Back to Journals » International Journal of General Medicine » Volume 14
Adverse Perinatal Outcomes Among Grand Multiparous and Low Multiparous Women and Its Associated Factors in North Shewa Zone Public Hospitals: The Role of Parity
Authors Tadese M , Desta Tessema S , Tsegaw Taye B
Received 6 August 2021
Accepted for publication 1 October 2021
Published 9 October 2021 Volume 2021:14 Pages 6539—6548
DOI https://doi.org/10.2147/IJGM.S333033
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mesfin Tadese, Saba Desta Tessema, Birhan Tsegaw Taye
Department of Midwifery, College of Medicine and Health Sciences, Debre Berhan University, Debre Berhan, Ethiopia
Correspondence: Mesfin Tadese
Department of Midwifery, College of Medicine and Health Sciences, Debre Berhan University, Debre Berhan, Ethiopia
Tel +251 915839921
Email [email protected]
Background: Adverse perinatal outcomes are the major cause of neonatal morbidity, mortality, and long-term physical and psychological consequences. Contradicting evidence across studies was reported about the impact of grand multiparity on adverse perinatal outcomes. Older literature reported increased incidence of perinatal complications in grand multiparas, but, recent reports failed to support this finding. In addition, there is a paucity of comparative studies on perinatal outcomes. Thus, the study aimed to compare the perinatal outcomes in grand multiparous (GM) and low multiparous (LM) women who give birth in North Shewa Zone Public Hospitals, Ethiopia, 2021.
Methods: A comparative cross-sectional study was done among 540 (180 GM and 360 LM) women from January 1 to March 30, 2021. The data were collected using a structured and pre-tested questionnaire through interviews and reviewing patient charts. SPSS version 25 was used for data analysis. The data were entered using Epi-Data version 4.6. The Hosmer–Lemeshow goodness-of-fit was applied to test for model fitness. The statistical significance level was declared at a p-value of ≤ 0.05.
Results: In this study, the prevalence of adverse perinatal outcomes was 14.1% (95% CI: 10.9– 17.2). Stillbirth/IUFD (33.3%) and low APGAR score (60%) were frequently occurred complications in grand multiparas. Nevertheless, meconium aspiration (26%), admission to NICU (65.2%), macrosomia (61%), and prematurity (52.2%) were higher in low multiparous women. Age above 35 years (AOR (CI) = 2.61 (1.23– 5.53)), rural residence (AOR (CI) = 8.31 (3.05– 22.6)), being a government employee (AOR (CI) = 0.19 (0.05– 0.69)), lack of antenatal care (AOR (CI) = 9.76 (3.03– 31.5)), and previous pregnancy complications (AOR (CI) = 3.10 (1.63– 5.90)) were significant predictors of adverse perinatal outcomes. However, parity did not show a statistically significant association with perinatal outcomes.
Conclusion: Maternal age, residence, occupation, lack of antenatal care, and previous pregnancy complications were significant associates of perinatal outcome. There was no statistically significant difference in perinatal outcome between GM and LM women. Socio-economic development, good antenatal care, and early identification and treatment of complications are needed regardless of parity.
Keywords: adverse perinatal outcomes, grand multiparous, low multiparous, parity, Ethiopia
Introduction
The adverse perinatal outcome remains the major challenge to the public health sector in both low-and-middle-income countries. Prematurity, low birth weight, stillbirth, and congenital malformations constitute some of the common adverse birth outcomes.1 Globally, an estimated 2.6 million stillbirths occurred each year, one in every 16 seconds. Ninety-eight percent of these deaths occurred in low-and middle-income countries and 75% in Sub-Saharan Africa and Southern Asia. However, over 40% of stillbirths could have been prevented through high-quality antepartum, intrapartum, and postpartum care, and timely access to emergency obstetric care.2 One of the significant risk factors for these deaths was grand multiparity.3
Grand multiparity is the delivery of five or more live births and stillbirths after the age of viability. The term was first introduced in 1934 by Solomon as “the dangerous multiparas”. The author described it as dangerous because pregnancy complications and maternal mortality increased steadily from the 5th to 10th pregnancy.4 However, recent reports fail to support these findings.
A secondary analysis of the Nigerian Demographic and Health Survey determined the magnitude of adverse perinatal outcomes at 14.9%.5 A systematic review and meta-analysis study in Sub-Saharan Africa reported a pooled prevalence of 29.7%.6 Besides, the magnitude of perinatal complication was 18.2% in Butajira,7 21% in Bale Zone,8 and 18.3% in Hawassa town.9 Further, in Southern Ethiopia, one-fourth (24.9%) of multiparous women had at least one adverse birth outcome. This study also found a higher prevalence of stillbirth (38.9%), low APGAR score (51.9%), and low birth weight (40.7%) among grand multiparous women, while a higher risk of meconium aspiration (9.8%), need for resuscitation (14.7%), and macrosomia (57.4%) among low multiparous women.1
Contradicting evidence across studies was reported about the impact of grand multiparity on adverse perinatal outcomes. In Tanzania, meconium-stained amniotic fluid and low APGAR (Appearance, Pulse, Grimace, Activity, and Respiration) scores were significant among neonates born to grand multiparous women.10 Grand multiparity was also found to increase the risk of neonatal admission to intensive care units11 and fetal macrosomia.12 Compared to low multiparas, neonates of grand multipara are at higher risk of low birth weight13 and stillbirth.3 Contrarily, in Uganda, the risk of stillbirth declines with increasing parity.14 Similarly, a comparative cohort study in the same country found no difference in fetal outcome between grand multiparous and low multiparous women.15 Besides, a systematic review and meta-analysis finding showed that grand multiparity did not increase the risk of adverse pregnancy outcomes.16 Further in South Ethiopia, parity showed an insignificant difference in perinatal outcomes.1 Hence, in the absence of clear and consistent evidence, classifying grand multiparous women as a high-risk group would raise the socioeconomic burdens to families and health systems as well as physical and psychological stress to the mother and her families.
A cohort study in Uganda reported the significant association of gestational age <34 weeks at delivery and low birth weight with adverse birth outcomes.17 Advanced maternal age, maternal illiteracy, short birth interval, and complication during pregnancy had also positive associations with adverse perinatal outcomes (APO).18 Additionally, a Nigerian study reported that referred cases, previous history of stillbirths, gestational age at delivery, and mode of delivery were associated with stillbirths.19 Female neonates and women who had undergone female genital mutilation were more likely to have stillbirth.20 In Southern Ethiopia, less than four prenatal visits and previous home delivery were independent predictors of APO.1
Ethiopia has made a substantial struggle towards improving the maternal and children health. Since 2000 impressive progress has been made. Maternal and child mortality due to complications during delivery has reduced by half, and half (48%) of women now give birth in a facility. The key interventions were preventing or treating the most important causes of child mortality – in particular essential immunizations, malaria prevention and treatment, vitamin A supplementation, birth spacing, scaling up family planning, training health extension workers, early and exclusive breast feeding and improving socio-economic conditions. In addition, over 38,000 health workers, 16,000 health posts, and more than 3000 health centers have been constructed to increase access to essential services. However, low utilization of maternal health services, ensuring timely arrival, and service quality at facilities remains a challenge. These conditions have been exacerbated as the health extension programme struggles to meet the demand for routine quality healthcare and to respond to drought, conflict or disease outbreaks, including COVID-19.21,22
To achieve the sustainable development goal (SDG) 3.2 determining the adverse perinatal outcomes have a higher advantage in reducing severe neonatal morbidity, mortality, and long-term complications along with good maternal and neonatal health continuum of care. Additionally, in Ethiopia, there is a paucity of comparative studies on adverse perinatal outcomes. The finding of the study may be used as a baseline for large-scale studies done on birth outcomes. Thus, the study aimed to compare perinatal outcomes in multiparous women and identify independent predictors of adverse perinatal outcomes in North Shewa Zone Public Hospitals, 2021.
Methods
Study Setting and Period
The study was done in North Shewa Zone public hospitals from January 1 to March 30, 2021. North Shewa is one of the 10 zones in the Amhara regional state. The Zone is bordered on the south and the west by the Oromia region, on the north by South Wollo, and on the east by the Afar region. It has 23 districts with a population of 1,837,490; 928,694 men and 908,796 women. Debre Birhan is the capital city of the North Shewa Zone and is located 130 km Northeast of Addis Ababa on the Ethiopian highway. It is the highest town in Africa with an elevation of 2840m. There are 12 Hospitals (2 private, 10 Public; 9 primary and 1 comprehensive Specialized Hospital). There are about 766 Nurses, 303 midwives, 120 Laboratory professionals, 130 Pharmacists, 150 General Practitioners, 15 Specialists, 25 integrated emergency surgical officers (IESO), 54 Anesthesia, 22 Radiology technicians, and 15 mental health professionals working in the zone.
Study Design and Population
This is a comparative cross-sectional study conducted on multiparous women who gave birth in the study areas during the study period.
Eligibility Criteria
Selected multiparas with a single fetus/neonate at a gestational age of ≥28 weeks were included. Whereas multiparas with twin gestation/delivery, with known medical conditions, ie, DM, HIV, and hypertension, who delivered at other health institutions or home delivery, and those who were unable to communicate or seriously ill were excluded from the study.
Sample Size and Sampling Procedure
The sample size calculation was computed using EPI INFO version 7.2.2.6 statistical software. The following assumptions were made: the power (1-β) 80%, the ratio of controls to cases 2, percent of outcome in unexposed group 20.66%, and odds ratio 1.87.1 Adding a 10% non-response rate, the final sample size was 548 (183 GM and 365 LM).
There are ten public hospitals in North Shewa Zone. Five hospitals were recruited by lottery methods. The average number of deliveries in the selected hospitals was 689 per month. Then, proportional allocation of the sample size to the selected hospitals was made based on their respective number of deliveries per month. All study participants were selected consecutively as they present. First, cases (grand multiparous women) were identified and then consecutively two low multiparous women from the same hospital were interviewed and assessed.
Data Collection Tool and Quality Control
A structured and pre-tested interviewer-administered questionnaire was used to collect the data. The questionnaire was first prepared in English and translated to the local language (Amharic) and then back to English by an independent translator to keep the consistency of the instrument. The items of information requested include the socio-demographic characteristics, obstetrics and contraception history, pregnancy complications, and fetal outcomes. A pretest was done on 5% of the samples (9 GM and 18 LM) in Arerti primary hospital and necessary amendments were considered following the result.
Five data collectors and two supervisors participated in the data collection. The investigators trained data collectors and supervisors for one day about the tool and data collection procedure. The data were collected through face-to-face interviews and a review of clinical documents. For mothers having a normal delivery, data were collected 1–2 hours after delivery. Mothers who gave birth through cesarean or complicated vaginal delivery waited until they are fully awake. The supervisors and principal investigators checked the completeness, consistency, and clarity of the data.
Study Variable
The outcome/dependent variable was perinatal outcome. Independent/exposure variables were socio-demographic variables (age, educational level, marital status, income, occupation), reproductive history (inter-pregnancy interval, parity, etc.), obstetric and contraception factors (ANC follow-up, distance of health institution, previous obstetric complication, contraception use, place of delivery, etc.).
Definition of Terms
Low multiparity (LM): a woman with 2–4 deliveries after 28 weeks of gestation.
Grand multiparity (GM): a woman with ≥5 births after 28 weeks of gestation.
Perinatal outcomes: was at least one adverse fetal/newborn outcome ie, stillbirth, low birth weight, macrosomia, meconium aspiration syndrome, congenital malformation, need for resuscitation, and low Apgar score between 28 weeks of gestation and discharge from the hospital.
Macrosomia: birth weight ≥4000 g weighed during the first 15 minutes of delivery.
Low Apgar score: a score of less than seven recorded at the 5th minute of delivery.
Stillbirth: the death of the fetus in the uterus before birth at or after 28-week gestational age.
Mistimed/unplanned pregnancy: Women who did not desire the current pregnancy but did not use effective contraception either due to side effects, religious prohibition, or partner disapproval.
Alcohol consumption: refers to the use of either Tej, Tella, Areke, or Beer.
Data Management and Analysis
The data were cleaned, coded, and entered into Epi-Data version 4.6 and exported to SPSS version 25.0 statistical software for analysis. Univariable analysis and cross-tabulation of variables were done for GM and LM. Variables with a p-value of ≤0.25 were included in the multivariable logistic regression analysis. The Hosmer–Lemeshow goodness-of-fit was applied to test for model fitness. Statistically significant variables were declared at a p-value of ≤0.05. The strength of association was interpreted using an adjusted odds ratio (AORs) with a 95% confidence interval.
Ethical Approval
An ethical clearance letter was obtained from the Institutional Review Boards of Debre Berhan University. A formal letter was also written to the selected study hospitals. Written informed consent was obtained from the study participants. For illiterate mothers, information was read and asked for thumbprint the consent form. Any information related to the study participants’ identification was not recorded to maintain confidentiality. The study was conducted in accordance with the declaration of Helsinki ethical principles.
Result
Baseline Characteristics
A total of 540 (180 LM and 360 GM) women were interviewed, making a 98.9% response rate. The mean (±SD) age of LM and GM women was 28.59±4.15 and 34.77±4.34, respectively. Around 20% of women who develop adverse perinatal outcomes were above 35 years. One-fourth (26.6%) of rural residents and 22.2% of mothers who attended primary school had at least one adverse perinatal outcome. Further, 21.7% of women married before 18 years developed perinatal complications (Table 1).
 |
Table 1 Bivariable and Multivariable Logistic Regression Analysis of Variables with Adverse Perinatal Outcome in North Shewa Zone Public Hospitals, 2021 |
Obstetrics and Contraception History
The mean (±SD) birth weight of newborns was 3103.33±634.29 and 3103.33±607.85 grams for LM and GM, respectively. A higher proportion of grand multiparous women developed adverse birth outcomes than low multiparas (16.7% vs 12.8%). Besides, perinatal complications were common in women with no ANC visits (44%), previous obstetric complications (21%), and previous home delivery (25%). A higher percentage of male (16%) newborns developed adverse perinatal outcomes. Further, 20% of women who ever not used contraception developed adverse perinatal outcomes compared to those who ever used (12%) (Table 1).
Adverse Perinatal Outcomes
The prevalence of adverse perinatal outcomes was 14.1% (95% CI: 10.9–17.2). Stillbirth/IUFD (33.3%) and low APGAR score (60%) frequently occurred in grand multiparas Nevertheless, meconium aspiration (26%), admission to NICU (65.2%), macrosomia (61%), and prematurity (52.2%) were higher in low multiparous women (Figure 1).
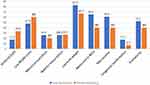 |
Figure 1 Adverse perinatal outcome in low multiparous and grand multiparous women who gave birth in North Shewa Zone Public Hospitals, 2021. |
Determinants of Adverse Perinatal Outcomes
Bivariable logistic regression analysis was computed, and variables with a p-value of ≤0.25 were entered into the multivariable logistic regression analysis model. In the final model, maternal age, residence, maternal occupation, antenatal care, and previous obstetric complication have shown a statistically significant association with adverse perinatal outcomes (Table 1).
Mothers aged above 35 years were approximately three times more likely to develop adverse birth outcomes compared to those aged between 21–34 years (AOR (CI)= 2.61 (1.23–5.53)). The odds of adverse perinatal outcomes were eight times higher among rural residents than the urban counterparts (AOR (CI)= 8.31 (3.05–22.6)). Government employees had less risk of adverse birth outcomes compared to self-employed (AOR (CI)= 0.19 (0.05–0.69)). Lack of antenatal care increased the risk of adverse perinatal outcomes by ninefold (AOR (CI)= 9.76 (3.03–31.5)). Additionally, adverse perinatal outcomes were three times more common in women with previous obstetric complications (AOR (CI)= 3.10 (1.63–5.90)) (Table 1).
Discussion
This study compared the perinatal outcomes in multiparous women. Stillbirth/IUFD and low APGAR score frequently occurred in grand multiparas. Maternal age, residence, occupation, lack of antenatal care, and previous pregnancy complications were significant predictors of adverse perinatal outcomes. However, parity did not show a statistically significant difference in perinatal outcomes.
According to this study, there was no statistically significant difference in perinatal outcomes between low multiparous and grand multiparous women. However, stillbirth/IUFD and low APGAR scores were higher in grand multiparous women. On the other hand, meconium aspiration, NICU admission, macrosomia, and prematurity were reported higher in low multiparous women. This finding was consistent with the studies done in Tanzania,3,10 Hawassa,1 and Jimma.23 A comparative study in Nigeria was also found a higher proportion of perinatal mortality among grand multiparous women, indicating the need for meticulous care to these mothers during pregnancy and delivery.24 Further, parity was not found to be a statistically significant factor for adverse perinatal outcomes in Southern Ethiopia.1 On the contrary, in Uganda, the risk of stillbirth declines with increasing parity.14 Besides, a significant association between grand multiparity and adverse fetal outcomes was reported in other studies.15,25,26 These differences might be due to variation in study design, setting, socio-economic status, and possible confounders, ie, adverse outcomes attributable to chronic disease. Adverse birth outcomes in the previous studies might be also attributed to low health service utilization of grand multiparas. Additionally, accessible and quality prenatal care differences in study subjects could explain the inconsistencies.
This study confirmed a significant association between antenatal care visits and birth outcomes. Lack of antenatal care (ANC) increased the risk of adverse perinatal outcomes by ninefold. This was consistent with the studies done in Wag Himra Zone27 and Southern Ethiopia.1 Similarly, a systematic review and meta-analysis study indicated that mothers who attended at least one ANC visit were more likely to give birth to an alive neonate that survives.28 Prenatal care follow-up allows the women to access information related to danger signs of pregnancy, birth plan, and place of delivery. It also helps to early identify and treat complications/diseases, ie, HIV/AIDS, syphilis, hypertension in pregnancy, and malaria. Moreover, women attending prenatal care are more likely to have a skilled birth attendant and hence their newborns will have access to basic essential newborn care and neonatal resuscitation. Thus, further improvement of the quality of antenatal care and mobilization of pregnant women to the new WHO recommended focused ANC care is needed to reduce adverse birth outcomes and achieve sustainable development goals.
It was observed that previous pregnancy complications had a positive association with adverse birth outcomes. Women with previous obstetric complications were three times at higher risk of perinatal complications. A prospective cohort study in Uganda found that preterm delivery and low birth weight were independent risk factors for adverse birth outcomes.17 Similarly, in Northern Ethiopia, the obstetric complication was a significant determinant of perinatal birth outcome.27 Another Cohort study in the Tigray region showed that women with pregnancy-induced hypertension born babies with a higher risk of low birth weight, birth asphyxia, small for gestational age, preterm delivery, stillbirth, admission to NICU, and perinatal death.29 This might be due to pregnancy complications have a higher rate of recurrence and most are associated with reduced oxygen and nutrient supply to the fetus (placental insufficiency), which may result in preterm birth, low birth weight, and stillbirth.
Advanced maternal age was found to be an associated risk factor for adverse fetal outcomes. Mothers aged above 35 years were nearly three times more likely to have an adverse birth outcome. This finding is in line with the studies done in Awi Zone,18 Debre Tabor,30 Shashemene,31 and Ethiopia.28 The reason might be that aging makes the uterus lax and limits the physical ability to bear a child. Old blood vessels in the uterus may also cause uteroplacental insufficiency and may result in abortion, growth retardation, and stillbirths. In addition, the risk of developing medical and obstetrical complications increases as age advances, ie, hypertension, diabetes, and preterm birth.
The odds of adverse perinatal outcomes were eight times higher among rural residents than their urban counterparts. A similar finding was reported in Canada,32 Wag Himra Zone,27 and Arba Minch.33 The possible explanation is that urban mothers had better socioeconomic status, ie, better education and income, and access to health facilities. More likely to reach health institutions before a complication arises. Besides, rural women had a high workload and problems with transportation to reach health facilities that result in delays in accessing medical care. They are also less likely to deliver in comprehensive hospitals that have specialized NICU and emergency obstetric care as this is found in more urban areas.
Finally, this study found a statistically significant association between occupation and adverse fetal outcomes. Government employees were 81% less likely to develop adverse birth outcomes compared to self-employed. The possible explanation might be that government workers are more likely to be educated and stay aware of the latest pregnancy information by regularly checking updates. In Italy, educated mothers had reduced odds of preterm birth, low birth weight, small for gestational age, and respiratory distress.34 Similarly, in Northwest Ethiopia, mothers who had no formal education were three times higher to have adverse perinatal outcomes.18
Limitation
The finding of this study should be interpreted with the following limitations. Since it is a snapshot, it shares the limitation of cross-sectional study to draw a causal relationship. Due to insufficient count of cases, it was not possible to examine each specific adverse perinatal outcome separately with parity. There may be recall bias on previous obstetric characteristics. In addition, as this was done in the hospital setting, the perinatal outcome of women delivered at home was not assessed. Further, this study does not include adverse perinatal outcomes after 24 hours of birth.
Conclusion and Recommendations
The adverse perinatal outcome was significantly associated with age, residence, occupation, lack of antenatal care, and previous obstetric complications. Parity showed an insignificant association with perinatal outcomes. Reproductive age women should work and improve their economic status to reduce the burden of adverse perinatal outcomes. All pregnant women should attend at least four antenatal care visits starting before 12 weeks of gestation. Additionally, health care providers should early identify and treat complications during antenatal care through good history, physical, and laboratory examination. Skilled birth attendants, ie, midwives, nurses, doctors, health officers, and health extension workers should give attention to both low and grand multiparous women during labor and delivery for their different adverse perinatal outcomes. Particularly, giving attention to grand multiparous women would have a paramount benefit to reduce stillbirth. Further, researchers are recommended to perform longitudinal studies to establish a causal relationship.
Abbreviations
ANC, Antenatal care; APO, Adverse Perinatal Outcomes; DBU, Debre Berhan University; GM, Grand Multipara; LM, Low Multipara; NICU, Neonatal Intensive Care Unit; SPSS, Statistical Package for Social Sciences.
Data Sharing Statement
The data sets are available from the corresponding author and can be shared upon reasonable request.
Acknowledgments
The authors are grateful to Debre Berhan University (DBU) for approval and financing the study. We would also like to extend our appreciation to the study participants, data collectors, and supervisors.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The study was funded by Debre Berhan University. Every phase of the study was evaluated and monitored by the College of Health Sciences. The funder has no role in the design, analysis, and interpretation of the study.
Disclosure
The authors declare no conflicts of interest for this work.
References
1. Bililign Yimer N, Tenaw Z, Solomon K, Mulatu T. Inadequate prenatal visit and home delivery as determinants of perinatal outcomes: does parity matter? J Pregnancy. 2019;2019. doi:10.1155/2019/9024258
2. Wojcieszek A, Frøen JF, Lawn JE, et al. Ending preventable stillbirths. An executive summary for The Lancet’s series. TheLancet. 2016:1–8. Available from: https://www.thelancet.com/pb/assets/raw/Lancet/stories/series/stillbirths2016-exec-summ.pdf.
3. Muniro Z, Tarimo CS, Mahande MJ, Maro E, Mchome B. Grand multiparity as a predictor of adverse pregnancy outcome among women who delivered at a tertiary hospital in Northern Tanzania. BMC Pregnancy Childbirth. 2019;19(1):1–8. doi:10.1186/s12884-019-2377-5
4. Simonsen SE, Varner MW. Grand Multiparity. United States: UpToDate; 2014.
5. Roberman J, Emeto TI, Adegboye OA. Adverse birth outcomes due to exposure to household air pollution from unclean cooking fuel among women of reproductive age in Nigeria. Int J Environ Res Public Health. 2021;18(2):634. doi:10.3390/ijerph18020634
6. Tamirat KS, Sisay MM, Tesema GA, Tessema ZT. Determinants of adverse birth outcome in Sub-Saharan Africa: analysis of recent demographic and health surveys. BMC Public Health. 2021;21(1):1–10. doi:10.1186/s12889-021-11113-z
7. Abdo RA, Halil HM, Birhanu LZ, Defara DA, Kebede BA. Prevalence and associated factors of adverse birth outcome among deliveries at Butajira hospital, Southern Ethiopia. J Gynecol Womens Health. 2019;15(4):555920.
8. Degno S, Lencha B, Aman R, et al. Adverse birth outcomes and associated factors among mothers who delivered in Bale zone hospitals, Oromia Region, Southeast Ethiopia. J Int Med Res. 2021;49(5):030006052110132. doi:10.1177/03000605211013209
9. Tsegaye B, Kassa A. Prevalence of adverse birth outcome and associated factors among women who delivered in Hawassa town governmental health institutions, south Ethiopia, in 2017. Reprod Health. 2018;15(1):1–10. doi:10.1186/s12978-018-0631-3
10. Mgaya AH, Massawe SN, Kidanto HL, Mgaya HN. Grand multiparity: is it still a risk in pregnancy? BMC Pregnancy Childbirth. 2013;13(1):1–8. doi:10.1186/1471-2393-13-241
11. Al-Shaikh GK, Ibrahim GH, Fayed AA, Al-Mandeel H. Grand multiparity and the possible risk of adverse maternal and neonatal outcomes: a dilemma to be deciphered. BMC Pregnancy Childbirth. 2017;17(1):1–7. doi:10.1186/s12884-017-1508-0
12. Al-Farsi YM, Brooks DR, Werler MM, Cabral HJ, Al-Shafaee MA, Wallenburg HC. Effect of high parity on occurrence of some fetal growth indices: a cohort study. Int J Womens Health. 2012;4:289. doi:10.2147/IJWH.S32190
13. Bekele A, Seyoum G, Tesfaye K, Fantahun Y. The effects of maternal age and parity on the birth weight of newborns among mothers with singleton pregnancies and at term deliveries. Ethiop J Health Dev. 2019;33(3):182–187.
14. Asiki G, Baisley K, Newton R, et al. Adverse pregnancy outcomes in rural Uganda (1996–2013): trends and associated factors from serial cross sectional surveys. BMC Pregnancy Childbirth. 2015;15(1):1–12. doi:10.1186/s12884-015-0708-8
15. Nijiru J, Biryabarema C, Kagawa M. Fetal outcomes among grand multiparous and multiparous women in Mulago hospital, Uganda. East Afr Med J. 2013;90(3):84–88.
16. Shah PS; Knowledge Synthesis Group on Determinants of LBW/PT births. Parity and low birth weight and preterm birth: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2010;89(7):862–875. doi:10.3109/00016349.2010.486827
17. Lugobe HM, Muhindo R, Kayondo M, et al. Risks of adverse perinatal and maternal outcomes among women with hypertensive disorders of pregnancy in southwestern Uganda. PLoS One. 2020;15(10):e0241207. doi:10.1371/journal.pone.0241207
18. Getaneh T, Asres A, Hiyaru T, Lake S. Adverse perinatal outcomes and its associated factors among adult and advanced maternal age pregnancy in Northwest Ethiopia. Sci Rep. 2021;11(1):1–12. doi:10.1038/s41598-021-93613-x
19. Okonofua FE, Ntoimo LFC, Ogu R, et al. Prevalence and determinants of stillbirth in Nigerian referral hospitals: a multicentre study. BMC Pregnancy Childbirth. 2019;19(1):1–9. doi:10.1186/s12884-019-2682-z
20. Nonterah EA, Agorinya IA, Kanmiki EW, et al. Trends and risk factors associated with stillbirths: a case study of the Navrongo War Memorial Hospital in Northern Ghana. PLoS One. 2020;15(2):e0229013. doi:10.1371/journal.pone.0229013
21. World Health Organization (WHO). Success factors for women’s and children’s health: Ethiopia; 2015.
22. Maternal, Neonatal and Child Health | Ethiopia | U.S. Agency for International Development [Internet]; [cited September 30, 2021]. Available from: https://www.usaid.gov/ethiopia/global-health/maternal-and-child-health.
23. Aragaw FA, Mahtemsilllasie M, Jarso H. Grand multiparity and pregnancy related complications among women who gave birth at Jimma University specialized hospital, Jimma, Southwest Ethiopia. Gynecol Obs. 2017;7(4):438.
24. Omole-Ohonsi A, Ashimi AO. Grand multiparity: obstetric performance in Aminu Kano teaching hospital, Kano, Nigeria. Niger J Clin Pract. 2011;14(1):6. doi:10.4103/1119-3077.79231
25. Qamar A, Asif U, Qamar S. Maternal and fetal outcome in grand multipara. PAFMJ. 2015;65(1):135–140.
26. Afzal A, Mahajan N, Firdous N. Pregnancy outcomes in grand multiparous patients: a hospital based study from Jammu and Kashmir, India. Int J Reprod Contracept Obstet Gynecol. 2016;5(3):788–792. doi:10.18203/2320-1770.ijrcog20160585
27. Seyoum E, Bekele A, Tsegaye AT, Birhanu S. Magnitude and determinants of adverse perinatal outcomes in Tefera Hailu Memorial Hospital, Sekota Town, Northern Ethiopia. Glob Pediatr Health. 2021;8:2333794X211015524.
28. Gedefaw G, Alemnew B, Demis A. Adverse fetal outcomes and its associated factors in Ethiopia: a systematic review and meta-analysis. BMC Pediatr. 2020;20:1–12. doi:10.1186/s12887-020-02176-9
29. Berhe AK, Ilesanmi AO, Aimakhu CO, Mulugeta A. Effect of pregnancy induced hypertension on adverse perinatal outcomes in Tigray regional state, Ethiopia: a prospective cohort study. BMC Pregnancy Childbirth. 2020;20(1):1–11. doi:10.1186/s12884-019-2708-6
30. Kebede AS, Muche AA, Alene AG. Factors associated with adverse pregnancy outcome in Debre Tabor town, Northwest Ethiopia: a case control study. BMC Res Notes. 2018;11(1):1–6. doi:10.1186/s13104-018-3932-2
31. Ediris M, Belachew T, Yadassa F, Getu K. Disparities in adverse pregnancy outcomes between advanced maternal age and younger age in Ethiopia: institution based comparative cross-sectional study. Int J Nurs Midwifery. 2018;10(6):54–61. doi:10.5897/IJNM2017.0288
32. Lisonkova S, Haslam MD, Dahlgren L, Chen I, Synnes AR, Lim KI. Maternal morbidity and perinatal outcomes among women in rural versus urban areas. CMAJ. 2016;188(17–18):E456–65. doi:10.1503/cmaj.151382
33. Gebremeskel F, Gultie T, Kejela G, Hailu D, Workneh Y. Determinants of adverse birth outcome among mothers who gave birth at hospitals in Gamo Gofa zone, southern Ethiopia: a facility based case control study. Qual Prim Care. 2017;25(5):259–266.
34. Cantarutti A, Franchi M, Compagnoni MM, Merlino L, Corrao G. Mother’s education and the risk of several neonatal outcomes: an evidence from an Italian population-based study. BMC Pregnancy Childbirth. 2017;17(1):1–10. doi:10.1186/s12884-017-1418-1
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
