1371/journal.pone.0177782
7. Bates CK, Carroll N, Potter J. The challenging pelvic examination. J Gen Intern Med. 2011;26(6):651–657. doi:10.1007/s11606-010-1610-8
8. Clarke MA, Fetterman B, Cheung LC, et al. Epidemiologic evidence that excess body weight increases risk of cervical cancer by decreased detection of precancer. J Clin Oncol. 2018;36(12):1184–1191. doi:10.1200/JCO.2017.75.3442
9. Sandelowski M. This most dangerous instrument: propriety, power, and the vaginal speculum. J Obstet Gynecol Neonatal Nurs. 2000;29(1):73–82. doi:10.1111/j.1552-6909.2000.tb02759.x
10. Palsgaard P, Yerrabelli RS, Hojati A, Whitmore E. Using a condom or glove to improve pelvic exam visualization: a guide. SAGE Open Med. 2022;10:20503121221146069. PMID: 36568345; PMCID: PMC9772927. doi:10.1177/20503121221146069
11. Nadhif MH, Irsyad M, Ocviyanti D. Biomechanically compliant gynecologic training simulator. Simul Healthc. 2023;18(2):135–143. PMID: 35363667. doi:10.1097/SIH.0000000000000654
12. Egorov V, Murphy M, Lucente V, et al. Quantitative assessment and interpretation of vaginal conditions. Sex Med. 2018;6(1):39–48. doi:10.1016/j.esxm.2017.08.002
13. Bouquet JM, Chernau A, McLaughlin R, et al. A new vaginal speculum and an inexpensive kit to screen and treat dysplasia and cancer of the cervix. J Womens Health Care. 2019;8:470. doi:10.35248/2167-0420.19.8.470
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.