Back to Journals » Psychology Research and Behavior Management » Volume 15
Adverse Childhood Experiences (ACEs) in Adults with Cystic Fibrosis
Authors O'Leary C , Edwards V, Hardcastle KA, McCulloch A, Duckers JM
Received 8 March 2022
Accepted for publication 7 June 2022
Published 28 June 2022 Volume 2022:15 Pages 1601—1605
DOI https://doi.org/10.2147/PRBM.S322425
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Igor Elman
Video abstract presented by Catherine O'Leary.
Views: 99
Catherine O’Leary,1 Vivien Edwards,1 Katherine A Hardcastle,2 Anna McCulloch,1 Jamie M Duckers1
1All Wales Adult Cystic Fibrosis Service, Cardiff and Vale University Health Board, Llandough, UK; 2Policy and International Health, WHO Collaborating Centre on Investment for Health & Well-being, Public Health Wales, Wrexham, UK
Correspondence: Catherine O’Leary, Email [email protected]
Objective: This exploratory study examines the prevalence of adverse childhood experiences (ACEs) in adults with cystic fibrosis (CF).
Design: Childhood exposure to 16 ACEs was measured during an annual review assessment (N = 80).
Methods: CF patients (n = 80) attending the All Wales Adult CF Service for a routine annual review assessment completed an adapted version of the Centers for Disease Control and Prevention (CDC) short-form ACE questionnaire alongside measures of psychological well-being.
Results: In this sample, 65 (78%) reported at least one type of childhood adversity and 11 (14%) experienced four or more ACEs. Parental divorce or separation and verbal abuse were the most frequently reported ACEs. Illness related trauma in childhood was also prevalent with 52 (64%) reporting having experienced a painful or frightening medical procedure and 23 (28%) feeling forced to have treatment or a procedure.
Conclusion: Individuals with CF reported a number of childhood traumas including trauma relating to medical procedures. Those with a history of ACEs may have increased risks of emotional and physical difficulties and may benefit from additional support from the CF psychosocial team.
Keywords: adverse childhood experiences, ACEs, cystic fibrosis, trauma, ACE, CF
Introduction
Much of the research examining trauma in early life such as physical, emotional and sexual abuse or witnessing domestic violence describes these adversities as Adverse Childhood Experiences (ACEs). Awareness of ACEs was initially raised by a collaborative study between the Centers for Disease Control and Prevention (CDC) and Kaiser Permanente.1 This research found that people who had experienced adversity in childhood were at a much higher risk for many long term health conditions including cancer, lung disease, heart disease and mental health illness even after controlling for differences in lifestyle choices. There was also a cumulative risk with more ACEs resulting in increased risk; an ACE score of 4 or more substantially increased risks of mental and physical illness and a person with seven or more ACEs had triple the lifetime risk of lung cancer and three and a half times the risk of ischemic heart disease.1 These associations have been confirmed in subsequent global research and ACEs have now been linked with more than 40 negative outcomes including an increased likelihood of health-harming behaviours, obesity, unemployment and a decreased life expectancy.2–6
Berens et al (2017)7 have described the complex interaction between biological mechanisms, resulting in changes to brain structure and activity, changes to the responsiveness of the neuroendocrine system, heightened inflammatory reactivity and changes to microbiome functioning. Through changes across body systems including neurological, immunological and hormonal development, early life trauma becomes “biologically embedded”, increasing risks of common health problems.
A large-scale UK based study8 measured the prevalence of ACEs in a nationally representative sample and examined their association with chronic disease development and health service use in adulthood. A total of 50% of adults in Wales suffered at least one ACE as a child and 14% suffered four or more. As with previous research, exposure to ACEs increased risks of physical and mental health problems. Additionally, those with more ACEs had fewer resilience resources as adults.
Despite the growing body of research, there is currently no published information about the prevalence of ACEs in Cystic Fibrosis (CF) and how this compares with the general population. Children with CF may be protected against early adversity since they are likely to have increased involvement with healthcare agencies throughout childhood. However, evidence suggests that disabled children are more likely to be maltreated and neglected than others.9 Additionally, growth, behaviour and other problems may be overlooked and seen to be the result of a disability.10 Furthermore, treatments in CF are often complex and time-consuming and there is evidence that parents and care-givers perceive this as a high burden11 which may result in strain to family life and finances.12
Individuals with CF may also have an increased risk of experiencing traumas specifically related to living with the condition during childhood such as having to undergo frightening procedures. Given the recognised importance of ACEs in predisposing individuals to chronic ill health, it is important to understand the prevalence of trauma in an adult CF population.
Methods
Patients (n = 82) attending the All Wales Adult CF Service completed an adapted version of the CDC short-form ACE questionnaire at annual review. This questionnaire measures exposure to 11 ACEs before the age of 18. The ACE questionnaire was adapted to include an additional 5 items relating to growing up with CF such as being forced to have a procedure or being frightened by a hospital admission. Each ACE was scored as 1 (exposure to ACE) or 0 (no exposure). ACE Total score was calculated by summing the number of ACEs experienced using only the original 11 items and not medical/health related trauma. Measures of depression (PHQ9) and anxiety (GAD7) and a semi-structured psycho-social interview were also administered. The PHQ9 and GAD7 are short, well validated and commonly used depression and anxiety measures. Both measures can be scored as a continuous variable with a higher score representing higher levels of depression or anxiety. A score of 10 represents a cut point for moderate depression or anxiety.
The annual review is a clinic appointment in which the results of all assessments CF patients have had during the past year are reviewed. At this appointment, patients are reviewed by members of the specialist multidisciplinary team including the CF psychosocial team. Cardiff and Vale University Health Board deemed this work a service evaluation and ethical approval was not required. The ACE questionnaire was incorporated as part of the psychosocial routine assessment which was conducted face to face with either a clinical psychologist or social worker. The purpose of assessing ACEs was explained to patients who could choose to complete the questionnaire having given verbal consent. A total of 2 patients declined to complete the ACE assessment. Lung function was assessed at the same time as part of the annual review. Associations between ACE Total score and other variables was assessed using Pearson’s correlation.
Results
A total of 80 patients (29 female and 51 male) completed the measures. Mean age was 32 years (range: 18–58) and mean FEV1 was 69% predicted (range: 21–116). On the anxiety scale the mean score fell in the normal range (4.7; range: 0–18) and on the depression scale the mean score fell in the mild range (5.2; range 0–18). The overall prevalence of ACEs (not including exposure to medical/health related trauma) is shown in Figure 1, and Table 1 shows the prevalence of each individual ACE.
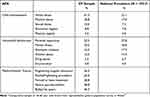 |
Table 1 The Prevalence of Each Individual ACE in a CF Population, Compared with National Prevalence Data for the Whole Population |
 |
Figure 1 The prevalence of total ACEs reported (N = 80). |
There was a significant correlation between number of ACEs reported and depression and anxiety; between PHQ9 and ACE total r = 0.35 (p = 0.002) and between GAD7 and ACE total r = 0.30 (p = 0.008). There was no significant relationship between ACE total score and FEV1% predicted, gender or age (p > 0.05).
Discussion and Conclusions
Our results show that ACEs in an adult CF population are prevalent and similar to those found in the Welsh general population. Higher levels of parental separation and verbal abuse may relate to the difficulties of raising a child with a chronic health condition.11–13
Our study also found childhood medical trauma relating specifically to having CF is widespread. The most prevalent was the experience of having a painful or frightening medical procedure. Around a third reported being forced to have a procedure in childhood. There is some evidence to suggest that experience of restraint to deliver treatment is linked to speech and language problems, distrust of medical care, post-traumatic stress disorder (PTSD) and a negative self-image14 and should only be used when there is no reasonable alternative.15 A history of trauma, especially that occurring in a health setting, is likely to impact on trust in professionals and adherence to treatment and may be an additional risk factor for poor outcomes. While this study did not show a link between ACE score and current physical health, future research could focus on the relationship between changes in respiratory health and ACEs in a larger population of CF patients.
Possible limitations of this study include the risk of memory bias on self-report, retrospective data. Some researchers have attempted to address this using both prospective and retrospective methods of data collection16 but this is also methodologically challenging as prospective data are usually provided by proxy, for example by parents and teachers, and there is likely to be under-reporting by proxy reporters who are unaware of a trauma.
Whilst the link between childhood trauma and future health has been demonstrated in numerous studies, Anda et al17 have recently cautioned against the use of an ACE questionnaire as a screening tool and recommend that it should not be used as a diagnostic tool to measure risk at the individual level. They describe an ACE score based on 10 childhood traumas as a “relatively crude measure of cumulative childhood stress exposure”. The questionnaire, like the adapted one used in this study, does not account for factors such as intensity, frequency or timing of the stressor, or protective factors such as social support. As we have seen in this study, children may be exposed to stressors not included in the 10 ACE questionnaire such as traumas relating to a health condition.
Given the high prevalence of childhood stress, including stress related to growing up with CF, we recommend that a wider medical history which considers ACEs, medical and CF related trauma, in addition to factors such as resilience and social support, should become a routine part of the care of adults with CF. Talking to CF patients about their exposure to childhood trauma is more likely to measure prevalence rather than waiting for individuals to spontaneously disclose information as victims of childhood abuse have been found to wait from between 9 to 16 years before disclosure with many never doing so.18
Reducing a comprehensive psychosocial assessment to the use of an ACE screening tool is unlikely to be helpful to individuals or healthcare professionals. Whilst there is evidence to suggest that screening tools are considered acceptable by individuals with or without trauma,19 recalling childhood trauma such as sexual abuse is likely to be distressing. Recent research looking at acceptable ways to assess ACEs in CF populations20 suggests that individuals with CF may be more comfortable disclosing ACEs as a total number experienced, rather than disclosing each individual ACE and would prefer a conversation about ACEs to be separate from their clinical appointment. Furthermore, a mismanaged assessment with poorly trained professionals may not only be distressing but has the potential to be retraumatising for the individual.21 It is also important that there is the availability of after-care and ongoing support if needed. Psychosocial professionals within CF teams, who are able to provide follow-up care, are well placed to ask adult CF patients about their experience of trauma in childhood in a safe and sensitive manner.
By assessing early life adversity, CF teams can provide trauma informed care which takes these experiences into account when planning care and psychosocial support to help mitigate risks.
Data Sharing Statement
Raw data were generated at the All Wales Cystic Fibrosis Service, Cardiff and Vale University Health Board. Derived data supporting the findings of this study are available from the corresponding author [CJO] on request.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Felitti VJ, Anda RF, Nordenberg D, et al. The relationship of adult health status to childhood abuse and household dysfunction. Am J Prev Med. 1998;14:245–258. doi:10.1016/S0749-3797(98)00017-8
2. Waite R, Shewokis PA. Childhood trauma and adult self-reported depression. ABNF J. 2012;23:8–13.
3. Lu W, Mueser KT, Rosenberg SD, Jankowski MK. Correlates of adverse childhood experiences among adults with severe mood disorders. Psychiatr Serv. 2008;59:1018–1026. doi:10.1176/ps.2008.59.9.1018
4. Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet. 2017;2:e356–e366. doi:10.1016/S2468-2667(17)30118-4
5. Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span. JAMA. 2001;286(24):3089–3096. doi:10.1001/jama.286.24.3089
6. Bellis MA, Hughes K, Ford K, Rodriguez GR, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Health. 2019;4(10):e517–e528. doi:10.1016/S2468-2667(19)30145-8
7. Berens AE, Jensen SKG, Nelson CA. Biological embedding of childhood adversity: from physiological mechanisms to clinical implications. BMC Med. 2017;15:135. doi:10.1186/s12916-017-0895-4
8. Hughes K, Ford K, Davies AR, Homolova L, Bellis MA. Sources of Resilience and their Moderating Relationships with Harms from Adverse Childhood Experiences. Cardiff: Public Health Wales; 2018. Available from: http://www.wales.nhs.uk/sitesplus/documents/888/ACE%20&%20Resilience%20Report%20(Eng_final2).pdf.
9. Leeb RT, Bitsko RH, Merrick MT, Armour BS. Does childhood disability increase risk for child abuse and neglect? J Ment Health Res Intellect Disabil. 2012;5(1):4–31. doi:10.1080/19315864.2011.608154
10. Sullivan PM, Knutson JF. Maltreatment and disabilities: a population-based epidemiological study. Child Abuse Negl. 2000;24(10):1257–1273. doi:10.1016/S0145-2134(00)00190-3
11. Glasscoe C, Hope HF, Lancaster GA, et al. Development and preliminary validation of the challenges of living with cystic fibrosis (CLCF) questionnaire: a 46-item measure of treatment burden for parent/carers of children with CF. Psychol Health. 2022;8:1–25. doi:10.1080/08870446.2021.2013483
12. Fitzgerald C, George S, Somerville R, Linnane B, Fitzpatrick P. Caregiver burden of parents of young children with cystic fibrosis. J Cyst Fibros. 2018;17(1):125–131. doi:10.1016/j.jcf.2017.08.016
13. Namkung EH, Song J, Greenberg JS, Malik MR, Floyd FJ. The relative risk of divorce in parents of children with developmental difficulties: impacts on lifelong parenting. J Intellect Dev Disabil. 2015;7(1):33–50. doi:10.1352/1944-7558-120.6.514
14. Brenner M. Child restraint in the acute setting of pediatric nursing: an extraordinarily stressful event. Issues Compr Pediatr Nurs. 2007;30(1–2):29–37. doi:10.1080/01460860701366658
15. Royal College of Nursing. ‘Restrictive physical intervention and therapeutic holding for children and young people’. Guidance for nursing staff; 2010. Available from: http://www.rcn.org.uk/__data/assets/pdf_file/0016/-312613/003573.pdf.
16. Houtepen LC, Heron J, Suderman MJ, et al. Adverse childhood experiences in the children of the Avon longitudinal study of parents and children (ALSPAC) [Version 1; peer review: 3 approved]. Wellcome Open Res. 2018;3:106. doi:10.12688/wellcomeopenres.14716.1
17. Anda RF, Porter LE, Brown DW. Inside the adverse childhood experience score: strengths, limitations, and misapplications. Am J Prev Med. 2020;59(2):293–295. PMID: 32222260. doi:10.1016/j.amepre.2020.01.009
18. Read J, McGregor M, Coggan C, Thomas DR. Mental health services and sexual abuse: the need for staff training. J Trauma Dissociation. 2006;7(1):33–50. doi:10.1300/J229v07n01_04
19. Goldstein E, Athale N, Sciolla AF, Catz SL. Patient preferences for discussing childhood trauma in primary care. Perm J. 2017;21:16–055. doi:10.7812/TPP/16-055
20. Williams WA
21. Leasy M, O’Gurek DT, Savoy ML. Unlocking clues to current health in past history: childhood trauma and healing. Fam Pract Manag. 2019;26(2):5–10. PMID: 30855124.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
