Back to Journals » Patient Preference and Adherence » Volume 12
Adherence to endocrine therapy among Chinese patients with breast cancer: current status and recommendations for improvement
Authors Gao P, You L, Wu D, Shi A , Miao Q , Rana U, Martin DP , Du Y, Zhao G, Han B, Zheng C , Fan Z
Received 1 March 2018
Accepted for publication 7 April 2018
Published 22 May 2018 Volume 2018:12 Pages 887—897
DOI https://doi.org/10.2147/PPA.S167004
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Pin Gao,1 Lili You,2 Di Wu,1 Aiping Shi,1 Qing Miao,3 Ujala Rana,4 Dustin Paul Martin,3 Ye Du,1 Gang Zhao,1 Bing Han,1 Chao Zheng,5 Zhimin Fan1
1Department of Breast Surgery, First Hospital of Jilin University, Changchun, Jilin, China; 2Department of Endocrinology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, Guangdong, China; 3Department of Surgery, Medical College of Wisconsin, Milwaukee, WI, USA; 4Division of Neonatology, Department of Pediatrics, Medical College of Wisconsin, Milwaukee, WI, USA; 5Department of Breast Surgery, Second Hospital of Shandong University, Jinan, Shandong, China
Background: Postoperative endocrine therapy is known to reduce recurrence and mortality in patients with estrogen receptor (ER)- or progestogen receptor (PR)-positive breast cancer. Correlates and determinants of compliance with endocrine therapy among Chinese patients with breast cancer are not known. The aim of this study was to elucidate the efficacy and adherence of endocrine therapy in China and suggest effective improvements on the adherence.
Patients and methods: We analyzed the survival of 1,110 patients eligible for endocrine therapy and adherence of 699 patients to endocrine therapy. Kaplan–Meier curves, log-rank tests and Cox proportional hazard models were used to evaluate survival, and logistic regression models were used to assess variables associated with treatment adherence.
Results: Long-term endocrine therapy was associated with lower recurrence rate (HR 0.72; 95% CI 0.56–0.93; p=0.013). Adherence to endocrine therapy was only 63.1%. Sociodemographic characteristics of patients, clinical- and medication-related characteristics and patients’ attitudes were associated with adherence to endocrine therapy.
Conclusion: Adherence to endocrine therapy in Chinese patients with ER+/PR+ breast cancer was <65%. Both patients and physicians should take progressive steps to improve the rate of adherence.
Keywords: breast cancer, endocrine therapy, adherence
Introduction
Breast cancer is the most common cancer in females around the world.1 Nearly half of these cases and 60% of breast cancer-related deaths occur in developing countries.1 Although the incidence of breast cancer in Asia is lower than that in the USA and European countries,1 the annual incidence of breast cancer in China is increasing by 3% each year.2,3 In patients with estrogen receptor (ER)- or progestogen receptor (PR)-positive breast cancer, endocrine therapy has been shown to reduce the incidence of recurrence, metastasis and death.4 According to the National Comprehensive Cancer Network guidelines, patients with ER-/PR-positive invasive breast cancer are eligible for treatment with tamoxifen (TAM) or aromatase inhibitors (AIs), and there is an additional benefit from ovarian ablation or suppression in premenopausal women.5 Nonadherence to the full course of treatment is one of the major reasons for the failure of endocrine therapy. In multicenter clinical trials, such as the Arimidex, Tamoxifen Alone or in Combination trial, the reported nonadherence to endocrine therapy was of the order of 8%–28%.6,7 In the real-world clinical settings, however, nonadherence rates are likely to reach about 50%.8,9 Several factors may influence adherence, such as age, occurrence of complications, financial constraints, lack of information, therapeutic regimen and adverse events.9–11
China is a developing country with a large population and several minority groups. Although the incidence of breast cancer is increasing every year, very few studies have assessed the treatment efficacy and adherence among Chinese patients with breast cancer. The aim of this study was to assess the correlation between survival of patients with hormone receptor-positive breast cancer and treatment adherence. In addition, we assessed the reasons for nonadherence and have suggested feasible strategies to improve adherence.
Patients and methods
Study design and participants
All patients in this retrospective analysis were identified from the First Hospital of Jilin University via the Bethune-Laval Oncology Unit database system (established in 1998, in collaboration with Laval University, Canada). A total of 1,110 patients were enrolled in this study. There was no restriction of age or sex. The inclusion criteria were as follows:
- Primary breast cancer diagnosed by histopathological examination or biopsy specimens between April 1, 2005 and December 31, 2010.
- ER- and/or PR-positive status (>1% positive on immunohistochemical staining).
- T stage<T4 and the absence of distant metastasis.
Out of the 1,110 patients, 699 completed a survey on factors associated with endocrine therapy either telephonically or via face-to-face interview. Data collection was completed on December 31, 2016. The data were analyzed anonymously. The patient selection criteria are shown in Figure 1. Written informed consent was obtained from all patients, and the study was approved by the ethics committee of the First Hospital of Jilin University.
Definition
Adherence includes compliance and/or persistence. Compliance was defined as adherence to the prescribed medications (TAM 20 mg, anastrozole 1 mg or letrozole 2.5 mg) and interruption of <180 days. Persistence was defined as continuation of endocrine therapy for at least 5 years or until the first recurrence, metastasis or death.12,13 In our study, very few of the nonadherent patients belonged to the noncompliance group. Therefore, we mainly focused on the analysis of persistence.
Overall survival (OS) was defined as the time from the the date of diagnosis or date of surgery. Disease-free survival (DFS) was defined as the time from the date of the primary surgery to the date of relapse.
Statistical analyses
Data pertaining to 1,100 ER+/PR+ patients were included in this analysis. Non-normally distributed continuous variables are presented as median (25th to 75th percentiles), and between-group differences were assessed by Kruskal–Wallis test or Mann–Whitney U test. Normally distributed continuous variables are expressed as mean ± SD, and between-group differences were assessed by independent t-test and analysis of variance. Data pertaining to categorical variables are expressed as frequencies and percentages, and between-group differences were assessed by chi-squared test and Fischer’s test, as appropriate. Follow-up began at the time of diagnosis of breast cancer. Patients who were lost to follow up at the first interview were excluded from the survival analysis. Survival analysis of endocrine therapy and related factors was performed using Kaplan–Meier method and compared by log-rank test. Median survival was estimated by the Kaplan–Meier method. Factors associated with adherence to endocrine therapy were assessed using univariate and multivariate logistic regression models. OR and their 95% CIs were used for quantitative analysis. Independent-risk factors associated with p-values <0.05 were identified on multivariate analysis after adjusting for confounding variables. All analyses were performed using SPSS 18.0 software (SPSS Inc., Chicago, IL, USA).
Results
Nonadherence to endocrine therapy is associated with poor clinical outcome
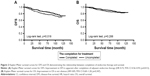
A total of 1,110 patients with hormone receptor-positive breast cancer met the patient selection criteria. The demographic and clinical characteristics are summarized in Table S1. In our study, 92.6% of these patients were followed up for a median duration of 79 months (range 1–122) until December 31, 2016. Among these, 38 patients experienced a relapse, 18 developed contralateral breast cancer, 99 developed distant recurrence, 28 died of breast cancer and 17 patients died of other diseases. DFS and OS at 5 years were 83% and 89%, respectively. Completion of 5 years of endocrine therapy decreased recurrence and death by 28% and 15%, respectively (Table 1). Improvement in DFS was apparent after the completion of adjuvant endocrine therapy (Figure 2A; HR 0.72; 95% CI 0.56–0.93; p=0.013). However, improvement in OS was not obvious (Figure 2B; HR 0.85; 95% CI 0.60–1.20; p=0.347). Survival analysis of other factors is presented in Table S2. Because of the sensitivity of immunohistochemistry, there are still many patients diagnosed as having ER-/PR+ breast cancer.14,15 Therefore, these patients were also included in survival analysis.
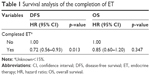  | Table 1 Survival analysis of the completion of ET |
Adherence to endocrine therapy in China is not lower than that in other countries
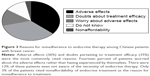
Out of the 699 patients who completed the survey, only 441 (63.1%) completed endocrine therapy, whereas 258 (36.9%) patients did not (80 of these never initiated endocrine therapy). Out of these 699 patients, 351 (50.2%) received only TAM, 177 (25.3%) received only AIs and 55 (7.9%) received both TAM and AI. Adherence to AIs and TAM was 75.7% and 69.2%, respectively. Causes of nonadherence are shown in Figure 3. Of the patients who discontinued the treatment (Figure 3), 36% of patients discontinued endocrine therapy because of its side effects, another 14% stopped treatment after reading the package insert about side effects rather than after having experienced by themselves. There are 35% of patients doubting about the efficacy of endocrine therapy, and 12% were not aware of the necessity.
Association between sociodemographic characteristics and adherence to endocrine therapy
According to our survey results (Table 2), financial constraints (OR 0.55; 95% CI 0.34–0.89; p=0.015), insurance coverage (OR 0.60; 95% CI 0.42–0.88; p=0.01) and education level of patient (OR 2.32; 95% CI 1.35–3.79; p=0.01) had a significant influence on adherence rate. Occupation was not found to be a significant factor. Although we hypothesized that patients employed in a healthcare-related field would have a better understanding of the necessity of endocrine therapy, this subgroup of patients did not exhibit significantly higher adherence than others (Table 2).
Association between clinical- and medication-related characteristics and adherence to endocrine therapy
Poor adherence among patients who were diagnosed with breast cancer before the year 2008 was largely driven by suboptimal endocrine therapy as compared with patients who were diagnosed after the year 2008 (OR 0.63; 95% CI 0.46–0.87; p=0.005). Patients diagnosed with more advanced stage of breast cancer usually had higher adherence rate. For example, patients with one to three metastatic lymph nodes were more likely to take standard medications than their node-negative counterparts (OR 1.56; 95% CI 1.07–2.27; p=0.02). Patients with node-positive breast cancer, especially those with involvement of >4 nodes, are often prescribed adjuvant radiotherapy. Of these patients, the ones who received radiotherapy were more likely to complete endocrine therapy (OR 2.45; 95% CI 1.77–3.38; p<0.001). Completion of the recommended six to eight cycles of chemotherapy was also observed to positively influence adherence (OR 2.43; 95% CI 1.75–3.38; p<0.001). These results showed that adherence for a patient was reflected not only in long-term endocrine therapy but also in other adjuvant therapies. Long-term treatment of TAM can cause adverse effects, such as hot flashes, gynecologic complications, sexual problem, sleeping disorders, bone loss, arthralgia and myalgia, some are even unbearable.16,17 Adverse effects of endocrine therapy are another obstacle to the completion of treatment (OR 0.22; 95% CI 0.13–0.3; p<0.01). As shown in Figure 3, side effect (36%) was the top reason for nonadherence in this study, especially the intolerable adverse effects (OR 0.93; 95% CI 0.05–0.19; p=0.041). Other factors associated with adherence, identified on univariate and multivariate analyses, are summarized in Table 3.
Association between patient’s attitude, education level and adherence to endocrine therapy
A patient’s attitude is shaped by the belief on the diagnosis or treatment protocol by physicians, the understanding of endocrine therapy and their access to information (Table 4). Patients who had a skeptical attitude (OR 0.18; 95% CI 0.10–0.33; p<0.001) or those who were not convinced about the efficacy of endocrine therapy (OR 0.02; 95% CI 0.01–0.06; p<0.001) were more likely to show poor adherence to endocrine therapy. Adherence rates were higher when patients had a good understanding of the efficacy, mechanisms of action and the potential adverse effects of treatment (OR 0.10; 95% CI 0.05–0.19; p<0.01). Well-educated patients, according to previous results, are more likely to accept new information and tend to have higher incomes. Such patients are likely to be more aware of cancer-related information because of better exposure to print and electronic media or have friends with access to medical education and are more likely to comply with endocrine therapy (OR 2.76; 95% CI 1.47–5.42; p=0.003) than those who depend only on the doctor’s advice for treatment-related information.
Improvement of endocrine therapy in clinical practice
As shown in Figure 3, most of the patients discontinued endocrine therapy because of doubts about treatment efficacy and the adverse effects. Therefore, physicians can help improve treatment adherence by inculcating a positive attitude among patients toward endocrine therapy and control of adverse effects.
First, establishment of a good relationship with patients, counseling them regarding their disease condition and convincing them about the necessity of full course of endocrine therapy, is a challenge for every physician. In the real-world clinical settings in China, some families tend to conceal the seriousness of the disease from the patients in order not to perturb them.18 However, patients who underestimate the severity of their condition are more likely to pay inadequate attention to adjuvant therapy. In our study, 54% of the patients in the adherence group and only 11.2% in the nonadherence group believed in the efficacy of endocrine therapy. Among patients with poor adherence, 7.8% were not even aware of the necessity of endocrine therapy and 42.1% believed that they had recovered from breast cancer and that the oral tablets were not of much use. From the year 2007 onward, multidisciplinary consultations are routinely provided for breast cancer patients after surgery in our hospital. This may be an effective way to improve adherence to endocrine therapy among patients treated at our hospital. Oncologists discuss the various available treatment options and involve the patients and their families in treatment decision-making. Such an approach also enables the family members to support the patient in adhering to treatment.
Second, helping patients manage their side effects is very important. Medication toxicity can be relieved by pharmacological or nonpharmacological means. For example, nonsteroidal anti-inflammatory drugs, analgesics, cyclooxygenase-2 inhibitors, opioids and vitamin D supplements can be used to alleviate arthralgia and myalgia.19 Sometimes, switching of treatment from an AI to TAM or from one AI to another AI may also alleviate toxic effects of endocrine therapy.20,21
Periodic reminder to patients is another way to improve treatment adherence. In the Patient’s Anastrozole Compliance to Therapy trial, standard therapy plus reminders were shown to improve compliance with adjuvant endocrine therapy.22 Other methods such as marked-up calendars, reminder notes, pill boxes and frequent monitoring have been used to enhance adherence as well.22
Discussion
TAM for premenopausal ER+/PR+ breast cancer patients and AIs alone or in combination with TAM for postmenopausal patients have been shown to prolong DFS and OS in many randomized controlled clinical trials.4,7,23 Completion of 5 years of treatment was shown to be associated with significantly longer DFS and OS when compared to only 1–2 years of treatment.4 Although the patients in this study have longer DFS, the OS was not longer. Sequence therapy with TAM and AIs will improve DFS significantly;24 therefore, it may be a good choice for postmenopausal patients with early breast cancer.
TAM was not introduced to Chinese breast cancer patients until the 1990s, which is much later than that in other developed countries. Prehn et al25 found that Chinese patients are less likely to receive adjuvant therapy after surgery; however, the status of adherence to endocrine therapy in China is not clear. This study focuses on the patients in Jilin province, which is located in the northeast of China, and is famous for agriculture. A majority of the population is of Han ethnic origin. The GDP and the education level in Jilin province rank in the middle level among all provinces in China. The First Hospital of Jilin University caters to patients from nearby provinces, both from urban and rural areas. Therefore, patients who attend our hospital are representative of a large geographic area. We used the patient information at our hospital to evaluate the status of endocrine therapy in China.
In clinical practice, the adherence is not very high across the world. In previous studies, the rates of non-adherence or discontinuation were found to be as high as 50% around the world.9 Improvement in adherence to endocrine therapy is a global priority. In our study, the adherence rates for of AIs and TAM were 69.2% and 75.7%, respectively, which are at par with those reported from developed countries (77%–81% for AI26,27 and 49%–63% for TAM28,29). This observation is not consistent with the results of Prehn et al’s25 study, in which Chinese women were shown to be less likely to receive adjuvant treatment. This may be because the patients in China were more likely to accept doctors’ advice in recent years. In the current study, sociodemographic, clinical- and medication-related and patients’ attitude-related characteristics were found to be the three major factors associated with adherence to endocrine therapy. Physicians have many ways to help improve endocrine therapy adherence.
Over the years, there has been a gradual improvement in access to treatment for breast cancer and awareness regarding endocrine therapy. Therefore, treatment adherence among patients diagnosed before 2008 was not optimal (60.1% vs 39.9%). In previous studies, extreme age (age >65 or <35 years) of patient,9,30 presence of comorbidity and concurrent treatment for chronic diseases were associated with nonadherence of endocrine therapy,10,31,32 which is inconsistent with our results (Tables 2 and 3). In contrast to our hypothesis, we did not observe improved treatment adherence among breast cancer patients who had a positive family history of breast cancer. Adherence to endocrine therapy among patients belonging to minority population groups was not significantly inferior than that among patients from majority groups; this implies that language difficulties or poor access to education among minority groups may not be a significant contributor to nonadherence to endocrine therapy.
Consistent with the results of Fink et al’s32 study, in which a positive correlation was observed between treatment adherence and metastatic involvement of >4 lymph nodes, we also observed a positive correlation between treatment adherence and involvement of one to three metastatic lymph nodes. This suggests that patients with more advanced disease were more likely to follow the doctors’ advice and adhere to treatment. Endocrine therapy may cause some adverse effects. Consistent with the results of other studies,10,33 side effects were a major cause of nonadherence in this study. This phenomenon indicates a flawed perception of the efficacy and adverse effect profile of endocrine therapy among the Chinese women. Indeed, adverse effects of endocrine therapy have been reported to be a predictor of good efficacy.34
However, patients’ awareness of the benefits and risks of endocrine therapy is also important. Informing patients about both the benefits and the risks of endocrine therapy has a positive effect on adherence. Healthcare providers are better equipped to facilitate improved compliance with endocrine therapy among their patients. Patients who underwent follow-up examinations at the oncology unit were found to be more likely to adhere to endocrine therapy than those who received follow-up care at other units.10 A good relationship between patients and healthcare providers is known to have a positive impact on adherence.33 In a study on postmenopausal women in Europe, only 26% of the patients were aware of the risk of recurrence and only 15% were aware of the side effects of long-term endocrine therapy.35,36 Effective patient–physician communication is known to improve adherence to endocrine therapy.31 Oncologists should ensure adequate patient education regarding their medical condition, importance of endocrine therapy, the prescribed medications, their dosage, mechanism of action, potential side effects, possible severity and the potential decrease in the severity of side effects over time.37,38
Conclusion
In this study, greater adherence to endocrine treatment significantly reduced the recurrence of breast cancer. Unfortunately, patient adherence to endocrine therapy in clinical practice is not more than 65%. Both patient- and medical-related factors were found to affect patient adherence. Adequate patient education and management of side effects are key steps by which healthcare providers can help improve treatment compliance. Sustained efforts by both physicians and patients will help improve survival rate and quality of life of patients with ER+/PR+ breast cancer.
Advantages and limitation
This is the first study that investigated the efficacy of endocrine therapy and the associated adherence rates among women with hormone receptor-positive breast cancer treated at a single center in the northeast China. An analysis of the factors with nonadherence is presented. Information pertaining to treatment adherence was obtained directly from the patients. The reasons for nonadherence reflect the patients’ attitudes and the barriers faced by Chinese breast cancer patients in the real-world setting. However, 37% (411/1,110) of the eligible patients did not complete the survey, which may have affected our results.
Acknowledgments
We thank all the staff members in the Department of Breast Surgery at the First Hospital of Jilin University who helped collect patients’ information in the past 10 years. This work was supported by a grant from Canada International Development Agency (PSCLU010-282/19156) and another grant from National Natural Science Foundation of China (No 30872194).
Disclosure
The authors report no conflicts of interest in this work.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. | ||
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. | ||
Hong W, Dong E. The past, present and future of breast cancer research in China. Cancer Lett. 2014;351(1):1–5. | ||
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365(9472):1687–1717. | ||
Gradishar WJ, Anderson BO, Balassanian R, et al. NCCN guidelines insights breast cancer, version 1.2016. J Natl Compr Canc Netw. 2015;13(12):1475–1485. | ||
Chlebowski RT, Geller ML. Adherence to endocrine therapy for breast cancer. Oncology. 2006;71(1–2):1–9. | ||
Howell A, Cuzick J, Baum M, et al. Results of the ATAC (Arimidex, Tamoxifen, alone or in combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet. 2005;365(9453):60–62. | ||
Hershman DL, Kushi LH, Shao T, et al. Early discontinuation and nonadherence to adjuvant hormonal therapy in a cohort of 8,769 early-stage breast cancer patients. J Clin Oncol. 2010;28(27):4120–4128. | ||
van Herk-Sukel MP, van de Poll-Franse LV, Voogd AC, Nieuwenhuijzen GA, Coebergh JW, Herings RM. Half of breast cancer patients discontinue tamoxifen and any endocrine treatment before the end of the recommended treatment period of 5 years: a population-based analysis. Breast Cancer Res Treat. 2010;122(3):843–851. | ||
Friese CR, Pini TM, Li Y, et al. Adjuvant endocrine therapy initiation and persistence in a diverse sample of patients with breast cancer. Breast Cancer Res Treat. 2013;138(3):931–939. | ||
Lin JH, Zhang SM, Manson JE. Predicting adherence to tamoxifen for breast cancer adjuvant therapy and prevention. Cancer Prev Res (Phila). 2011;4(9):1360–1365. | ||
Kilic N, Myrick ME, Schmid SM, Gueth U. Eligibility, compliance and persistence of sequential therapy with aromatase inhibitors following 2–3 years of tamoxifen in endocrine adjuvant breast cancer therapy. Oncology. 2011;81(3–4):151–157. | ||
Barron TI, Connolly R, Bennett K, Feely J, Kennedy MJ. Early discontinuation of tamoxifen: a lesson for oncologists. Cancer. 2007;109(5):832–839. | ||
Maleki Z, Shariat S, Mokri M, Atri M. ER-negative/PR-positive breast carcinomas or technical artifacts in immunohistochemistry? Arch Iran Med. 2012;15(6):366–369. | ||
Clarke R, Liu MC, Bouker KB, et al. Antiestrogen resistance in breast cancer and the role of estrogen receptor signaling. Oncogene. 2003;22(47):7316–7339. | ||
van Nes JG, Fontein DB, Hille ET, et al. Quality of life in relation to tamoxifen or exemestane treatment in postmenopausal breast cancer patients: a Tamoxifen Exemestane Adjuvant Multinational (TEAM) Trial side study. Breast Cancer Res Treat. 2012;134(1):267–276. | ||
Morales L, Neven P, Timmerman D, et al. Acute effects of tamoxifen and third-generation aromatase inhibitors on menopausal symptoms of breast cancer patients. Anticancer Drugs. 2004;15(8):753–760. | ||
Wang DC, Guo CB, Peng X, Su YJ, Chen F. Is therapeutic non-disclosure still possible? A study on the awareness of cancer diagnosis in China. Support Care Cancer. 2011;19(8):1191–1195. | ||
Dent SF, Gaspo R, Kissner M, Pritchard KI. Aromatase inhibitor therapy: toxicities and management strategies in the treatment of postmenopausal women with hormone-sensitive early breast cancer. Breast Cancer Res Treat. 2011;126(2):295–310. | ||
Guth U, Myrick ME, Schotzau A, Kilic N, Schmid SM. Drug switch because of treatment-related adverse side effects in endocrine adjuvant breast cancer therapy: how often and how often does it work? Breast Cancer Res Treat. 2011;129(3):799–807. | ||
Briot K, Tubiana-Hulin M, Bastit L, Kloos I, Roux C. Effect of a switch of aromatase inhibitors on musculoskeletal symptoms in postmenopausal women with hormone-receptor-positive breast cancer: the ATOLL (articular tolerance of letrozole) study. Breast Cancer Res Treat. 2010;120(1):127–134. | ||
Hadji P, Blettner M, Harbeck N, et al. The Patient’s Anastrozole Compliance to Therapy (PACT) program: a randomized, in-practice study on the impact of a standardized information program on persistence and compliance to adjuvant endocrine therapy in postmenopausal women with early breast cancer. Ann Oncol. 2013;24(6):1505–1512. | ||
Cuzick J, Sestak I, Baum M, et al; ATAC/LATTE Investigators. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncol. 2010;11(12):1135–1141. | ||
Ryden L, Heibert Arnlind M, Vitols S, Hoistad M, Ahlgren J. Aromatase inhibitors alone or sequentially combined with tamoxifen in postmenopausal early breast cancer compared with tamoxifen or placebo – meta-analyses on efficacy and adverse events based on randomized clinical trials. Breast. 2016;26:106–114. | ||
Prehn AW, Topol B, Stewart S, Glaser SL, O’Connor L, West DW. Differences in treatment patterns for localized breast carcinoma among Asian/Pacific islander women. Cancer. 2002;95(11):2268–2275. | ||
Huiart L, Dell’Aniello S, Suissa S. Use of tamoxifen and aromatase inhibitors in a large population-based cohort of women with breast cancer. Br J Cancer. 2011;104(10):1558–1563. | ||
Dittmer C, Roeder K, Hoellen F, Salehin D, Thill M, Fischer D. Compliance to adjuvant therapy in breast cancer patients. Eur J Gynaecol Oncol. 2011;32(3):280–282. | ||
Ma AM, Barone J, Wallis AE, et al. Noncompliance with adjuvant radiation, chemotherapy, or hormonal therapy in breast cancer patients. Am J Surg. 2008;196(4):500–504. | ||
McCowan C, Shearer J, Donnan PT, et al. Cohort study examining tamoxifen adherence and its relationship to mortality in women with breast cancer. Br J Cancer. 2008;99(11):1763–1768. | ||
Partridge AH, Wang PS, Winer EP, Avorn J. Nonadherence to adjuvant tamoxifen therapy in women with primary breast cancer. J Clin Oncol. 2003;21(4):602–606. | ||
Lash TL, Fox MP, Westrup JL, Fink AK, Silliman RA. Adherence to tamoxifen over the five-year course. Breast Cancer Res Treat. 2006;99(2):215–220. | ||
Fink AK, Gurwitz J, Rakowski W, Guadagnoli E, Silliman RA. Patient beliefs and tamoxifen discontinuance in older women with estrogen receptor – positive breast cancer. J Clin Oncol. 2004;22(16):3309–3315. | ||
Cluze C, Rey D, Huiart L, et al. Adjuvant endocrine therapy with tamoxifen in young women with breast cancer: determinants of interruptions vary over time. Ann Oncol. 2012;23(4):882–890. | ||
Henry NL. Endocrine therapy toxicity: management options. Am Soc Clin Oncol Educ Book. 2014;34:e25–e30. | ||
Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47(6):555–567. | ||
Wengstrom Y, Aapro M, Leto di Priolo S, Cannon H, Georgiou V. Patients’ knowledge and experience of adjuvant endocrine therapy for early breast cancer: a European study. Breast. 2007;16(5):462–468. | ||
Briest S, Stearns V. Adjuvant aromatase inhibitors and emerging quality-of-life considerations. Expert Rev Anticancer Ther. 2008;8(1):1–4. | ||
Hartigan K. Patient education: the cornerstone of successful oral chemotherapy treatment. Clin J Oncol Nurs. 2003;7(6 Suppl):21–24. |
Supplementary materials
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.