Back to Journals » Clinical Ophthalmology » Volume 17
Agreement of Corneal Diameter and Anterior Chamber Depth Measurements with the IOLMaster 500 and the IOLMaster 700 Optical Biometers in Myopic Eyes
Authors Tañá-Rivero P, Tello-Elordi C, Orts-Vila P, Tañá-Sanz P, Tañá-Sanz S
Received 7 March 2023
Accepted for publication 21 April 2023
Published 29 April 2023 Volume 2023:17 Pages 1245—1253
DOI https://doi.org/10.2147/OPTH.S409132
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Pedro Tañá-Rivero, Cristina Tello-Elordi, Paz Orts-Vila, Pedro Tañá-Sanz, Santiago Tañá-Sanz
Cataract Department, Oftalvist Alicante, Alicante, Spain
Correspondence: Pedro Tañá-Rivero, Cataract Department, Oftalvist Alicante, C/ Angel Lozano n° 11, Alicante, 03001, Spain, Tel +34 965 141 500, Email [email protected]
Purpose: To assess the agreement in automated corneal diameter (CD) and anterior chamber depth (ACD, measured from corneal epithelium to lens) distances measurements between the IOLMaster 500 and 700 optical biometers in myopic eyes.
Methods: One hundred and sixteen eyes of 116 myopic patients aged between 21 to 60 years were included in this study. Measurements of CD and ACD distances were taken with each biometer for all patients in the same session. A t-test and a p-value less than 0.05 was considered statistically significant when the measurements were compared. The agreement between biometers was studied by applying a Bland–Altman analysis.
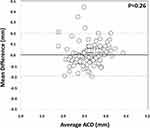
Results: The mean CD values obtained using the IOLMaster 500 and 700 biometers were 12.26± 0.35 mm and 12.13± 0.34 mm, respectively. The mean ACD distance values were 3.61± 0.29 mm and 3.62± 0.31, for the IOLMaster 500 and 700 biometers, respectively. There were statistically significant differences between the two devices only for CD measurements (p< 0.001), but not for ACD measurements (p=0.26). The limits of agreement obtained were wide in both types of measurements, being 0.422 mm for the CD distance and 0.389 mm for the ACD distance.
Conclusion: There were statistically significant differences between the IOLMaster 500 and 700 biometers regarding CD but not in ACD measurements in healthy myopic eyes. These differences could be clinically significant in some cases. According to these results, medical judgement should be used to assess whether the two devices could be used interchangeably for CD and ACD measurements during the clinical practice.
Keywords: anterior chamber depth, white-to-white, IOLMaster 500, IOLMaster 700, optical biometry
Introduction
The use of ocular biometry is necessary for cataract and refractive surgery planning, considering that it provides a measurement of several ocular parameters used in intraocular lens (IOL) calculations. Specifically, the measurement of corneal diameter (CD) and anterior chamber depth (ACD, measured from corneal epithelium to lens) distances has become increasingly important in cataract and refractive surgery, calculating phakic or pseudophakic IOL power and size. Different clinical studies have been published focusing on device interchangeability to measure CD or ACD distances. There are several techniques available for the measurement of CD and ACD distances based on manual techniques, for CD measurement (ie surgical calipers), and automated, for CD and ACD measurement (ie optical biometry).
Optical biometers are frequently used to measure CD and ACD distances in clinical practice. Two of the most popular optical biometers are the IOLMaster 500, that uses partial coherence interferometry (PCI), and the IOLMaster 700, that uses swept-source optical coherence tomography (SS-OCT), both from Carl Zeiss Meditec AG, Jena, Germany. There are some publications comparing these devices in different ocular populations/conditions, such as children, cataract, and healthy patients, but some of these studies show discrepancies in their findings and whether they can be used interchangeably during clinical practice.1–11 Mean differences between devices reported varied from −0.157 to 0.128 mm for CD and from −0.082 to 0.109 mm for ACD measurements. In addition to the mean differences, the limits of agreement (LoA) should be also considered to ascertain if the devices can be used interchangeably. Previous literature has reported CD LoA width varying from 0.47 mm8 up to 1.9 mm6 and ACD LoA width varying from 0.30 mm6 up to 1.00 mm.7 Then, considering the differences found in these previous clinical studies, we consider that a comparative study of the two devices in a large sample should be carried out. Specifically, we were interested to analyse possible differences in myopic eyes. The findings reported will provide clinicians with useful information in order to improve cataract and refractive surgery outcomes when they use these specific values to calculate IOL parameters.
Then, the objective of the present study was to assess the possible differences in automated CD and ACD measurements in myopic eyes between two common optical biometers used: the IOLMaster 500 and the IOLMaster 700. The LoA between the two devices were also obtained in order to ascertain if they can be used interchangeably clinically.
Methods
This single-centre observational study was conducted in accordance with the tenets of the Helsinki Declaration, approval from the Oftalvist Institutional Review Committee (01-2023) was received, and all patients provided written informed consent before they participated.
Patients and Procedure
The established inclusion criteria were healthy patients with age ranging from 21 to 60 years old and refractive error (spherical equivalent) ranging from −0.50 to −18.00 diopters (D). Refraction was measured using an automatic autorefractometer, and the assessment of corneal abnormality was done with the slit-lamp. CD and ACD distance measurements were obtained using both devices, but only right eyes were considered for the study due to the similarity of parameters between eyes.11 Both biometers were calibrated prior to each measurement session. The measurements were done in a single session.
Optical Biometers: IOLMaster 700 and 500
The IOLMaster 700 is based on SS-OCT technology with a scanning rate of 2000 scans/s. The scan provides the horizontal CD and ACD distances being measured with a light-emitting diode (LED) source of 800 nm. The IOLMaster 500 provides the CD distance using a LED light source and uses an image-based slit lamp system for ACD measurements.
Statistical Analysis and Sample Size
Excel software was used for data analysis (v. 2016, Microsoft Corporation, Redmond, WA, USA) and SPSS statistical software for statistical analysis (v. 24.0, IBM Corp., Armonk, NY, USA). Shapiro–Wilk test was employed to check the normality of the distribution, and the t-test was used to find possible statistically significant differences between the paired measurements taken using the 2 optical biometers (p value <0.05 was considered statistically significant). To evaluate the agreement between the biometers a Bland–Altman analysis was applied. We also determined the following values: average difference, confidence interval of the average difference at 95%, and the 95% LoA (being calculated as the mean difference ±1.96 standard deviation).
The sample size was calculated based on McAlinden et al11,12 for agreement studies. We considered a desired confidence interval for the LoA of 0.03 mm for the CD value as the primary outcome. This value is less than 0.1 mm, considered to be the limit of precision of commercially available calipers.13 Considering this value and the standard deviation of the differences obtained in a first examination of 30 patients, the sample size required for the agreement was 94.
Results
A total of 116 right eyes of 116 patients between 21 to 60 years were examined in this study. The mean spherical equivalent in our sample was −4.06±2.85D (mean ± standard deviation) (ranging from −0.50 D to −15.88 D), and the mean age was 37.54±11.79 years. All measurements were fully obtained in all patients using both optical biometers, and no complications were reported during the study.
The mean values obtained for the CD distance using the IOLMaster 700 and 500 optical biometers were 12.13±0.34 mm and 12.26±0.35 mm, respectively. The mean ACD values found for the two optical biometers were 3.62±0.31 mm and 3.61±0.29 mm, respectively. Table 1 shows the mean values with ranges for each parameter and optical biometer used. This table also shows the level of agreement between the two optical biometers, with the mean difference ± standard deviation, the 95% confidence interval, the 95% LoA, and the LoA range for the comparison between CD and ACD values obtained using the two optical biometers. Statistically signficant differences were obtained only for CD measurements when compared between the two devices (p<0.001) but not for ACD values (p=0.26). Figure 1 shows the Bland–Altman plot obtained for the comparison between the two optical biometers for the CD measurements. For the ACD measurement comparison, Figure 2 plots the Bland–Altman graph.
 |
Table 1 Mean ± Standard Deviation (Range) and Agreement Between the IOLMaster 700 and 500 for the Corneal Diameter Distance and Anterior Chamber Depth (Measured from Corneal Epithelium to Lens) |
Discussion
The purpose of our study was to ascertain the interchangeability of two optical biometers to provide CD and ACD measurements under clinical practice. CD and ACD distances are important parameters that are used, for instance, for phakic and pseudophakic IOL calculations during standard clinical procedures, so it is important to be sure that these parameters are obtained reliably and with proper accuracy in order to provide the best refractive outcome after any ocular surgery.
As stated earlier, different peer-reviewed clinical studies have been published showing the agreement between the IOLMaster 500 and 700 in children, cataract, and healthy patients. Table 2 shows those studies analysing both biometers, indicating the conditions of the sample. However, no studies have been done specifically in healthy myopic eyes in order to ascertain if the two devices are interchangeable in these eyes during clinical practice.
 |
Table 2 Published Studies Reporting Data on Corneal Diameter and Anterior Chamber Depth Agreement Between the IOLMaster 700 and the IOLMaster 500 Optical Biometers |
Corneal Diameter
Our results revealed that there were statistically significant differences between the two optical biometers when measuring CD distance (p<0.001). The mean difference between biometers was −0.133±0.108 mm, and the LoA ranged from −0.345 to 0.078 mm, giving a LoA width of 0.424 mm. We found a significant difference between devices: the IOLMaster 500 measured a longer CD distance than IOLMaster 700. Table 3 summarizes the outcomes reported by previous clinical studies on CD agreement. Our results broadly agree with them. Specifically, Srivannaboon et al1 in 100 cataract eyes found that the CD agreement for the two biometers was high with a mean difference of −0.101 mm (p=0.24, LoA width=0.75 mm). Similarly, Bullimore et al6 found in 51 cataract eyes a mean value of −0.0 mm (p=0.60, LoA width=0.60 mm) but also for 49 healthy eyes with a mean value of −0.1 mm (p=0.46, LoA width=1.90 mm). They concluded that the CD values were not different between biometers. In contrast, Yang et al7 in a sample of 146 cataract eyes of 83 patients reported statistically significant differences between biometers with a mean value of −0.150 mm (p<0.001, LoA width=1.19 mm). Huang et al8 in 109 cataract eyes of 109 patients found a mean value of 0.04 mm with a LoA width of 0.77 mm, and the Bland–Altman plots showed relatively low agreement. The mean differences for the whole sample of healthy children or adults were higher (0.09 and 0.12 mm, with LoA width ranging from 0.47 to 0.63 mm). Shi et al9 found that the difference between the two devices was statistically significant in a sample of 110 eyes of 110 children-adolescents; nevertheless, the Bland–Altman plot analysis indicated that the consistency of the two biometers for the CD distance measurement was good (LoA width=0.67 mm). Specifically, Jiang et al10 analysed a large sample of 518 cataract eyes of 391 patients as a function of the axial length and found that the two devices had a good agreement in measuring CD distance (except for values of axial length less than 22.00 mm and those values between 24.00 and 26.00 mm, which had a moderate agreement). Note that both biometers use the same technology using a light LED source to obtain CD measurement, but the limbus edge detection may vary among measurements; hence, this could be the source of the mean difference we have obtained. However, despite the statistically significant differences found, they were small. In addition, the LoA range (width) was less than half a millimetre (0.424 mm, Table 1), which could be considered clinically not meaningful. For IOL power, for example, when the Barrett and Holladay 2 formulas use CD, small differences may be expected and also to choose the size of a phakic IOL since surgeons consider it to the nearest 0.50 mm. Then, taking into account the small mean difference and LoA range obtained for CD distance values between the two biometers, we can be consider the two devices interchangeable for CD measurement in clinical practice. However, it should be noted that the LoA range is close to the 0.50 step of phakic IOL sizes.
 |
Table 3 Published Studies Reporting Data on Corneal Diameter Agreement Between the IOLMaster 700 and IOLMaster 500 Optical Biometers |
Anterior Chamber Depth
Our results revealed that there were no statistically significant differences between the two biometers when measuring ACD distance (p=0.26). The mean difference between the biometers was 0.005±0.099 mm, and the LoA varied from −0.190 to 0.200 mm, the LoA width being 0.390 mm. Table 4 summarizes the findings found in previous clinical studies on ACD agreement. Our results such as CD measurement previously discussed agree with them. Srivannaboon et al1 showed no statistically significant differences between the values obtained using the two biometers (mean difference of 0.04 mm, p=0.64, with a LoA width=0.44 mm). Akman et al2 in a sample of 188 cataractous eyes reported a statistically significant difference, but this difference is quite small for clinical relevance (−0.08 mm, p<0.001). They indicated that the IOLMaster 700 optical biometer correlated very highly with the 500 but noted that the 500 biometer did not measure in some eyes (n=13). This device analyses the image obtained by means of a slit-illumination system (optical section of the anterior chamber), and the 700 uses an image provided by the SS-OCT. Kunert et al3 in 120 cataractous eyes found a mean non-significant difference of 0.017 mm (p=0.151, LoA width=0.44 mm); Shajari et al4 in 79 cataract eyes and Lee et al5 in a large sample of 175 cataract eyes also showed a similar value without significant difference (0.017 mm and p=0.11, and 0.02 mm and p=0.06, respectively). Bullimore et al6 both in healthy and cataract eyes reported non-statistically significant differences between biometers with mean differences close to 0 mm (p>0.6). In contrast, Yang et al7 found that ACD did not correlate between biometers, being longer for the 500 device (mean difference of 0.065 mm with LoA width=1.004 mm, p=0.003). As previously indicated, the IOLMaster 700 measures ACD distance in the optical axis, but the IOLMaster 500 may not measure this axis since this biometer uses a lateral slit-beam technique. Huang et al8 for the whole sample analysed found a mean difference of 0.02 mm with a LoA of 0.39 mm. Shi et al9 found significant differences in 101 eyes of 101 children–adolescents, but it was within the acceptance range in clinical practice, and concluded that the differences can be ignored for a practical clinical application. Jiang et al,10 with the largest cataract sample assessed, showed a high agreement between biometers. They reported a statistically significant difference between devices, the 500 biometer measuring a longer ACD distance than the 700 biometer. However, they considered that based on the 95% confidence interval, the ACD distance measured by both biometers was of excellent reliability. In our sample the mean values obtained were similar between devices (3.62 mm versus 3.61 mm, mean difference 0.005 mm, see Table 1).
 |
Table 4 Published Studies Reporting Data on Anterior Chamber Depth Agreement Between the IOLMaster 700 and IOLMaster 500 Optical Biometers |
Similarly to our previous discussion with the CD values found, it should be noted that the mean difference we have obtained between the two biometers was small (0.005±0.099 mm) but the LoA range was about 0.4 mm. This value should be considered since it has been reported that a difference of 0.1 mm in the ACD distance would lead to a refraction change of 0.15 D for IOL power calculation in the eyes with an average corneal curvature and axial length,14 and 1 mm of ACD deviation could lead to a 1.5 D of refractive error in IOL power.15 In the worst-case scenario, considering our LoA range of 0.390 mm, this would lead to a 0.58 D refraction change, which should be considered. In addition, this LoA range cannot be assumed to be negligible when considering the safety distance in a patient to be implanted with a phakic IOL. It is necessary to point out that ACD values vary with accommodation and need to be carefully controlled when ACD is being measured. Surgeons should always keep in mind not only the mean difference obtained, but also the LoA between biometers. A clinical criterion should assess whether the two instruments could be used interchangeably for ACD measurement.
Nevertheless, our study has some limitations that should be considered. Our study only assessed myopic healthy patients, and healthy eyes with other refractive errors should be analysed. In addition, a large sample would be desirable in order to evaluate the effect of age among the values obtained. We hope to address these limitations in a future study.
In conclusion, from the results obtained in our study, medical judgement should be used to assess whether the IOLMaster 500 and 700 biometers could be used interchangeably for ACD and CD distances measurement during standard clinical practice in healthy myopic eyes.
Acknowledgments
The current research was supported by an investigator-sponsored study from STAAR Surgical AG.
Disclosure
Dr Pedro Tañá-Rivero reports grants from Staar Surgical, during the conduct of the study; grants from Alcon Labs, grants from AST Products Inc., Carl Zeiss Meditec, Heidelberg Engineering, Hoya, HumanOptics, Johnson&Johnson, and grants from BVI, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Srivannaboon S, Chirapapaisan C, Chonpimai P, et al. Clinical comparison of a new swept-source optical coherence tomography-based optical biometer and a time-domain optical coherence tomography-based optical biometer. J Cataract Refract Surg. 2015;41:2224–2232.
2. Akman A, Asena L, Güngör SG. Evaluation and comparison of the new swept source OCT-based IOLMaster 700 with the IOLMaster 500. Br J Ophthalmol. 2016;100(9):1201–1205. doi:10.1136/bjophthalmol-2015-307779
3. Kunert KS, Peter M, Blum M, et al. Repeatability and agreement in optical biometry of a new swept-source optical coherence tomography-based biometer versus partial coherence interferometry and optical low-coherence reflectometry. J Cataract Refract Surg. 2016;42(1):76–83. doi:10.1016/j.jcrs.2015.07.039
4. Shajari M, Cremonese C, Petermann K, Singh P, Müller M, Kohnen T. Comparison of axial length, corneal curvature, and anterior chamber depth measurements of 2 recently introduced devices to a known biometer. Am J Ophthalmol. 2017;178:58–64. doi:10.1016/j.ajo.2017.02.027
5. Lee HK, Kim MK. Comparison of a new swept-source optical biometer with a partial coherence interferometry. BMC Ophthalmol. 2018;18(1):269. doi:10.1186/s12886-018-0936-6
6. Bullimore MA, Slade S, Yoo P, Otani T. An evaluation of the IOLMaster 700. Eye Contact Lens. 2019;45(2):117–123. doi:10.1097/ICL.0000000000000552
7. Yang CM, Lim DH, Kim HJ, Chung TY, Grulkowski I. Comparison of two swept-source optical coherence tomography biometers and a partial coherence interferometer. PLoS One. 2019;14:e0223114. doi:10.1371/journal.pone.0223114
8. Huang J, Zhao Y, Savini G, et al. Reliability of a new swept-source optical coherence tomography biometer in healthy children, adults, and cataract patients. J Ophthalmol. 2020;2020:8946364. doi:10.1155/2020/8946364
9. Shi Q, Wang GY, Cheng YH, Pei C. Comparison of IOL-master 700 and IOL-master 500 biometers in ocular biological parameters of adolescents. Int J Ophthalmol. 2021;14(7):1013–1017. doi:10.18240/ijo.2021.07.08
10. Jiang J, Pan X, Zhou M, Wang X, Zhu H, Li D. A comparison of IOLMaster 500 and IOLMaster 700 in the measurement of ocular biometric parameters in cataract patients. Sci Rep. 2022;12(1):12770. doi:10.1038/s41598-022-16985-8
11. McAlinden C, Khadka J, Pesudovs K. Statistical methods for conducting agreement (comparison of clinical tests) and precision (repeatability or reproducibility) studies in optometry and ophthalmology. Ophthalmic Physiol Opt. 2011;31(4):330–338. doi:10.1111/j.1475-1313.2011.00851.x
12. McAlinden C, Khadka J, Pesudovs K. Precision (repeatability and reproducibility) studies and sample-size calculation. J Cataract Refract Surg. 2015;41(12):2598–2604. doi:10.1016/j.jcrs.2015.06.029
13. Mohamed A, Nankivil D, Pesala V, et al. The precision of ophthalmic biometry using calipers. Can J Ophthalmol. 2013;48(6):506–511. doi:10.1016/j.jcjo.2013.07.007
14. Norrby S. Sources of error in intraocular lens power calculation. J Cataract Refract Surg. 2008;34(3):368–376. doi:10.1016/j.jcrs.2007.10.031
15. Olsen T. Calculation of intraocular lens power: a review. Acta Ophthalmol Scand. 2007;85(5):472–485. doi:10.1111/j.1755-3768.2007.00879.x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.