Back to Journals » Clinical Ophthalmology » Volume 16
Age-Specific Outcomes of Conservative Approach and Probing for Congenital Nasolacrimal Duct Obstruction
Authors Lekskul A , Preechaharn P , Jongkhajornpong P , Wuthisiri W
Received 21 February 2022
Accepted for publication 17 May 2022
Published 7 June 2022 Volume 2022:16 Pages 1821—1828
DOI https://doi.org/10.2147/OPTH.S362680
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Apatsa Lekskul, Puncharut Preechaharn, Passara Jongkhajornpong, Wadakarn Wuthisiri
Department of Ophthalmology, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Wadakarn Wuthisiri, Department of Ophthalmology, Faculty of Medicine Ramathibodi Hospital, Mahidol University, 270 Rama 6 Road, Thung Phayathai Subdistrict, Ratchathewi District, Bangkok, 10400, Thailand, Tel +66 61 194 7887, Email [email protected]
Purpose: To evaluate the resolution rate of lacrimal sac massage and the efficacy of primary probing among different age groups of patients with CNLDO in Thai population.
Patients and Methods: Retrospectively reviewed the medical records of patients younger than 10 years of age who had been diagnosed with CNLDO, from January 1st, 2011, to October 31st, 2021. Patients were divided into two groups. The conservative treatment group comprised patients who had received Crigler’s maneuver and topical antibiotic when indicated; the intervention group comprised patients who had received probing.
Results: There were 469 patients in the conservative treatment group and 108 patients in the probing group. In the conservative treatment group; the patients were categorized into five groups according to age: 0 to < 6 months, 6 to < 12 months, 12 to < 18 months, 18 to < 24 months, and ≥ 24 months. The resolution rates for these age groups were 99.25%, 96.23%, 64.71%, 50%, and 62.07%, respectively. The rate of spontaneous resolution was significantly associated with patient age (p < 0.01). In the intervention group; the patients were categorized into four age groups according to age: 0 to < 12 months, 12 to < 24 months, 24 to < 36 months, and ≥ 36 months. The success rates of primary probing for these age groups were 92.86%, 89.29%, 85.71%, and 94.12%, respectively. The success rate of primary probing was not significantly associated with patient age (p > 0.05).
Conclusion: The Crigler’s maneuver is a safe and highly effective procedure for the management of CNLDO in patients of multiple ages, particularly patients less than 12 months of age. According to the high spontaneous resolution rate and the low rate of complications, the clinicians may delay surgical intervention when desired.
Keywords: CNLDO, Crigler maneuver, lacrimal sac massage, probing, repeat probing
Introduction
Congenital nasolacrimal duct obstruction (CNLDO) is a common cause of epiphora in infants; its prevalence rate of 5% to 20%,1,2 although only 2–6% of affected individuals will need intervention.3 The pathogenesis of CNLDO most commonly involves an imperforate membrane at the distal end of the nasolacrimal duct (the valve of Hasner). However, in some difficult cases, the pathogenesis may involve bony abnormalities and narrowing of the lacrimal drainage system.2 The clinical manifestations include epiphora, increased tear meniscus, the presence of mucopurulent discharge, and crusting of the lashes. The fluorescein dye disappearance test is used to confirm a diagnosis of CNLDO; its sensitivity and specificity are 100% and 85%, respectively.4
By 12 months of age, more than 90% of children respond to conservative treatment comprising lacrimal sac massage and topical antibiotic when indicated. Because CNLDO has a high rate of resolution, early intervention might be unnecessary.5–11 Resolution rates in the second year of life are not extensively characterized. Some authors have suggested that delayed treatment could increase the rate of intervention failure,13 perhaps because of prolonged inflammation and fibrosis in the lacrimal drainage system.3,5,6,14 However, some reports have found no age-related reductions in success rate.12,15,16 When conservative treatment does not lead to lacrimal duct opening, invasive procedures for CNLDO (eg, probing, balloon dacryocystoplasty, and silicone intubation) are recommended.8
Probing of the nasolacrimal duct has been advocated as a first-line treatment because it is a highly effective and uncomplicated surgical technique.8,12 However, the optimal timing for the probing procedure remains controversial. The success rate of early probing in children younger than 24 months of age reportedly ranges from 70% to 97%.3,6,12,17
Benefits of early probing intervention include the prevention of complications such as acute dacryocystitis, periorbital cellulitis, and inflammation around the ocular area; such intervention also helps children and caregivers to avoid the burden of CNLDO symptoms.16,18 However, to balance these benefits with the procedural and general anesthesia risks, as well as the high rate of spontaneous resolution in patients with uncomplicated cases, thorough discussions with caregivers are necessary.
To our knowledge, there is minimal information concerning CNLDO treatment outcomes in Thailand. Thus, we evaluated the resolution rate of lacrimal sac massage as conservative treatment for CNLDO; we also reported the efficacy of primary probing as a therapeutic intervention among different age groups of patients with CNLDO.
Materials and Methods
This study protocol was approved by the Institutional Review Board of the Faculty of Medicine, Ramathibodi Hospital, Mahidol University (approval No. MURA2021/965). The study was conducted in accordance with the tenets of the Declaration of Helsinki. We retrospectively reviewed the electronic medical records of patients younger than 10 years of age who had been diagnosed with CNLDO, at Ramathibodi Hospital, Mahidol University from January 1st, 2011, to October 31st, 2021. The review board waived the requirement for consent due to the retrospective nature of the study All the relevant data will not be disclosed to the public.
Patients
All enrolled patients exhibited CNLDO. The diagnosis was made based on a history of nasolacrimal duct obstruction symptoms prior to 6 months of age, as well as the presence of at least one sign of CNLDO (eg, epiphora, increased tear meniscus and mucopurulent discharge). The fluorescein dye disappearance test was used to confirm the diagnosis in patients with suspected CNLDO.
Patients were excluded if they had been diagnosed with tearing associated with other conditions (eg, eyelid malposition, primary congenital glaucoma, congenital fistula of the lacrimal sac, and any causes of ocular surface irritation), had undergone previous intervention for CNLDO, or had incomplete records. Demographic data were collected for all patients; these data included sex, age, comorbid diseases, duration of follow-up, epiphora laterality, dacryocystitis status, preseptal cellulitis status, orbital cellulitis status, and the timing and number of surgical interventions.
Patients were divided into two groups. The first group comprised patients who had received conservative treatment; the second group comprised patients who had received probing intervention. Patients in the conservative treatment group were recommended to perform 10 strokes of lacrimal sac compression by pressing the finger inward against the lacrimal sac at the medial canthus for 2–3 seconds, four times per day using the Crigler maneuver;19,21 they also received topical antibiotic treatment when there were evidences of mucopurulent discharge or conjunctivitis. Patients in probing group received treatment as described in the next section.
Surgical Procedure
Patients received surgical treatment from two surgeons (AL and WW); all probing procedures were performed with the patients under general anesthesia. The lower punctum was dilated using an appropriately sized punctum dilator. A McIntyre lacrimal cannula was vertically inserted in the lower punctum and advanced in the ampulla; it was then horizontally rotated into the lower canaliculus with lateral tension on the eyelid. When a hard stop was encountered, approximately 8–10 mm from the punctum, the exposed part of the probe was rotated 90 degrees until the probe became aligned parallel to the midline and above the patient’s brow, while maintaining contact between the probe and the lacrimal bone. Subsequently, the probe was advanced inferiorly and slightly posterolaterally through the nasolacrimal duct (approximately 20 mm). Concurrently, a suction tube was placed in the same nostril; passage of fluid in the draining suction tube was indicative of patency. We usually use the lower canaliculi of the affected eye in our probing procedure except there was some difficulty with the lower canaliculi then we used the upper canaliculi. Combined treatment comprising topical antibiotic with corticosteroid drops was administered for several days after probing. Parents were recommended to return for follow-up within 1 month after probing procedure.
Outcome Measurement
In the conservative treatment group, the primary outcome was the presence of spontaneous resolution among different age groups of patients with CNLDO. Spontaneous resolution was defined as the absence of symptoms and/or the absence of signs of CNLDO. Failure was defined as the presence of persistent symptoms and/or signs of CNLDO (eg, mucopurulent discharge and persistent epiphora) during the follow-up period or within 1 month after probing procedure. The secondary outcome in the conservative treatment group was the age at the time of spontaneous resolution.
In the intervention group, we reported the success rate of primary probing procedure in different age groups. Defining the success rate as the resolution of symptoms and/or signs of CNLDO after primary probing procedure.
For the patients with bilateral CNLDO; both eyes of the patients were enrolled to the study.
Statistical Analysis
Only one eye per patient was included into the analysis. In patients with bilateral CNLDO, the worst eye was selected. Continuous variables with non-normal distributions are shown as medians and interquartile ranges. Patients in each treatment group were divided into age-specific subgroups according to the age distribution of the data. The success rates in the conservative treatment and the intervention groups are shown as numbers with percentages. The chi-squared test and logistic regression analysis were used to compare successful outcomes among age groups. All results are shown with 95% confidence intervals and p-values. p <0.05 was considered to indicate statistical significance. All statistical analyses were performed using Stata software (version 16, StataCorp LLC, College Station, TX, USA).
Results
Electronic medical records were reviewed for 1222 patients; of these, 533 were eligible for inclusion in this study. There were 469 patients (255 boys and 214 girls) in the conservative treatment group. Forty-four patients (9.38%) did not respond to conservative treatment (range from 1 week to 40 months). They consequently received probing. There were 108 patients (51 boys and 57 girls) in the intervention group, which included both patients undergoing primary probing and patients who did not respond to conservative treatment (Figure 1). Sixty-four patients received initial probing due to various surgical indications such as their care giver refuse to perform Crigler maneuver or present at the age over one year.
 |
Figure 1 Study algorithms in treatment of CNLDO. |
In the conservative treatment group, the median age (interquartile range, min-max) of patients at presentation was 4 months (2–9 months, 1–50 months). Of 469 patients in the conservative treatment group, 425 (90.62%) had spontaneous resolution after conservative treatment. Patients were categorized into five groups according to age at presentation: 0 to <6 months, 6 to <12 months, 12 to <18 months, 18 to <24 months, and ≥24 months. The resolution rates for these age groups were 99.25%, 96.23%, 64.71%, 50%, and 62.07%, respectively (Figure 2). The rate of resolution was significantly associated with patient age (p < 0.001); it was not associated with patient sex (p = 0.261) or CNLDO laterality (p = 0.323). Patients in older age groups had significantly lower resolution rates than did patients aged 0 to <6 months (Table 1). The median resolution times for the five age groups, calculated from the beginning of treatment until the resolution of CNLDO, were 1.4 months (1–2.1 months), 3 months (1.8–4.2 months), 3.5 months (1.3–4.9 months), 1.8 months (1.3–3 months), and 2.8 months (1.6–3.9 months), respectively.
 |
Table 1 Results of Logistic Regression Analyses Assessing Factors Associated with the Success of Conservative Treatment in Patients with Congenital Nasolacrimal Duct Obstruction |
 |
Figure 2 Success rate of spontaneous resolution (%) among different age group. |
In the intervention group, the median patient age (interquartile range, min-max) was 19 months (13–30 months, 4–110 months). These patients were categorized into four age groups according to age: 0 to <12 months, 12 to <24 months, 24 to <36 months, and ≥36 months. The success rates of primary probing for these age groups were 92.86%, 89.29%, 85.71%, and 94.12%, respectively (Figure 3). The success rate of primary probing was not significantly associated with patient age (p > 0.05), patient sex (p = 0.862), and CNLDO laterality (p = 0.574) as shown in Table 2. The first probing procedure was successful in 99 patients (91.67%). Nine patients (8.33%) required another procedure because they did not respond to the first intervention. The interval time from first intervention to second intervention range from 4 weeks to 31 months. After the second probing procedure, patency was achieved in 8/9 patients (one patient in the 0 to <12 months group, six patients in the 12 to <24 months group, and one patient in the 24 to <36 months group); only one patient in the 24 to <36 months group required a third probing procedure.
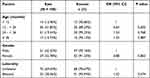 |
Table 2 Results of Logistic Regression Analyses Assessing Factors Associated with the Success of Primary Probing in Patients with Congenital Nasolacrimal Duct Obstruction |
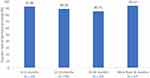 |
Figure 3 Success rate of probing (%) among different age group. |
Notably, acute dacryocystitis was presented in 0.37% of patients (2/533 patients), which were classified in the surgical intervention group.
Discussion
CNLDO is a common lacrimal system disorder in children. The management of CNLDO remains controversial. Resolution reportedly occurs in up to 90% of affected children by the age of 12 months.5–11,19,20 The Pediatric Eye Disease Investigator Group found that 66% of infants aged 6 to 10 months exhibit CNLDO resolution within 6 months of initiating nonsurgical treatment.21 Resolution rates in the second year of life have not been extensively reported. Sathiamoorthi et al reported that the rate of resolution was highest in the first few months of life, then declined until 9 months of age and was stable thereafter; the rate of resolution in patients aged 14 to 24 months ranged from 41.8% to 48.8%.5 Furthermore, Nakayama et al reported that resolution of CNLDO occurred after the age of 12 months in 45% of Japanese infants.22 In our study, we found that the rate of resolution depended on patient age; it was 96–99% during the first year of life, then dramatically decreased to 50%–64%, similar to the findings by Sathiamoorthi et al and Nakayama et al. Our patients aged 12 to <18 months, 18 to <24 months, and >24 months had significantly lower rates of resolution than did patients aged 0 to <6 months (p < 0.001). In the study by Sathiamoorthi et al, male patients exhibited faster resolution than did female patients; unilateral obstructions resolved faster than did bilateral obstructions.5 In another prospective study, the Pediatric Eye Disease Investigator Group reported that the probability of treatment success was lower in eyes of patients with bilateral disease.12 However, a subsequent study by the Pediatric Eye Disease Investigator Group reported no association of patient sex or obstruction laterality with resolution of CNLDO in patients aged 6 to 10 months.21 In our study, the rate of CNLDO resolution did not depend on patient sex (p = 0.261) or disease laterality (p = 0.325); however, our findings may not be broadly generalizable because this study included a smaller number of patients than did previous studies. Karti et al reported that the mean age of resolution was 6.8 ± 1.88 months among patients who regularly received effective lacrimal sac massage during the follow-up period.9 In our study, the median (interquartile range) resolution age of the conservative treatment group was 4 months (2–9 months) for patients of all ages, consistent with findings by Karti et al that the resolution of CNLDO tended to occur during the first year of life.
The optimal time for surgical treatment of CNLDO remains controversial. Because of the high efficacy of conservative treatment, multiple studies have suggested that probing should be delayed until patients reach the age of 12–15 months.5,11,13 The surgical interventions available for treatment of CNLDO include probing, balloon dacryocystoplasty, and silicone intubation.8 However, probing is generally the preferred primary intervention because of its simplicity and safety, as well as its high success rate.8,23,24 In previous studies, the success rate of probing intervention in patients less than 12 months of age ranged from 78% to 97%.12,25–27 In our study, the success rate of probing intervention among such patients was 92.86% (13/14 patients), similar to the previous findings. Among the 14 patients who underwent early probing in our study, two had dacryocystitis; for the remaining 12 patients, the caregivers refused to perform the Crigler maneuver. Moreover, we determined the success rates of primary probing in multiple age groups; these were 92.86%, 89.29%, 85.71%, and 94.12% in patients 0 to <12 months, 12 to <24 months, 24 to <36 months, and ≥36 months, respectively (Figure 2). These results contrasted with the findings in previous reports, which showed that the success rate of probing intervention decreased with age.25,28 However, the number of patients in each group was insufficient for our study to identify a significant relationship between age and the success rate of probing intervention. Such an investigation would explain the high success rate of primary probing among patients older than 36 months (94.12%; 16/17 patients). Nevertheless, this outcome may be insightful for clinicians who wish to perform probing as a primary surgical intervention for patients older than 36 months of age. Some studies also suggested that the success rate of probing intervention did not decrease in older children.15,16 The Pediatric Eye Disease Investigator Group did not find that probing success was associated with patient age between 6 and <36 months.12 Some authors have reported that the success rate of probing intervention did not significantly decrease until patients were at least 4 years of age.13,29,30 However, multiple studies have shown that patient age is correlated with the success of primary nasolacrimal duct probing.3,25,31 Furthermore, the success rate of primary probing intervention for CNLDO was significantly reduced when such treatment was performed in children aged ≥ 36 months.24,28 Finally, Kashkouli et al reported a significant reduction in the success rate of probing intervention after the age of 24 months.32 According to the success rate of probing decreased significantly after the 2 years of age in previous report,32 We recommend patients who was failed with conservative treatment underwent probing procedure by 1 year old and also patients in any age who frequently infection and dacryocystitis. In our result, the patients who underwent probing after 2 years old due to the late presentation of the patients to the hospital. These patients were immediate schedule for probing procedure. The high success rate of probing in patients older than 2 years old in our study confirm that even the patients older than 2 years old, the first intervention could be probing before considering complex intervention as silicone intubation and balloon dacryocystoplasty.
To our knowledge, there have been few studies concerning repeat probing in patients who did not respond to previous probing intervention. The success rate of repeat probing has ranged from 56% to 87%.2,3,6 Katowitz et al reported a 52% success rate for repeat probing (13/25 patients) among patients aged 6–18 months and an 18% success rate for repeat probing (3/17 patients) among patients aged 18–24 months.25 Additionally, Beato et al reported an 85.7% success rate for repeat probing (12/14 eyes), similar to the success rate of repeat probing in our study (88%) (8/9 patients). However, fewer patients underwent repeat probing in our study and the study by Beato et al, compared with the study by Katowitz et al.
The most common and concerning complication associated with CNLDO is acute dacryocystitis.18,33 Ffooks reported that the incidence of acute dacryocystitis as a complication of CNLDO was approximately 1.6% (7/440 patients).33 In our study, acute dacryocystitis was present in 1.8% of patients (2/108) in the intervention group; it was not present in the conservative treatment group. The low rates of complications was similar to Ffooks finding and might be related to the use of a topical antibiotic protocol.
This study had a few notable strengths. First, it included large numbers of Asian patients in both conservative treatment and intervention groups. Second, we reported the success rates in both groups among patients of various ages. Third, the study included patients who underwent treatment from two experienced pediatric ophthalmologists, using the same technique in a single surgical facility. Finally, we reported the success rate of repeat probing in patients who did not respond to primary probing.
There were also a few limitations in this study. First, it had a retrospective design. Second, because our institute is a tertiary referral hospital, most patients were referred from other hospitals. However, the findings in this study constitute hospital-based data that may not be representative of most patients with CNLDO. Third, each age group included a small number of patients (particularly the oldest patients in the intervention group), which hindered the statistical interpretation of the probing intervention success rate among age groups.
Conclusion
Our findings indicate that the Crigler maneuver is a safe and highly effective procedure for the management of CNLDO in patients of multiple ages, particularly patients less than 12 months of age; it might help such patients to avoid unnecessary anesthesia risks related to surgical intervention. We encourage the use of probing as the primary surgical intervention in patients with CNLDO, including patients older than 36 months of age especially in the naïve surgical treatment patients, because the operation has a very high success rate15,31 (16/17 patients, 94.12%). The incidences of serious complications such as acute dacryocystitis and preseptal cellulitis were very low because of the antibiotic protocol; this protocol provided the necessary support for clinicians to delay surgical intervention when desired.
Acknowledgment
We thank Ryan Chastain-Gross, Ph.D., from Edanz (https://www.edanz.com/ac) for editing a draft of this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sathiamoorthi S, Frank RD, Mohney BG. Incidence and clinical characteristics of congenital nasolacrimal duct obstruction. Br J Ophthalmol. 2019;103(4):527–529. doi:10.1136/bjophthalmol-2018-312074
2. Moscato EE, Kelly JP, Weiss A. Developmental anatomy of the nasolacrimal duct: implications for congenital obstruction. Ophthalmology. 2010;117(12):2430–2434. doi:10.1016/j.ophtha.2010.03.030
3. Swierczynska M, Tobiczyk E, Rodak P, Barchanowska D, Filipek E. Success rates of probing for congenital nasolacrimal duct obstruction at various ages. BMC Ophthalmol. 2020;20(1):403. doi:10.1186/s12886-020-01658-9
4. Kashkouli MB, Mirzajani H, Jamshidian-Tehrani M, Shahrzad S, Sanjari MS. Fluorescein dye disappearance test: a reliable test in assessment of success after dacryocystorhinostomy procedure. Ophthalmic Plast Reconstr Surg. 2015;31(4):296–299. doi:10.1097/IOP.0000000000000308
5. Sathiamoorthi S, Frank RD, Mohney BG. Spontaneous resolution and timing of intervention in congenital nasolacrimal duct obstruction. JAMA Ophthalmol. 2018;136(11):1281–1286. doi:10.1001/jamaophthalmol.2018.3841
6. Hung CH, Chen YC, Lin SL, Chen WL. Nasolacrimal duct probing under topical anesthesia for congenital nasolacrimal duct obstruction in Taiwan. Pediatr Neonatol. 2015;56(6):402–407. doi:10.1016/j.pedneo.2015.04.001
7. Lin AE, Chang YC, Lin MY, Tam KW, Shen YD. Comparison of treatment for congenital nasolacrimal duct obstruction: a systematic review and meta-analysis. Can J Ophthalmol. 2016;51(1):34–40. doi:10.1016/j.jcjo.2015.10.002
8. Vagge A, Ferro Desideri L, Nucci P, et al. Congenital nasolacrimal duct obstruction (CNLDO): a review. Diseases. 2018;6:96. doi:10.3390/diseases6040096
9. Karti O, Karahan E, Acan D, Kusbeci T. The natural process of congenital nasolacrimal duct obstruction and effect of lacrimal sac massage. Int Ophthalmol. 2016;36(6):845–849. doi:10.1007/s10792-016-0208-5
10. Young JD. Managing congenital lacrimal obstruction in general practice. BMJ. 1997;315:293–296.
11. Avram E. Insights in the treatment of congenital nasolacrimal duct obstruction. Rom J Ophthalmol. 2017;61(2):101–106. doi:10.22336/rjo.2017.19
12. Repka MX, Chandler DL, Beck RW, et al.; Pediatric Eye Disease Investigator Group. Primary treatment of nasolacrimal duct obstruction with probing. Ophthalmology. 2008;115(3):577–584.
13. el-Mansoury J, Calhoun JH, Nelson LB, Harley RD. Results of late probing for congenital nasolacrimal duct obstruction. Ophthalmology. 1986;93(8):1052–1054. doi:10.1016/s0161-6420(86)33621-2
14. Rajabi MT, Abrishami Y, Hosseini SS, Tabatabaee SZ, Rajabi MB, Hurwitz JJ. Success rate of late primary probing in congenital nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus. 2014;51(6):360–362. doi:10.3928/01913913-20140909-02
15. Eshragi B, Fard MA, Masomian B, Akbari M. Probing for congenital nasolacrimal duct obstruction in older children. Middle East Afr J Ophthalmol. 2013;20(4):349–352. doi:10.4103/0974-9233.120018
16. Ali MJ. Pediatric acute dacryocystitis. Ophthalmic Plast Reconstr Surg. 2015;31(5):341–347. doi:10.1097/IOP.0000000000000472
17. Beato J, Mota A, Goncalves N, et al. Factors predictive of success in probing for congenital nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus. 2017;54(2):123–127. doi:10.3928/01913913-20161013-02
18. Alaboudi A, Al-Shaikh O, Fatani D, Alsuhaibani AH. Acute dacryocystitis in pediatric patients and frequency of nasolacrimal duct patency. Orbit. 2021;40(1):18–23. doi:10.1080/01676830.2020.1717548
19. Bansal O, Bothra N, Sharma A, Walvekar P, Ali MJ. Congenital nasolacrimal duct obstruction update study (CUP study): paper I-role and outcomes of Crigler’s lacrimal sac compression. Eye. 2021;35(6):1600–1604. doi:10.1038/s41433-020-01125-1
20. Macewen CJ, Young JDH. Epiphora during the first year of life. Eye. 1991;5:596–600. doi:10.1038/eye.1991.103
21. Pediatric Eye Disease Investigator Group. Resolution of congenital nasolacrimal duct obstruction with nonsurgical management. Arch Ophthalmol. 2012;130(6):730–734. doi:10.1001/archophthalmol.2012.454
22. Nakayama T, Watanabe A, Rajak S, Yamanaka Y, Sotozono C. Congenital nasolacrimal duct obstruction continues trend for spontaneous resolution beyond first year of life. Br J Ophthalmol. 2020;104(8):1161–1163. doi:10.1136/bjophthalmol-2019-314980
23. Kashkouli MB, Karimi N, Khademi B. Surgical management of congenital nasolacrimal duct obstruction; one procedure for all versus all procedures for one. Curr Opin Ophthalmol. 2019;30(5):364–371. doi:10.1097/ICU.0000000000000584
24. Dhiman R, Chawla B, Chandra M, Bajaj MS, Pushker N. Clinical profile of the patients with pediatric epiphora in a tertiary eye care center. Indian J Ophthalmol. 2017;65(1):2–6. doi:10.4103/0301-4738.202306
25. Katowitz JA, Welsh MG. Timing of initial probing and irrigation in congenital nasolacrimal duct obstruction. Ophthalmology. 1987;94(6):698–705. doi:10.1016/s0161-6420(87)33392-5
26. Mannor GE, Rose GE, Frimpong-Ansah K, Ezra E. Factors affecting the success of nasolacrimal duct probing for congenital nasolacrimal duct obstruction. Am J Ophthalmol. 1999;127:616–617. doi:10.1016/S0002-9394(98)00432-2
27. Alakus MF, Dag U, Balsak S, et al. Is there an association between congenital nasolacrimal duct obstruction and cesarean delivery? Eur J Ophthalmol. 2020;30(6):1228–1231. doi:10.1177/1120672119889522
28. Arora S, Koushan K, Harvey JT. Success rates of primary probing for congenital nasolacrimal obstruction in children. J AAPOS. 2012;16(2):173–176. doi:10.1016/j.jaapos.2011.12.151
29. Kushner BJ, Rogers GL, Walson PD, Bremer DL, McGregor ML. The management of nasolacrimal duct obstruction in children between 18 months and 4 years old. J AAPOS. 1998;2:257–260. doi:10.1016/s1091-8531(98)90080-5
30. Robb RM. Success rates of nasolacrimal duct probing at time intervals after 1 year of age. Ophthalmology. 1998;105(7):1307–1310. doi:10.1016/s0161-6420(98)97038-5
31. Kashkouli MB, Kassaee A, Tabatabaee Z. Initial nasolacrimal duct probing in children under age 5: cure rate and factors affecting success. J AAPOS. 2002;6(6):360–363. doi:10.1067/mpa.2002.129041
32. Kashkouli MB. Late and very late initial probing for congenital nasolacrimal duct obstruction: what is the cause of failure? Br J Ophthalmol. 2003;87:1151–1153. doi:10.1136/bjo.87.9.1151
33. Ffooks OO. Lacrimal abscess in the newborn: a report of seven cases. Br J Ophthalmol. 1960;45:562.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
