Back to Journals » OncoTargets and Therapy » Volume 11
Afatinib versus gemcitabine/cisplatin for first-line treatment of Chinese patients with advanced non-small-cell lung cancer harboring EGFR mutations: subgroup analysis of the LUX-Lung 6 trial
Authors Wu YL , Xu CR , Hu CP, Feng J, Lu S , Huang Y, Li W, Hou M, Shi JH, Märten A, Fan J, Peil B, Zhou C
Received 21 December 2017
Accepted for publication 14 May 2018
Published 30 November 2018 Volume 2018:11 Pages 8575—8587
DOI https://doi.org/10.2147/OTT.S160358
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Geoffrey Pietersz
Video abstract presented by Yi-Long Wu.
Views: 331
Yi-Long Wu,1 Chong-Rui Xu,1 Cheng-Ping Hu,2 Jifeng Feng,3 Shun Lu,4 Yunchao Huang,5 Wei Li,6 Mei Hou,7 Jian Hua Shi,8 Angela Märten,9 Jean Fan,10 Barbara Peil,11 Caicun Zhou12
1Guangdong Lung Cancer Institute, Guangdong General Hospital and Guangdong Academy of Medical Sciences, Guangzhou, Guangdong, China; 2Department of Pulmonary Medicine, Xiangya Hospital, Central South University, Changsha, Hunan, China; 3Department of Internal Medicine, Jiangsu Provincial Tumor Hospital, Nanjing, Jiangsu, China; 4Shanghai Lung Cancer Center, Shanghai Chest Hospital, Shanghai Jiao Tong University, Shanghai, China; 5Department of Thoracic Surgery, Yunnan Tumor Hospital (The Third Affiliated Hospital of Kunming Medical University), Kunming, Yunnan, China; 6Department of Hematology & Oncology, Cancer Center, First Hospital of Jilin University, Changchun, Jilin, China; 7Lung Cancer Centre, West China Hospital, Sichuan University, Chengdu, Sichuan, China; 8Department of Oncology, Lin Yi Tumor Hospital, Linyi, Shandong, China; 9Department of Oncology, Boehringer Ingelheim GmbH, Ingelheim, Germany; 10Department of Oncology, Boehringer Ingelheim Pharmaceuticals, Inc., Ridgefield, CT, USA; 11Department of Oncology, Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim, Germany; 12Department of Medical Oncology, Shanghai Pulmonary Hospital, Yangpu District, Shanghai, China
Introduction: Non-small-cell lung cancer (NSCLC) is the leading cause of cancer death in China. Four epidermal growth factor receptor (EGFR)-targeted tyrosine kinase inhibitors – afatinib, erlotinib, icotinib, and gefitinib – are available for first-line treatment of NSCLC in China; however, there are few data to guide treatment choice. The Phase III LUX-Lung 6 trial compared afatinib with platinum-based chemotherapy for first-line treatment of patients from Southeast Asia with EGFR mutation-positive advanced NSCLC. This post hoc analysis assessed the findings from LUX-Lung 6 in Chinese patients.
Clinical trial registration: ClinicalTrials.gov: NCT01121393.
Materials and methods: Previously untreated patients with EGFR mutation-positive stage IIIB/IV lung adenocarcinoma were randomized 2:1 to receive afatinib or ≤6 cycles of gemcitabine/cisplatin. The key outcomes were progression-free survival (PFS; primary), objective response rate, disease control rate, overall survival (OS), duration of response and disease control, patient-reported outcomes, and safety. Three hundred and twenty-seven patients from mainland China were treated (89.8% of overall LUX-Lung 6 population; afatinib 217, gemcitabine/cisplatin 110).
Results: PFS was significantly longer with afatinib than gemcitabine/cisplatin (median 11.0 versus 5.6 months; hazard ratio [HR], 0.30 [95% CI, 0.21, 0.43]; P<0.0001). Overall, there was no significant difference in OS between treatment arms; however, in a subgroup analysis, afatinib significantly improved OS versus gemcitabine/cisplatin in patients with an EGFR Del19 mutation (median 31.6 versus 16.3 months; HR, 0.61 [95% CI, 0.41, 0.91]; P=0.0146). Afatinib was well tolerated, with most treatment-related adverse events (TRAEs) being of grade 1 or 2 severity. The most common grade 3/4 TRAEs with afatinib were rash/acne (15.9%/0.5%), stomatitis (6.1%/0%), and diarrhea (5.6%/0%). TRAEs leading to permanent discontinuation were reported in 12 patients (5.6%) receiving afatinib and 43 (41.7%) receiving gemcitabine/cisplatin. Afatinib significantly improved PFS compared with standard first-line chemotherapy in Chinese patients with EGFR mutation-positive NSCLC and demonstrated a manageable safety profile.
Conclusion: The findings support the rationale for using afatinib as a first-line treatment option for this patient population.
Keywords: afatinib, NSCLC, EGFR, first-line, Phase III, Chinese patients
Materials and methods
Patients and study design
The study design and eligibility criteria of LUX-Lung 6 (NCT01121393) have been published previously.12 In brief, LUX-Lung 6 was a randomized, open-label, Phase III study conducted in China, Thailand, and South Korea (Supplementary slides). Of the 36 centers participating in the study, 30 were in China. Eligible patients had pathologically confirmed previously untreated stage IIIB (with pleural effusion) or IV lung adenocarcinoma, an Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0 or 1, measurable disease according to Response Evaluation Criteria in Solid Tumors, version 1.1, and adequate organ function. In addition, tumor tissue had to be EGFR mutation-positive as assessed at a central laboratory using the Therascreen EGFR 29 kit (Qiagen, Manchester, UK). Eligible patients were randomly assigned to receive afatinib or gemcitabine/cisplatin in a 2:1 ratio, stratified by EGFR mutation (L858R, Del19, or other).
The study was conducted in accordance with the Declaration of Helsinki and guidelines on Good Clinical Practice, and the protocol was approved by local ethics committees at each participating center (Table S1). All patients provided written informed consent for trial participation.
Treatments
Patients received either oral afatinib (40 mg/day) or up to 6 cycles of cisplatin 75 mg/m2 on day 1 plus gemcitabine 1,000 mg/m2 on days 1 and 8 of a 21-day cycle. Patients continued treatment until disease progression, intolerable toxic effects, or withdrawal of consent. Patients receiving afatinib were permitted to dose escalate to 50 mg/day after the first 21-day cycle in the absence of grade >1 TRAEs. Afatinib was withheld for up to 14 days and then dose reduced by 10 mg decrements (minimum 20 mg/day) for treatment-related grade 3 or selected prolonged grade 2 AEs. Dose reductions or interruptions for patients receiving gemcitabine/cisplatin were in accordance with guidance provided in the current summaries of product characteristics. Patients who remained on afatinib treatment for ≥36 months were defined as long-term responders (LTRs).
Outcomes and assessments
The primary end point was PFS according to independent central review. Key secondary end points were ORR (complete response [CR] or partial response [PR]), disease control rate (DCR; CR, PR, or stable disease), OS, duration of response and disease control, patient-reported outcomes (PROs), and safety.
Tumor assessments were performed by computed tomography or magnetic resonance imaging every 6 weeks for the first 48 weeks and then every 12 weeks thereafter until disease progression or start of new anticancer therapy. Brain imaging and bone scans were performed if clinically indicated. Scans were reviewed by an independent central imaging review group consisting of radiologists and oncologists.
PROs were assessed at randomization and every 3 weeks thereafter until disease progression or start of new anticancer therapy using the self-administered cancer-specific European Organisation for Research and Treatment of Cancer quality of life core questionnaire QLQ-C30,24 and the lung cancer-specific module QLQ-LC13.25 Safety was monitored weekly, with incidence and intensity of AEs graded according to National Cancer Institute Common Terminology Criteria for Adverse Events version 3.0.
Pharmacokinetics
For patients randomized to the afatinib arm, blood sampling was performed to estimate the afatinib trough (predose) plasma concentrations at steady state. Plasma afatinib concentrations (free base) were analyzed using a validated high-performance liquid chromatography tandem mass spectrometry method at Boehringer Ingelheim Pharma GmbH & Co. KG, Drug Metabolism and Pharmacokinetics Germany, Biberach, Germany.
Statistical analyses
Kaplan–Meier estimates were used to construct survival curves and calculate median PFS and OS. A Cox proportional-hazard model was used to derive hazard ratios (HRs) and 95% confidence intervals (CIs); treatment groups were compared using a log-rank test. Prespecified subgroup analyses were conducted by sex, age (<65 years versus ≥65 years), EGFR mutation type (Del19 versus L858R versus other), ECOG PS (0 versus 1), and smoking history.
PROs focused on the NSCLC-related symptoms of cough (question 1 of QLQ-LC13), dyspnea (questions 3–5 of QLQ-LC13 and question 8 of QLQ-C30), and pain (questions 9 and 19 of QLQ-C30, and questions 10–12 of QLQ-LC13). The following analyses were undertaken: percentage of patients whose symptoms improved (≥10-point decrease from baseline score), remained stable, or deteriorated (≥10-point increase from baseline score); time to deterioration of symptoms; and mean difference in symptom scores over time (longitudinal analysis). Statistical analyses were performed using SAS (version 9.2 or later).
Results
Patients and baseline characteristics
Of the 364 patients randomized in LUX-Lung 6,327 (89.8%) were from mainland China. A total of 217 patients were randomized to afatinib; 110 patients were randomized to gemcitabine/cisplatin. Three patients in the afatinib group and seven in the gemcitabine/cisplatin group did not receive any treatment; thus, the treated sets comprised 214 and 103 patients, respectively.
There were no notable differences in baseline characteristics between the Chinese subgroup and the overall LUX-Lung 6 population (Table 1). Consistent with the overall LUX-Lung 6 population, there was a slightly higher proportion of males (37.3% versus 30.9%), slightly more patients with ECOG PS 1 (79.7% versus 63.6%), slightly more current or ex-smokers (23.0% versus 13.6%), and more patients with two metastatic sites (38.7% versus 27.3%) in the afatinib group compared to the gemcitabine/cisplatin group (Supplementary slides).
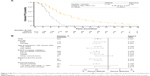
Treatment exposure
Median treatment duration with afatinib was 389.5 days (range 3–1, 256 days); 37 patients had their afatinib dose escalated to 50 mg/day. At the end of treatment, 141 patients (65.9%) had had no dose reductions, 59 (27.6%) had one dose reduction, and 14 (6.5%) had two dose reductions. The median time to first dose reduction with afatinib was 72 days and the median dose interruption before dose reduction was 6 days. Median duration of treatment on gemcitabine/cisplatin was 86 days (range 1–154 days). A total of 36 patients (38.7%) received all of their gemcitabine/cisplatin courses without interruption; 26 (28.0%) had a worst delay of 4–6 days and 31 (33.3%) had a worst delay of >6 days. At the time of analysis, there were 20 Chinese afatinib LTRs, with a median treatment duration of 56.8 months (range: 37.3–68.2 months); eight patients remained on treatment. Dose modifications among the LTRs are shown in Figure 1 and do not indicate an impact of dose adjustment on long-term responses (Supplementary slides).
  | Figure 1 Dose adjustments among Chinese patients who were LTRs to afatinib. |
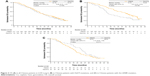
PFS
Independently assessed median PFS was 11.0 months with afatinib versus 5.6 months with gemcitabine/cisplatin (HR, 0.30 [95% CI, 0.21, 0.43]; P<0.0001; Figure 2A). Significant PFS advantage with afatinib over gemcitabine/cisplatin was also observed in patients with common EGFR (Del19 or L858R) mutations (median 11.0 versus 5.6 months; HR, 0.26 [95% CI, 0.18, 0.37]; P<0.0001). Similar PFS advantage with afatinib over gemcitabine/cisplatin was observed in other patient subgroups, including individual mutation categories (Figure 2B; Supplementary slides); PFS was significantly prolonged with afatinib versus gemcitabine/cisplatin both in patients with an EGFR Del19 mutation (median 13.7 versus 5.6 months with gemcitabine/cisplatin; HR, 0.21 [95% CI, 0.13, 0.36]; P<0.0001) and those with the EGFR L858R mutation (median 8.3 versus 5.6 months; HR, 0.33 [95% CI, 0.20, 0.56]; P<0.0001).
OS
Overall, in Chinese patients, OS was not significantly different with afatinib and gemcitabine/cisplatin (median 23.1 versus 23.2 months; HR, 0.96 [95% CI, 0.73, 1.27]; P=0.7765; Figure 3A); median OS in patients with common mutations was 23.6 versus 23.0 months, respectively (HR, 0.82 [95% CI, 0.62, 1.10]; P=0.1917). However, in patients with an EGFR Del19 mutation, afatinib significantly improved OS versus gemcitabine/cisplatin (median 31.6 versus 16.3 months; HR, 0.61 [95% CI, 0.41, 0.91]; P=0.0146; Figure 3B); there was no significant difference in the EGFR L858R subgroup (median 18.7 versus 24.5 months; HR, 1.31 [95% CI, 0.85, 1.99]; P=0.2171; Figure 3C). Among the 20 patients with long-term response on afatinib (LTRs), five patients had survival times of more than 5 years (Supplementary slides).
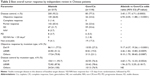
Tumor response
The ORR was significantly higher with afatinib than with gemcitabine/cisplatin (66.8% versus 23.6%; odds ratio [OR], 6.94 [95% CI, 4.05, 11.88]; P<0.0001); three patients (1.4%) experienced a CR with afatinib (versus none with gemcitabine/cisplatin; Table 2). The DCR was also significantly higher with afatinib than with gemcitabine/cisplatin (92.2% versus 77.3%; OR, 3.45 [95% CI, 1.77, 6.71]; P=0.0003).
Most patients who achieved an objective response with afatinib did so within the first 6 weeks (103/145, 71%), that is, by the first visit, and almost all of those who achieved an objective response did so by 18 weeks (137/145, 94.5%). The median duration of objective response was 9.7 months with afatinib and 4.2 months with gemcitabine/cisplatin. The median duration of disease control was 11.1 months with afatinib and 5.6 months with gemcitabine/cisplatin.
Significantly more patients achieved an objective response with afatinib compared with gemcitabine/cisplatin in all of the mutation subgroups examined (Table 2). The difference between the treatment arms was particularly pronounced in patients with a Del19 mutation (77.5% versus 27.3%; OR, 9.17 [95% CI, 4.37, 19.26]; P<0.0001). The DCR was only significantly different between the treatment groups in patients with a Del19 mutation (93.7% versus 76.4%; OR, 4.60 [95% CI, 1.72, 12.33]; P=0.0024).
Safety
The most common TRAEs are shown in Table 3. Almost all patients experienced at least one TRAE (98.6%–99.0%). Most TRAEs were of grade 1 or 2 severity. Similar proportions of patients experienced grade 3 TRAEs in each treatment arm (35.5% and 35.9% with afatinib and chemotherapy, respectively), but substantially more patients in the gemcitabine/cisplatin group experienced grade 4 TRAEs (21.4%) than in the afatinib group (0.9%). The most common treatment-related grade 3/4 AEs in the afatinib group were diarrhea (5.6%/0%), rash/acne (16.4%/0%), and stomatitis (6.1%/0%), whereas vomiting (18.4%/0.9%), nausea (8.7%/0%), neutropenia (28.2%/0.5%), and leukopenia (16.5%/0.5%) were the most common treatment-related grade 3/4 AEs in the gemcitabine/cisplatin group (Table 3).
TRAEs leading to permanent discontinuation of the study drug were reported in 12 patients (5.6%) in the afatinib arm and 43 patients (41.7%) in the gemcitabine/cisplatin arm. No patients in the afatinib group discontinued treatment because of diarrhea; the most common reason for discontinuation was rash (5/12 patients). The most common reasons for discontinuing gemcitabine/cisplatin were vomiting (15/43; 35%), nausea (11/43; 26%), and neutropenia (10/43; 23%).
Serious TRAEs were reported in 6.1% of patients in the afatinib group and 4.9% of patients in the gemcitabine/cisplatin group. Two grade 5 (fatal) AEs were considered possibly related to treatment, one in each treatment group. These were sudden death in the afatinib group and cardiac failure in the gemcitabine/cisplatin group.
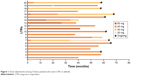
PROs
Analysis of PROs focused on three key symptoms that are most important to patients with NSCLC: cough, dyspnea, and pain. Significantly greater proportions of patients in the afatinib group had improvements in cough (76.8% versus 55.4%; P=0.0003), dyspnea (71.3% versus 47.8%; P=0.0001), and pain (63.9% versus 43.5%; P=0.0012) than in the gemcitabine/cisplatin group (Figure 4). There were significant improvements in all items related to cough, dyspnea, and pain except “dyspnea rested” and “pain in arm/shoulder”. Time to deterioration of cough (HR, 0.43 [95% CI, 0.28, 0.67]; P=0.0001), dyspnea (HR, 0.51 [95% CI, 0.37, 0.71]; P<0.0001), and pain (HR, 0.62 [95% CI, 0.45, 0.87]; P=0.0044) were all delayed with afatinib versus chemotherapy (Supplementary slides).
Pharmacokinetics
Afatinib trough plasma concentrations showed high variability (geometric coefficient of variation [gCV] 47.1%–90.3%) for all dose groups and over all pharmacokinetic (PK) visits (Table 4). Mean trough plasma concentrations at the last PK observation on day 43, however, were at a similar level for all dose groups, by which time most patients would have received any required dose adjustments (Table 4). The geometric mean trough plasma concentration was 20.6 ng/mL (gCV 47.1%) for patients whose dose had been reduced to afatinib 30 mg, 21.5 ng/mL (gCV 63.5%) for patients who remained on afatinib 40 mg, and 23.5 ng/mL (gCV 61.5%) for patients whose dose had been escalated to afatinib 50 mg.
Discussion
To our knowledge, this subgroup analysis of LUX-Lung 6 is the largest analysis of treatment with an EGFR-targeted agent, following upfront mutation testing, in Chinese patients. Our analysis demonstrated that afatinib significantly improved PFS, ORR, and (in patients with an EGFR Del19 mutation) OS versus gemcitabine/cisplatin in patients from mainland China. Furthermore, efficacy benefits were largely consistent across patient subgroups, including mutation type (Del19 or L858R). Importantly, the efficacy benefits with afatinib were complemented by improvements in PROs for symptoms that are most important to patients with NSCLC: cough, dyspnea, and pain. There were 20 LTRs, of whom eight remain on treatment at the time of analysis. Overall, the tolerability profile of afatinib was consistent with previous experience and was considerably less severe than that experienced with platinum-based chemotherapy; TRAEs were largely manageable on treatment and discontinuation due to AEs was rare. Together, these data demonstrate that afatinib should be considered as a first-line treatment option in Chinese patients with EGFR mutation-positive NSCLC.
Given the availability of several EGFR TKIs in China, it is a pertinent question to ask the following: which agent is the most suitable first-line treatment of choice in which patient? At present, few head-to-head clinical trial data comparing EGFR TKIs in Chinese patients are available to help guide treatment decisions. The recent CTONG0901 Phase III trial compared the efficacy and safety of gefitinib and erlotinib in 265 Chinese patients with EGFR mutation-positive NSCLC in any line. Findings showed no significant difference in PFS (median 13.0 versus 10.4 months; HR, 0.81 [95% CI, 0.62, 1.05]; P=0.108) or OS (median 22.9 versus 20.1 months; HR, 0.84 [95% CI, 0.63, 1.13]; P=0.250) between the two treatment arms.26 LUX-Lung 7 is the only published head-to-head trial between two EGFR-targeted agents specifically in a first-line setting. In this trial, 48 of 319 randomized patients were from China. For the overall dataset, afatinib significantly improved PFS (median 11.0 versus 10.9 months; HR, 0.73 [95% CI, 0.57, 0.95]; P=0.017) and TTF (median 13.7 versus 11.5 months; HR, 0.73 [95% CI, 0.58, 0.92]; P=0.0073) with a trend toward improved OS, despite not being powered to detect any difference in OS versus gefitinib (median OS 27.9 versus 24.5 months; HR, 0.85 [95% CI, 0.66, 1.09]; P=0.1950).17,18,27
Although cross-trial comparisons are difficult, and clearly do not substitute for prospective head-to-head data, it is of interest to view this large LUX-Lung 6 subanalysis (n=327) dataset in the context of available Chinese data with erlotinib, gefitinib, and icotinib. Two trials provide data on erlotinib in Chinese patients: the Phase III OPTIMAL trial examined the efficacy and safety of erlotinib (n=82) versus gemcitabine/carboplatin (n=72) in Chinese patients with EGFR mutation-positive NSCLC (common mutations only),14,28 while a subsequent Asian Phase III trial, ENSURE – which largely included Chinese patients (~80%) – compared erlotinib (n=110) versus gemcitabine/cisplatin (n=107) in the same treatment setting.13 The recent Phase III CONVINCE trial compared icotinib (n=148) versus cisplatin/pemetrexed (n=137) in Chinese patients with EGFR mutation-positive NSCLC (common mutations only).15 In contrast to erlotinib and icotinib, few data are available that have assessed gefitinib specifically in Chinese patients with EGFR mutation-positive NSCLC. The Phase III trials, NEJ-002 and WJTOG3405, were undertaken specifically in Japanese patients.7,8 Although IPASS included 372 patients from China, analysis in EGFR mutation-positive patients was difficult to interpret as a low proportion of patients recruited in China provided a tumor sample to determine EGFR mutation status (38%).29 In OPTIMAL, erlotinib conferred PFS advantage versus chemotherapy in Chinese patients (HR, 0.16 [95% CI, 0.10, 0.26]; P<0.0001), although it should be noted that efficacy was analyzed in patients who “had received at least one dose of study drug” rather than in the intent-to-treat population. Additionally, no clinical study report was available for this trial when reviewed by the European Medicines Agency. PFS advantage with erlotinib was also observed in a subgroup analysis of Chinese patients in the ENSURE study, but with a higher HR than that is observed in OPTIMAL (HR, 0.30 [95% CI, 0.18, 0.49]).13,14 In the Chinese subanalysis of IPASS, there was no significant difference in PFS with gefitinib and chemotherapy in EGFR mutation unselected patients (median 6.8 versus 6.8 months; HR, 0.79 [95% CI, 0.62, 1.01]; P=0.065).29 In CONVINCE, icotinib significantly improved PFS versus chemotherapy in Chinese patients (median 11.2 versus 7.9 months; HR, 0.61 [95% CI, 0.43, 0.87]; P=0.006).15
Like afatinib, gefitinib, icotinib, and erlotinib were associated with better tolerability profiles compared to chemotherapy in Chinese patients with NSCLC.13–15,29 TRAEs were reported in 87.0%–87.3% with erlotinib, 83.2% with gefitinib, and 54.1% with icotinib. Treatment-related serious AEs were reported in 2.4%–2.7% with erlotinib and 2.2% with gefitinib. The most common grade 3/4 AEs with erlotinib were rash (2.4%–6.4%) and elevated alanine transaminase (ALT; 3.6% in OPTIMAL; none reported in ENSURE); the most common grade 3/4 AEs with gefitinib were rash/acne (3.8%) and elevated ALT (3.8%). The most common grade 3/4 AEs with icotinib were rash (14.9%) and diarrhea (7.4%). Treatment discontinuations due to AEs were required in 1.2%–2.7% of patients treated with erlotinib and 2.0% of patients treated with icotinib; no dose discontinuations because of AEs were required with gefitinib in the Chinese subanalysis of IPASS.
One important distinguishing feature of the LUX-Lung 6 Chinese data compared with available Chinese data for gefitinib, icotinib, and erlotinib is that afatinib uniquely conferred OS advantage versus chemotherapy in patients with an EGFR Del19 mutation. This finding is consistent with the overall LUX-Lung 6 dataset of Del19 patients (median 31.4 versus 18.4 months; HR, 0.64 [95% CI, 0.44, 0.94]), as well as the LUX-Lung 3 study (median 33.3 versus 21.1 months; HR, 0.54 [95% CI, 0.36, 0.79]).16 In contrast, erlotinib did not confer OS advantage over chemotherapy in Del19 patients in either OPTIMAL (HR, 1.52 [95% CI, 0.91, 2.52]) or ENSURE (HR, 0.79 [95% CI, 0.48, 1.30]).13,28 Likewise, no OS advantage was observed with icotinib versus chemotherapy in Del19 patients in CONVINCE.15 The observation of OS benefit with afatinib in patients with Del19 mutations is unlikely to be attributable to imbalances in post-progression therapy because crossover rates in LUX-Lung 6 were similar in patients with Del19 and L858R mutations.16 It is possible that the achievement of significant OS benefit with afatinib but not erlotinib nor icotinib reflects the differences in mechanism of action between afatinib and first-generation TKIs. Notably, afatinib potently and irreversibly inhibits all members of the ErbB family, whereas first-generation TKIs reversibly inhibit EGFR only.30,31
In this subanalysis of LUX-Lung 6, TRAEs were reported by most patients, and treatment with afatinib was associated with the expected gastrointestinal and dermatologic AEs. These were managed with supportive care and protocol-defined dose reductions; post hoc analyses demonstrated that dose reduction effectively mitigated TRAEs without impacting efficacy. Consequently, few patients had to discontinue afatinib treatment because of AEs (5.6%), and none because of diarrhea. This suggests that the established protocols for managing AEs associated with afatinib are robust and effective in Chinese patients. Furthermore, although AEs were common with afatinib, substantial improvements in health-related quality of life were reported, including improvements in all domains of lung-cancer symptoms, suggesting that the beneficial effects of afatinib outweigh its AEs.
Consistent with previous studies, the variability in afatinib plasma concentrations was high for all dose groups. Analysis of the LUX-Lung 3 and overall LUX-Lung 6 data has demonstrated that, in general, patients with high trough plasma concentrations were more likely to require a dose reduction to afatinib 30 mg within the PK observation period of 43 days.19 The PK data suggest that the individual tolerability-driven dose modification is effective at reducing excessive afatinib levels. Importantly, observations from the overall LUX-Lung 3 and LUX-Lung 6 datasets showed that such tolerability-guided dose adjustment does not affect therapeutic efficacy. In both cases, median PFS was similar in patients who reduced their dose during the first 6 months versus those who did not (LUX-Lung 3: 11.3 versus 11.0 months; HR, 1.25 [95% CI, 0.91, 1.72]; LUX-Lung 6: 12.3 versus 10.0 months; HR, 1.00 [95% CI, 0.69, 1.46]).19
Limitations of this analysis include that it is a subgroup analysis of a larger study; however, it is notable that the population of over 300 Chinese patients represented ~90% of the population of the parent study.12 The open-label nature of the study is also a limitation, although, in this analysis, assessment of the patients’ scans was conducted by an independent central panel of radiologists and oncologists, and sensitivity analyses did not suggest any bias. Finally, it should be noted that chemotherapy would not now be regarded as the state-of-the-art comparator arm in randomized trials in patients with EGFR mutation-positive NSCLC; since the initiation of LUX-Lung 6 in 2010, TKIs have become the first-line treatment of choice in this setting. However, gemcitabine/cisplatin was commonly used in Asia at the time that the study was designed, and the regulatory authorities approved this choice as a comparator.12
Conclusion
This analysis of Chinese patients with EGFR mutation-positive NSCLC has demonstrated that afatinib is more effective and has more durable effects than standard first-line chemotherapy. Furthermore, to our knowledge, afatinib is the only TKI to demonstrate improved OS versus standard chemotherapy in patients harboring an EGFR Del19 mutation. Together, the findings suggest that afatinib should be considered a first-line treatment option for this patient population.
Acknowledgments
We thank the patients, their families, and all the investigators who participated in this study. The authors were fully responsible for all content and editorial decisions, were involved at all stages of manuscript development, and have approved the final version. This work was supported by Boehringer Ingelheim. Medical writing assistance, supported financially by Boehringer Ingelheim, was provided by Lynn Pritchard of GeoMed, an Ashfield company, part of UDG Healthcare plc, during the preparation of this manuscript.
Disclosure
Y-LW reports consultancy fees from AstraZeneca; and lecture fees from AstraZeneca, Eli Lilly, Pfizer, Roche, and Sanofi. CZ reports lecture fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly, Roche, and Sanofi. AM, JF, and BP report employment by Boehringer Ingelheim. The authors report no other conflicts of interest in this work.
References
Chen W, Zheng R, Zeng H, Zhang S. The incidence and mortality of major cancers in China, 2012. Chin J Cancer. 2016;35(1):73. | ||
Hong QY, Wu GM, Qian GS, et al; Lung Cancer Group of Chinese Thoracic Society; Chinese Alliance Against Lung Cancer. Prevention and management of lung cancer in China. Cancer. 2015;121(Suppl 17):3080–3088. | ||
Li MJ, He Q, Li M, Luo F, Guan YS. Role of gefitinib in the targeted treatment of non-small-cell lung cancer in Chinese patients. Onco Targets Ther. 2016;9(9):1291–1302. | ||
Reck M, Heigener DF, Mok T, Soria JC, Rabe KF. Management of non-small-cell lung cancer: recent developments. Lancet. 2013;382(9893):709–719. | ||
Reck M, Popat S, Reinmuth N, et al. ESMO Guidelines Working Group. Metastatic non-small-cell lung cancer (NSCLC): ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25(Suppl 3):iii27–iii39. | ||
Shi Y, Sun Y, Ding C, et al. China experts consensus on icotinib for non-small cell lung cancer treatment (2015 version). J Thorac Dis. 2015;7(10):E468–E472. | ||
Maemondo M, Inoue A, Kobayashi K, et al; North-East Japan Study Group. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362(25):2380–2388. | ||
Mitsudomi T, Morita S, Yatabe Y, et al; West Japan Oncology Group. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11(2):121–128. | ||
Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–957. | ||
Rosell R, Carcereny E, Gervais R, et al; Spanish Lung Cancer Group in collaboration with Groupe Français de Pneumo-Cancérologie and Associazione Italiana Oncologia Toracica. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13(3):239–246. | ||
Sequist LV, Yang JC, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol. 2013;31(27):3327–3334. | ||
Wu YL, Zhou C, Hu CP, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(2):213–222. | ||
Wu YL, Zhou C, Liam CK, et al. First-line erlotinib versus gemcitabine/cisplatin in patients with advanced EGFR mutation-positive non-small-cell lung cancer: analyses from the phase III, randomized, open-label, ENSURE study. Ann Oncol. 2015;26(9):1883–1889. | ||
Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12(8):735–742. | ||
Shi YK, Wang L, Han BH, et al. First-line icotinib versus cisplatin/pemetrexed plus pemetrexed maintenance therapy for patients with advanced EGFR mutation-positive lung adenocarcinoma (CONVINCE): a phase 3, open-label, randomized study. Ann Oncol. 2017;28(10):2443–2450. | ||
Yang JC, Wu YL, Schuler M, et al. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol. 2015;16(2):141–151. | ||
Park K, Tan EH, O’Byrne K, et al. Afatinib versus gefitinib as first-line treatment of patients with EGFR mutation-positive non-small-cell lung cancer (LUX-Lung 7): a phase 2B, open-label, randomised controlled trial. Lancet Oncol. 2016;17(5):577–589. | ||
Paz-Ares L, Tan EH, O’Byrne K, et al. Afatinib versus gefitinib in patients with EGFR mutation-positive advanced non-small-cell lung cancer: overall survival data from the phase IIb LUX-Lung 7 trial. Ann Oncol. 2017;28(2):270–277. | ||
Yang JC, Sequist LV, Zhou C, et al. Effect of dose adjustment on the safety and efficacy of afatinib for EGFR mutation-positive lung adenocarcinoma: post hoc analyses of the randomized LUX-Lung 3 and 6 trials. Ann Oncol. 2016;27(11):2103–2110. | ||
Schuette W, Schirmacher P, Eberhardt WE, et al. EGFR mutation status and first-line treatment in patients with stage III/IV non-small cell lung cancer in Germany: an observational study. Cancer Epidemiol Biomarkers Prev. 2015;24(8):1254–1261. | ||
Sekine I, Yamamoto N, Nishio K, Saijo N. Emerging ethnic differences in lung cancer therapy. Br J Cancer. 2008;99(11):1757–1762. | ||
Skov BG, Hogdall E, Clementsen P, et al. The prevalence of EGFR mutations in non-small cell lung cancer in an unselected Caucasian population. APMIS. 2015;123(2):108–115. | ||
Shi Y, Li J, Zhang S, et al. Molecular epidemiology of EGFR mutations in Asian patients with advanced non-small-cell lung cancer of adenocarcinoma histology – Mainland China subset analysis of the PIONEER study. PLoS One. 2015;10(11):e0143515. | ||
Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–376. | ||
Bergman B, Aaronson NK, Ahmedzai S, Kaasa S, Sullivan M. The EORTC QLQ-LC13: a modular supplement to the EORTC Core Quality of Life Questionnaire (QLQ-C30) for use in lung cancer clinical trials. EORTC Study Group on quality of life. Eur J Cancer. 1994;30A(5):635–642. | ||
Yang JJ, Zhou Q, Yan HH, et al. A phase III randomised controlled trial of erlotinib vs gefitinib in advanced non-small cell lung cancer with EGFR mutations. Br J Cancer. 2017;116(5):568–574. | ||
Corral J, Park K, Yang JCH, et al. Afatinib (A) vs gefitinib (G) in patients with EGFR mutation-positive (EGFRm+) NSCLC: updated OS data from the phase IIb trial LUX-Lung 7 (LL7). Poster presented at: European Lung Cancer Conference; May 07, 2017; Geneva, Switzerland. | ||
Zhou C, Wu YL, Chen G, et al. Final overall survival results from a randomised, Phase III study of erlotinib versus chemotherapy as first-line treatment of EGFR mutation-positive advanced non-small-cell lung cancer (OPTIMAL, CTONG-0802). Ann Oncol. 2015;26(9):1877–1883. | ||
Wu YL, Chu DT, Han B, et al. Phase III, randomized, open-label, first-line study in Asia of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer: evaluation of patients recruited from mainland China. Asia Pac J Clin Oncol. 2012;8(3):232–243. | ||
Li D, Ambrogio L, Shimamura T, et al. BIBW2992, an irreversible EGFR/HER2 inhibitor highly effective in preclinical lung cancer models. Oncogene. 2008;27(34):4702–4711. | ||
Solca F, Dahl G, Zoephel A, et al. Target binding properties and cellular activity of afatinib (BIBW 2992), an irreversible ErbB family blocker. J Pharmacol Exp Ther. 2012;343(2):342–350. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.