Back to Journals » Journal of Pain Research » Volume 10
An evaluation of two different methods of coccygectomy in patients with traumatic coccydynia
Authors Ogur HU, Seyfettinoğlu F, Tuhanioğlu Ü , Cicek H, Zohre S
Received 1 December 2016
Accepted for publication 9 March 2017
Published 12 April 2017 Volume 2017:10 Pages 881—886
DOI https://doi.org/10.2147/JPR.S129198
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Hasan Ulas Ogur, Firat Seyfettinoğlu, Ümit Tuhanioğlu, Hakan Cicek, Sefa Zohre
Department of Trauma and Orthopedics, Adana Numune Training and Research Hospital, Adana, Turkey
Purpose: The aim of this study was to evaluate the results of partial and total coccyx excisions in patients with traumatic coccydynia resistant to conservative treatment.
Patients and methods: The study included 22 patients (from a total of 27) who underwent partial or total coccygectomy because of persistent coccydynia between December 2007 and January 2014. There were 15 females and 7 males with a mean age of 33.6 years (range 23–46 years). Partial coccygectomy was performed in 14 patients and total coccygectomy in 8. They were evaluated according to their pre- and postoperative visual analog scale (VAS) scores. The mean follow-up period was 28 months (range 16–48 months).
Results: The mean VAS scores in the total excision group were 8.88±0.64 preoperatively and 2.5±2.67 at the final postoperative follow-up examination. In the partial excision group, these values were 8.79±0.89 preoperatively and 2.5±2.85 postoperatively. No statistically significant difference was determined between the two groups with respect to the mean scores (p>0.05). No rectum injury was seen in any patient. When the VAS scores of the patients were evaluated as a whole, excellent and good results were obtained in 78%. Patient satisfaction with the operation was 90%.
Conclusion: Coccyx excision is a successful treatment method in patients with long-term coccydynia who are resistant to conservative treatment. Two different surgical methods can be applied in the treatment and both of them have low complication rates and high patient satisfaction.
Keywords: partial excision, total excision, coccyx, visual analog scale
Introduction
Coccyx is the most distal part of the spine and is generally formed of four, and sometimes five, segments. Anatomically, there is a relationship with the fifth sacral and coccygeal nerve root and the terminal sympathetic plexus, and it is connected to the pelvic muscles. Pain occurring in the coccyx region is known as coccydynia or coccygodynia.1,2 The reason, in most cases, is trauma that is mostly associated with a fall onto the tailbone. Other reasons may be masses such as chordoma or intradural schwannoma, infections, or idiopathic pain of unknown origin, which could be owing to sacrococcygeal joint degeneration.3 In addition to trauma-related acute pain, there may be pain for a long time associated with nonunion of fracture. Sometimes, pain associated with lumbar stenosis and disk degeneration may be confused with coccydynia. Coccydynia is defined as pain that occurs in the coccyx at the moment of sitting or that occurs while sitting in the same position for a long period.3,4
The first stage of treatment comprises conservative modalities such as anti-inflammatory drugs, rest, seating support with a seating ring or a soft cushion, hot water baths, and local anesthetic or steroid injections.1–4 Following acute trauma, manipulation under anesthesia can be applied in addition to conservative methods. In the treatment of persistent coccydynia resistant to conservative treatment methods, successful results have been reported from coccygectomy.4–8 Although there are many reports in literature regarding the successful results of total coccygectomy in the surgical treatment of chronic coccydynia, the data on the clinical results of partial coccygectomy are limited.6–10 The aim of this study was to evaluate the results of partial and total coccygectomy for chronic coccydynia and to evaluate the efficacy of the two surgical methods.
Patients and methods
After obtaining approval from the Adana Numune Research and Educational Hospital institutional review board (IRB) (decision no: 21, dated February 24, 2017), the study included 22 patients (from a total of 27) who underwent partial or total coccygectomy because of persistent coccydynia between December 2007 and January 2014. Informed consent form was obtained from all patients. There were 15 females and 7 males with a mean age of 33.6 years (range 23–46 years). The indication of coccygectomy was defined as symptomatic coccydynia for at least 1 year and had been unresponsive to conservative treatments for at least 6 months. There was a history of trauma in the etiology of all the patients. In 2 patients, there was a history of suspected trauma, and for these 2 patients, differential diagnosis was made from magnetic resonance imaging (MRI). All patients were called for examination to obtain feedback. They were evaluated with respect to whether or not there were clinical complaints, sensitivity in the coccyx region, and duration of pain-free sitting. Radiological evaluation was made from anteroposterior and lateral coccyx radiographs. Pre- and postoperative pain levels were evaluated by using the visual analog scale (VAS) scores, where patients grade the pain from 0 to 10 (0 = no pain, 10 = intolerable pain). Those with complete pain relief were evaluated as very good (0–1 points), those with recovery of most of the pain and only a slight pain when sitting for long periods as good (2–3 points), those with a slight decrease in pain as moderate (4–6), and those with the same level of pain as preoperatively or a worsening of the pain level as poor (≥6 points) results. Finally, the patients were asked if they were satisfied with the result of the operation.
Conservative treatment was applied as intermittent anti-inflammatory therapy, a change in sitting habits for at least 6 months, the use of a soft cushion or a seating ring, hot water baths, and at least one application of combined local anesthetic and steroid injection (40 mg methylprednisolone acetate 20 mg/mL, 1 cc prilocaine HCl). The patients were classified according to the Postacchini and Massobrio classification.11 The distribution of the patients according to the type of operation and the Postacchini Massobrio groups is shown in Table 1. Partial coccygectomy was performed in 14 patients and total coccygectomy in 8. All the operations were performed by a single experienced surgeon (SZ). The mean follow-up period was 28 months (range 16–48 months).
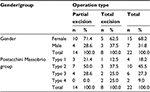  | Table 1 Distribution of patients according to gender, type of operation, and Postacchini Massobrio groups |
Surgical technique
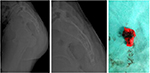
All the patients were operated under general anesthesia in the prone position. Preoperatively, antibiotic prophylaxis (2 g cefazolin Na intravenous [IV]) was administered to all patients. The gluteal regions were pulled laterally with adhesive drapes. In the patients undergoing partial excision, a longitudinal incision of ~3 cm was made in the coccyx midline, and the painful and hypermobile segment was excised from the soft tissue with the surgical technique described by Key.8,12 Following the excision of the painful, hypermobile segment, the operation was completed (Figures 1 and 2). A distance was maintained from the rectal sphincter. The integrity of the rectum was checked, and the layers were closed in the anatomic planes. In patients undergoing total excision, a 3–5 cm longitudinal incision was made in the same way and the Key surgical technique was applied.8,12 Briefly, by sharp dissection, the posterior surface of the coccyx is exposed as much as possible. If it is bent forward, the tip cannot be exposed until later. After the posterior surface of the coccyx has been well exposed, the posterior part of the intervertebral disk between the coccyx and the sacrum is cut with a knife. The ligaments between the inferior part of the sacrum and the first segment of the coccyx are then carefully cut away from the coccyx. After the lateral part of the first segment is freed, it is grasped with a towel clip and, by twisting it from side to side, the remaining attachments to the sacrum are put on tension and cut with a knife. The coccyx is then pulled gently backward – that is, in the direction tending to pull it out of the wound – and, by sharp dissection with a knife, the aponeurotic fibers are cut from its lateral borders, and the tissues are cut from its deep surface. The coccyx was elevated and held with a clothes-peg clamp. It was excised by dissection from the rectum and soft tissue in a craniocaudal direction (Figures 3 and 4). In the postoperative period, taking the healing period of soft tissue into consideration, it was recommended to use a seating cushion for 2 weeks. The antibiotic prophylaxis was continued for 48 hours. No special diet was applied postoperatively, but fiber-rich intake was recommended to prevent constipation.
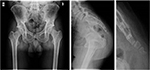  | Figure 1 Partial excision preoperative images. |
  | Figure 2 Partial excision postoperative images and excised coccygeal segment. |
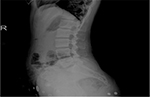  | Figure 3 Total excision preoperative view. |
  | Figure 4 Total excision postoperative view. |
The VAS scores of the patients were evaluated at 6 months, 12 months, and the final follow-up examination postoperatively. The degree of relief in the painful area compared to the preoperative values, how long the patient could sit before the onset of pain, and the level of pain relief in daily work and social life were evaluated.
Statistical analysis
The analysis of the study data was made with SPSS 20 software (IBM Corporation, Armonk, NY, USA). Conformity to normal distribution of unit numbers was assessed with the Shapiro–Wilk test. In the interpretation of the results, the significance level of 0.05 was used: a value of p<0.05 indicated that variables were not of normal distribution and p>0.05 indicated normal distribution of the variables. In the examination of differences between groups where the variables were not normally distributed, the Mann–Whitney U test was applied. The correlations between variables not of normal distribution were examined with Spearman’s correlation analysis. A value of p>0.05 was accepted as statistically significant.
Results
İn the total excision, the mean VAS scores group were 8.88±0.64 preoperatively, 3.2±2.13 at 6 months, and 2.5±2.67 at the 1 year and final postoperative follow-up examinations. In the partial excision group, these values were 8.79±0.89 preoperatively and 2.5±2.85 from 6 months onward postoperatively. No statistically significant difference was determined between the two groups with respect to the mean scores (p>0.005, Table 2).
In the partial excision group, excellent results were obtained in 9 patients, good in 2, moderate in 2, and poor in 1. The ratio of excellent and good results was 78.5%. In the total excision group, excellent results were obtained in 5 patients, good in 1, moderate in 1, and poor in 1. The ratio of excellent and good results was 75%. According to the Postacchini Massobrio classification, the 2 patients with moderate results in the partial excision group were Types 2 and 3 and the 1 patient with a poor result was Type 1. In the total excision group, the patient with a moderate result was Type 3 and the patient with a poor result was Type 2.
When all the patients were evaluated as a whole, a significant reduction was determined in the clinical complaints of 20 of the 22 patients. Excellent results were obtained in 14 patients, good in 3, moderate in 3, and poor in 2. Excellent and good results were seen in 17 (78%) patients. Excellent and good results were obtained in 11 of the 14 patients in the partial excision group and in 6 of the 8 patients in the total excision group (Table 3). When the patients were asked if they were satisfied with the result of the operation, a positive response was obtained from 20 (90%) of 22 patients.
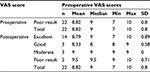  | Table 3 Preoperative VAS status of the pre- and postoperative VAS scores Abbreviations: VAS, visual analog scale; Min, minimum; Max, maximum; SD, standard deviation. |
No wound site infection was observed in the partial excision group. In 2 patients in the total excision group, superficial wound infection responded well to oral antibiotic therapy. No surgical debridement was necessary in any patient, and no rectum injury was seen in any case.
The mean operating time was 50±5.18 min (range 40–60 min) in the total excision group and 35±4.87 min (range 25–40 min) in the partial excision group (Table 4).
  | Table 4 Results of the Mann–Whitney U test related to the difference in gender and operation type with respect to operating time Abbreviations: Min, minimum; Max, maximum; SD, standard deviation. |
Discussion
Patients with coccydynia are often seen in daily orthopedic practice. These patients are usually treated conservatively, and in treatment-resistant patients or those who have been neglected, the pain can become chronic. Follow-up of conservative treatment is important in forming the first stage of treatment.10–14 However, patients suffering with chronic pain that is unresponsive to conservative treatment should be informed that surgical treatment provides pleasing results and increases comfort.6,7,14 As there is no completely objective evaluation system that can be used to evaluate the results of coccyx surgery, more subjective evaluation and the pain-focused VAS system have been used in previous studies.12,14–19 In this study, the VAS pain scoring system was used.
In literature, excellent and good results have been reported at rates of 60%–90% from coccygectomy because of chronic coccydynia.15–18 Capar et al14 reported 83.3% excellent and good results and Kerr et al9 reported 84.6%. Other studies have reported rates of 84%16 and >90%,15 with Cebesoy et al even reaching 100% success rate.8 In this study, using two different surgical techniques, excellent and good results were obtained in 78% according to the VAS scores and patient satisfaction was stated at the rate of 90%.
Coccygectomy can be applied as total or partial.2,5,7,9 Some research studies have stated that total coccygectomy is effective, that rates of dissatisfaction are higher in partial coccygectomy, and that these may require revision surgery.6–9,19 In a comparative study by Ramirei et al,2 failure rates were higher in cases applied with partial coccygectomy, and in another study, 3 patients with an unsuccessful result were all patients who had undergone partial coccygectomy.5 In another study, it was reported that good results obtained in patients with partial excision were associated with a high rate of sacrococcygeal fusion seen in some populations, and this was the reason for patient satisfaction. It was stated that in patients with intercoccygeal instability, if there is sacrococcygeal fusion, a good result can be obtained from partial excision.6
Sehirlioglu et al applied total or partial coccygectomy to a series of 74 patients because of traumatic coccydynia and although the revision rates were high in those applied with partial revision, it was recommended that both methods could be applied.5 In this study, there was no statistical difference with respect to patient satisfaction with the treatment between the patients applied with total and partial excision, and similar success rates were obtained. No revision was necessary in any patient applied with partial coccygectomy in this study.
In two different studies, the mean operating time for total coccygectomy was reported as 50 min, and a similar time was seen in the total excision group of this study.2,8 However, the mean operating time of the partial excision group was shorter. Although there was no difference between the two groups with respect to patient satisfaction, the operating time was shorter (mean 35 min) can be considered an advantage of partial excision.
In the differential diagnosis of traumatic coccydynia, evaluation with MRI may sometimes be necessary. Even if the coccyx appears normal, although taken in a supine position, MRI is useful in situations where the pain in the coccyx region could be due to bursitis, tumor, or disk pathologies.8 In this study, benefit was gained from MRI used in the differential diagnosis of 2 patients with a suspected trauma history.
The incision area in coccyx excision is accepted as a clean–contaminated wound.14,20 The use of prophylactic antibiotics is recommended to prevent surgical wound site infection. Previous studies have reported superficial wound site infection at rates of up to 20%.5,8 Wood and Mehbod compared two groups where prophylactic antibiotics were used and not used and reported that the antibiotic therapy reduced infection rates by 16%.20 Bayne et al17 reported infection rates of 16.6% and Pennekamp et al21 reported 19.6%. In this study, 2 g cefazolin Na IV was applied as prophylaxis for 48 hours. Superficial infection was seen in 2 patients. As these 2 patients were both applied with total excision, a larger incision was made, and they were exposed to a longer operating time. Although there was no statistically significant difference between these two operating techniques with respect to time, as there was an insufficient number of patients with superficial infection, no statistically significant correlation could be made between infection and the type of operation. In terms of making clear conclusions, the low number of cases can be accepted as a limitation of this study.
Conclusion
Consistent with the findings of previous studies in literature, successful results were obtained in this study from coccygectomy in the treatment of posttraumatic coccydynia unresponsive to conservative treatment. Thus, in patients with persistent coccydynia, it can be considered unnecessary to be too insistent on conservative treatment. Coccygectomy can be applied as total or partial with two different surgical methods. In this study, although there was no statistically significant difference between the 2 different surgical methods with respect to clinical results, both the shortness of the operating time and that it is a less invasive surgery, that is, partial coccygectomy can be considered as a surgical option with satisfactory results in patients with chronic coccydynia.
Disclosure
The authors report no conflicts of interest in this work.
References
Hanley EN, Ode G, Jackson Iii BJ, Seymour R. Coccygectomy for patients with chronic coccydynia: a prospective, observational study of 98 patients. Bone Joint J. 2016;98-B(4):526–533. | ||
Ramirei A, Domenicucci M, Cellocco P, Miscusi M, Costanzo G. Acute traumatic instability of the coccyx: results in 28 consecutive coccygectomies. Eur Spine J. 2013;22(Suppl 6):s939–s944. | ||
Ersen O, Ekinci S, Koca K, Akyildiz F, Bilgiç S. Coccygectomy as a surgical option in the treatment of chronic traumatic coccygodynia. Asian Spine J. 2015;9(3):492. | ||
Mouhsine E, Garofalo R, Chevalley F, et al. Posttraumatic coccygeal instability of the coccyx. Spine J. 2006;6(5):544–549. | ||
Sehirlioglu A, Ozturk C, Oguz E, Emre T, Bek D, Altinmakas M. Coccygectomy in the surgical treatment of traumatic coccygodynia. Injury. 2007;38(2):182–187. | ||
Hodges SD, Eck JC, Humpreys SC. A treatment and outcomes analysis of patients with coccydynia. Spine J. 2004;4(2):138–140. | ||
Bilgic S, Kurklu M, Yurttas Y, et al. Coccygectomy with or without periosteal resection. Int Orthop. 2010;34(4):537–541. | ||
Cebesoy O, Guclu B, Kose KC, Basarir K, Guner D, Us AK. Coccygectomy for coccygodynia: do we really have to wait? İnjury. 2007;38(10):1183–1188. | ||
Kerr EE, Benson D, Schrot RJ. Coccygectomy for chronic refractory coccygodynia: clinical case series and literature review. J Neurosurg Spine. 201;14(5):654–663. | ||
Haddad B, Prasad V, Khan W, Alam M, Tucker S. Favourable outcomes of coccygectomy for refractory coccygodyina. Ann R Coll Surg Engl. 2014;96(2):136–139. | ||
Postacchini F, Massobrio M. Idiopathic coccygodynia. Analysis of fifty-one operative cases and a radiographic study of the normal coccyx. J Bone Joint Surg Am. 1983;65(8):1116–1124. | ||
Key JA. Operative treatment of coccygodynia. J Bone Joint Surg Am. 1937;19(3):759–764. | ||
Maigne JY, Lagauche D, Doursounian L. Instability of the coccyx in coccydynia. J Bone Joint Surg (Br). 2000;82(7):1038–1041. | ||
Capar B, Akpinar N, Kutluay E, Müjde S, Turan A. Coccygectomy in patients with coccydynia. Acta Orthop Traumatol Turc. 2007;41(4):277–280. Turkish. | ||
Grosso NP, van Dam BE. Total coccygectomy for the relief of coccygodynia: a retrospective review. J Spinal Disord. 1995;8(4):328–330. | ||
Balain B, Eisenstein SM, Alo GO, et al. Coccygectomy for coccydynia: case series and review of literature. Spine. 2006;31(13):E414–E420. | ||
Bayne O, Bateman JE, Cameron HU. The influence of etiology on the results of coccygectomy. Clin Orthop Relat Res. 1984;190:266–272. | ||
Doursounian L, Maigne JY, Faure F, Chatellier G. Coccygectomy for instability of the coccyx. Int Orthop 2004;28(3):176–179. | ||
Hellberg S, Strange-Vognsen HH. Coccygodynia treated by resection of the coccyx. Acta Orthop Scand. 1990;61(5):463–465. | ||
Wood KB, Mehbod AA. Operative treatment for coccygodynia. J Spinal Disord Tech. 2004;17(6):511–515. | ||
Pennekamp PH, Kraft CN, Stütz A, Wallny T, Schmitt O, Diedrich O. Coccygectomy for coccygodynia: does pathogenesis matter? J Trauma. 2005;59(6):1414–1419. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

