Back to Journals » Therapeutics and Clinical Risk Management » Volume 18
An Evaluation of the Efficacy and Safety of Vibegron in the Treatment of Overactive Bladder
Authors Frankel J, Staskin D, Varano S, Kennelly MJ, Jankowich RA, Haag-Molkenteller C
Received 11 September 2021
Accepted for publication 13 February 2022
Published 3 March 2022 Volume 2022:18 Pages 171—182
DOI https://doi.org/10.2147/TCRM.S310371
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Garry Walsh
Jeffrey Frankel,1 David Staskin,2 Susann Varano,3 Michael J Kennelly,4 Rachael A Jankowich,5 Cornelia Haag-Molkenteller5
1Seattle Urology Research Center, Seattle, WA, USA; 2Tufts University School of Medicine, Boston, MA, USA; 3Clinical Research Consulting, Milford, CT, USA; 4Carolinas Medical Center, Charlotte, NC, USA; 5Urovant Sciences, Irvine, CA, USA
Correspondence: Jeffrey Frankel, PO Box 1192, Mercer Island, WA 98040, USA, Tel +1 206 972 2775, Email [email protected]
Abstract: Pharmacologic treatment for overactive bladder (OAB), which is characterized by bothersome symptoms such as urgency and urge urinary incontinence (UUI), includes anticholinergics and β3-adrenergic receptor agonists. Anticholinergics are associated with adverse effects including dry mouth, constipation, cognitive impairment, and increased risk of dementia. Therefore, the drug class of β3-adrenergic receptor agonists may represent an effective, safe treatment option. Vibegron, a β3-adrenergic receptor agonist, was approved for use in Japan (2018) and the United States (2020). Over the past 3 years, 2 phase 3 trials (EMPOWUR, EMPOWUR extension) have been conducted with once-daily vibegron 75 mg for the treatment of OAB, and additional secondary and subgroup analyses have detailed the efficacy and safety of vibegron. In the international phase 3 EMPOWUR trial, treatment with vibegron was associated with significant improvements compared with placebo in efficacy outcomes of micturition frequency, UUI episodes, urgency episodes, and volume voided as early as week 2 that were sustained throughout the 12-week trial. The 40-week EMPOWUR extension study, following the 12-week treatment period, demonstrated sustained efficacy in patients receiving vibegron for 52 weeks. Treatment with vibegron was also associated with improvements in patient-reported measures of quality of life. Across studies, vibegron was generally safe and well tolerated. A separate, dedicated ambulatory blood pressure monitoring study showed that treatment with vibegron was not associated with clinically meaningful effects on blood pressure or heart rate. Across all studies, vibegron was efficacious, safe, and well tolerated and thus represents a valuable treatment option for patients with OAB. Here, nearly 1 year after US approval, we review the published data on efficacy and safety of vibegron 75 mg for the treatment of OAB.
Keywords: adrenergic agonist, β-adrenergic receptor, urinary bladder overactive, urinary incontinence, vibegron
Plain Language Summary
Millions of adults worldwide have symptoms of overactive bladder. Overactive bladder can make a person feel like they need to urinate immediately and may be hard to control. Treatment for overactive bladder can include bladder training, but some patients take medication to help with their symptoms. Many medications exist, but some may cause side effects like dry mouth and constipation. Vibegron is a newer medication that works differently than older medications. In this review article, we discuss how well vibegron helped improve symptoms in clinical trials for patients with overactive bladder. Patients who took vibegron, including those over 65 years old, showed more improvement in their symptoms compared with patients who were given placebo (a pill with no medicine in it). Patients who took vibegron also had improved quality of life compared with patients who took a placebo. These studies showed that vibegron works well, is safe, and may be able to help patients who have overactive bladder manage their symptoms better.
Introduction
Overactive bladder (OAB) is prevalent in an estimated 550 million individuals worldwide1 and is characterized by bothersome symptoms such as urgency with or without urge urinary incontinence (UUI).2,3 OAB affects both men and women, and prevalence increases with age;4 however, symptoms such as UUI may disproportionately affect women.5 Patients with OAB experience the urge to urinate, associated with stretching of the detrusor muscle, at a low bladder volume.6 The etiology of OAB is not fully understood, and the major cause may vary between patients. Models explaining the pathophysiology of OAB have been reviewed elsewhere.6
Behavioral therapy with or without oral pharmacologic therapies are first-line treatments for reducing the symptom burden associated with OAB.5 Second-line treatment includes oral pharmacologic agents,5 such as anticholinergics and β3-adrenergic receptor agonists mirabegron and vibegron. However, anticholinergics are associated with adverse effects including cognitive impairment and increased risk of dementia.7,8 In addition, anticholinergic side effects such as dry mouth and constipation may limit treatment persistence.9,10 These effects increase with increasing anticholinergic burden,8,11 which is frequently seen in older adults who may encounter polypharmacy.12 It has also been reported that incidence of anticholinergic-related side effects is numerically higher when an anticholinergic is administered concomitantly with a β3-adrenergic receptor agonist vs anticholinergic monotherapy.13–15 The emergence of β3-adrenergic receptor agonists for the treatment of OAB demonstrated efficacy with a safety profile that was associated with a low incidence of adverse effects.16,17
β1-, β2-, and β3-adrenergic receptors are structurally related G-protein coupled receptors with distinct expression patterns and functions.18 β3-adrenergic receptors are highly expressed in the urinary bladder and detrusor muscles; here, β3-adrenergic receptors account for 94% to 97% of β-adrenergic receptor mRNA.19,20 Activation of the β3-adrenergic receptor in the detrusor smooth muscle increases bladder capacity by relaxing the detrusor during bladder filling.19 However, β-adrenergic receptors (predominantly β1 and β2) are also expressed on cardiac tissue,21 potentiating concerns about off-target effects. Vibegron was intentionally pharmaceutically designed to be highly specific for the β3-adrenergic receptor.22,23 In cell-based assays, both vibegron and mirabegron were highly selective at β3-adrenergic receptors;24 however, vibegron showed no measurable β1 and low β2 activity compared with mirabegron, which showed measurable β1 and some β2 activity. Vibegron showed a higher maximum response at β3-adrenergic receptors compared with mirabegron (99.2% vs 80.4%, respectively).24 Additionally, vibegron does not inhibit cytochrome P450 (CYP) 2D6 or other major CYP isoenzymes25,26 and thus may be less likely to be subject to clinically relevant drug–drug interactions27 than other medications that are CYP2D6 inhibitors such as mirabegron.28,29
Vibegron received approval for the treatment of OAB in adults in Japan (BEOVA®) in September 2018 at a 50-mg dose and in the United States (GEMTESA®25) in December 2020 at a 75-mg dose. In the United States, vibegron 75 mg is available as a once-daily treatment and can be swallowed whole with water or crushed and mixed with applesauce.25 In its US label, vibegron is indicated for the treatment of OAB with symptoms of urge urinary incontinence, urgency, and urinary frequency.25 Here, we review the efficacy and safety of once-daily vibegron 75 mg for the treatment of OAB.
Overview of Completed Trials
The efficacy and safety of vibegron 75 mg has been investigated for use in treating OAB across a 12-week, international, phase 3, randomized, double-blind, controlled trial (EMPOWUR) and a 52-week phase 3, randomized, double-blind, controlled extension trial (EMPOWUR extension; Table 1).16,30 The cardiovascular safety of vibegron was additionally assessed in a dedicated 28-day phase 1 ambulatory blood pressure monitoring (ABPM) trial.31 The ABPM trial included only placebo as a comparator because the focus was on blood pressure and heart rate compared with placebo. EMPOWUR included both placebo and active control (tolterodine 4 mg extended release [ER]); because of ethical considerations, the EMPOWUR extension included only active control. Patients were women and men ≥18 years old in the EMPOWUR and EMPOWUR extension studies (age range, 18–93 years). To ensure the patient population in EMPOWUR was representative of the real-world population, enrollment of male patients was capped at 15%, and ≤25% of all patients could have OAB dry (without urinary incontinence at baseline). Women ultimately represented 85.2% of patients in EMPOWUR; 77.0% of all patients experienced OAB wet (with urinary incontinence at baseline), and 43.3% were ≥65 years old. In the extension study, 78.2% were women, and 46.5% of all patients were ≥65 years old. The EMPOWUR and EMPOWUR extension studies required participants to have a history of OAB for ≥3 months and, based on a patient voiding diary, an average of ≥8 micturitions per day, ≥1 UUI episode per day for OAB wet, and ≥3 urgency episodes per day for OAB dry. The phase 1 ABPM study included women (74.6%) and men (25.4%) 45 to 75 years old with OAB and did not require a voiding diary because the endpoints were focused on ambulatory blood pressure and not OAB symptoms. In the EMPOWUR study, efficacy assessments were measured as early as week 2. Subgroup, secondary, and post hoc analyses of the primary EMPOWUR study (Table 2) included assessment of patient-reported outcomes,32 age subgroups (≥65 years old and ≥75 years old),33 efficacy in patients with OAB dry (without urinary incontinence) vs OAB wet (with urinary incontinence),34 and efficacy and safety in women.35,36
 |
Table 1 Overview of Primary Vibegron Studies |
 |
Table 2 Overview of Secondary, Post Hoc, and Subgroup Analyses of EMPOWUR |
The pivotal, phase 3 EMPOWUR trial was a 12-week, double-blind, placebo- and active-controlled trial that assessed the efficacy and safety of vibegron in adult patients with OAB (NCT03492281).16 In EMPOWUR, the coprimary endpoints were change from baseline to week 12 in average daily number of micturitions and in average daily number of UUI episodes (patients with OAB wet only). Key secondary endpoints included change from baseline to week 12 in average daily number of urgency episodes, average daily volume voided per micturition, and the percentage of patients with OAB wet reporting ≥75% reduction in average daily number of UUI episodes. Safety was assessed through adverse event (AE) reporting.
In addition to the primary EMPOWUR analyses, publications arising from the EMPOWUR study include patient-reported quality of life (QoL) measures,32 efficacy and safety in older adults,33 efficacy in patients with OAB wet vs OAB dry,34 and efficacy and safety in women.36 Patient-reported QoL was assessed through the OAB-questionnaire (OAB-q), which included a health-related QoL (HRQL) score (consisting of subscales for coping, concern, sleep, and social interaction) and symptom bother score, as well as the patient global impression (PGI) of severity, control, frequency, leakage, and change.
Patients who completed the EMPOWUR trial could enroll in the EMPOWUR extension trial (NCT03583372).30 The EMPOWUR extension was a 40-week-long study to investigate the long-term efficacy and safety of vibegron. Patients who received vibegron or active control (tolterodine 4 mg ER) for 12 weeks in EMPOWUR continued with the same treatment for the next 40 weeks of the study; patients who received placebo in EMPOWUR were randomly assigned 1:1 to receive vibegron or active control. The primary endpoint was safety, assessed by AE reporting. Secondary endpoints included change from baseline at week 52 in average daily number of micturitions, UUI episodes, urgency episodes, and total urinary incontinence episodes.
ABPM is a sensitive method used to detect small changes in blood pressure (2–3 mmHg) and in heart rate and is an important aspect for drugs in development. The phase 1 ABPM study was conducted to compare the blood pressure and heart rate effect profile of once-daily vibegron 75 mg compared with placebo in patients with OAB.31 The primary endpoint in this study was change from baseline to day 28 in mean daytime (waking hours) ambulatory systolic blood pressure. Key secondary endpoints were change from baseline to day 28 in mean daytime ambulatory diastolic blood pressure and heart rate and in mean 24-hour ambulatory systolic blood pressure, diastolic blood pressure, and heart rate. In this trial, safety was assessed through AE reporting, laboratory assessments, and in-clinic vital signs.
Efficacy
Short-Term Efficacy
In EMPOWUR, statistically significant improvements from baseline were seen at week 12 with vibegron vs placebo for average daily number of micturitions (least squares [LS] mean, ‒1.8 vs ‒1.3, respectively; P<0.001; Figure 1) and UUI episodes (‒2.0 vs ‒1.4; P<0.0001).16 Additionally, statistically significant improvements were seen with vibegron compared with placebo in the average daily number of urgency episodes (‒2.7 vs ‒2.0), average volume voided per micturition (23.5 vs 2.2 mL), and percentage of patients achieving a ≥75% reduction in average daily number of UUI episodes (49.3% vs 32.8%; P<0.01, all). Statistically significant improvements in efficacy were seen with vibegron treatment as early as week 2 for all coprimary and evaluated key secondary endpoints (urgency episodes, volume voided, and percentage of patients experiencing a ≥75% reduction in average daily number of UUI episodes). A subgroup analysis in women showed reductions from baseline at week 12 in micturitions (‒1.9 vs ‒1.4), UUI episodes (‒2.1 vs ‒1.4), and urgency episodes (‒2.8 vs ‒1.9) with vibegron vs placebo that were comparable with the overall population.36
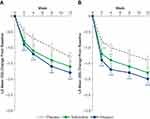 |
Figure 1 LS mean change from baseline in average daily number of (A) micturitions and (B) UUI episodes over 12 weeks. *P < 0.05. **P < 0.01. ***P < 0.001 vs placebo. Reprinted with permission from Wolters Kluwer Health, Inc.: Staskin D, Frankel J, Varano S, Shortino D, Jankowich R, Mudd PN, Jr. International phase III, randomized, double-blind, placebo and active controlled study to evaluate the safety and efficacy of vibegron in patients with symptoms of overactive bladder: EMPOWUR. J Urol. 2020;204(2):316–324. Available from: https://www.auajournals.org/doi/10.1097/JU.0000000000000807.16 Abbreviations: LS, least squares; UUI, urge urinary incontinence. |
The symptoms associated with OAB can cause significant emotional and psychological impact,37 and patient-reported outcomes represent an important way to assess improvement that may be more meaningful to patients. As part of the EMPOWUR trial, the OAB-q and PGI were used to assess QoL, and these results were presented in a subsequent publication.32 Treatment with vibegron was associated with significant improvements compared with placebo at week 12 in OAB-q HRQL total score (including coping, concern, and sleep subscales) and symptom bother score (P<0.01 each), as well as PGI measures of severity, control, frequency, leakage, and change (P<0.001 each). Greater proportions of patients receiving vibegron compared with placebo reported the best possible responses to individual PGI measures (responses ranged from much worse to much better; P<0.05 each).
As OAB prevalence increases with age,2 a subpopulation analysis of the phase 3 EMPOWUR trial specifically evaluated the efficacy and safety in adults ≥65 and ≥75 years old (Table 3). In the older adult population, treatment with vibegron was associated with significant reductions from baseline at week 12 vs placebo in average daily number of micturitions (LS mean: ≥65 years, ‒1.9 vs ‒1.0, respectively; ≥75 years, ‒2.1 vs ‒1.2; P<0.05 each), UUI episodes (≥65 years, ‒2.0 vs ‒1.2; ≥75 years, ‒2.0 vs ‒0.4; P<0.001 each), and urgency episodes (≥65 years, ‒2.7 vs ‒1.7; ≥75 years, ‒2.6 vs ‒0.9; P<0.01 each), suggesting that treatment with vibegron is efficacious in these populations. Significantly more patients ≥65 years old (population including those ≥75 years old) treated with vibegron vs placebo experienced ≥75% reduction in UUI episodes (P<0.0001) and a 50% reduction in urgency episodes (P<0.05).
 |
Table 3 Key Patient Baseline Demographics and Clinical Characteristics of Patients ≥65 Years Old (a Subpopulation Analysis from the EMPOWUR Trial) |
In a post hoc analysis of the efficacy of vibegron in patients with or without urinary incontinence at baseline, referred to as OAB wet vs OAB dry, respectively, treatment with vibegron was associated with significant reductions from baseline at week 12 compared with placebo in average daily urgency episodes (LS mean: wet, ‒3.0 vs ‒2.4, respectively; dry, ‒2.6 vs ‒1.6) and micturition frequency (wet, ‒2.1 vs ‒1.7; dry, ‒1.8 vs ‒1.0) in both populations (P<0.05 each). Significant reductions in urgency episodes were seen with vibegron vs placebo as early as week 2 and were maintained throughout the 12-week trial for the wet and dry populations (P<0.05 each).
Long-Term Efficacy
Continued treatment with vibegron 75 mg for an additional 40 weeks (52 weeks total) was associated with significant improvements from baseline compared with tolterodine in average daily number of UUI (LS mean, ‒2.2 vs ‒1.7, respectively; P<0.05; Figure 2) and total urinary incontinence episodes (‒2.5 vs ‒1.9; P<0.05; Figure 3).30 Additionally, sustained reductions from baseline were seen in average daily urgency episodes throughout the 52-week trial (Figure 3). In a post hoc analysis, patients who received placebo in EMPOWUR and vibegron in the extension study (40 weeks of treatment with vibegron) also experienced reductions from baseline in average daily number of micturitions, UUI episodes, urgency episodes, and total urinary incontinence episodes. In exploratory responder analyses, greater percentages of patients with OAB wet receiving vibegron for 52 weeks compared with tolterodine reported ≥50% reductions in total urinary incontinence episodes (71.1% vs 61.9%, respectively) and ≥75% reductions in UUI episodes (61.0% vs 54.4%). Additionally, a greater percentage of patients receiving vibegron (40.8%) compared with tolterodine (34.2%) experienced ≥100% reduction in UUI episodes (ie, were dry).
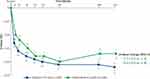 |
Figure 2 LS mean change from baseline in average daily number of UUI episodes over 52 weeks. *P < 0.05. Reprinted with permission from Wolters Kluwer Health, Inc.: Staskin D, Frankel J, Varano S, Shortino D, Jankowich R, Mudd PN, Jr. Once-daily vibegron 75 mg for overactive bladder: long-term safety and efficacy from a double-blind extension study of the international phase 3 trial (EMPOWUR). J Urol. 2021;205(5):1421–1429. Available from: https://www.auajournals.org/doi/10.1097/JU.0000000000001574.30 Abbreviations: LS, least squares; ER, extended release. |
 |
Figure 3 LS mean change from baseline in average daily number of (A) urgency episodes and (B) total urinary incontinence episodes over 52 weeks. *P < 0.05. Reprinted with permission from Wolters Kluwer Health, Inc.: Staskin D, Frankel J, Varano S, Shortino D, Jankowich R, Mudd PN, Jr. Once-daily vibegron 75 mg for overactive bladder: long-term safety and efficacy from a double-blind extension study of the international phase 3 trial (EMPOWUR). J Urol. 2021;205(5):1421–1429. Available from: https://www.auajournals.org/doi/10.1097/JU.0000000000001574.30 Abbreviations: LS, least squares; ER, extended release. |
Safety
Overall Safety and Tolerability
Vibegron was well tolerated in the clinical trials. The study completion rate was 90% after 12 weeks of treatment with vibegron in EMPOWUR. In the EMPOWUR extension study, both those continuing treatment with vibegron (52 weeks of treatment) and those switching from placebo to vibegron (40 weeks of treatment) had completion rates of 86%. Discontinuations due to AEs were low and comparable with placebo in the EMPOWUR study (1.7% with vibegron vs 1.1% with placebo) and were lower than tolterodine in the EMPOWUR extension study (1.5% with vibegron vs 3.4% with tolterodine). In the ABPM study, the rate of study completion was 97% for both vibegron and placebo.
Serious AEs occurred at rates comparable with placebo (1.5% vs 1.1% for vibegron vs placebo, respectively) in EMPOWUR and with tolterodine (3.3% vs 4.3% for vibegron vs tolterodine, respectively) in the EMPOWUR extension. In EMPOWUR, the most frequently occurring treatment-emergent AEs (TEAEs) with incidence greater with vibegron than placebo were headache and nasopharyngitis (Table 4). Incidence of hypertension was similar between vibegron and placebo treatment groups. In the EMPOWUR extension, the most common TEAEs with vibegron were hypertension (incidence similar to active control, tolterodine), UTI, and headache (Table 5). In the ABPM study, the most frequently occurring TEAEs with vibegron were hypertension, URTI, and headache. Drug hypersensitivity was reported as a TEAE in 2 patients (0.4%) receiving vibegron in EMPOWUR; no patients reported a TEAE of drug hypersensitivity in the EMPOWUR extension. In EMPOWUR and the EMPOWUR extension, rates of dry mouth, a commonly occurring anticholinergic-related AE, were lower with vibegron (1.7% and 1.8%, respectively) than with tolterodine (6.5% and 5.2%, respectively). The incidence of TEAE of urinary retention was infrequently observed in the 12-week EMPOWUR and 40-week EMPOWUR extension trials, occurring in 3 of 545 (2 men, 1 woman) and 3 of 273 (2 men, 1 woman) patients with vibegron, respectively. One man who experienced an AE of urinary retention reported the AE on the day he started the extension trial, and therefore the AE was included in both trials. In addition, no clinically meaningful changes in postvoid residual volume were observed with vibegron in the EMPOWUR or EMPOWUR extension studies. Urinary retention has been reported in patients taking vibegron, and the full prescribing information for vibegron includes a precaution to monitor for urinary retention, particularly in patients with bladder outlet obstructions and patients taking anticholinergic medications for OAB, who may be at greater risk for experiencing urinary retention.
 |
Table 4 Adverse Events by Treatment Group in the EMPOWUR Trial (Safety Analysis Set) |
 |
Table 5 Adverse Events by Treatment Group in the EMPOWUR Extension Trial (Safety Set Extension) |
In the EMPOWUR age subgroup analysis, the most common TEAEs occurring with vibegron at a rate greater than placebo for the ≥65-year-old subgroup were headache, dry mouth, and upper respiratory tract infection (URTI) and in the ≥75-year-old subgroup were UTI, URTI, diarrhea, and dyspnea. Similar to the overall safety results, rates of dry mouth in patients ≥65 years old were lower with vibegron (3.3%) compared with tolterodine (7.0%). In a post hoc analysis of safety in women, women receiving vibegron displayed a slightly higher incidence of headache, nasopharyngitis, and nausea compared with those receiving placebo; however, the overall incidence was consistent with the results of the EMPOWUR study.
There was 1 death reported in the EMPOWUR study in the tolterodine group (cerebrovascular accident; not considered treatment related by the investigator) and 1 death reported in the EMPOWUR extension study in the vibegron group (arteriosclerotic cardiovascular disease; not considered treatment related by the investigator). In the ABPM study, there were no deaths nor study treatment‒related serious TEAEs.
Cardiovascular Safety
In EMPOWUR, the rate of AEs of hypertension was low overall and comparable between groups (vibegron, 1.7%; placebo, 1.7%; tolterodine, 2.6%), and the rate of AEs of blood pressure increase was similarly low (vibegron, 0.7%; placebo, 0.9%; tolterodine, 1.9%). In the extension study, the rate of AEs of hypertension was similar between vibegron and tolterodine (8.8% vs 8.6%, respectively), and the rate of AEs of blood pressure increase were reported in 0.7% with vibegron and 1.7% with tolterodine. In EMPOWUR, atrial fibrillation occurred in 1 patient each from the placebo, vibegron, and tolterodine groups (all in patients ≥65 years old) and in the extension study was not observed with vibegron compared with 2 patients receiving tolterodine. Hypertension was the most commonly reported TEAE in the ABPM study, occurring in 5 of 106 (4.7%) patients in the vibegron group compared with 4 of 108 (3.7%) in the placebo group. One patient who experienced a TEAE of hypertension with vibegron was taking a prohibited medication known to increase blood pressure (phentermine). Furthermore, no events of hypertension with vibegron were considered related to study treatment.
In the dedicated ABPM study, the primary endpoint was change from baseline to day 28 in mean daytime systolic blood pressure. There was no statistically significant increase associated with vibegron treatment compared with placebo (LS mean, 0.82 vs 0.01 mmHg, respectively). The primary endpoint was evaluated against an upper bound of the 90% CI of 3.5 mmHg, and the actual upper bound was <2.5 mmHg, providing strong evidence that vibegron does not lead to clinically significant changes in blood pressure. Additionally, there were no statistically significant increases in mean daytime diastolic blood pressure (0.50 vs 0.55 mmHg) or heart rate (1.08 vs 0.19 bpm) after 28 days of treatment with vibegron compared with placebo. No significant differences were seen between vibegron and placebo for the mean changes from baseline in 24-hour systolic blood pressure (0.60 vs 0.03 mmHg), diastolic blood pressure (0.51 vs 0.70 mmHg), or heart rate (0.80 vs ‒0.15 bpm). The mean changes from baseline were similar in patients with or without pre-existing hypertension. In sum, treatment with once-daily vibegron 75 mg was not associated with clinically meaningful or statistically significant changes in blood pressure or heart rate.
Conclusion
Vibegron is the newest approved medication in the class of β3-adrenergic receptor agonists used to treat patients with OAB. In 2 phase 3 trials, once-daily vibegron 75 mg was associated with significant reductions in key symptoms of OAB. In 1 phase 1 28-day ABPM study, treatment with vibegron 75 mg was not associated with statistically significant or clinically meaningful effects on blood pressure or heart rate. Treatment with vibegron was overall safe and well tolerated in older adults, women, and patients with or without urinary incontinence. The safety profile of vibegron lacks some of the bothersome side effects associated with anticholinergics, suggesting that treatment with vibegron may lead to improvements in persistence. Improvements in patient-reported QoL measures suggest that vibegron achieves both objective measures of clinical efficacy and subjective measures of symptomatic improvement that may be perceived as more meaningful by patients. Improvements associated with treatment with vibegron seen in women were consistent with those observed in the overall population. Overall, older adults, regardless of sex or OAB type, tolerated vibegron well, suggesting the potential to successfully use vibegron for OAB across varying populations. These combined data suggest that vibegron is a valuable addition to the repertoire of treatments for OAB. Further investigation into the real-world effectiveness of vibegron is warranted based on the promising efficacy and safety data seen in clinical trials.
Acknowledgments
Medical writing and editorial support was provided by Wendy Kandell, PhD, and Krystina Neuman, PhD, CMPP, of The Curry Rockefeller Group, LLC (Tarrytown, NY), and was funded by Urovant Sciences, Inc. (Irvine, CA).
Disclosure
J Frankel is an investigator for Urovant Sciences, an investigator and speaker for Astellas Pharma and Pfizer Inc, and a speaker for Tolmar Inc. D Staskin is an investigator and consultant for Urovant Sciences; a consultant, investigator, and speaker for Astellas Pharma; and a consultant for New Uro B.V. S Varano is principal investigator for Clinical Research Consulting, holds academic positions at Sacred Heart University and University of Bridgeport, and is paid consultant and speaker for Urovant Sciences. M J Kennelly has received grant and/or research study funding from Allergan, Amphora, Astellas, Axonics, Boston Scientific, Coloplast, Cook Myosite, Dignify Therapeutics, EBT Medical, FemPulse, Ipsen, Taris, and Uro1 and is a consultant for Allergan, Astellas, Boston Scientific, Coloplast, Laborie, and Urovant Sciences. R A Jankowich was an employee of Urovant Sciences. C Haag-Molkenteller is an employee of Urovant Sciences. The authors report no other conflicts of interest in this work.
References
1. Irwin DE, Kopp ZS, Agatep B, Milsom I, Abrams P. Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int. 2011;108(7):1132–1138. doi:10.1111/j.1464-410X.2010.09993.x
2. Coyne KS, Sexton CC, Vats V, Thompson C, Kopp ZS, Milsom I. National community prevalence of overactive bladder in the United States stratified by sex and age. Urology. 2011;77(5):1081–1087. doi:10.1016/j.urology.2010.08.039
3. Coyne KS, Wein A, Nicholson S, Kvasz M, Chen CI, Milsom I. Comorbidities and personal burden of urgency urinary incontinence: a systematic review. Int J Clin Pract. 2013;67(10):1015–1033. doi:10.1111/ijcp.12164
4. Coyne KS, Sexton CC, Bell JA, et al. The prevalence of lower urinary tract symptoms (LUTS) and overactive bladder (OAB) by racial/ethnic group and age: results from OAB-POLL. Neurourol Urodyn. 2013;32(3):230–237. doi:10.1002/nau.22295
5. Gormley EA, Lightner DJ, Burgio KL, et al. Diagnosis and Treatment of Overactive Bladder (Non-Neurogenic) in Adults: AUA/SUFU Guideline. American Urological Association; 2019.
6. Leron E, Weintraub AY, Mastrolia SA, Schwarzman P. Overactive bladder syndrome: evaluation and management. Curr Urol. 2018;11(3):117–125. doi:10.1159/000447205
7. Ruxton K, Woodman RJ, Mangoni AA. Drugs with anticholinergic effects and cognitive impairment, falls and all-cause mortality in older adults: a systematic review and meta-analysis. Br J Clin Pharmacol. 2015;80(2):209–220. doi:10.1111/bcp.12617
8. Dmochowski RR, Thai S, Iglay K, et al. Increased risk of incident dementia following use of anticholinergic agents: a systematic literature review and meta-analysis. Neurourol Urodyn. 2021;40(1):28–37. doi:10.1002/nau.24536
9. Benner JS, Nichol MB, Rovner ES, et al. Patient-reported reasons for discontinuing overactive bladder medication. BJU Int. 2010;105(9):1276–1282. doi:10.1111/j.1464-410X.2009.09036.x
10. Yeowell G, Smith P, Nazir J, Hakimi Z, Siddiqui E, Fatoye F. Real-world persistence and adherence to oral antimuscarinics and mirabegron in patients with overactive bladder (OAB): a systematic literature review. BMJ Open. 2018;8(11):e021889. doi:10.1136/bmjopen-2018-021889
11. Tiisanoja A, Syrjälä AM, Komulainen K, et al. Anticholinergic burden and dry mouth among Finnish, community-dwelling older adults. Gerodontology. 2018;35(1):3–10. doi:10.1111/ger.12304
12. Ganz ML, Liu J, Zou KH, Bhagnani T, Luo X. Real-world characteristics of elderly patients with overactive bladder in the United States. Curr Med Res Opin. 2016;32(12):1997–2005. doi:10.1080/03007995.2016.1226167
13. Herschorn S, Chapple CR, Abrams P, et al. Efficacy and safety of combinations of mirabegron and solifenacin compared with monotherapy and placebo in patients with overactive bladder (SYNERGY study). BJU Int. 2017;120(4):562–575. doi:10.1111/bju.13882
14. Kelleher C, Hakimi Z, Zur R, et al. Efficacy and tolerability of mirabegron compared with antimuscarinic monotherapy or combination therapies for overactive bladder: a systematic review and network meta-analysis. Eur Urol. 2018;74(3):324–333. doi:10.1016/j.eururo.2018.03.020
15. Mitcheson HD, Samanta S, Muldowney K, et al. Vibegron (RVT-901/MK-4618/KRP-114V) administered once daily as monotherapy or concomitantly with tolterodine in patients with an overactive bladder: a multicenter, phase IIb, randomized, double-blind, controlled trial. Eur Urol. 2019;75(2):274–282. doi:10.1016/j.eururo.2018.10.006
16. Staskin D, Frankel J, Varano S, Shortino D, Jankowich R, Mudd PN
17. Herschorn S, Barkin J, Castro-Diaz D, et al. A phase III, randomized, double-blind, parallel-group, placebo-controlled, multicentre study to assess the efficacy and safety of the β3 adrenoceptor agonist, mirabegron, in patients with symptoms of overactive bladder. Urology. 2013;82(2):313–320. doi:10.1016/j.urology.2013.02.077
18. Schena G, Caplan MJ. Everything you always wanted to know about β(3)-AR * (* but were afraid to ask). Cells. 2019;8(4):357. doi:10.3390/cells8040357
19. Yamaguchi O. β3-adrenoceptors in human detrusor muscle. Urology. 2002;59(5 suppl 1):25–29. doi:10.1016/s0090-4295(01)01635-1
20. Nomiya M, Yamaguchi O. A quantitative analysis of mRNA expression of α1 and β-adrenoceptor subtypes and their functional roles in human normal and obstructed bladders. J Urol. 2003;170(2 Pt 1):649–653. doi:10.1097/01.ju.0000067621.62736.7c
21. Wachter SB, Gilbert EM. Beta-adrenergic receptors, from their discovery and characterization through their manipulation to beneficial clinical application. Cardiology. 2012;122(2):104–112. doi:10.1159/000339271
22. Lorca M, Morales-Verdejo C, Vasquez-Velasquez D, et al. Structure-activity relationships based on 3D-QSAR CoMFA/CoMSIA and design of aryloxypropanol-amine agonists with selectivity for the human β3-adrenergic receptor and anti-obesity and anti-diabetic profiles. Molecules. 2018;23(5):1191. doi:10.3390/molecules23051191
23. Edmondson SD, Zhu C, Kar NF, et al. Discovery of vibegron: a potent and selective β3 adrenergic receptor agonist for the treatment of overactive bladder. J Med Chem. 2016;59(2):609–623. doi:10.1021/acs.jmedchem.5b01372
24. Brucker BM, McHale K, King J, Mudd PN Selectivity and maximum response of vibegron and mirabegron for β3-adrenergic receptors.
25. Urovant Sciences, Inc. GEMTESA® (Vibegron). [Prescribing Information]. Irvine, CA; 2020.
26. Rutman MP, King JR, Bennett N, Ankrom W, Mudd PN. Once-daily vibegron, a novel oral β3 agonist, does not inhibit CYP2D6, a common pathway for drug metabolism in patients on OAB medications. J Urol. 2019;201:e231.
27. Rutman MP, Horn JR, Newman DK, Stefanacci RG. Overactive bladder prescribing considerations: the role of polypharmacy, anticholinergic burden, and CYP2D6 drug‒drug interactions. Clin Drug Investig. 2021;41(4):293–302. doi:10.1007/s40261-021-01020-x
28. Takusagawa S, Miyashita A, Iwatsubo T, Usui T. In vitro inhibition and induction of human cytochrome P450 enzymes by mirabegron, a potent and selective beta3-adrenoceptor agonist. Xenobiotica. 2012;42(12):1187–1196. doi:10.3109/00498254.2012.700140
29. Krauwinkel W, Dickinson J, Schaddelee M, et al. The effect of mirabegron, a potent and selective β3-adrenoceptor agonist, on the pharmacokinetics of CYP2D6 substrates desipramine and metoprolol. Eur J Drug Metab Pharmacokinet. 2014;39(1):43–52. doi:10.1007/s13318-013-0133-1
30. Staskin D, Frankel J, Varano S, Shortino D, Jankowich R, Mudd PN
31. Weber M, White WB, King J, Walker A, Mudd PN, Haag-Molkenteller C. Effects of vibegron on ambulatory blood pressure in patients with overactive bladder: results from a double-blind study. Blood Pressure Monitoring. 2021;Epub ahead of print. doi:10.1097/MBP.0000000000000572
32. Frankel J, Varano S, Staskin D, Shortino D, Jankowich R, Mudd PN
33. Varano S, Staskin D, Frankel J, Shortino D, Jankowich R, Mudd PN
34. Staskin D, Frankel J, Varano S, et al. Vibegron for the treatment of patients with dry overactive bladder: a subgroup analysis from the EMPOWUR trial. J Urol. 2021;206(suppl 3):e1107-1108. doi:10.1097/JU.0000000000002103.15
35. Newman D, Varano S, Shortino D, Jankowich R, Mudd PN Jr. Efficacy and safety of vibegron for the treatment of overactive bladder in women: a subgroup analysis from the EMPOWUR trial. Female Pelvic Med Reconstr Surg. 2021;27(10S):S1-S129. doi:10.1097/SPV.0000000000001103
36. Varano S, Newman D, Shortino D, Jankowich R, Mudd PN Jr. Efficacy and safety of vibegron for the treatment of overactive bladder in women: a subgroup analysis from the EMPOWUR trial.
37. Milsom I, Kaplan SA, Coyne KS, Sexton CC, Kopp ZS. Effect of bothersome overactive bladder symptoms on health-related quality of life, anxiety, depression, and treatment seeking in the United States: results from EpiLUTS. Urology. 2012;80(1):90–96. doi:10.1016/j.urology.2012.04.004
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
