Back to Journals » Open Access Surgery » Volume 13
An Endoscopic Study on the Prevalence of Accessory Maxillary Sinus Ostium in Patients with Chronic Rhinosinusitis in Dar es Salaam, Tanzania
Authors Abraham ZS , Kahinga AA , Mapondella KB, Massawe ER, Ntunaguzi D
Received 28 May 2020
Accepted for publication 4 August 2020
Published 18 August 2020 Volume 2020:13 Pages 61—64
DOI https://doi.org/10.2147/OAS.S264176
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Luigi Bonavina
Zephania Saitabau Abraham,1 Aveline Aloyce Kahinga,2 Kassim Babu Mapondella,2 Enica Richard Massawe,2 Daudi Ntunaguzi2
1Department of Surgery, University of Dodoma, College of Health and Allied Sciences, Dodoma, Tanzania; 2Department of Otorhinolaryngology, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania
Correspondence: Zephania Saitabau Abraham Email [email protected]
Aim: We aimed to determine the prevalence of and characterize accessory maxillary sinus ostium (AMO) in patients with chronic rhinosinusitis at a private health facility which serves the largest number of patients seeking treatment under private practice in Tanzania’s largest city.
Introduction: Chronic rhinosinusitis is a common condition in otorhinolaryngology practice. It has been postulated in the available literature that accessory maxillary ostium may play a role in the development of chronic maxillary sinusitis. AMO has been frequently identified during routine nasal endoscopy. Its found in the medial wall of the maxillary sinus and located in the lateral wall of the nose. There is no study to date that has been conducted in Tanzania to characterize AMO in patients with chronic rhinosinusitis when seen at the clinic despite the growing use of endoscopy on an outpatient basis.
Methods: Fifty adult patients with symptoms of chronic rhinosinusitis attending the ENT clinic on an outpatient basis were selected and then computerized tomography scan of the nose and paranasal sinuses (CT scan PNS) was performed. Nasal endoscopy was done to all patients to determine the presence and location of AMO.
Results: Of all the 50 studied patients, CT scan PNS depicted positive signs of rhinosinusitis in 35 patients (70%). Upon nasal endoscopy of the 35 patients, AMO was found in 25 patients (71.4%). Of the 15 patients with no depicted CRS upon CT scan, AMO was found in 4 (26.7%) patients.
Conclusion: Nasal endoscopy provides additional evidence of obstruction of natural sinus ostia thus leading to chronic maxillary rhinosinusitis apart from CT PNS. Such observation is of importance to clinicians who are to execute management of these patients.
Keywords: endoscopic, accessory, maxillary, chronic, rhinosinusitis, Tanzania
Introduction
The maxillary sinus is also known as the Antrum of the Highmore and is the largest of the paranasal sinuses and the most commonly affected in sinusitis.1 Anatomical variations have been suggested to play a role in the pathogenesis of chronic rhinosinusitis.1–5
During evolution, Homo sapiens changed to an upright posture and the maxillary sinus ostium also got rotated to a higher position and the sinus lost the advantage of gravitational drainage. It has to depend upon the ciliary action and effective ventilation of the nasal cavity to clear the secretions.1
Mucociliary transport is directed through the natural ostium in the maxillary sinus, and the accessory ostium does not play a role in its physiologic drainage.4,6 On the contrary, drained mucus may enter into the maxillary sinus through the accessory ostium, and may play a role in the pathogenesis of chronic maxillary rhinosinusitis. This phenomenon has been known as “mucus recirculation”.1,4,6 This is why the presence of the accessory ostium may play a role in the pathogenesis of CRS.
Structures located on the lateral nasal wall, especially the nasal septum, turbinates, bulla ethmoidalis and the uncinate process, play an important role in directing the nasal airflow. During inspiration, the nasal airflow creates a negative pressure in the nasal cavity which helps in the sinus drainage.1 When there is a mucosal swelling, the cilia get paralysed, resulting in poor mucus clearance and mucus stasis in the sinus and secondary infection.2,5-9
Infection increases the mucosal swelling further and blocks the natural sinus ostium. A vicious cycle is formed and the pressure inside the maxillary sinus builds up, which leads to a rupture of the weaker membranous part of the medial wall, facilitating drainage, and an accessory maxillary ostium (AMO) is thus created.1,6 It has been compared to the perforation of the tympanic membrane in the case of acute otitis media.2 It is not clearly known whether accessory maxillary ostium (AMO) is acquired or is a congenital anatomical variation as a result of congenital dehiscence of the fontanelles.1–7,10,11
The objective of the study was to identify the presence of AMO during nasal endoscopy in patients with symptoms of chronic rhinosinusitis following CT scan of the nose and paranasal sinuses (CT scan PNS).
Methods
The study was conducted in the outpatient clinic at the Department of Otorhinolaryngology of Ekenywa Specialised Hospital from January to December 2019. Fifty adult patients aged between 18 and 69 years attending the clinic with symptoms suggestive of chronic rhinosinusitis such as nasal obstruction, nasal discharge, sneezing, headache and post nasal drip for more than 4 weeks were recruited.
Any patient under 18 years of age and all other patients with prior history of nasal trauma, nasal surgery or comorbid conditions like diabetes, hypertension or bleeding disorders were excluded from recruitment into the study.
Recruited patients, after giving a written informed consent, were subjected to nasal endoscopy under local anesthesia to identify the presence of any AMO since nasal endoscopy remains a routinely performed procedure for patients with rhinological complaints whenever attending our hospital. For the sake of thorough nasal endoscopy, local anaesthesia and decongestion of the nasal cavity was achieved by application of ephedrine (1%) nasal drops and waiting for about 5–10 minutes to achieve maximum decongestion prior to nasal endoscopy using 0 and 30 degrees’ rigid scopes attached to a camera and monitor. The classical triple pass nasal endoscopy was done before all 50 patients were sent for CT scan PNS and various abnormal findings like septal deviations, septal spurs, septal perforations, concha bullosa, nasal polyps and anomalies of the uncinated process such as rotated uncinated process, presence of any accessory ostia at the uncinated process, and anomalies of bulla ethmoidalis or middle turbinate, for example paradoxical middle turbinate, were clearly documented. The presence of AMO, location, numbers and presence of any discharge through the AMO were carefully documented. The re-circulation phenomenon was observed endoscopically at the clinic. Appropriate medical or surgical treatments were advised and carried out for some of these patients. Patients were divided into cases and controls, where cases were those with AMO and controls were those without AMO, and the incidence of CRS was compared in both groups. Data were then analyzed using SPSS version 21.
Ethical approval to conduct the study was received from the Ekenywa Specialized Hospital Research Ethics Committee and written informed consent obtained from participants’ parents/legal guardians prior to recruitment into the study, with adherence to the Declaration of Helsinki.
Results
Age and Sex Distribution of Patients with Chronic Rhinosinusitis (n=50)
In this study, the majority were males (32, 64%) while females attributed 18 (36%) of all the study participants. The male to female ratio was found to be 1.7:1 (Table 1).
 |
Table 1 Age and Sex Distribution of Patients with Chronic Rhinosinusitis (n=50) |
Symptoms of Patients with Chronic Rhinosinusitis (n=50)
The most common presenting symptoms in this study were postnasal drip (96%), nasal discharge (96%), headache (94%), facial pain (80%) and nasal obstruction (76%), whereas sneezing was the least reported symptom (30%) (Table 2).
 |
Table 2 Symptoms of Patients with Chronic Rhinosinusitis (n=50) |
Age Distribution of Patients with Accessory Maxillary Ostium (n=25)
AMO was identified during nasal endoscopy in a total of 25 patients (71.4%) among those 35 patients with chronic rhinosinusitis depicted by CT scan PNS. Of those 25 patients with AMO, the majority were males 17 (68%) while females accounted for 8 (32%) of the cases (Table 3).
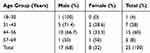 |
Table 3 Age Distribution of Patients with Accessory Maxillary Ostium (n=25) |
Lateralization of the Accessory Maxillary Ostium (n=25)
AMO was found unilaterally in 19 (76%) patients while bilaterally was found in 6 (24%) of patients. Males predominated in both unilaterality (68.4%) and bilaterality (66.7%) (Table 4).
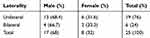 |
Table 4 Lateralization of the Accessory Maxillary Ostium (n=25) |
Location of AMO in Relation to Fontanelle
In this study, we found AMO to be located mostly in the posterior fontanelle (16, 64%) while the anterior fontanelle had AMO in 9 (36%) patients. Five patients had bilateral AMOs located in the posterior fontanelle on one side and the anterior fontanelle on the other side. Three patients had bilateral AMOs and were all located on the posterior fontanelle on either side.
Significance of AMO in the Non-CRS and CRS Groups
The p-value for the association between AMO in the non-CRS and CRS groups is less than 0.001 and thus statistically significant, thus supporting the role of AMO in the pathogenesis of CRS.
Discussion
Chronic rhinosinusitis is a commonly encountered disease in otorhinolaryngology practice. Accessory maxillary ostium has been postulated to be one of the commonest causes of chronic maxillary sinusitis due to recirculation of mucus between the natural ostium and AMO. There may be a vicious circle between chronic sinusitis and AMO. Mucus recirculation from AMO may lead to chronic sinusitis, and chronic sinusitis may promote the formation of AMO.1,4,6-8 Despite being the commonest cause, it has been understudied in otorhinolaryngology practice. It is not clearly known whether AMO is congenital or acquired. Some authors suggest that AMO develops congenitally due to a closure defect of the maxillary sinus fontanelles. Some others claim that it develops after recurrent infections due to perforation of the fontanelles. Recurrent episodes of infections may perforate the weak fontanelle membrane.1,4-7
There has been variability in terms of the prevalence of AMO in patients with chronic rhinosinusitis, where our study found a prevalence of 71.4%. Such a finding appears to correlate with what was found by Varadharajan et al and Sahin et al, where such prevalence was 62.5% and 14% respectively.1,6
In terms of bilaterality of AMO in patients with chronic rhinosinusitis, unilaterality (76%) was found to be predominant over bilaterality (24%). Such a finding appears to differ with what was found by Sahin et al, where bilaterality (68%) predominated over unilaterality (32%).6 In terms of the relationship of AMOs and fontanelles, AMO was located more on the posterior fontanelle (64%) than the anterior fontanelle (36%). This finding correlates with what was found in the same study by Sahin et al where the anterior fontanelle (0.61%) was least involved by AMO.6
Conclusion
Our study has revealed AMO to be quite prevalent in patients with chronic rhinosinusitis and thus supporting the vicious cycle between chronic rhinosinusitis and AMO. Although the study employed few cases, it yet has elucidated significant findings on the prevalence and bilaterality of AMO which has been understudied in the available literature. A mere identification of AMO at the clinic may aid otorhinolaryngologists in increasing their index of suspicion in diagnosing chronic rhinosinusitis and thus executing prompt expertise management even in the absence of imaging modalities like a CT scan.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Varadharajan R, Sahithya S, Venkatesan R, Gunasekaran A, Suresh S. An endoscopic study on the prevalence of the accessory maxillary ostium in chronic sinusitis patients. Int J Otorhinolaryngol Head Neck Surg. 2020;6(1):40–44.
2. Tiwari R, Goyal R. Study of anatomical variations on CT in chronic sinusitis. Indian J Otolaryngol Head Neck Surg. 2015;67(1):18–20. doi:10.1007/s12070-014-0734-2
3. Mahajan A, Mahajan A, Gupta K, Verma P. Anatomical variations of osteomatal complex: an endoscopic study. Anat Physiol Biochem Int J. 2018;5(2):555659.
4. Kane KJ. Recirculation of mucus as a cause of persistent sinusitis. Am J Rhinol. 1997;11(5):361–370. doi:10.2500/105065897781286034
5. Mahajan A, Mahajan A, Gupta K, Verma P, Lalit M. Anatomical variations of accessory maxillary sinus ostium: an endoscopic study. Int J Anat Res. 2017;5(1):3485–3490.
6. Sahin C, Ozcan M, Unal A. Relationship between development of accessory maxillary sinus and chronic sinusitis. Med J DY Patil Univ. 2015;8(5):606. doi:10.4103/0975-2870.164978
7. Yenigun A, Fazliogullari Z, Gun C, Uysal II, Nayman A, Karabulut AK. The effect of the presence of the accessory maxillary ostium on the maxillary sinus. Eur Arch Otorhinolaryngol. 2016;273(12):4315–4319. doi:10.1007/s00405-016-4129-8
8. Zhu JH, Lee HP, Lim KM, Gordon BR. Effect of accessory ostia on maxillary sinus ventilation: a computational fluid dynamics (CFD) study. Respir Physiol Neurobiol. 2012;183(2):91–99. doi:10.1016/j.resp.2012.06.026
9. Murthy DD, Rao BR, Rao SS. Analytical study of anatomical variations of nose and Pns in Ct scan and chronic sinusitis. IOSR J Dent Med Sci. 2016;15(7):30–35. doi:10.9790/0853-150713035
10. Ozel HE, Ozdogan F, Esen E, Genc MG, Genc S, Selcuk A. The association between septal deviation and the presence of a maxillary accessory ostium. Int Forum Allergy Rhinol. 2015;5(12):1177–1180. doi:10.1002/alr.21610
11. Aramani A, Karadi RN, Kumar S. A study of anatomical variations of osteomeatal complex in chronic rhinosinusitis patients-CT findings. J Clin Diagn Res. 2014;8(10):KC01. doi:10.7860/JCDR/2014/6788.3956
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
