Back to Journals » Research Reports in Clinical Cardiology » Volume 13
Adherence to Secondary Prophylaxis and Risk Factors Among Patients with Rheumatic Heart Disease at Public Hospitals in Addis Ababa, Ethiopia, 2021–2022
Authors Adal AB , Fetensa G , Chamiso TM , Tiruneh CT , Jebesa MG, Bitew ZW
Received 20 May 2022
Accepted for publication 30 September 2022
Published 12 October 2022 Volume 2022:13 Pages 73—84
DOI https://doi.org/10.2147/RRCC.S373939
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Kones
Abebaw Bires Adal,1 Getahun Fetensa,2 Tekalign Markos Chamiso,3 Chalachew Teshome Tiruneh,4 Melkamu Getaneh Jebesa,5 Zebenay Workneh Bitew6
1College of medicine and health science, department of nursing, Injibara University, Injebara, Ethiopia; 2Department of surgical nursing, St. Paul’s millennium medical college, Addis Ababa, Ethiopia; 3Department of cardiovascular nursing, St. Paul’s millennium medical college, Addis Ababa, Ethiopia; 4Department of care and treatment, AIDS Healthcare Foundation, Addis Ababa, Ethiopia; 5Department of cardiovascular nursing, St Paul’s millennium medical college, Addis Ababa, Ethiopia; 6Department of Pediatrics and child health nursing, St. Paul’s millennium medical college, Addis Ababa, Ethiopia
Correspondence: Abebaw Bires Adal, Injibara University, Injebara, Ethiopia, Email [email protected] Chalachew Teshome Tiruneh, AIDS Healthcare Foundation, Addis Ababa, Ethiopia, Email [email protected]
Background: Rheumatic heart disease is a preventable cardiovascular disease that affects over forty million people worldwide. Poor adherence to secondary prophylaxis increases the risk of recurrent acute rheumatic fever. Studies on adherence to secondary prophylaxis in Ethiopia are scarce. Thus, this study aimed to determine adherence to secondary prophylaxis and risk factors among patients with rheumatic heart disease.
Methods: Facility-based cross-sectional study design was employed to conduct this study from December 25/2021 to January 22/2022. The study was performed among rheumatic heart disease patients in randomly selected four public hospitals in Addis Ababa. Data were collected through face-to-face interviews using a structured questionnaire from follow-up patients after using a pre-tested questionnaire. Data were entered into EPI info version 7.2 and exported to SPSS version 26 for analysis. Multivariable logistic regression analysis was performed using variables with a p-value of less than 0.25 in bi-variable logistic regression analysis. Adjusted Odds Ratio (AOR) with a 95% confidence interval was estimated to determine the strength of association with poor adherence. Statistical significance multivariable logistic regression analysis was declared when the p-value is < 0.05.
Results: Three hundred and eighty-one study participants completed the study with a response rate of 95%. The mean age of the respondents was 26.45 ± 10.5 years. The overall poor level of adherence was 29.1% (95% CI: 24.7– 33.8%). Rural residency (AOR = 2.637, 95% CI: 1.068– 6.513), living with > family members (AOR = 2.879, 1.282– 6.465), living more than 30 km from health clinic (AOR = 3.247, 95% CI: 1.051– 10.033), lack of penicillin V (AOR = 6.772, 95% CI: 3.234– 14.177) and fear of catching Covid-19 (AOR = 0.04, 95% CI: 0.014– 0.114) were independently associated with risk factors for poor adherence.
Conclusion: Considerable proportion of patients with rheumatic heart disease in Addis Ababa had a poor level of adherence to secondary prophylaxis. Stakeholder’s better supply penicillin regularly and administers them at primary health-care facilities.
Keywords: rheumatic heart disease, secondary prophylaxis, adherence
Introduction
Acute rheumatic fever (ARF) results from an autoimmune response to pharyngitis caused by a group of streptococcus (GAS) bacterial infections. It involves the joints, brain, skin, and heart muscles. Long-term damage to cardiac valves caused by a single severe episode or multiple recurrent episodes of ARF is known as rheumatic heart disease (RHD).1 Rheumatic fever mostly affects children and adolescents in low- and middle-income countries, especially in areas where poverty is widespread and access to health services is limited. People living in overcrowded and poor conditions, including in Ethiopia, are at risk of developing this disease.2,3
The most effective treatment for preventing further infection is benzantine penicillin G (BPG), which is administered via intramuscular injection every month. Alternatively, daily oral penicillin V can be given to a selected number of patients if compliance is guaranteed.2,4 Secondary prophylaxis is the continuous administration of penicillin to patients with a previous attack of acute rheumatic fever or well-documented RHD. The rational use of secondary prophylaxis is a critical cost-effective intervention for preventing morbidity and mortality related to ARF and RHD. Patients with RHD are expected to receive at least 80% of the annual prescribed injections. Otherwise, there is a higher risk of recurrent ARF and complications.5 Adherence is the extent to which a person’s behavior in taking medication corresponds with the recommendations agreed upon by health-care providers.6 A patient is classified under good adherence when he/she takes was ≥80% of secondary prophylaxis for RHD (if injected more than nine times per year). Whereas, poor adherence is considered when the patient missed secondary prophylaxis for RHD at least three times per year.7
In 2019, an estimated 40.5 million cases of RHD were reported causing 306,000 deaths annually.8 The burden of the problem decreased significantly in the developed world. However, the morbidity and mortality in developing countries due to limited access to cardiac surgery and the cost related to surgical intervention remains high.9 Africa, Southeast Asia, and the Western Pacific regions are the primary victims accounting for 84% of all cases and 80% of estimated deaths in 2015. Socioeconomic and environmental factors such as poor housing, undernutrition, overcrowding, and poverty are contributors to the incidence, magnitude, and severity of ARF and RHD.10 The prevalence of RHD in East Africa is 17.9 cases per 1000 school children.11
Global adherence to treatment of chronic diseases including RHD in developed countries is only 50%, particularly affecting the poor population.6,7 Due to poor levels of adherence to secondary prophylaxis in patients with RHD continues to report high rates (7%) of an advanced stage of heart valve injury.12 Poor adherence to secondary prophylaxis increases ARF recurrence, worsens RHD, and rapidly leads to hospitalization and surgical intervention.13 In the Gambia, poor adherence to secondary prophylaxis leads to recurrence of ARF by 53.3%, worsening of RHD by 25%, and leading to progression to chronic valvular heart disease and increased surgery by 9.9%.14 Only one per cent of the world’s cardiothoracic surgeons are found in Africa with limited surgical intervention settings. Thus, most patients with chronic valvular heart disease die without undergoing cardiac surgery.15 Besides, poor adherence is associated with socioeconomic status, condition-related factors, patient-related factors, therapy-related factors, and health system-related factors.5,6,16,17
In Ethiopia, studies on adherence to secondary prophylaxis and associated factors are limited. There is only one study conducted among 145 adult patients in a single institution in Addis Ababa among them 30.3% were poor adherence and 37% were from Jimma zonal hospitals. The most common secondary prophylaxis medication in Ethiopia.16 This compromises the generalizability of the findings. In addition, all possible factors associated with poor adherence are not uncovered in Ethiopia. Therefore, this study aimed to determine the level of adherence to secondary prophylaxis and risk factors in patients with RHD at selected public hospitals in Addis Ababa, Ethiopia.
Methods and Materials
Study Area and Period
The study was conducted in Addis Ababa public hospitals. Addis Ababa is the capital city of Ethiopia. It is also the largest city in the country with a total population of 3,384,569 as reported by the 2007 census.18 There are 12 public hospitals in Addis Ababa to provide cardiac follow-up. Four hospitals were selected using a simple random sampling method, which was Tirunesh Beijing hospital, Zewditu memorial hospital, Yekatit 12 hospital, and Saint Peter Specialized hospital. This included 1883 total RHD patients from the District Health Information Software 2 (DHIS 2) registration who were diagnosed before one year and 917 RHD patients appointed from appointment sheets during the study period. The study was conducted from December 25/2021 to January 22/2022.
Study Design and Population
A cross-sectional study was conducted to assess the level of adherence to secondary prophylaxis and the risk factors among patients with RHD at public hospitals in AA, Ethiopia. All registered patients at RHD clinic in Addis Ababa public hospitals were the source population and all registered patients at RHD in selected public hospitals of Addis Ababa were the study population. A selected RHD patient who was interviewed at the RHD clinic during the collection period at a selected public hospital in Addis Ababa was the study unit.
Inclusion and Exclusion Criteria
Patients with RHD who were diagnosed at least one year before the study period were included. However, patients who were critically ill and had no attendants were excluded.
Sample Size Determination and Sampling Procedure
The required sample size was calculated using the single population proportion formula since there was a previous study in Jimma zone hospitals. Poor adherence to secondary prophylaxis was 37%9 and desired precision of 5% and 95% confidence intervals were used for the calculation; the sample size was 358. With a 10% non-response rate, the final sample size was 394.
Sample Size Determination for the Second Objective
By using the double population proportion formula, the following sample size calculation was used for each independent variable by open epi info software 95% CI with 5% margin of error, 80% power, and 1 ratio of exposed to non-exposed outcomes. Three hundred and sixty-four is the largest sample size among others; so, by adding a 10% non-response rate it becomes 400 which is higher than 394; therefore, the final sample size of the study was 400.
Simple random sampling was used to select four hospitals. Next, the calculated sample size (400) was distributed to four hospitals using probability proportional to the size and the numbers of RHD patients required for the study in four hospitals were determined (Figure 1).
 |
Figure 1 The schemes presentation of sampling procedure to select study participants from Addis Ababa governmental hospitals, 2022. |
Therefore, 400 study participants were sampled from respective Hospitals by a simple random sampling method from a RHD clinic sheet using the patient’s medical registration number sampling frame.
Data Collection and Procedures
The questionnaire was adapted through reviewing different literature and previous similar studies.5,6,16 The questionnaire was translated to the local language Amharic and data were collected by face-to-face interviews with patients or their attendants/guardians for pediatric patients who came for follow-up during the study period. Medical data were reviewed from patient records. Eight data collectors and one supervisor were recruited among health-care providers who work in cardiac chronic outpatient departments.
Data Quality Control and Management
One day of training for 8 nurses and one physician was given on data collection methods and a pretest was done using 5% of 60 RHD patients at Alert hospital. The purpose of the pre-test was to ascertain patients ‘understanding of the items asked and the appropriateness of responses and time required to fill out the questionnaire. A reliability estimate was conducted and Cronbach’s alpha was 0.83 for adherence factors to secondary prophylaxis measurement tools. Daily supervision was conducted by the supervisor and principal investigator during data collection and data were checked for completeness on daily basis.
Data Analysis Procedure
After the data collection is completed, the data were checked for properly collected and recorded, coded, entered, and cleaned into EPI Info version (7.2) and exported to package for social science (SPSS) window version 26 for analysis. Descriptive statistics with including frequency, proportion, and mean of variables were used for reporting the descriptive results. Variables with a p-value <0.25 in the bi-variable logistic regression analysis were fitted to multiple logistic regression analysis. In the multivariate logistic regression model, fitness was tested using the Hosmer-Lemeshow goodness-of-fit. Adjusted odds ratio (AOR) with a 95% confidence interval was estimated to assess the strength of the association with poor adherence to secondary prophylaxis. A p-value less than 0.05 was considered significant. Finally, the processed data will be presented by creating frequency, and percentages with tables, text, and graphs.
Ethical Consideration
Before data collection, ethical clearance was obtained from St. Paul’s hospital millennium Medical College Institutional Review Board. A permission letter to conduct the study was secured from the Addis Ababa Regional Health Office, and selected hospitals. Informed consent was obtained from respondents and institutions to execute data collection procedures. Covid 19 protocol and safety were maintained. Information was kept anonymous and confidential.
Results
Socio-Demographic Characteristics
This study included 381 patients with rheumatic heart disease (RHD) who attended a follow-up cardiac clinic with a response rate of 95%. The mean age of the respondents was 26.45 (±10.5 years). Among the participants, 228 (59.8%) were females and 305 (80.1%) were urban residents. Regarding the marital status of the respondents, 192 (50.4%) were single, and 171 (44.9%) were married. The majority of patients attended elementary (1–8) education (34.9%). Unemployment accounted for 228 (59.8%) followed by non-governmental (driver, merchant, private) 101 (26.5%). The majority of respondents travelled 1–5 km to get a BPG injection at health facility 216 (56.7%) and public transportation 241 (63.3%) was mostly used to travel to the health facility (Table 1).
 |
Table 1 Socio-Demographic Characteristics of the Patients with RHD at Selected Governmental Hospitals, in Addis Ababa, Ethiopia, 2022 (n = 381) |
Clinical Characteristics of Participants
In this study, the majority 285 (74.8%) of the participants were diagnosed with RHD in the past ten years with a mean of 7.5±5.9. Most patients claim their disease condition was moderate by echocardiography evaluation from patients’ chart and sixty-two (16.3%) had a history of co-morbidities (ie, hypertension, Diabetics, Asthma). Most of the participants were aware that sore throat can be caused by bacteria 240 (63%), 254 (66.7%) knew sore throat can be associated with RHD and two-hundred sixty participants perceived that BPG can prevent recurrence and worsening of RHD. The mean waiting time for injection from a health facility was 27.9 ±19.3 minutes (Table 2).
 |
Table 2 Clinical Characteristics and Awareness Regarding RHD Among Respondents at Selected Governmental Hospitals, Addis Ababa, Ethiopia 2022 (n = 381) |
Adherence to Secondary Prophylaxis for RHD Patients
All participants reported that health professionals prescribed secondary prophylaxis drugs and 100% has been on BPG injection from patient’s card and almost 98.7% of participants had injection card for BPG. Most of 218 (57.2%) did not miss a monthly injection, 53 (13.9%) patients missed one to two injections, and 111 (29.1%) missed three and more than three injections. Two hundred seventy (70.9%) of the participants had good adherence whereas the left had poor adherence to BPG prophylaxis. One hundred and three (27.0%) did nothing followed by 50 (13.1%) waiting until the next appointment when they missed the injection and seven (1.8%) went a few days later and 4 (1.0%) others (ie, took alternative medication (herbal), non-functioned the health facilities due to instability, having pregnancy) when they missed monthly injections (Figure 2).
 |
Figure 2 Adherence to secondary prophylaxis patients with RHD at selected governmental hospitals in Addis Ababa, Ethiopia, 2022. |
Reason for Poor Adherence to Secondary Prophylaxis
Regarding the reason for missing injection of BPG, most of the patients 204 (53.5%) were due to lack of medication supply (ie, stock out [46.5%] and expired of the drug [3.1%]) followed by fear of injection pain 145 (38.1%) and poor awareness about the disease and prophylaxis 127 (33.3%) with respect, as detailed in (Figure 3).
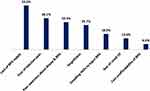 |
Figure 3 Reasons for poor adherence to secondary prophylaxis among patients with RHD at selected governmental hospitals in Addis Ababa, Ethiopia, 2022. |
Factors Associated with Poor Adherence to Benzantin Penicillin G for Patients with RHD
Bi-variable logistic regression analysis indicates that age, address, educational status, family size, distance from home to a health facility, insurance, admission, co-morbidity, lack of drug, fear of catching Covid-19, and duration of BPG prophylaxis were variables which qualify the assumption (p < 0.25) are taken as a candidate for multi-variable analysis. The multivariable logistic regression analysis results indicated that address, family size, distance, lack of penicillin, and fear of catching Covid-19 variables were associated with poor adherence to secondary prophylaxis for rheumatic heart disease. In multivariable logistic regression analysis, participants who had greater than five family members were 2.8 times (AOR = 2.879, 95% CI: 1.282–6.465, p < 0.01) more likely to have poor adherence to secondary prophylaxis compared to those who had ≤ five family members. Study participants who were living a distance from home to an injection facility greater than 30-kilometers were far to be 3.2 times (AOR = 3.247, 95% CI: 1.051–10.033, p < 0.041) more likely to be poor adherence than those who were far less than 30 kilometers distance. Study participants who were living in rural areas were 2.6 times more likely to have poor adherence than those who were in urban residency (AOR = 2.637, 95% CI: 1.068–6.513, p = 0.036). Patients who had a lack of BPG prophylaxis in a followed-up hospital were 6.7 times more likely to be poor adherence than those who did not lack BPG drug (AOR = 6.772, 95% CI: 3.234–14.177, P < 0.01). Similarly, the respondents who were not fear of catching Covid-19 to go to health facilities were 96% less likely to be in poor adherence compared with those who were fearful of catching Covid-19 (AOR = 0.04, 95% CI: 0.014–0.114, P < 0.01) (Table 3).
 |
Table 3 Bi-Variable and Multivariable Regression Analysis of Adherence to Secondary Prophylaxis Among Patients with RHD at Selected Governmental Hospitals, Addis Ababa, Ethiopia, 2022 |
Discussion
This study was a facility-based cross-sectional study designed to determine adherence to secondary prophylaxis among patients with RHD at selected governmental hospitals in Addis Ababa. This study also addressed socioeconomic, health system, condition, patient, and therapy-related factors that affected adherence to secondary prophylaxis for patients with RHD. Then the results addressed objective one and objective two.
In this study, the overall poor adherence level was 29.1% (95% CI: 24.7–33.8%). This finding is comparable with the study conducted in Pakistan’s 26.5%19 and Addis Ababa’s 32.1%16 and slightly low when compared to studies from Egypt, Jimma zones, and Brazil with 34.5%, 37%, and 35%, respectively.5,20,21 However, this result was considerably less poor22 adherence than that found by Jamaica 51.3%,23 India 50%,24 Uganda 46%,17 Sudan 68%,12 and Jimma Medical centre 44.8%.7
The variability in the level of adherence may reflect the different systems in which this study was done, different factors may influence adherence, study designs, study times, done in referral hospitals, and more participants were urban residencies in this study. Furthermore, improvement in BPG prophylaxis prescription habits by health-care workers (100%) and having injection cards (98.7%) by RHD patients have vital contributions to enhancing adherence to BPG.
In this study, the reason for poor adherence to secondary prophylaxis was lack of penicillin supply (53.5%), fear of injection pain (38.1%), forgetting of injection date (29.7%), unwilling health-care providers to administer BPG (18.9%), fear of catching Covid-19 to access health facility (13.6%), cost unaffordability (6.6%), distance from a health facility, and poor awareness about RHD disease and importance of BPG (33.3%). Furthermore, different studies reported reasons for poor adherence almost the same except for the new emerging variable (ie, fear of Covid-19) even if a variation in the percentage.5,7,12,17,23,25
Regarding Factors associated with poor adherence: The participants who were living in rural residency were positively significantly associated with poor adherence to secondary prophylaxis. This finding is in harmony with the study done in Jimma Zone hospitals, in Uganda, and South India.5,25,26 The reason that patients who live in rural areas have poor adherence to BPG prophylaxis is due to difficulty in accessing nearby health-care facilities.
In this study, participants who live greater than thirty kilometres away from health centers were positively significantly associated with poor adherence. This finding is supported by a study done in Jimma medical center and zonal hospitals.5,7 This might be due to not being easily accessible and cost affordable transportation.
The participants who had greater than five family members were 2.8 times poorly adhered to BPG prophylaxis. This is similar to a study done on the new Caledonia.25 This might be attributed to socioeconomic variables such as a family history of RHD as a result of overcrowding living conditions, which is likely secondary to a higher risk of streptococcal transmission in big families,27 cost unaffordability, and the increased cost of the imported drug.
The participants who had a lack of BPG drug in the follow-up hospitals were 6.7 times more a significant relation with poor adherence. This might be due to the scarcity of drugs secondary to not function of the pharmaceutical industry and country instability.
The respondents who were not fear of the catching Covid-19 pandemic to go health facility were 96% less likely associated with poor adherence to secondary prophylaxis of BPG. This is due to the restriction of patients from health-care facilities due to the declaration of lockdown policy by the countries.
In general, adherence to secondary prophylaxis has been shown to reduce the risk of ARF recurrences, worsening of RHD, and leading to chronic rheumatic valvular heart disease. Promoting adherence of patients to secondary prophylaxis should be addressed and assessed timely as the management modality.
Conclusion
Overall, adherence to secondary prophylaxis among patients with RHD in this finding did not address the expected WHO recommendation of the annual prescribed injection. After adjusting for other confounding variables, the main factors for poor adherence were lack of drugs, rural residency especially far from greater than thirty kilometers, fear of new emerging pandemics (Covid-19) to go health facility, patients had >5 family members were factors associated with poor adherence to secondary prophylaxis among patients with RHD.
Strength and Limitation
Strength
The strength of this study is as it was being done in multiple centers. This study now includes a variable that was not previously included (Covid-19).
Limitation
The study was conducted in Addis Ababa, which is assumed to have better health service coverage and drugs; however, it was better if it was conducted in semi-urban and rural areas. In another way, the period in which it was employed was when there is instability in the pharmaceutical production area and transportation problems, which it will be very difficult to conclude to patient perspectives only. The study was conducted only on patients, but it was better to include the health-care providers because the refusal to give the injection of BPG prophylaxis was 18.9%. Furthermore, the investigator gathered data on adherence based on verbal self-report, which could be sustainable to recall bias among participants.
Abbreviations
AA, Addis Ababa; AOR, Adjusted Odds Ratio; ARF, Acute Rheumatic Fever; BPG, Benzantin Penicillin G; CI, Confidence Interval; COVID-19, Corona Virus Infectious Disease at 2019; COR, Crude Odds Ratio; GAS, Group A Streptococcus; SPSS, Statistical Package For Social Science; RHD, Rheumatic Heart Disease; SPH, Saint Peter Hospital; STPHMMC, Saint Paul’s Hospital Millennium Medical College; TBGH, Tirunesh Beijing General Hospital; WHO, World Health Organization; YHMC, Yekatit 12 Hospital Medical College; ZMH, Zewditu Memorial Hospital.
Data Sharing Statement
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from the institutional review board (IRB) of St. Paul’s Hospital Millennium Medical College (SPHMMC). Informed consent was impractical for this study. This is in line with the Helsinki Declaration which is stated as “medical research using identifiable human material or data, physicians must normally seek consent for the collection, analysis, storage and/or reuse. There may be situations where consent would be impossible or impractical to obtain for such research or would pose a threat to the validity of the research. In such situations, the research may be done only after consideration and approval of a research ethics committee’’.28 Information was obtained from the patients and confidentiality was maintained.
Consent for Publication
All authors agreed that this manuscript is eligible for publication.
Acknowledgment
We thank St Paul’s millennium medical college research office and the school of nursing for providing an opportunity to prepare a thesis study. We thank study participants, supervisors and data collectors for their time and voluntary facilitation of the data collection process.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding to perform the study.
Disclosure
The authors declared that have no competing interests in this work.
References
1. Carapetis JR, Beaton A, Cunningham MW, et al. Acute rheumatic fever and rheumatic heart disease. PLoS Negl Trop Dis. 2016;2:15084.
2. Beaton A, Kamalembo FB, Dale J, et al. The American Heart Association’s call to action for reducing the global burden of rheumatic heart disease: a policy statement from the American Heart Association. Circulation. 2020;142(20):e358–e68. doi:10.1161/CIR.0000000000000922
3. Gemechu T, Parry EHO, Yacoub MH, Phillips DIW, Kotit S. Community-based prevalence of rheumatic heart disease in rural Ethiopia: five-year follow-up. PLoS Negl Trop Dis. 2021;15(10). doi:10.1371/journal.pntd.0009830
4. Asmare MH, Woldehanna F, Hunegnaw S, Janssens L, Vanrumste B. Prevalence of rheumatic heart disease in a major referral cardiology clinic in Ethiopia: a retrospective cross-sectional study. PLoS One. 2021;16(2):28.
5. Adem A, Dukessa Gemechu T, Jarso H. Rheumatic Heart disease patients’ adherence to secondary prophylaxis and associated factors at hospitals in Jimma Zone, Southwest Ethiopia: a multicenter study. Sci Rep. 2020;14:2399–2406.
6. Sabaté E, Sabaté E. Adherence to long-term therapies: evidence for action. World Health Organization; 2003.
7. Mohammed K, Demissie WR, Gare MB. Adherence of rheumatic heart disease patients to secondary prophylaxis and main reasons for poor adherence at Jimma Medical Center. E J Cardiovasc Med. 2019;7(1):22. doi:10.32596/ejcm.galenos.2019.00004
8. Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021. doi:10.1016/j.jacc.2020.11.010
9. Cannon J, Roberts K, Milne C, Carapetis JR. Rheumatic heart disease severity, progression and outcomes: a multi‐state model. J Am Heart Assoc. 2017;6(3). doi:10.1161/JAHA.116.003498
10. Katzenellenbogen JM, Bond‐Smith D, Seth RJ. Contemporary incidence and prevalence of rheumatic fever and rheumatic heart disease in Australia using linked data: the case for policy change. J Am Heart Assoc. 2020;9(19). doi:10.1161/JAHA.120.016851
11. Bimerew M, Beletew B, Getie A, Wondmieneh A, Gedefaw G, Demis A. Prevalence of rheumatic heart disease among school children in East Africa: a systematic review and meta-analysis. Pan Afr Med J. 2021;38:242.
12. Edwards JG, Barry M, Essam D, et al. Health system and patient-level factors serving as facilitators and barriers to rheumatic heart disease care in Sudan. Glob Health Res Policy. 2021;6(1):1–12. doi:10.1186/s41256-021-00222-2
13. Torres RA, Torres RA, de Crombrugghe G, et al. Improvement of rheumatic valvular heart disease in patients undergoing prolonged antibiotic prophylaxis. Front Cardiovasc Med. 2021;8. doi:10.3389/fcvm.2021.676098
14. Jaiteh LES, Drammeh L, Anderson ST, et al. Rheumatic heart disease in The Gambia: clinical and valvular aspects at presentation and evolution under penicillin prophylaxis. BMC Cardiovasc Disord. 2021: 21. doi:10.1186/s12872-020-01815-4
15. Watson G, Jallow B, Le Doare K, Pushparajah K, Anderson ST. Acute rheumatic fever and rheumatic heart disease in resource-limited settings. Arch Dis Child. 2015;100(4):370–375. doi:10.1136/archdischild-2014-307938
16. Mekonen KK, Yismaw MB. Adherence to benzathine penicillin g secondary prophylaxis and its determinants in patients with rheumatic heart disease at a cardiac center of an Ethiopian tertiary care teaching hospital. PLoS One. 2020;14:343–352.
17. Musoke C, Mondo CK, Zhang W, et al. Benzathine penicillin adherence for secondary prophylaxis among patients affected with rheumatic heart disease attending Mulago Hospital. Cardiovasc J Afr. 2013;24(4):124–129. doi:10.5830/CVJA-2013-022
18. CSA. Population and housing census Ethiopia; 2007.
19. Sial JA, Farman MT, Batra MK, Karim M. Adherence to secondary prophylaxis of rheumatic fever in patients with rheumatic heart disease in rural areas. Pak Heart J. 2018;51(3):30.
20. Balbaa A, ElGuindy A, Pericak D, Yacoub M, Schwalm J. An evaluation of secondary prophylaxis for rheumatic heart disease in rural Egypt. Glob Cardiol Sci Pract. 2015;2015(3):40. doi:10.5339/gcsp.2015.40
21. Pelajo CF, Lopez-Benitez JM, Torres JM, de Oliveira SK. Adherence to secondary prophylaxis and disease recurrence in 536 Brazilian children with rheumatic fever. Pediatr Rheumatol Online J. 2010;8(1):22. doi:10.1186/1546-0096-8-22
22. Kimambo RG. Process evaluation of HIV Prevention of Mother to Child Transmission Program (PMTCT) in Agaro Health Centre, Jimma Zone, Oromia: Jimma University; 2011.
23. Thompson SB, Brown CH, Edwards AM, Lindo JL. Low adherence to secondary prophylaxis among clients diagnosed with rheumatic fever, Jamaica. Pathog Glob Health. 2014;108(5):229–234. doi:10.1179/2047773214Y.0000000146
24. Prasad A, Prasad A, Singh BK, Kumar S. Compliance to the secondary prophylaxis and awareness of rheumatic heart disease: a cross-sectional study in low-income province of India. Fam Med Prim Care Rev. 2020;9(3):1431–1435. doi:10.4103/jfmpc.jfmpc_1056_19
25. Gasse B, Baroux N, Rouchon B, Meunier JM, Frémicourt ID, D’Ortenzio E. Determinants of poor adherence to secondary antibiotic prophylaxis for rheumatic fever recurrence on Lifou, New Caledonia: a retrospective cohort study. BMC Public Health. 2013;13(1):131. doi:10.1186/1471-2458-13-131
26. Nemani L, Maddury J, Barik R, Arigondam AK. A Cross-sectional study to look at the determinants of poor adherence to secondary penicillin prophylaxis for rheumatic heart disease at a tertiary care center in South India. J Clin Prevent Cardiol. 2018;7(1):5. doi:10.4103/JCPC.JCPC_25_17
27. Coffey PM, Ralph AP, Krause VL. The role of social determinants of health in the risk and prevention of group A streptococcal infection, acute rheumatic fever and rheumatic heart disease: a systematic review. PLoS Negl Trop Dis. 2018;12(6):e0006577. doi:10.1371/journal.pntd.0006577
28. Portaluppi F, Smolensky MH, Touitou Y. Ethics and methods for biological rhythm research on animals and human beings. Chronobiol Int. 2010;27(9–10):1911–1929. doi:10.3109/07420528.2010.516381
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
