Back to Journals » Patient Preference and Adherence » Volume 17
Adherence to Self - Care Practice Among Type 2 Diabetes Mellitus Patients Using the Theory of Planned Behavior and Health Belief Model at Comprehensive Specialized Hospitals of Amhara Region, Ethiopia: Mixed Method
Authors Simegn W , Mohammed SA , Moges G
Received 27 July 2023
Accepted for publication 10 December 2023
Published 13 December 2023 Volume 2023:17 Pages 3367—3389
DOI https://doi.org/10.2147/PPA.S428533
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Johnny Chen
Wudneh Simegn,1 Solomon Ahmed Mohammed,2 Getachew Moges2
1Department of Social and Administrative Pharmacy, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 2Department of Pharmacy, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Correspondence: Wudneh Simegn, Email [email protected]
Background: Diabetes mellitus is one of the major public health problems that requires appropriate self-care practices to reduce complications. The current study assessed adherence to self-care practices and associated factors using the theory of planned behavior and the health belief model among type 2 diabetes mellitus patients.
Methods: A facility-based, sequential explanatory mixed-method was undertaken at comprehensive specialized hospitals in the Amhara region of Ethiopia. A single population proportion formula was used to calculate sample size. Proportional allocation to the three study settings and systematic random sampling techniques were used to select 846 study participants. Logistic regression analysis was used to identify associated factors. Variables with a P-value less than 0.05 were declared statistically significant. For the qualitative study, purposive sampling was used to select sixteen key informants, and thematic analysis was performed.
Results: About 42.4% of the study participants had good adherence to self-care practices. Being a member of a diabetes association (AOR = 2.57, 95% CI: 1.51, 4.38), having a home glucometer (AOR = 2.52, 95% CI: 1.59, 4.02), having good glycemic control (AOR = 4.07, 95% CI: 2.53, 6.53), having low perceived barriers (AOR = 8.65, 95% CI: 4.65, 16.07), and having middle perceived barriers (AOR = 3.26, 95% CI: 1.88, 5.66) were significantly associated with good adherence to self-care practice. On the other hand, poor wealth index (AOR = 0.27, 95% CI: 0.16, 0.46), poor behavioral control (AOR = 0.59, 95% CI: 0.36, 0.97), poor behavioral intention (AOR = 0.36, 95% CI: 0.21, 0.64), low perceived benefits (AOR = 0.20, 95% CI: 0.08, 0.51), and middle perceived benefits (AOR = 0.57, 95% CI: 0.31, 0.83) were significantly associated with poor adherence to self-care practice. The key informants explored the influence of patients’ beliefs, self-efficacy, social support, and barriers on their self-care practices.
Conclusion: Less than half of type 2 diabetes mellitus patients had good adherence to self-care practices. This was more evident for patients who are members of a diabetes association, having a high wealth index, having a home glucometer, good behavioral control, good behavioral intentions, high perceived benefit, and poor perceived barriers. Appropriate intervention should be designed based on the aforementioned factors.
Keywords: adherence, health belief model, self-care practice, theory of planned behavior, type 2 diabetes mellitus
Introduction
The prevalence of diabetes mellitus (DM) is on a concerning rise globally. Current estimates indicate that 537 million people are affected by diabetes, with projections indicating a potential increase to 643 million by 2030 and 783 million by 2045.1 The higher prevalence is observed in Type 2 Diabetes mellitus (T2DM) which constitutes about 90 to 95% of DM patients.2,3 It is one of the top 10 causes of death and has a major impact on the lives and well-being of individuals, families, and societies across the world.2 In Ethiopia, more than 2.6 million adults were living with DM as evidenced in 2019.4
Self-care is critical for achieving the best glucose results and reducing complications such as amputation, nephropathy, neuropathy, retinopathy, cardiovascular disease, erectile dysfunction, depression, and skin lesions.5,6 For that matter, people living with diabetes are expected to be actively involved in their care by performing many complex self-care behaviors, including dietary control, regular exercise, psychosocial coping skills, medication use, and self-monitoring of Fasting Blood Sugar (FBS). Several studies have found that patient education programs, social support, self-efficacy, and a positive attitude can improve DFM self-care and maintain good glycemic control.5,7–9
A systematic review in Ethiopia showed the overall pooled prevalence of good DM self-care practice was 49%.10 Several studies were also conducted in Ethiopia to assess the magnitude of adherence to self-care practices. The finding of adherence to self-care practice indicated 48.0% in Addis Ababa;11 54.2% in Jimma Medical Center;12 55.8% in Dessie;13 42.7% in western Ethiopia;14 55.9% in Dire Dawa;15 63.8% in Dubti and Assaita hospitals;16 63.1% in Debre-Tabor Hospital;17 38.1% in Harar and Dire Dawa;18 54.3% in Benishangul Gumuz;19 28.4% in Bahir Dar Hospitals;20 and 60.3% in Addis Ababa public hospitals.21
Different socio-demographic factors and clinical conditions were reported to have a relationship with the adherence to self-care practices of people living with diabetes. Being female,12,22,23 having higher educational levels,13,15,22,24,25 and employing DM patients11,22 have good adherence to the recommended self-care practices and reduce the associated complications. Longer duration of diagnosis,8,24 DM patients with comorbidities,14,23,24 being members of the DM association,21 having DM education from health professionals,13,15–17,21 and having a glucometer at home11,13–15,17 also have better adherence to self-care practices. Patients with a higher income level had an impact on having good self-care practice among DM patients.12,15,26 In contrast to this, lower income levels are also reported to have better self-care practices.16,27
However, there have been no studies conducted employing both the Theory of Planned Behavior (TPB) and the Health Belief Model (HBM), along with a qualitative approach, to assess adherence to self-care practices and associated factors among T2DM patients. For a better understanding of reasons for poor adherence and associated factors of self-care practice, in-depth interviews can support the quantitative method to guide the design of interventions.28 Therefore, it is necessary to identify factors influencing the T2DM patients’ adherence to self-care practices and suggest an appropriate plan to the stakeholders. Therefore, the current study aimed to assess adherence to self-care practices and associated factors among T2DM patients through the integration of TPB and HBM with an explanatory sequential mixed study design at Comprehensive Specialized Hospitals (CSH) in the Amhara region of Ethiopia.
Methods
Study Design
A facility-based, mixed-methods sequential explanatory study was undertaken. A cross-sectional study design was employed for the quantitative approach, and a phenomenological study design was used for the qualitative approach. The mixed-methods design was chosen because it is an approach considering multiple perspectives and having methodological pluralism while maintaining a focus on people and their perceptions and experiences.29 It helps to provide richer data and to initiate new modes of thinking by attending to paradoxes that emerge from the two data sources.
Study Setting and Period
The research was conducted at three public CSHs, namely Tibebe Gion, Debre Tabor, and Dessie, situated in the Amhara region of Ethiopia. The Amhara Regional State is located in the Northwestern and North Central parts of Ethiopia. The region was selected due to the various socio-cultural experiences that are found across the population. In Ethiopia, the CSH is a health facility at the tertiary level of health care that provides curative and rehabilitative services. In the Amhara region, there were 84 hospitals (primary, general, and CSH), of which eight are CSHs and referral centers for general hospitals.30 The CSHs was selected as a study setting due to its service delivery to a higher number of DM patients with several socio-demographic characteristics.
Tibebe Ghion CSH is a teaching hospital of Bahir Dar University located in Bahir Dar, which is 565 km away from Addis Ababa, the capital city of the country. In the outpatient department service, an average of 400 T2DM patients attend DM follow-up clinics per month. Debre Tabor CSH is found in Debre Tabor town, in the South Gondar zone of Amhara Regional State. The town is 667 km away from Addis Ababa. About 600 T2DM patients are attending DM follow-up clinics per month. Dessie CSH is found in Dessie City, northeast Ethiopia. The City is located 401 kilometers from Addis Ababa. About 650 T2DM patients are attending DM follow-up clinics per month. The study was conducted from June 30–August 30, 2022.
Source of Population
The source of the population was all T2DM patients who were getting DM follow-up at the three CSHs in Amhara regional state.
Study Population
The study population was T2DM patients who were selected by sampling procedures and fulfilled the inclusion criteria.
Inclusion and Exclusion Criteria
T2DM patients over the age of 18 who were attending the selected CSHs one year after their diagnosis were included. Patients were excluded if they were pregnant, unable to communicate (having hearing problems), had mental problems (depression, stress, or anxiety), or severely ill for both study designs during the data collection period.
Sample Size Calculation and Sampling Technique
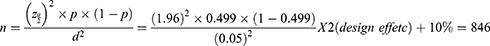
For the quantitative study, the sample size was calculated using a single population proportion formula with the assumptions of a 95% confidence interval (CI), a marginal error (d) of 5%, and based on the previous study conducted in Gondar with HBM (low perceived severity = 49.9%).24 Considering the design effect (two stages) and adding a 10% non-response rate, the final sample size was 846.
The three CSHs, Tibebe Ghion CSH, Debre Tabor CSH, and Dessie CSH, were selected by lottery method out of a total of eight CSHs. The number of T2DM patients attending DM follow-up clinics per month was taken from each selected CSH. The sample size was proportionally allocated to each of the selected CSHs. A systematic random sampling technique was used by calculating the K value using the sampling frame from each selected CSHs (Figure 1). The sampling frame (list of patients) was obtained from the registration books of each follow-up clinic in the CSHs. The lottery method was used to select the first T2DM patient.
 |
Figure 1 Schematic presentation of the sampling procedure for the assessment of adherence to self-care practice among T2DM patients at CSHs of Amhara Region, Ethiopia (n=794). |
A purposive sampling technique was used for the qualitative study. The study participants were selected with the help of health professionals working in the study setting. Patients from different groups, such as age, sex, educational level, income level, duration of diagnosis or follow-up, and patient’s residence, were selected. Sixteen patients were used for in-depth interviews, considering the saturation of information about emerging themes. It was discontinued at the point where relative saturation of the topic had been achieved (16 in-depth interviews).
Data Collection Instrument
For the quantitative study, the instrument had four parts. Part one included items about patients’ socio-demographics, clinical, and socio-economic information. Part two included a Summary of Diabetes Self-Care Activities (SDSCA) with some modifications. Self-care activities during the past 7 days were assessed using 5 domains (diet, physical exercise, medication, blood glucose testing, and foot care). The items were adapted from the a previous study.17
Part three included the constructs of TPB. The constructs were based on TPB constructs by Ajzen (1991), from the TPB manual for health services researchers, and from previous studies.31–33 The instrument has been validated among Spanish people and resulted in a Cronbach alpha of 0.7834 and was also used in Ghana, which indicated fit to African countries.35
Part four included constructs of HBM. Questionnaires to assess the constructs of HBM were adopted from Becker and Janz (1985) developed a 16-items DM HBM Scale,36 which have been proven to be reliable from previous study in Ethiopia.24,37–39
For the phenomenological study design, a semi-structured interview guide was prepared to explore ideas among 16 T2DM patients. It had two parts. Part 1 included questions related to basic sociodemographic information and the duration of DM (sex, age, level of education, residence, and duration of diagnosis). Part 2 included nine semi-structured questions, followed by probes to support the constructs of TPB and HBM.
Pilot Study and Procedure
For the quantitative study design, a pilot study was conducted to ascertain the validity and reliability of the instruments. The TPB manual also recommended the piloting of the questionnaire by more than five respondents to check clarity for respondents.31 A pilot study was conducted with the same inclusion criteria as the main study among T2DM patients who were not part of the main study. About 30 T2DM patients were selected. The validity and reliability tests were checked to use the questionnaire for the main study. Factor analysis (principal component analysis) was used for validity, and Cronbach’s alpha was used for reliability testing to assure the cultural adaptability of Ethiopia.34 A pilot was conducted among two patients to assess the ease of understanding of the interview guide and process. Based on the pilot study, the interview guide was made with a few modifications.
Forward and Back Translation Procedures
The principal investigator prepared all the items in English. One professional has performed the translation from English to Amharic. This forward translation was then translated by a second professional back to Amharic. There was no difference between the two English versions.
Data Collection Procedure
The data collection had two phases. The quantitative data collection has been conducted in the first phase. Six data collectors with previous experience in data collection and three professional supervisors were recruited. One supervisor and two data collectors were assigned to each study setting. Intensive follow-up was implemented in each study setting by the supervisors. The DM follow-up days were pre-informed by each CSH. Study participants were contacted during their outpatient visit to the diabetes center at each CSH. The data was collected through face-to-face interviews with study participants, from whom informed consent was obtained.
The second phase was the qualitative data collection. The principal investigator conducted all recruitment and in-depth interviews with one professional assistant. The patients were individually asked for consent after being informed about the purpose of the study. They were also assured that their participation was voluntary, and they were at liberty to withdraw at any time during the interview.
The venue of the in-depth interview was the free space at the CSH compound. The investigator also used additional phone interviews due to a shortage of time at the CSH. All interviews were audio-recorded by obtaining permission from the study participants and taking notes on the key issues and observations. The interview lasted between 26 and 35 minutes.
The interviews were transcribed verbatim in Amharic and then translated into English for data analysis. The interviews were guided by a topic guide that allowed for the exploration of the main themes. Probes for each question were used as necessary to elicit further comments, and participants were encouraged to share their ideas in case they had anything related to the topic. All the information from the interview was documented by the investigator.
Quality Control
The current research used mixed methods, which allow the integration of quantitative and qualitative data to increase the integrity of the research and its internal validity. For the quantitative study, the researcher attempted to check the validity and reliability of the tools by factor analysis (principal component analysis) and Cronbach’s alpha coefficient, respectively, on the pilot study to assure the cultural adaptability and internal consistency of the tools. The Cronbach’s alpha coefficient for all variables was above the 0.7 value, which indicated acceptable internal consistency.40 Training was given to the supervisors and data collectors for half a day on objectives, methods, the study instrument, the ethics of the study, and the data collection procedure by the principal investigator. The supervisors had daily meetings with the principal investigator on the phone.
For the qualitative study, sensitivity to context, commitment, coherence, impact, and importance were used to guide the qualitative data collection and analysis. The interview guide has been evaluated by the two senior professionals from the department of pharmacy. A few amendments were made based on the discussion. Theoretical triangulation, methodological triangulation, and investigator triangulation were also undertaken to enhance the validity. The principal investigator created a good rapport with potential participants. The researcher addressed any issues and got additional points and comments. The researcher has separated himself from the text through his understanding in a reflective way.
Reflexivity
Issues of Reflexivity: The Principal Investigator Status as an Insider
The principal investigator is a senior pharmacy professional who can offer certain strengths and limitations for this study. He was non-judgmental during the in-depth interview and maintained professionalism. He operated with an awareness of insider bias in his work and justified how other key informants responded to him. He had tried to eliminate much subjectivity at the stages of data collection and analysis. In order to achieve bracketing, the researcher was mentally prepared throughout the research process by putting aside his own knowledge, examining his thoughts and consciousness, maintaining his curiosity in the area, following the cues of participants, using semi-structured interviews with probing interesting areas, focusing but not leading, suspending predisposition during data analysis, and introducing measures to enhance the trustworthiness of the data analysis.41
Variables of the Study
Dependent variable: Adherence to self-care practice.
Independent Variables: Socio-demographic information included sex, age, marital status, religion, residence, educational level, and occupation. Socio-economic information included the average monthly income and wealth index. Clinical and related information included items such as having ever read any books about diabetes, using social media as a source of information, receiving training or DM education about DM, being a member of a DM association, using health professionals as a source of information, using cigarette, Khat, and alcohol, the length of time living with DM, the current eye status, having a family history of DM, having diabetes foot ulcers, having comorbidity, having a glucometer at their house, using drugs or herbs to treat their DM without a prescription in the last three months, and the current FBS. The TPB constructs included attitude, subjective norms, behavioral control, and behavioral intention. The HBM constructs included perceived susceptibility, perceived severity, perceived benefit, and perceived barriers.
Operational Definition
Adherence to Self-Care Practice
The five domains of self-care practice, such as dietary practices, regular exercise, foot care, medication, and blood glucose monitoring, were measured by twelve items. Adherence to self-care was defined as “good” if the respondents scored the mean (the data was normally distributed) and above of the overall self-care practice score (minimum score 0 and maximum score 84), as explained in the previous studies elsewhere.8,15,19,24,39,42,43
TBP Constructs
For each construct of the TPB model (attitude, subjective norm, behavioral control, and behavioral intention), study participants were dichotomized as good or poor for each construct based on the summed score of the Likert scale questions. Scores above the mean (all the data measuring the four constructs were normally distributed) were considered to indicate having a good attitude toward self-care practice, having good subjective norms toward self-care practice, having good behavioral control toward self-care practice, and having good intention toward self-care practice. This cut point is based on the manual of TPB.31
HBM Constructs
All the constructs of the HBM were measured as high, medium, and low if the respondents scored above 75%, between 50% and 75%, and below 50% of the summed score of the Likert scale questions, respectively, similar to the previous study.24
Good Glycemic Control
Study participants with FBS levels ranging from 70 to 130 mg/dL.
Data Management and Statistical Analysis
For the quantitative measurements, the data was collected by the application of Kobo Collect on smartphones and tablets. The Electronic Kobo Collect data collection tool has been used in the previous study as it can be run offline, making it possible to collect data anywhere and facilitating data sharing between the data collectors and the investigator.44 The collected data was transmitted online, as the data tabulation process is automatic. This reduced the cost by avoiding paper duplication and allowing easy reporting and daily monitoring of the data collection process. At the final stage of the data collection, it was exported to SPSS version 26 for analysis. Descriptive statistics (frequency, mean, and percentage) were computed to describe variables. Cronbach’s alpha coefficient of internal consistency was used to check the reliability of all scales. Principal component analysis was used as an extraction method for factor loading. Skewness and kurtosis were used to test the normal distribution of data to use the mean for dichotomization.
Bi-variable logistic regression was used to identify candidate variables for multiple logistic regressions. Variables with a P-value ≤0.2 were candidate variables for multivariable logistic regression. Backward regression was used to eliminate variables in the multiple logistic regression. Multiple logistic regression was used to identify independent variables that were significantly associated with the outcome variables. All variables with a p-value <0.05 were declared to be associated with adherence to self-care practices. The qualitative data was exported to open-code software. The investigator coded after repeatedly reading the transcriptions. A thematic analysis approach was used to categorize the codes through several iterations. The result was written in narrative form under each theme, and double quotation marks were used to present the direct quotes of key informants.
Results
Quantitative Findings
Psychometric Characteristics of the Tool
The Cronbach’s alpha reliability and factor analysis for validity of each scale in the pilot study were checked to assure the cultural adaptability of the tool in Ethiopia. The Cronbach’s alpha test was 0.951, 0.882, 0.881, 0.911, 0.902, 0.807, 0.903, 0.883, and 0.915 for self-care practice, attitude, subjective norms, behavioral control, behavioral intention, perceived severity, perceived susceptibility, perceived benefit, and perceived barriers, respectively. All the Cronbach’s alpha reliability results showed acceptable internal consistency (> 0.7). Variation inflation factor and Pearson correlation were used to assure the absence of multicollinearity among independent variables. The determinant value for items assured that the data was fit for factor analysis. Principal component analysis has been used as an extraction method for factor loads for all variables. The extraction sums of squared loadings for items of all measured variables were one-factor loadings. This indicated that the data yielded by each scale is unidimensional and representative of a single underlying construct.
Socio Demographic and Economic Information of Study Participants
In the current study, seven hundred and ninety-four participants were enrolled, giving an overall response rate of 93.85%. Three hundred and seventy (46.6%) were females. The mean age of the participants was 54.12, with a standard deviation (SD) of 11.268, and ranged from 34 to 89 years. Approximately 28.8% of the participants in the study were employed, with merchants comprising 28.2% and housewives accounting for 19.9%. The wealth index of the participants was classified into poor (27.7%), middle (39.8%), and rich (32.5%) categories (Table 1).
 |
Table 1 Socio-Demographic and Socio-Economic Variables Among T2DM Patients at CSHs of Amhara Region, Ethiopia (n=794) |
Clinical and Related Information of Study Participants
A total of three hundred and thirty-two participants (41.8%) had read books pertaining to DM. Approximately 43.3% had encountered information about DM management through social media, while around 40.4% had received training or education on DM. Additionally, only 19.8% of the patients were affiliated with DM associations. More than two-thirds of the study participants (69.3%) had been told to have regular self-care practices to manage their DM by their healthcare providers. About 29.5% of study participants had a family history of DM. More than two-thirds of the study participants (70.2%) had at least one comorbidity; 13.5% of the study participants had diabetes foot ulcers; and 7.2% of the study participants had diabetes retinopathy. Only 22% of the study participants had a glucometer at home. About 76.3% of participants had good glycemic control (FBS = 70–130 mg/dL) (Table 2).
 |
Table 2 Clinical and Related Information Among T2DM Patients at CSHs of Amhara Region, Ethiopia (n=794) |
The Level of Constructs Under TPB
Approximately 54.7% of the participants in the study exhibited a positive attitude. Similarly, around 62.7% demonstrated good subjective norms, and approximately 66.2% displayed good behavioral control. Moreover, a substantial majority, about 72.5%, showcased positive behavioral intentions (Figure 2).
 |
Figure 2 Respondents’ distribution to the level of constructs under TPB at CSHs of Amhara Region, Ethiopia (n=794). |
The Level of Constructs Under HBM
A significant majority of the study participants reported high levels of perceived severity (70.2%), perceived susceptibility (74.3%), perceived benefit (73.3%), and perceived barrier (71.8%) (Figure 3).
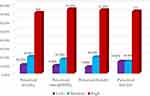 |
Figure 3 Respondents’ distribution to the level of constructs under HBM at CSHs of Amhara Region, Ethiopia (n=794). |
Adherence to Self-Care Practice Among T2DM Patients
In this study, approximately 42.4% (95% CI: 38.9%, 46.0%) of the participants demonstrated good adherence to self-care practices. Employing their mean value as a threshold, it was found that 66.4% of the participants exhibited inadequate adherence to the recommended blood sugar testing. Additionally, over half (55.0%) of the study participants displayed insufficient adherence to the recommended foot care, while more than two-thirds (70.8%) demonstrated good adherence to the prescribed medication by their physicians (Figure 4).
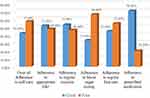 |
Figure 4 Adherence to self-care practice among T2DM patients at CSHs of Amhara Region, Ethiopia (n=794). |
Associated Factors of Adherence to Self-Care Practice
In this study, variables such as having previously read books about DM, receiving information about DM management through social media, undergoing training or education about DM, being a member of a DM association, having a family history of DM, possessing a glucometer, achieving glycemic control, wealth index, behavioral control, behavioral intention, perceived benefit, and perceived barriers were considered as candidate variables for multiple logistic regression (with a p-value less than 0.2).
In the final model, being a member of a DM association had 2.57 times (adjusted odds ratio (AOR) = 2.57, 95% CI: 1.51, 4.38) better adherence to self-care practices as compared to those study participants who were not members of a diabetic association. DM patients with a home glucometer had 2.52 times (AOR = 2.52, 95% CI: 1.59, 4.02) better adherence to self-care practices than their counterparts. DM patients with good glycemic control had 4.07 times (AOR = 4.07, 95% CI: 2.53, 6.53) better adherence to self-care practice than DM patients with poor glycemic control. Study participants with low perceived barriers had 8.65 times (AOR = 8.65, 95% CI: 4.65, 16.07), and those with middle perceived barriers had 3.26 times (AOR = 3.26, 95% CI: 1.88, 5.66) better adherence to self-care practice than study participants with higher perceived barriers.
In this study, 73% of study participants with a poor wealth index (AOR = 0.27, 95% CI: 0.16, 0.46) had less adherence to self-care practice as compared to the study participants with a higher wealth index. About 41% of study participants with poor behavioral control (AOR = 0.59, 95% CI: 0.36, 0.97) had less adherence to self-care practices than those with good behavioral control. About 64% of study participants with poor behavioral intention (AOR = 0.36, 95% CI: 0.21, 0.64) had less adherence to self-care practice than study participants with good behavioral intention. About 80% of study participants with low perceived benefit (AOR = 0.20, 95% CI: 0.08, 0.51), and 49% of study participants with middle perceived benefit (AOR = 0.51, 95% CI: 0.31, 0.83) had less adherence to self-care practice than DM patients with higher perceived benefit (Table 3).
 |
Table 3 Associated Factors of Adherence to Self-Care Practice Among T2DM Patients at CSHs of Amhara Region, Ethiopia (n=794) |
Qualitative Findings
In the current study, the investigator interviewed a total of 16 T2DM patients, of whom 9 were males and 7 were females. The participants were between the ages of 34 and 68 years old. Six participants had diplomas and above educational levels; 2 participants were in grades 9–12; 5 participants were in grades 5–8; and 3 participants were unable to read and write. Regarding their current work, 5 of them were employed; 5 of them were merchants; 3 of them were housewives; 1 participant was a farmer; and 2 participants were retired. The participants’ residences were from both the town14 and the rural.2 The duration of the diagnosis ranged from 2 years up to 42 years.
The thematic analysis resulted in having 42 codes in 16 subthemes, which were grouped into five key themes. The first theme was the current self-care practice of T2DM patients, which included the recommended self-care practice and the use of plants as subthemes. The second theme was beliefs about DM, which included severity of the disease, susceptibility to the disease, benefit of self-care practice, and attitude toward the importance of self-care practice as sub-themes. The third theme was the self-efficacy of DM patients, which included self-confidence and opportunities that would help with self-care practice as subthemes. The fourth theme was social support, which included health professionals, family, and friends/others as subthemes. The last theme was barriers to self-care practice, which included economic, health facility, infrastructure, personal, and influence of others as subthemes.
The Current Self-Care Practice of DM Patients
Most key informants13 described that they attempted to care for themselves through self-care practice. Some of them5 reported using healthy diets like teff (Eragrostis tef), barley, vegetables, and fruits and avoiding eating sugar-containing foods such as wheat and maize, potatoes, bread, and fatty foods. They also added that they controlled their blood sugar level by following the recommended self-care practices.
One key informant portrayed that:
I don’t eat potatoes; I eat teff injera and vegetables. I never used meat-containing foods; I reduced fatty foods; and I didn’t drink sweetened beverages. my sugar level is normal. (41, female, government employee)
One key informant described that he has a list of foods and drinks to follow, which is recommended for DM management. He needs further training related to DM management. He also explored the fact that he always tries to find possible techniques on the internet and social media that would help him manage his DM. The finding was further substantiated by another key informant.
I have put a list of important types of foods in my house. I found them by reading. I am pleased to take any available related training. (55, male, government employee)
This key informant also added that the absence of important goods in the market and the higher cost have affected his ability to achieve his dietary goals.
He said,
Currently, goods are becoming highly expensive. Even though I have enough money in my pocket, I cannot get the required goods in the market. (55, male, government employee)
Nevertheless, a small number of key informants2 expressed that despite their efforts to utilize available resources at home and steer clear of sugar-containing foods, they encountered challenges in meeting the complete demands of self-care through diet. This difficulty arose from a lack of financial resources to fulfill their dietary needs and the presence of a large number of family members residing with them.
One key informant described that
I avoid sugar-containing foods, but making my diet fit for the management of my DM is difficult. I live with 11 members of my family. It is hard to buy vegetables and fruits as they can’t be affordable. (54, female, government employee)
Almost all key informants14 described having regular physical exercise every day as much as possible due to their daily work. However, one key informant mentioned being unable to do regular physical exercise due to back pain and being afraid of physical damage during exercise.
One key informant portrayed that,
My physician told me to do light physical exercise, but I do have back pain while trying to walk and get easily ill. I am also afraid of falling. (46, housewife)
Almost all key informants13 described the fact that they usually wash their hands and legs with soap and water to protect themselves from foot ulcers. All of the key informants mentioned that they took their medication as per physician order. They reported even taking the medication with proper instruction and timing. However, a few key informants3 described that they sometimes missed their medication when the drug was out of the market for a short period of time.
One key informant described that:
I always take my medication appropriately as told by the physician. But sometimes the drug is out of the hospital and tells us to come back after the drug resupply again. The medication was jumped this time for about 3–5 days. (35, female, government employee)
All key informants described that they check their blood sugar level or have a medical checkup at the nearest clinic when they feel symptoms but do not have a regular blood sugar checkup. One key informant mentioned that she had a glucometer to monitor her blood sugar level by herself, which she measured when feeling symptoms. She also added that the presence of a glucometer helped her increase the number of blood glucose tests while she felt symptoms.
One key informant portrayed that:
I measure my blood sugar at home. I have equipment for checking blood glucose at home, which can reduce the need for hospitalization. I am skilled at controlling my blood sugar. (35, female, government employee)
Two key informants explored several types of DM management on their own. They described that Moringa Olivera, honey, and holy water have been used by them to reduce their blood sugar levels.
One key informant described,
I have taken Moringa for a long time. I have gotten advantages from it. I would like to recommend to the minister of health to carry out research regarding Moringa, or Shiferaw. (66, male, retired)
Beliefs to Self-Care Practice
All of the key informants believed that self-care was the best way to avoid DM complications and save their lives, which would keep them alive in the same way as others. Most of the key informants9 also described that medical follow-up alone was not effective without the appropriate self-care practice in daily life. One key informant described that without self-care practice, complications could not be prevented, which resulted in death.
One of the key informants described that
my self-care practice helped me care for myself to correct my blood glucose, thereby saving my life from complications and death. (42, male, merchant)
Even though one key informant ignored the benefit of self-care practice, almost all the key informants15 believed they were getting benefits from self-care practice. They thought that it had a critical role in controlling the development of complications associated with DM, preventing hospitalization, living a healthy life, and preventing death.
One key informant said,
I have gotten a lot of benefits from caring for myself. My complications are supposed to be reduced by controlling my blood glucose through self-monitoring. I observed difficulties when I didn’t care for myself. My blood glucose level was elevated. (54, male, government employee)
All key informants explored the risk of DM if self-care was not practiced and if left untreated upon blood glucose rising. They also believed the risk of unwanted feeding systems would result in a serious outcome. They thought that life had become dangerous and that it had become difficult to live healthy for a prolonged time due to raised blood sugar, which resulted in foot ulcers and finally death.
One key informant described that
if there is no self-care practice for DM, it is dangerous for life. It causes high blood sugar levels, foot ulcers, and other complications that can last for a long time and eventually lead to death. (66, male, retired)
Most11 key informants believed that DM is a severe disease that causes fatigue, stress, and burning sensations throughout the body, including the joints, as well as blindness and body defects if proper self-care practices were not followed. They described that blood glucose will be elevated, resulting in loss of consciousness, numbness of the foot, foot ulcers, hypertension, and death if they do not take the medication(s) as prescribed.
One key informant portrayed,
I might have died. Previously, I have faced a problem, which is falling on the road and losing consciousness, and thus the local personnel are taking me to my house. (36, male, farmer)
One key informant also described the transition of DM as hereditary, and he wanted to advise societies that the cause is not the patients themselves.
He said,
I would like to inform Ethiopians that DM is a hereditary disease. For example, I have a family history of DM. (66, male, retired)
But almost all the other key informants14 believed the cause of DM was the almighty God and that God still saved their lives. A few of the key informants2 also described the use of holy water as something that would help them to have good feelings and even reduce their blood glucose level.
One key informant portrayed,
God saves my life; he gives me and keeps me if I live based on the recommendation of health professionals. (42, male, merchant)
Another key informant added,
“I sometimes used the holy water at the Orthodox Church; I even attended this week. It makes me happy while using it, and my blood sugar was reduced from 140 to 120 this week. (46, housewife)
Self-Efficacy
Most key informants14 were confident in carrying out self-care practices.
One key informant portrayed,
I am self-assured in carrying out self-care practices; I eat a healthy diet; I never drink alcohol; and I wear socks and shoes that are comfortable for my feet. (52, male, government employee)
Some key informants5 described reading books and using social media to obtain information about DM. One participant described how getting formal education from a college helped him better adhere to self-care practices.
One key informant described,
I used to be a health care practitioner, so I have a good understanding of my disease condition. This helps me to control this disease in an effective manner. (60, male, merchant)
In contrast to the above finding, one key informant never wanted to carry out self-care practices as recommended by health care professionals. She described that nobody was with her, that financial barriers would make her unable to participate, and that she was ignorant of the recommended self-care practice.
She described,
I don’t want to do anything to take care of myself due to the low income I gain per month. I always live a similar life, like a normal person. I am always frustrated because nobody is with me when death comes one day. (34, female, merchant)
Social Support
All key informants mentioned the role of health professionals and other similar patients. Most key informants11 explored how they received information on how to manage it. They described getting advice on what things are prohibited and allowed for them and being told to take their medication on time and not to stop the medications they are taking. Except for one participant who described the absence of family with her, almost all key informants15 also explored the role of family in improving self-care practices by washing their legs, giving them food, taking them to the hospital when they feel sick, and giving medication on time.
One key informant portrayed,
My family had a huge role in protecting me from the problems associated with my DM. I am washing my legs, preparing the appropriate food, and alarming my medication time. I can’t survive this disease if my family does not live with me. (68, male, retired)
Almost all key informants14 explored the role of other communities, saying that they did not force them to eat meals that were not recommended for DM patients because the people knew what meals were recommended for DM patients. Some key informants2 described the feeling of being sad because they thought they were bothering others and also influencing families. They believed that the norm of social culture’s eating habits influenced DM patients’ food preparation and food selection.
One key informant described,
In our community, the people know what meals I should take, and they don’t force me to eat meals that are not recommended for DM patients. (55, male, government employee)
Two key informants described that they were members of a DM association that would help them access updated information on DM management from the association. But they felt the poor performance of the association at the current time.
One of the key informants described that:
I contributed three birr, they gave me kooks, and there was also a meeting for discussion. I have got a lot of information there, but these days it is not well functioning. (50, housewife)
Two key informants described how health insurance saved their lives. They were not worried about the cost of drugs and appreciated the health system’s provision of health insurance. They also advised others to have health insurance.
One key informant described,
Thanks to the government. I take medication without a fee since I have health insurance that covers my treatment expenses. I only pay for renewed health insurance. (58, housewife)
Barriers of Self-Care Practice
Only two key informants described that they did not perceive barriers to adhering to self-care practices. Almost all key informants14 described several kinds of barriers to adhering to self-care practices. They reported difficulties adhering to the recommended self-care practices because they faced challenges in obtaining a healthy diet. Additionally, the increased expenses associated with managing complications related to DM, such as eye problems, posed further obstacles, exacerbated by the current cost inflation. They also added that their income level has affected self-care practices, which leads to being unable to afford medical and non-medical costs.
One key informant portrayed,
Current living costs are also beyond my capacity. In addition to DM, I also have vision problems and also take medication for vision. (52, male, government employee)
A key informant revealed that economic challenges, solitary living, and a lack of support hindered her ability to adopt an appropriate feeding style. She shared how her meager daily income significantly impacted her capacity to adhere to the recommended feeding style and other potential methods of DM self-care. Furthermore, she highlighted that inadequate DM management often leads to elevated blood sugar levels and persistent symptoms, underscoring the impact of these challenges on her overall well-being.
She explored,
I have a poor daily income. The money gained from a very small shop by selling beer was not enough to follow the recommended diet, but rather to continue living without taking care of myself by appropriate feeding. (34, female, merchant)
Nearly all key informants15 observed a rise in the number of DM patients and identified a shortage of physicians as a hindrance to receiving quality service and counseling from doctors. A few key informants3 noted the absence of a dedicated clinic for DM patients at the hospital, which could aid in diagnosis, management, monitoring, and counseling for DM patients. They emphasized the need for government attention to address the needs of individuals with DM.
One key informant portrayed,
The number of patients is imbalanced with the number of health professionals in the hospital. Ineffective service in terms of appropriate counseling is observed. The doctors are bored. (46, housewife)
The majority13 of the key informants discovered that the cost of medication and supplies is the most significant barrier. They described that drugs were not available in the hospital and were forced to be purchased in a private pharmacy, which led to higher costs.
One key informant portrayed,
The medications are not always available in government hospitals, and we are obliged to go to a private pharmacy to get the medications at a higher cost. (52, male, government employee)
Two key informants explained that the lack of transportation to reach the health facility or the absence of a health facility in close proximity to their residence creates challenges in maintaining proper self-care practices. This difficulty arises from a lack of updated information and regular checkups to monitor their sugar levels.
One key informant portrayed,
I am living far away from the town and I can’t check my sugar level regularly, and I can’t even reach the health facility upon symptoms as the health facility takes about 3 hours by foot transportation. (36 years, male, farmer)
Two key informants described how the problems with the water supply have resulted in poor care of their cleanliness. They explored that a shortage of water supply leads to difficulty taking daily foot care. They mentioned that they tried to save water with the large container for the next period of water supply, but the stored water was finished before the next round of water supply.
One key informant portrayed that:
I consistently prioritize my cleanliness by regularly washing my clothes and cleansing my legs daily. However, there are occasions when the water supply is disrupted. I make an effort to save water in containers, but it might run out before the next supply. In such cases, I might skip washing my legs temporarily. (55, male, governmental employee)
Some of the key informants3 explored that they had obstacles with regard to self-care practice. Forgetting to take medications, failing to keep appointments, drinking alcohol and coffee, having a strong desire to drink alcohol, aging, retirement, and comorbidity are all described as risk factors.
One key informant portrayed,
I feel like I am struggling for nothing. I face such things some of the time. Otherwise, I need to treat it. I am afraid of the complications, missing medical appointments, and feeding carelessly. (68, male, retired)
Two key informants also outlined the difficulty of contending with social stigma and discrimination, as they faced challenges in living together and participating in teamwork due to their exclusion from social activities. Furthermore, the cultural context impacted their ability to prepare food independently.
One key informant portrayed,
I have faced social stigma and discrimination. I was isolated from teamwork as society believed that I couldn’t work at all. This leads me to an economic disadvantage. (36, male, farmer)
Discussion
In the current study, 337 study participants (42.4%) had good adherence to self-care practice. The finding is in line with the studies conducted in western Ethiopia in 2020 (42.7%)14 and in the Gurage Zone in 2022 (39.6%),45 and it is higher than the study conducted in Tigray in 2017 (37.3%).39 The possible variation of this result might be related to the period gap resulting in some improvements in the health care systems,46 socio-demographic characteristics, and methods in which the current study used multi-facility and a large sample size, while the previous study used a single institution and a lower sample size (278 patients).
The current finding reveals a prevalence lower than that reported in various locations, including a Ethiopia (systematic review) in 2020 (49%),10 Gondar in 2021 (55.6%),24 Hadiya Zone in 2019 (52.3%),38 Addis Ababa in 2021 (48.0%),11 Jimma Medical Center in 2021 (54.2%),12 Dessie in 2021 (55.8%),13 Dire Dawa in 2020 (55.9%),15 Dubti and Assaita hospitals in 2020 (63.8%),16 Debre-Tabor in 2018 (63.1%),17 Arsi zone in 2021 (53.3%),47 and Benishangul Gumuz in 2018 (54.3%).19 The discrepancy could be attributed to the timing of the present study, conducted post-COVID-19 pandemic48–50 and following the conflict in Northern Ethiopia, which impacted the socio-economic landscape,51,52 potentially leading to a decline in adherence to self-care practices.
Other factors contributing to the observed variation may include socio-cultural distinctions and methodological discrepancies, as elaborated below. The previous study in Gondar, Addis Ababa, Dessie, Dire Dawa, Jimma Medical Center, and Debre-Tabor used a single institution.11–13,15,17,24 A systematic review in Ethiopia and a study in Gondar, Hadiya Zone, Dire Dawa, and Benishangul Gumuz were studied among both types of DM patients.10,15,19,24,38,47 Study in Addis Ababa used only four domains (excluding adherence to medication) to calculate the overall self-care practice.11 A study in Jimma Medical Center used single yes-or-no questions for each domain to assess adherence to self-care practice.12 Another study conducted in Dessie used a percentage score (60% of total self-care practices) to calculate adherence to self-care practices.13 However, in contrast to prior studies, the current research employed a substantial sample size, gathered data specifically from T2DM patients, adopted a multi-facility study setting, and utilized a mean cutoff point for categorizing self-care practices as either good or poor.
The current finding is also lower than a study conducted in Thailand (55.9%).53 The variation in results could stem from differences in the study setting, encompassing cultural disparities, economic status variations (given Ethiopia’s lower-income status, with patients potentially unable to afford personal glucometers and a healthy diet), lifestyle distinctions, and methodological variances. Notably, the prior study involved 212 patients with 16 items and 3 domains (diet control, physical activity, and medication adherence), while the current study, with a larger sample size, employed 12 items across 5 domains, which included regular blood sugar testing and foot care.
In this study, more than two-thirds of the participants (70.8%) adhered to the prescribed medication as compared to other domains of self-care practice, which is similar to the previous study in Dubti and Assaita hospitals.16 Possibly, the explanation lies in receiving sufficient guidance from healthcare professionals on proper medication administration during medical follow-up.54 Similar to the study conducted in Addis Ababa, in Jimma Medical Center, and in Dessie,11–13 less adherence to blood sugar testing (33.6%) was observed as compared to other domains of self-care practice. The cause could be attributed to the absence of a self-testing glucometer and the limited proximity of health facilities to patients’ residential areas. The qualitative aspect of the present study discovered that DM patients, when experiencing symptoms, would check their blood sugar level or seek a medical checkup at the nearest clinic. However, they reported a lack of regular blood sugar checkups at home due to the absence of a self-testing glucometer.
In the present study, membership in the DM association, possession of a glucometer, glycemic control, wealth index, behavioral control, behavioral intention, perceived benefit, and perceived barriers demonstrated significant associations with adherence to self-care practices (p-value<0.05).
Study participants who are members of the DM association had higher odds of good adherence to self-care practice than their counterparts. This is substantiated by the prior research.21 This could be attributed to the information disseminated by the association office. The qualitative aspect of this study also highlighted the significance of belonging to the DM association for accessing current information on self-care practices. In contrast to the present discovery, the qualitative study in Addis Ababa found that patients lacked awareness of any personal benefits they could derive from the association, despite being members.7 The difference could be attributed to socio-cultural variations, disparities in health facility accessibility, and variations in the study period.
Study participants who had a home glucometer had more than two times better adherence to self-care practices as compared to study participants who did not have a glucometer in their house. This association is consistent with the previous study conducted elsewhere.11,13–15,17 It is unsurprising that having a glucometer at home would result in more frequent blood sugar level checks throughout the week, allowing patients to stay informed about their blood sugar status, thereby contributing to good self-care practices.17 The qualitative aspect also affirmed that possessing a glucometer can enhance the frequency of blood sugar tests, thereby establishing improved self-care practices.
In the current study, DM patients with good glycemic control had a significant association with good adherence to self-care practices. The cause could be an elevation in FBS levels due to insufficient self-care practices among the study participants.55 This is substantiated by the qualitative results. The explanation could be that maintaining a controlled FBS level may serve as motivation for patients to adhere to self-care practices. However, another study in Eastern Ethiopia showed that uncontrolled blood glucose had a significant association with better DM self-care activities.18 The disparity could be attributed to additional external factors.
The current study showed a significant association between the wealth index and adherence to self-care practice. DM patients with a poor wealth index had less adherence to self-care practices. A similar association was also identified in the previous studies.15,56 The association is unsurprising, considering that patients with a higher wealth index are likely to exhibit improved self-care practices.56 In contrast to the current finding, another study in Harari, Eastern Ethiopia, showed that higher-income patients were less likely to perform the recommended self-care practice.37 The disparity could be attributed to variations in the study period and socio-cultural differences among the study participants.
DM patients with poor behavioral control had poor self-care practices. It is supported by previous studies conducted elsewhere.27,53,57–61 This is expected, given that patients with higher self-efficacy are likely to achieve better outcomes and effectively navigate obstacles for long-term health benefits.53,59 In this study, it was demonstrated that self-efficacy or behavioral control significantly contributes to preserving patients’ lives and adhering to comprehensive self-care practices, establishing it as a key strategy for intervention objectives. The qualitative results of the present study also affirmed the significance of behavioral control in relation to self-care practices.
Similar to the previous studies conducted in China62 and in Tarakan,58 DM patients with poor behavioral intention had poor adherence to self-care practice. The cause could be attributed to patients’ intentions, which have the potential to enhance their ability to adhere to the recommended self-care practices. This suggests that the level of intention to follow self-care practices holds significant influence.
In the present study, there was no significant association between attitude and subjective norms with adherence to self-care practices. This could be attributed to the strong impact of the two constructs, behavioral control, and behavioral intention, on the adherence to self-care practices. In contrast to the current study, there was a significant association between subjective norms and adherence to self-care in Gahanna35 and in Thailand.53 However, the qualitative findings suggested that the two constructs were extensively examined, influencing adherence to self-care practices. Previous studies have also acknowledged the role of families, health professionals, and other community members in the context of DM patients.59,60 Individuals with familial support may also benefit from enhanced disease-related information, educational opportunities, and potentially higher income.15
Overall, this study established that the TPB can serve as a crucial predictor for DM self-care practices among DM patients. Previous studies have similarly recommended the implementation of TPB-based education to improve self-care practices among individuals with DM.59,61
In the current study, perceived benefit is significantly associated with adherence to self-care practices of DM patients. Study participants with low perceived benefit and with middle perceived benefit had less adherence to self-care practice than study participants with high perceived benefit. It was consistent with the previous studies in Ethiopia,24,39 China,63 and Iran.64 This could be attributed to a heightened understanding that recognizing the benefits increases the likelihood of adopting the recommended self-care practices. This underscores the significant role of perceived benefits in DM self-care practices, suggesting a need for health providers to conduct educational campaigns about the advantages of self-care practices. Unlike the current study, a prior investigation at the University of Gondar CSH revealed an association between high perceived benefit and poor self-care practices.24 Various external factors could have played a role in producing contradictory outcomes. Additionally, the in-depth interviews suggested that a lack of belief in the benefits of self-care practices was associated with poor adherence to such practices.
The present study identified the negative associations between self-care practice and perceived barriers. DM patients with low perceived barriers had 8.6 times and those with middle perceived barriers had 3.3 times better adherence to self-care practices than those study participants with high perceived barriers. The finding is consistent with several previous studies conducted in Ethiopia24,39 and abroad.63,64 This could be attributed to the negative aspects of a specific health action, serving as potential obstacles to adopting the recommended self-care practices.65 The adverse influence of perceived barriers was corroborated by the qualitative findings in the present study. Additionally, other studies have highlighted that the inaccessibility of medications has had an impact on self-care practices.66,67 Similar studies have also pointed out the influence of financial constraints on lower adherence to self-care practices.28,68
In the current study, perceived severity and perceived susceptibility were not predictors of adherence to self-care practice, which is similar to the previous studies in Tigray39 and Malaysia.27 The reason might be the presence of other variables that highly affect adherence to self-care practices. The other studies in Harari, Gondar, and China also showed perceived susceptibility was not significantly associated with self-care practice, but there was a significant association between perceived severity and self-care practice, in contrast to the current finding.24,63 Another study in Hamadan, Iran, also showed a significant association between perceived susceptibility and perceived severity and adherence to self-care practices, in contrast to the current findings.57 The discrepancy could stem from variations in sample size, socio-cultural factors, and health policies. The qualitative aspect of the present study revealed that DM patients held perceptions of severity and susceptibility.
Strength and Limitation of the Study
The strengths of the current study include the utilization of a large sample size, a multi-facility approach, the integration of two theoretical models (TPB and HBM) to identify predictors, and the application of explanatory sequential mixed methods. The study has limitations, including the use of a cross-sectional dataset, which restricts causal interpretations, and reliance on self-reporting, susceptible to recall bias and social desirability bias, particularly during face-to-face interviews, potentially underestimating current self-care practices.
Conclusion
A majority of the participants with T2DM exhibited inadequate adherence to self-care practices. Being a member of the DM association, having a glucometer, good glycemic control, wealth index, behavioral control, behavioral intention, perceived benefit, and perceived barriers were significantly associated with adherence to self-care practice. The majority of key informants explored economic barriers as the primary obstacle to adhering to self-care practices. Access to DM associations, accessing glucometers, improving beliefs about the benefits of self-care practice, lowering barriers such as drug unavailability and service delivery at health facilities, and assisting economically disadvantaged DM patients are all intended to improve adherence to self-care practice.
Abbreviations
AOR, Adjusted odds ratio; CSH, Comprehensive specialized hospital; CI, Confidence interval; DM, Diabetes mellitus; FBS, Fast blood sugar; HBM, Health Belief Model; TPB, Theory of planned behavior; T2DM, Type 2 diabetes mellitus.
Data Sharing Statement
The data can be made available to the corresponding author upon a reasonable request.
Ethical Considerations
Ethical clearance was obtained from Wollo University, College of Medicine and Health Science, with ethical review approval reference number CMHS/661/14. Permission was obtained at the medical director’s office of each CSH. The participation of respondents was voluntary with written informed consent after a detailed explanation of the purpose of the study. The data collectors were informed that the participants had the full right to discontinue or refuse to participate in the study. No personal identifiers were incorporated. The participants were informed that the collected data was used for research purposes only. The authors confirmed that the participants’ informed consent included the publication of anonymized responses. This study was conducted according to the Declaration of Helsinki.
Acknowledgments
The authors are grateful to the data collectors, facilitators, study participants, and Wollo University.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no conflict of interest in this work.
References
1. Magliano DJ, Boyko EJ. IDF diabetes atlas; 2022.
2. Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract. 2019;157:107843. doi:10.1016/j.diabres.2019.107843
3. Bukhsh A, Khan TM, Nawaz MS, Ahmed HS, Chan KG, Goh B-H. Association of diabetes knowledge with glycemic control and self-care practices among Pakistani people with type 2 diabetes mellitus. Diabetes Metab Syndr Obes. 2019;12:1409. doi:10.2147/DMSO.S209711
4. Hailu FB, Moen A, Hjortdahl P. Diabetes self-management education (DSME)–Effect on knowledge, self-care behavior, and self-efficacy among type 2 diabetes patients in Ethiopia: a controlled clinical trial. Diabetes Metab Syndr Obes. 2019;12:2489. doi:10.2147/DMSO.S223123
5. Mohebi S, Parham M, Sharifirad G, Gharlipour Z, Mohammadbeigi A, Rajati F. Relationship between perceived social support and self-care behavior in type 2 diabetics: a cross-sectional study. J Educ Health Promot. 2018;2:7.
6. Seng JJB, Kwan YH, Lee VSY, et al. Differential health care use, diabetes-related complications, and mortality among five unique classes of patients with type 2 diabetes in Singapore: a latent class analysis of 71,125 patients. Diabetes Care. 2020;43(5):1048–1056. doi:10.2337/dc19-2519
7. Tewahido D, Berhane Y, Atkin SL. Self-care practices among diabetes patients in Addis Ababa: a qualitative study. PLoS One. 2017;12(1):e0169062. doi:10.1371/journal.pone.0169062
8. Gurmu Y, Gela D, Aga F. Factors associated with self-care practice among adult diabetes patients in West Shoa Zone, Oromia Regional State, Ethiopia. BMC Health Serv Res. 2018;18(1):1–8. doi:10.1186/s12913-018-3448-4
9. Rusdiana MS, Amelia R, Amelia R. The effect of diabetes self-management education on Hba1c level and fasting blood sugar in type 2 diabetes mellitus patients in primary health care in Binjai City of North Sumatera, Indonesia. Open Access Maced J Med Sci. 2018;6(4):715. doi:10.3889/oamjms.2018.169
10. Ketema DB, Leshargie CT, Kibret GD, et al. Level of self-care practice among diabetic patients in Ethiopia: a systematic review and meta-analysis. BMC Public Health. 2020;20(1):1–12. doi:10.1186/s12889-020-8425-2
11. Wolderufael M, Dereje N. Self-care practice and associated factors among people living with type 2 diabetes in Addis Ababa, Ethiopia: a facility-based cross-sectional study. Diabetes Metab Syndr Obes. 2021;14:1. doi:10.2147/DMSO.S287352
12. Mekonnen Y, Hussien N. Self-care related knowledge, attitude, and practice and associated factors among patients with type 2 diabetes in JMC, Ethiopia. Diabetes Metab Syndr Obes. 2021;14:535. doi:10.2147/DMSO.S296112
13. Addis SG, Kassahun SA, Ayele SA, Nega AD, Tegegne KD. Self-care practice and associated factors among type 2 adult diabetic patients on follow up clinic of Dessie referral hospital, Northeast Ethiopia. J Clin Nurs. 2021;5(1):31. doi:10.29328/journal.cjncp.1001034
14. Oluma A, Mosisa G, Abadiga M, Tsegaye R, Habte A, Abdissa E. Predictors of adherence to self-care behavior among patients with diabetes at public hospitals in West Ethiopia. Diabetes Metab Syndr Obes. 2020;13:3277. doi:10.2147/DMSO.S266589
15. Getie A, Geda B, Alemayhu T, Bante A, Aschalew Z, Wassihun B. Self-care practices and associated factors among adult diabetic patients in public hospitals of Dire Dawa administration, Eastern Ethiopia. BMC Public Health. 2020;20(1):1–8. doi:10.1186/s12889-020-09338-5
16. Gulentie TM, Yesuf EM, Yazie TS, Kefale B. Predictors of diabetes self-care practice among patients with type 2 diabetes in public hospitals in northeastern Ethiopia: a facility-based cross-sectional study. Diabetes Metab Syndr Obes. 2020;13:3137. doi:10.2147/DMSO.S273682
17. Tiruneh SA, Ayele AA, Emiru YK, et al. Factors influencing diabetes self-care practice among type 2 diabetes patients attending diabetic care follow up at an Ethiopian General Hospital, 2018. J Diabetes Metab Disord. 2019;18(1):199–206. doi:10.1007/s40200-019-00408-z
18. Ayele BH, Mengesha MM, Tesfa T. Predictors of self-care activities of outpatient diabetic residents in Harar and Dire Dawa: a hospital-based cross-sectional study. SAGE Open Med. 2019;7:2050312119865646. doi:10.1177/2050312119865646
19. Chali SW, Salih MH, Abate AT. Self-care practice and associated factors among Diabetes Mellitus patients on follow up in benishangul gumuz regional state public hospitals, Western Ethiopia: a cross-sectional study. BMC Res Notes. 2018;11(1):1–8. doi:10.1186/s13104-018-3939-8
20. Abate TW, Tareke M, Tirfie M. Self-care practices and associated factors among diabetes patients attending the outpatient department in Bahir Dar, Northwest Ethiopia. BMC Res Notes. 2018;11(1):1–5. doi:10.1186/s13104-018-3874-8
21. Mamo M, Demissie M. Self care practice and its associated factors among diabetic patients in Addis Ababa public hospitals, cross sectional study. J Diabetes Cholest Metabol. 2016;1(1):2–5.
22. Alodhayani A, Almutairi KM, Vinluan JM, et al. Association between self-care management practices and glycemic control of patients with type 2 diabetes mellitus in Saud Arabia: a cross–sectional study. Saudi J Biol Sci. 2021;28(4):2460–2465. doi:10.1016/j.sjbs.2021.01.047
23. Dedefo MG, Ejeta BM, Wakjira GB, Mekonen GF, Labata BG. Self-care practices regarding diabetes among diabetic patients in West Ethiopia. BMC Res Notes. 2019;12(1):1–7. doi:10.1186/s13104-019-4258-4
24. Melkamu L, Berhe R, Handebo S. Does patients’ perception affect self-care practices? The perspective of health belief model. Diabetes Metab Syndr Obes. 2021;14:2145. doi:10.2147/DMSO.S306752
25. Zeru MA, Tesfa E, Mitiku AA, Seyoum A, Bokoro TA. Prevalence and risk factors of type-2 diabetes mellitus in Ethiopia: systematic review and meta-analysis. Sci Rep. 2021;11(1):1–15. doi:10.1038/s41598-021-01256-9
26. Niguse H, Belay G, Fisseha G, Desale T, Gebremedhn G. Self-care related knowledge, attitude, practice and associated factors among patients with diabetes in ayder comprehensive specialized hospital, North Ethiopia. BMC Res Notes. 2019;12(1):1–7. doi:10.1186/s13104-019-4072-z
27. Yee KC, Md Said S, Abdul Manaf R. Identifying self-care behaviour and its predictors among type 2 diabetes mellitus patients at a district of Northern Peninsular Malaysia. Mal J Med Health Sci. 2018;14(2):17–29.
28. Mogre V, Johnson NA, Tzelepis F, Paul C. Barriers to diabetic self‐care: a qualitative study of patients’ and healthcare providers’ perspectives. J Clin Nurs. 2019;28(11–12):2296–2308. doi:10.1111/jocn.14835
29. Johnson RB, Onwuegbuzie AJ. Mixed methods research: a research paradigm whose time has come. Educ Res. 2004;33(7):14–26. doi:10.3102/0013189X033007014
30. Brhane M, Kassahun G. Hospital Service in Ethiopia and Its Spatial Distribution Around the Ethiopia. Divers Equal Health Care. 2021;18(11):482–487.
31. Francis J, Eccles MP, Johnston M, et al. Constructing questionnaires based on the theory of planned behaviour: a manual for health services researchers; 2004.
32. Ajzen I. Constructing a Theory of Planned Behavior Questionnaire. Amherst, MA; 2006.
33. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi:10.1016/0749-5978(91)90020-T
34. Caro-Bautista J, Espinar-Toledo M, Villa-Estrada F, et al. Development and psychometric validation of an instrument to identify barriers to self-care among Spanish patients with type 2 diabetes on the basis of theory of planned behavior. Value Health. 2019;22(9):1033–1041. doi:10.1016/j.jval.2019.04.1921
35. Mogre V, Johnson NA, Tzelepis F, Hall A, Paul C. Barriers to self-care and their association with poor adherence to self-care behaviours in people with type 2 diabetes in Ghana: a cross sectional study. Obes Med. 2020;18:100222. doi:10.1016/j.obmed.2020.100222
36. Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11(1):1–47. doi:10.1177/109019818401100101
37. Ayele K, Tesfa B, Abebe L, Tilahun T, Girma E, Bacurau RFP. Self care behavior among patients with diabetes in Harari, Eastern Ethiopia: the health belief model perspective. PLoS One. 2012;7(4):e35515. doi:10.1371/journal.pone.0035515
38. Dea YC. Predictors of diabetes self-care practice and associated factors among patient on follow up at Hadiya zone, health institutions southern Ethiopia, using health belief model, cross-sectional study design. Endocrinol Metabol Res. 2019;4:1–17.
39. Mariye T, Tasew H, Teklay G, Gerensea H, Daba W. Magnitude of diabetes self-care practice and associated factors among type two adult diabetic patients following at public Hospitals in central zone, Tigray Region, Ethiopia, 2017. BMC Res Notes. 2018;11(1):1–6. doi:10.1186/s13104-018-3489-0
40. Gatt S, Sammut R. An exploratory study of predictors of self-care behaviour in persons with type 2 diabetes. Int J Nurs Stud. 2008;45(10):1525–1533. doi:10.1016/j.ijnurstu.2008.02.006
41. Kim H-K, Jun M, Rhee S, Wreen M. Husserlian phenomenology in Korean nursing research: analysis, problems, and suggestions. J Educ Eval Health Prof. 2020;17. doi:10.3352/jeehp.2020.17.17
42. Champion VL, Skinner CS. The health belief model. Health Behav Health Edu. 2008;4:45–65.
43. Addisu Y, Eshete A, Hailu E. Assessment of diabetic patient perception on diabetic disease and self-care practice in Dilla University Referral Hospital, South Ethiopia. J Metabolic Synd. 2014;3(166):1000166.
44. Elshami M, Al-Slaibi I, Ghithan RJ, et al. Women’s awareness of breast cancer symptoms: a national cross-sectional study from Palestine. BMC Public Health. 2022;22(1):1–13. doi:10.1186/s12889-021-12274-7
45. Emire MS, Zewudie BT, Tarekegn TT, et al. Self-care practice and its associated factors among diabetic patients attending public hospitals in Gurage zone southwest, Ethiopia. PLoS One. 2022;17(9):e0271680. doi:10.1371/journal.pone.0271680
46. Assefa Y, Hill PS, Gilks CF, Admassu M, Tesfaye D, Van Damme W. Primary health care contributions to universal health coverage, Ethiopia. Bulletin of the World Health Organization. 2020;98(12):894. doi:10.2471/BLT.19.248328
47. Kassa RN, Ibrahim IY, Hailemariam HA, Habte MH. Self-care practice and its predictors among adults with diabetes mellitus on follow up at public hospitals of Arsi zone, southeast Ethiopia. BMC Res Notes. 2021;14(1):1–6. doi:10.1186/s13104-021-05511-0
48. Aklilu TM, Abebe W, Worku A, et al. The impact of COVID-19 on care seeking behavior of patients at tertiary care follow-up clinics: a cross-sectional telephone survey Addis Ababa, Ethiopia. medRxiv. 2020;1:11.
49. Shimels T, Asrat Kassu R, Bogale G, et al. Magnitude and associated factors of poor medication adherence among diabetic and hypertensive patients visiting public health facilities in Ethiopia during the COVID-19 pandemic. PLoS One. 2021;16(4):e0249222. doi:10.1371/journal.pone.0249222
50. Ayele TA, Shibru H, Mequanent Sisay M, et al. The effect of COVID-19 on poor treatment control among ambulatory Hypertensive and/or Diabetic patients in Northwest Ethiopia. PLoS One. 2022;17(5):e0266421. doi:10.1371/journal.pone.0266421
51. Dadi AF. The mental health consequences of war in northern Ethiopia: why we should be concerned. Lancet Psychiatr. 2022;9(3):194–195. doi:10.1016/S2215-0366(22)00013-X
52. Abdulkadr AA, Neszmélyi GI. Root Causes and the Socio-Economic Impact of the Ongoing War Between the TPLF and the Federal Government of Ethiopia (2 November 2020–15 October 2021). Afrika Tanulmányok/Hungarian J Afr Stud. 2021;15(4):37–52. doi:10.15170/AT.2021.15.4.3
53. Paleeratana W. Predicting diabetic self-care management based on the theory of planned behavior among elderly with type 2 diabetes in Thailand. Сахарный диабет. 2019;22(4):367–376.
54. Rezaei M, Valiee S, Tahan M, Ebtekar F, Ghanei Gheshlagh R. Barriers of medication adherence in patients with type-2 diabetes: a pilot qualitative study. Diabetes Metab Syndr Obes. 2019;589–599. doi:10.2147/DMSO.S197159
55. Prabawati D, Natalia L. The effectiveness of self-care model on diabetes self-management behaviour. Indones Nurs J Educ Clin. 2020;5(1):1–7.
56. Mutyambizi C, Pavlova M, Hongoro C, Groot W. Inequalities and factors associated with adherence to diabetes self-care practices amongst patients at two public hospitals in Gauteng, South Africa. BMC Endocr Disord. 2020;20(1):1–10. doi:10.1186/s12902-020-0492-y
57. Vazini H, Barati M. The health belief model and self-care behaviors among type 2 diabetic patients. Iran J Diabetes Obes. 2014;6(3):107–113.
58. Damayanti A, Tamtomo D, Indarto D. Theory of planned behavior implementation on the factors affecting self-care management in type 2 diabetes mellitus patients. J Health Promo Behav. 2018;3(2):139–145. doi:10.26911/thejhpb.2018.03.02.08
59. Zeidi IM, Morshedi H, Otaghvar HA. A theory of planned behavior-enhanced intervention to promote health literacy and self-care behaviors of type 2 diabetic patients. J Prev Med Hyg. 2020;61(4):E601. doi:10.15167/2421-4248/jpmh2020.61.4.1504
60. Amer FA, Mohamed MS, Elbur AI, Abdelaziz SI, Elrayah ZA. Influence of self-efficacy management on adherence to self-care activities and treatment outcome among diabetes mellitus type 2. Pharm Pract. 2018;16(4):1274. doi:10.18549/PharmPract.2018.04.1274
61. Babazadeh T, Jafaralilou H, Ghaffari-Fam S, Oliaei S, Sadra V, Sarbazi E. Self-care behaviors in diabetic type 2 patients in the countryside of Tabriz, Iran: application of the extended theory of reasoned action (ETRA). Ann Ig. 2020;32(3):254–262. doi:10.7416/ai.2020.2348
62. Lin C-Y, Cheung MK, Hung AT, Poon PK, Chan SC, Chan CC. Can a modified theory of planned behavior explain the effects of empowerment education for people with type 2 diabetes? Ther Adv Endocrinol Metab. 2020;11:2042018819897522. doi:10.1177/2042018819897522
63. Hu Y, Liu H, Wu J, Fang G. Factors influencing self-care behaviours of patients with type 2 diabetes in China based on the health belief model: a cross-sectional study. BMJ open. 2022;12(8):e044369. doi:10.1136/bmjopen-2020-044369
64. Karimy M, Araban M, Zareban I, Taher M, Abedi A. Determinants of adherence to self-care behavior among women with type 2 diabetes: an explanation based on health belief model. Med J Islam Repub Iran. 2016;30:368.
65. Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2(4):328–335. doi:10.1177/109019817400200403
66. Tusubira AK, Nalwadda CK, Akiteng AR, et al. Social support for self-care: patient strategies for managing diabetes and hypertension in rural Uganda. Ann Glob Health. 2021;87(1):86. doi:10.5334/aogh.3308
67. Ali M, Alemu T, Sada O. Medication adherence and its associated factors among diabetic patients at Zewditu Memorial Hospital, Addis Ababa, Ethiopia. BMC Res Notes. 2017;10(1):1–5. doi:10.1186/s13104-017-3025-7
68. Adu MD, Malabu UH, Malau-Aduli AE, Malau-Aduli BS, Rodda S. Enablers and barriers to effective diabetes self-management: a multi-national investigation. PLoS One. 2019;14(6):e0217771. doi:10.1371/journal.pone.0217771
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.