Back to Journals » Clinical Ophthalmology » Volume 16
Active Learning to Characterize the Full Contrast Sensitivity Function in Cataracts
Authors Vingopoulos F , Kasetty M, Garg I , Silverman RF, Katz R , Vasan RA, Lorch AC, Luo ZK , Miller JB
Received 28 March 2022
Accepted for publication 3 June 2022
Published 21 September 2022 Volume 2022:16 Pages 3109—3118
DOI https://doi.org/10.2147/OPTH.S367490
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Filippos Vingopoulos,1,2 Megan Kasetty,1 Itika Garg,1,2 Rebecca F Silverman,1 Raviv Katz,1,2 Ryan A Vasan,3 Alice C Lorch,3 Zhonghui K Luo,3 John B Miller1,2
1Harvard Retinal Imaging Lab, Massachusetts Eye and Ear, Harvard Medical School, Boston, MA, USA; 2Retina Service, Massachusetts Eye and Ear, Harvard Medical School, Boston, MA, USA; 3Comprehensive Ophthalmology and Cataract Service, Massachusetts Eye and Ear, Department of Ophthalmology, Harvard Medical School, Boston, MA, USA
Correspondence: John B Miller, Harvard Retinal Imaging Lab, Massachusetts Eye and Ear, Harvard Medical School, 243 Charles St, Boston, MA, USA, Tel +1 617 573-3750, Fax +1 617 573-3698, Email [email protected]
Background: To characterize contrast sensitivity function (CSF) in cataractous and pseudophakic eyes compared to healthy control eyes using a novel quantitative CSF test with active learning algorithms.
Methods: This is a prospective observational study at an academic medical center. CSF was measured in eyes with visually significant cataract, at least 2+ nuclear sclerosis (NS) and visual acuity (VA) ≥ 20/50, in pseudophakic eyes and in healthy controls with no more than 1+ NS and no visual complaints, using the Manifold Contrast Vision Meter. Outcomes included Area under the Log CSF (AULCSF) and CS thresholds at 1, 1.5, 3, 6, 12, and 18 cycles per degree (cpd). A subgroup analysis as performed on cataract eyes with VA ≥ 20/25.
Results: A total of 167 eyes were included, 58 eyes in the cataract group, 77 controls, and 32 pseudophakic eyes with respective median AULCSF of 1.053 (0.352) vs 1.228 (0.318) vs 1.256 (0.360). In our multivariate regression model, cataract was associated with significantly reduced AULCSF (P= 0.04, β= − 0.11) and contrast threshold at 6 cpd (P= 0.01, β= − 0.16) compared to controls. Contrast threshold at 6 cpd was significantly reduced even in the subgroup of cataractous eyes with VA ≥ 20/25 (P=0.02, β=− 0.16).
Conclusion: The novel qCSF test detected disproportionate significant contrast deficits at 6 cpd in cataract eyes; this remained significant even in the cataractous eyes with VA ≥ 20/25. CSF testing may enhance cataract evaluation and surgical decision-making, particularly in patients with subjective visual complaints despite good VA.
Keywords: cataract, contrast sensitivity function, Contrast sensitivity, qCSF method
Introduction
Cataract surgery is one of the most commonly performed surgical procedures in all of medicine with an estimated 3.5 million cataract surgeries being performed in the United States every year and more than 23 million worldwide.1 One of the particularities of cataract surgery is that the decision on when to operate is usually based on subjective visual impairment rather than objective, clinically measured visual function metrics. Usually, when a patient feels that their cataract interferes significantly with their everyday vision-related activities, the surgeon will proceed to perform cataract surgery. Symptoms of cataract include worsening vision, muted color intensity, increased glare, halos, image ghosting and poor night vision and have been shown to be strongly correlated with vision-related quality of life.2
Despite visual acuity (VA) being the traditionally used functional metric to objectively evaluate visual function in the clinical setting, various vision-related quality of life scales prove that functional vision in cataract patients cannot be adequately approximated by evaluating VA alone.3–8 VA seems to correlate poorly with patients’ perception of visual disability due to their cataracts.9,10 It is not uncommon that cataract patients with very good visual acuity report subjective visual complaints.3,11–14 These patients are actually as likely to show comparable improvements in symptoms and visual function following surgery as those with decreased visual acuity.15–17 This underscores the need for functional metrics that correlate with patient reported outcomes (PRO) better than VA.
Contrast sensitivity (CS) quantifies the amount of lightness or darkness required to see an object compared to its background. The lower the contrast needed to detect an object (contrast threshold), the higher the contrast sensitivity.18 Cataracts increase the intraocular light scattering and thereby reduce the retinal image contrast.19 Compared to VA, contrast sensitivity seems to correlate better with subjectively perceived visual impairment20 and vision-related everyday activities, including mobility,21 target and face identification,22 driving,23 walking,24 and reading,25 inserting a key into a lock or a plug into a socket.20 Further, contrast sensitivity has been shown to be impaired earlier in the course of ocular pathologies when VA is still unaffected,26,27 the latter often under-estimating the onset and/or severity of visual impairment.28 Despite its promising role in visual function assessment in cataract, imperfections in the currently available contrast tests have prevented the adoption of contrast sensitivity evaluation in routine cataract consults. Conventional laboratory contrast testing is too time-consuming for clinical purposes.29 The traditionally used Pelli-Robson chart only evaluates contrast in one spatial frequency with typically large letters. Pre-printed letter charts that evaluate contrast across various spatial frequencies have shown ceiling/floor effects and poor test-retest repeatability.30–32
The quantitative contrast sensitivity function method (qCSF) leverages active-learning algorithms to test contrast sensitivity across multiple spatial frequencies, in a clinically feasible manner (2–5minutes per eye)33,34 and with both high test-retest reliability and sensitivity in detecting subtle changes in visual function.35 It has already been applied in retinal disorders,36–40 amblyopia,41 glaucoma42 and aging.43
Our group has previously employed the qCSF method and reported significant contrast sensitivity deficits in patients with macular disease and VA ≥20/30, that persisted even in eyes with VA ≥20/20−1.44 We herein present an initial prospective observational study employing the qCSF method to characterize contrast sensitivity function in cataractous and pseudophakic eyes compared to non-cataractous healthy controls.
Methods
This is a prospective, cross-sectional study approved by the Massachusetts Eye and Ear Institutional Review Board (2019P001311) and conducted in accordance with the Declaration of Helsinki and the Health Insurance Portability and Accountability Act. Written informed consent was obtained from all study participants, including consent for publication. Cataract and control subjects were recruited from the Comprehensive Service and Retina Service at the Massachusetts Eye and Ear campus at Longwood. Enrolment took place between December 2016 and February 2019.
Eligible cataract subjects had at least one eye with symptomatic cataract, with at least 2+ nuclear sclerosis (NS) with or without additional cataract subtypes. NO1NC1 of the Lens Opacities Classification System (LOCS) III was considered as 1+NS, while NO2NC1, NO1NC2 or NO2NC2 as 2+NS.45 Exclusion criteria included VA worse than 20/50, previous surgery, or any documentation of visually significant ocular pathology such as retinal, corneal or optic nerve disease. Control eyes were free of any visual significant ocular pathology. Eyes with a maximum of 1+ cataract of any subtype (no more than NO1NC1, no more than C1 and no more than P1) were included as controls so long as the subject did not complain of any visual symptoms; eyes with intraocular lenses without posterior capsular opacification were included in the pseudophakic group.
Clinical Assessment
All subjects underwent routine clinical examination, as appropriate for their scheduled clinic visit. This included documenting ocular medical history, intraocular pressure measured by applanation tonometry (Tono-Pen ® XL - Reichert Technologies, Depew, New York, USA) Snellen’s visual acuity, and slit lamp examination. Fundus examination and refraction were completed in accordance with the patient’s clinic visit. Pupillary dilation, if needed, was deferred until after visual testing was completed, so as to not interfere with contrast sensitivity testing at distance. Grading of the cataract was performed as part of the regular exam following dilation.
Contrast Sensitivity Testing Protocol
Patients were tested for qCSF during their regularly scheduled clinical visits prior to dilation in a standardized environment by a trained research assistant. The study eye or eyes were tested individually, with the fellow eye covered. Subjects used their habitual correction if applicable. If subjects did not have their habitual correction, trial frames with their most recent refraction were used. The Manifold Platform (Adaptive Sensory Technology, San Diego, CA) was employed, following a methodology previously described by our group.39 This novel computational device uses an adaptive computerized Bayesian algorithm to select personalized spatially-filtered optotypes that modulate in both contrast and spatial frequency. Specifically, three filtered Sloan letters of the same spatial frequency are simultaneously displayed in a horizontal line on the testing screen with decreasing contrast. The contrast of the right-most letter is chosen by the quantitative CSF method and is usually near threshold contrast, with the middle and left letters displayed at two and four times the contrast of the right letter, respectively.33 As these spatially-filtered optotypes are presented to the patient, the Bayesian algorithm utilized continuously updates and queries the probability of CSF parameters in order to maximize information gain.33 The patient verbally reports the letters to the experimenter who operates the test with a handheld tablet. The experimenter records either “correct”, “incorrect” or “no response.” The active learning system uses the collected patient data at one spatial frequency to improve sensitivity estimates across all frequencies. This allows for CS testing over a wide range of contrast (128 possible contrasts, 0.002% to 100%) and spatial frequency (19 optotype sizes, approximately 1 to 27 cycles per degree). This also allows relatively quick testing times (2–5 minutes per eye) and have been shown to have robust test-retest reliability.34,35 The test then estimates a CSF curve based off the 25 CSF trials, generating the area under the log contrast sensitivity function curve (AULCSF), integrated from 1 to 18 cycles per degree. The AULCSF is the broad metric of overall CSF.
Study Outcome Measures
Main outcomes measured in this study were outputs of the qCSF method, including AULCSF, contrast acuity (CA), and CS thresholds at six spatial frequencies [1, 1.5, 3, 6, 12, 18 cycles per degree (cpd)]. AULCSF represents a global measure of contrast sensitivity function. Contrast acuity measures the smallest optotype visible with the highest level of contrast (ie the spatial frequency where contrast threshold is 100%, illustrated by the intersection of the contrast sensitivity function curve with the x-axis). Contrast sensitivity thresholds quantify the lowest contrast level that can be seen at each spatial frequency. Baseline demographics were collected for all patients. Visual acuities were recorded and converted from Snellen’s VA to logMAR.
Statistical Analysis
Analysis was carried out using R version 3.4.1. The distribution of continuous numerical data was checked both graphically (histogram and boxplots) and by Shapiro–Wilk Normality Test. Non-normally distributed data was reported as median with Inter-Quartile Range (IGR) and assessed for statistical significance by non parametric tests like Mann Whitney U-Test. Categorical variables were assessed by Pearson’s Chi-squared test with Yates’ continuity correction when applicable. The statistical significance level was set as to two sided p-values <0.05. Mixed effects multiple linear regression model fit by REML (Restricted maximum likelihood) was used to account for the inclusion of both eyes of the same patient. These multilevel mixed models were used to assess the following Contrast Sensitivity Function outcomes like AULCSF, CA, and contrast thresholds at 1, 1.5, 3, 6, 12, 18 cpd between the different groups. Predictor variables were selected based on their unadjusted log-rank statistical significance (p ≤ 0.250) on the univariate analyses for all the potential confounders (eg age, gender, lens status, etc.) separately, for the initial multivariate model. A backward stepwise elimination procedure, based on the Akaike Information Criteria and statistical significance (p ≤ 0.05), was then used to achieve the multivariate models presented. Finally, using the approach described above, we evaluated the qCSF outcomes among various groups in our cohort.
Results
A total of 167 eyes were included, 58 eyes of 45 subjects with cataract(s) disease (19 males and 26 females), 77 eyes of 72 healthy controls (40 males and 32 females) and 32 pseudophakic eyes of 27 patients (12 males and 15 females). The median (IQR) age was 69.00 (11.00) years in the cataract group, 54.00 (19.50) years in the control group (P < 0.001) and 70.00 (8.00) years in the pseudophakic group (P < 0.001). Median (IQR) logMAR visual acuity was 0.097 (0.12) in the cataract group (20/25 Snellen equivalent) versus 0.00 (0.08) in the control group (20/20 Snellen equivalent) (P < 0.001), versus 0.010 (0.08) in the pseudophakic group (20/20 Snellen equivalent)(P < 0.001). Baseline characteristics are summarized in Table 1.
 |
Table 1 Baseline Characteristics |
CSF Outcome Measures in Cataract Eyes versus Controls versus Pseudophakic Eyes
AULCSF, CA and the contrast sensitivity thresholds at each specific spatial frequency for the cataract, control and pseudophakic group are shown in Table 2. (Table 2) AULCSF in the cataract group was 1.053 (0.352) versus 1.228 (0.318) in the control group versus 1.256 (0.360) in the pseudophakic group. When controlling for age in our multivariate regression model, the presence of cataract was associated with significantly reduced AULCSF compared to controls (P= 0.04, β= −0.11) while pseudophakia was not associated with significantly different AULCSF compared to controls (P=0.27, β= 0.07).
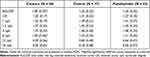 |
Table 2 Contrast Sensitivity Outcome Metrics for the Cataract, Control and Pseudophakic Group |
CA in the cataract group was 1.201 (0.170) versus 1.308 (0.216) in the control group versus 1.268 (0.178) in the pseudophakic group. When controlling for and age in our multivariate regression model, the presence of cataract was not associated with significantly reduced CA compared to controls (P= 0.12, β= −0.05) and pseudophakia was not associated with significantly different CA compared to controls (P=0.13, β= 0.05).
CSF threshold at 1 cpd in the cataract group was 1.339 (0.185) versus 1.387 (0.208) in the control group versus 1.409 (0.268) in the pseudophakic group. When controlling for age and sex in our multivariate regression model, the presence of cataract was not associated with significantly reduced CSF threshold at 1 cpd compared to controls (P= 0.80, β= 0.01) and pseudophakia was not associated with significantly different AULCSF compared to controls (P= 0.11, β= 0.06).
CSF threshold at 1.5 cpd in the cataract group was 1.365 (0.199) versus 1.448 (0.230) in the control group versus 1.450 (0.242) in the pseudophakic group. When controlling for age and sex in our multivariate regression model, the presence of cataract was not associated with significantly reduced CSF thresholds at 1.5 cpd compared to controls (P= 0.79, β= −0.01) and pseudophakia was not associated with significantly different AULCSF compared to controls (P= 0.09, β= 0.07).
CSF threshold at 3 cpd in the cataract group was 1.347 (0.225) versus 1.460 (0.275) in the control group versus 1.447 (0.237) in the pseudophakic group. When controlling for age in our multivariate regression model, the presence of cataract was not associated with significantly reduced CSF thresholds at 3 cpd compared to controls (P= 0.07, β= −0.08) and pseudophakia was not associated with significantly different AULCSF compared to controls (P= 0.32, β= 0.05).
CSF threshold at 6 cpd in the cataract group was 1.046 (0.457) versus 1.248 (0.239) in the control group versus 1.309 (0.406) in the pseudophakic group. When controlling for age in our multivariate regression model, the presence of cataract was associated with significantly reduced CSF thresholds at 6 cpd compared to controls (P= 0.01, β= −0.16) while pseudophakia was not associated with significantly different AULCSF compared to controls (P= 0.48, β= 0.05).
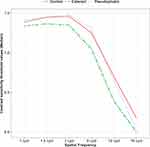
CSF threshold at 12 cpd in the cataract group was 0.386 (0.561) versus 0.694 (0.485) in the control group versus 0.638 (0.469) in the pseudophakic group. When controlling for age in our multivariate regression model, the presence of cataract was not associated with significantly reduced CSF threshold at 12 cpd compared to controls (P= 0.10, β= −0.12) and pseudophakia was not associated with significantly different AULCSF compared to controls (P= 0.20, β= 0.11). CSF thresholds at 18 cpd in the cataract group was 0.000 (0.051) versus 0.175 (0.480) in the control group versus 0.036 (0.368) in the pseudophakic group. When controlling for in our multivariate regression model, the presence of cataract was not associated with significantly reduced CSF thresholds at 18 cpd compared to controls (P= 0.17, β= −0.07) and pseudophakia was not associated with significantly different AULCSF compared to controls (P= 0.40, β= 0.05) Figure 1 represents the AULCSF, CA and reductions in contrast sensitivity thresholds at each spatial frequency in cataract eyes compared to control eyes and pseudophakic eyes (Figure 1).
Subgroup Analysis on Eyes with Very Good Visual Acuity (VA ≥20/25)
In a subgroup analysis including only the eyes with vision equal or better than 20/25, (27 cataract versus 63 control eyes), after controlling for age, contrast threshold at 6 cpd remained statistically significantly reduced in the cataract group when compared to the control group (P= 0.03, β= −0.14). Reductions in AULCSF, CA and in the lower (1, 1.5, 3 cpd) and higher (12, 18 cpd) spatial frequencies were also observed, though without reaching statistical significance (Figure 2).
Discussion
In this initial prospective cross-sectional observational study, we employed the novel qCSF method to characterize contrast sensitivity function in cataract disease and pseudophakic eyes compared to healthy controls. We detected a generalized decrease in the broad metric of CSF, AULCSF, and disproportionate deficits in contrast sensitivity thresholds in cataract eyes with subjective symptomatology versus healthy controls. Importantly, these disproportionate deficits in contrast sensitivity persisted even in cataract eyes with VA as good as 20/25 or better. This suggests that contrast sensitivity measured with the qCSF method may be able to detect more subtle changes in visual function in eyes with cataract than the VA does.
Perhaps most importantly, we detected a disproportionate decrease in contrast thresholds at the spatial frequency of 6 cpd, a spatial frequency that is particularly linked with vision-related everyday life activities. It has been shown that contrast sensitivity at 3 and 6 cpd is associated with everyday activities such as finding a door on a wall or discerning a bus from a car31 while contrast sensitivity thresholds specifically at 6 cpd was found to be the best predictor of road sign and object identification.22 The presence of cataract was not associated with significantly reduced CSF threshold at lower (1, 1.5, 3 cpd) or higher (12, 18 cpd) spatial frequencies. Pseudophakia was not associated with significantly different contrast outcome measures compared to control eyes. Of note, the contrast sensitivity deficits at 6 cpd detected herein in cataractous eyes would have gone unnoticed if contrast sensitivity testing was performed using the traditional Pelli-Robson chart that only tests contrast at the spatial frequency of 0.5–1cpd (when tested at 1 meter distance as the manual suggests). This is clinically relevant, and may lead physicians to overestimate the functional vision of patients during the cataract surgery decision-making process.
Many cataract studies have incorporated various contrast sensitivity tests attempting to evaluate patients’ visual function in a more accurate and comprehensive manner.4–8 Measuring contrast sensitivity thresholds across a wide spectrum of spatial frequencies seems to provide valuable information regarding how visual deficits may affect patients’ vision-related quality of life. As the traditional Pelli-Robson test is limited in that respect, other contrast sensitivity tests have been developed and reported in the clinical studies. However, none of these tests have yet been established and incorporated into the routine clinical practice. Currently available tests that evaluate contrast thresholds across various spatial frequencies such as the Vistech or the Functional Acuity Contrast Test (FACT) tests have been repeatedly shown to have ceiling effects, floor effects and poor test-retest repeatability such that they are not used in clinical practice.30,46,47 With the advent of the qCSF method, active learning algorithms enable the global shape of contrast sensitivity function to be tested in a time-efficient (2–5 minutes per eye) manner, across multiple spatial frequencies; at the same time the qCSF test has been shown to have high sensitivity in detecting subtle changes in visual function and great test-retest repeatability.34,35
An increasing importance is being placed on patient reported outcomes in cataract surgery, a measure that is guided mainly by the subjective visual impairment reported by the patient rather than deteriorating objectively measured visual function metrics. A visual function outcome that correlates to subjective visual impairment and vision-related everyday life activities better than visual acuity does, will enhance the clinician’s understanding of the patient’s experience of their vision. This will in turn guide surgical decision making in a patient-centered manner.
Unsurprisingly, cataract surgery improves not only visual function but also overall quality of life, self-assessed health and mental health, cognition, depression, earnings, mobility, self-care, life satisfaction, self-efficacy and self-reported overall happiness.48–50 Further, patient happiness after cataract surgery is strongly correlated with subjectively perceived improvement in their functional vision.48 For cataract surgeons, being able to routinely evaluate visual function in a way that is both objective and highly correlated with patients’ subjective visual complaints, would render surgical decision making a patient-centered process. Contrast sensitivity has been suggested in the past as a visual function metric that strongly correlates with subjective visual impairment and vision-related quality of life. Now with the time-efficient, sensitive and highly reliable qCSF method, contrast sensitivity has the potential to be incorporated in the routine clinical practice.
There are certain limitations in this study. This is only a moderate sample size cross-sectional study that included patients with at least 2+ nuclear sclerosis that may or may not also have other coexisting cataract subtypes. Therefore our results cannot be generalized to all cataract subtypes nor directed towards specific cataract subtypes. Another limitation of this exploratory study is the lack of standardization of cataract grading among several providers. Ideally future studies should employ the LOCS III system to improve the consistency of the grading.45 We set out to compare eyes with visually significant cataract to eyes that lacked visually significant ocular pathology. While none of the control subjects had visual symptoms, some did have mild opacification of the lens, no greater than 1+ NS. The fact that we still found statistically significant reductions in contrast sensitivity in our cataract study group compared to a control group with some mild cataract only strengthens our findings. Additionally, while pseudophakia was not associated with decreased CSF compared to cataract or controls, a sub-analysis based on type of intraocular lens (IOL) was not performed. Further studies utilizing qCSF testing to characterize CSF in pseudophakic eyes with different types of IOL would be valuable. A longitudinal follow up study is ongoing aiming to showcase the improvement in contrast sensitivity function after cataract surgery, investigating whether the beneficial effect on cataract surgery is even greater than the one currently measured employing VA as the only visual function metric.
In conclusion, employing the qCSF method, we detected disproportionate deficits in contrast sensitivity thresholds in cataract eyes versus controls, at specific spatial frequencies that are particularly linked with vision-related everyday life activities; these disproportionate deficits in persisted even in cataract eyes with VA ≥20/25, suggesting that contrast sensitivity may be able to detect more subtle changes in visual function of eyes with cataract than the traditional VA testing does. These deficits would have been missed using the traditional Pelli-Robson chart. Contrast sensitivity measured with the qCSF emerges as a promising adjunct visual function endpoint, with the potential to be incorporated in the standard routine cataract evaluation to enhance surgical decision-making for cataract surgery.
Data Sharing Statement
Data will be available upon reasonable request to Filippos Vingopoulos, [email protected].
Author Contributions
Concept and design: FV, MK, RAV, ACL, ZKL, JBM. Subject identification: RAV, ACL, ZKL, JBM. Data collection: FV, MK, RFS, RK Data analysis: IG, MK. Data interpretation: FV, MK, IG. Initial manuscript draft: FV, MK. Critical Revision of the manuscript: FV, MK, IG, RFS, RK, RAV, ACL, ZKL, JBM. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Lions International Equipment Fund and Massachusetts Lions Club (Grant #530125).
Disclosure
Vingopoulos, Kasetty, Garg, Silverman, Katz, Vasan, Luo: None, Miller: Consultant for Alcon, Allergan, Zeiss, Heidelberg, Genentech. Lorch: personal fees from Regeneron.
References
1. Lindstrom R. Thoughts on cataract surgery. Rev Ophthalmol. 2015;9:1.
2. Lee JE, Fos PJ, Sung JH, et al. Relationship of cataract symptoms of preoperative patients and vision-related quality of life. Qual Life Res. 2005;14(8):1845–1853. doi:10.1007/s11136-005-4348-8
3. Crabtree HL, Hildreth AJ, O’Connell JE, et al. Measuring visual symptoms in British cataract patients: the cataract symptom scale. Br J Ophthalmol. 1999;83(5):519–523. doi:10.1136/bjo.83.5.519
4. Smith AF. Criteria for cataract surgery: the role of visual acuity and visual function. Br J Ophthalmol. 1999;83(5):510–511. doi:10.1136/bjo.83.5.510
5. Superstein R, Boyaner D, Overbury O, et al. Glare disability and contrast sensitivity before and after cataract surgery. J Cataract Refract Surg. 1997;23(2):248–253. doi:10.1016/S0886-3350(97)80349-5
6. Elliott DB, Patla A, Bullimore MA. Improvements in clinical and functional vision and perceived visual disability after first and second eye cataract surgery. Br J Ophthalmol. 1997;81(10):889–895. doi:10.1136/bjo.81.10.889
7. Superstein R, Boyaner D, Overbury O. Functional complaints, visual acuity, spatial contrast sensitivity, and glare disability in preoperative and postoperative cataract patients. J Cataract Refract Surg. 1999;25:575–581. doi:10.1016/S0886-3350(99)80059-5
8. Elliott DB, Patla AE, Furniss M, et al. Improvements in clinical and functional vision and quality of life after second eye cataract surgery. Optom Vis Sci. 2000;77(1):13–24. doi:10.1097/00006324-200001000-00009
9. Steinberg EP, Tielsch JM, Schein OD, et al. The VF-14. An index of functional impairment in patients with cataract. Arch Ophthalmol. 1994;112(5):630–638. doi:10.1001/archopht.1994.01090170074026
10. Abrahamsson M, Carlsson B, Törnqvist M, et al. Changes of visual function and visual ability in daily life following cataract surgery. Acta Ophthalmol Scand. 1996;74(1):69–73. doi:10.1111/j.1600-0420.1996.tb00686.x
11. Mordue A, Parkin DW, Baxter C, et al. Thresholds for treatment in cataract surgery. J Public Health Med. 1994;16(4):393–398. doi:10.1093/oxfordjournals.pubmed.a043019
12. Elliott DB, Hurst MA, Weatherill J. Comparing clinical tests of visual function in cataract with the patient’s perceived visual disability. Eye. 1990;4(Pt 5):712–717. doi:10.1038/eye.1990.100
13. Bernth-Petersen P. Visual functioning in cataract patients. Methods of measuring and results. Acta Ophthalmol. 1981;59(2):198–205. doi:10.1111/j.1755-3768.1981.tb02979.x
14. Williamson TH, Strong NP, Sparrow J, et al. Contrast sensitivity and glare in cataract using the Pelli-Robson chart. Br J Ophthalmol. 1992;76(12):719–722. doi:10.1136/bjo.76.12.719
15. Schein OD, Steinberg EP, Cassard SD, et al. Predictors of outcome in patients who underwent cataract surgery. Ophthalmology. 1995;102(5):817–823. doi:10.1016/S0161-6420(95)30952-9
16. Desai P, Reidy A, Minassian DC, et al. Gains from cataract surgery: visual function and quality of life. Br J Ophthalmol. 1996;80(10):868–873. doi:10.1136/bjo.80.10.868
17. Rosen PN, Kaplan RM, David K. Measuring outcomes of cataract surgery using the quality of well-being scale and VF-14 visual function index. J Cataract Refract Surg. 2005;31(2):369–378. doi:10.1016/j.jcrs.2004.04.043
18. Pelli DG, Bex P. Measuring contrast sensitivity. Vision Res. 2013;90:10–14. doi:10.1016/j.visres.2013.04.015
19. Chua BE, Mitchell P, Cumming RG. Effects of cataract type and location on visual function: the blue mountains eye study. Eye. 2004;18(8):765–772. doi:10.1038/sj.eye.6701366
20. West SK, Rubin GS, Broman AT, et al. How does visual impairment affect performance on tasks of everyday life? The SEE project Salisbury eye evaluation. Arch Ophthalmol. 2002;120(6):774–780. doi:10.1001/archopht.120.6.774
21. Marron JA, Bailey IL. Visual factors and orientation-mobility performance. Am J Optom Physiol Opt. 1982;59(5):413–426. doi:10.1097/00006324-198205000-00009
22. Owsley C, Sloane ME. Contrast sensitivity, acuity, and the perception of ‘real-world’ targets. Br J Ophthalmol. 1987;71(10):791796. doi:10.1136/bjo.71.10.791
23. Owsley C, McGwin G Jr. Vision and driving. Vision Res. 2010;50(23):2348–2361. doi:10.1016/j.visres.2010.05.021
24. Geruschat DR, Turano KA, Stahl JW. Traditional measures of mobility performance and retinitis pigmentosa. Optom Vis Sci. 1998;75(7):525–537. doi:10.1097/00006324-199807000-00022
25. Leat SJ, Woodhouse JM. Reading performance with low vision aids: relationship with contrast sensitivity. Ophthalmic Physiol Opt. 1993;13(1):9–16. doi:10.1111/j.1475-1313.1993.tb00420.x
26. Jindra LF, Zemon V. Contrast sensitivity testing: a more complete assessment of vision. J Cataract Refract Surg. 1989;15(2):141–148. doi:10.1016/S0886-3350(89)80002-1
27. Woods RL, Wood JM. The role of contrast sensitivity charts and contrast letter charts in clinical practice. Clin Exp Optom. 1995;78(2):43–57. doi:10.1111/j.1444-0938.1995.tb00787.x
28. Murugappan M, Vayalil J, Bade A, et al. Reliability of quick contrast sensitivity function testing in adults without ocular disease and patients with retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2016;57(12):616.
29. Kelly DH, Savoie RE. A study of sine-wave contrast sensitivity by two psychophysical methods. Percept Psychophys. 1973;14(2):313–318. doi:10.3758/BF03212397
30. Pesudovs K, Hazel CA, Doran RML, et al. The usefulness of Vistech and FACT contrast sensitivity charts for cataract and refractive surgery outcomes research. Br J Ophthalmol. 2004;88(1):11–16. doi:10.1136/bjo.88.1.11
31. Richman J, Spaeth GL, Wirostko B. Contrast sensitivity basics and a critique of currently available tests. J Cataract Refract Surg. 2013;39(7):1100–1106. doi:10.1016/j.jcrs.2013.05.001
32. Bühren J, Terzi E, Bach M, et al. Measuring contrast sensitivity under different lighting conditions: comparison of three tests. Optom Vis Sci. 2006;83(5):290–298. doi:10.1097/01.opx.0000216100.93302.2d
33. Lesmes LA, Lu ZL, Baek J, et al. Bayesian adaptive estimation of the contrast sensitivity function: the quick CSF method. J Vis. 2010;10(3):
34. Dorr M, Wille M, Viulet T, et al. Next-generation vision testing: the quick CSF. Curr Dir Biomed Eng. 2015;1(1):131–134. doi:10.1515/cdbme-2015-0034
35. Hou F, Lesmes LA, Kim W, et al. Evaluating the performance of the quick CSF method in detecting contrast sensitivity function changes. J Vis. 2016;16(6):18. doi:10.1167/16.6.18
36. Silverman RF, Kasetty M, Vingopoulos F, et al. Measuring contrast sensitivity function with active learning in retinal vein occlusion: a new endpoint of visual function. Ophthalmic Surg Lasers Imaging Retina. 2020;51(7):392–400. doi:10.3928/23258160-20200702-04
37. Thomas M, Silverman RF, Vingopoulos F, et al. Active learning of contrast sensitivity to assess visual function in macula-off retinal detachment. J Vitreoretin Dis. 2021;5(4):313–320. doi:10.1177/2474126420961957
38. Wang J, Cui Y, Vingopoulos F, et al. Disorganisation of retinal inner layers is associated with reduced contrast sensitivity in retinal vein occlusion. Br J Ophthalmol. 2020;106:241–245.
39. Vingopoulos F, Wai KM, Katz R, et al. Measuring the Contrast sensitivity function in non-neovascular and neovascular age-related macular degeneration: the quantitative contrast sensitivity function test. J Clin Med. 2021;10(13):2768. doi:10.3390/jcm10132768
40. Vingopoulos F, Garg I, Kim EL, et al. Quantitative contrast sensitivity test to assess visual function in central serous chorioretinopathy. British J Ophthalmol. 2022. doi:10.1136/bjophthalmol-2021-320415
41. Hou F, Huang CB, Lesmes L, et al. qCSF in clinical application: efficient characterization and classification of contrast sensitivity functions in amblyopia. Invest Ophthalmol Vis Sci. 2010;51(10):5365–5377. doi:10.1167/iovs.10-5468
42. Lin S, Mihailovic A, West SK, et al. Predicting visual disability in glaucoma with combinations of vision measures. Transl Vis Sci Technol. 2018;7(2):22. doi:10.1167/tvst.7.2.22
43. Yan FF, Hou F, Lu ZL, et al. Efficient characterization and classification of contrast sensitivity functions in aging. Sci Rep. 2017;7(1):5045. doi:10.1038/s41598-017-05294-0
44. Wai KM, Vingopoulos F, Garg I, et al. Contrast sensitivity function in patients with macular disease and good visual acuity. Br J Ophthalmol. 2021;106:839–844. doi:10.1136/bjophthalmol-2020-318494
45. Chylack LT
46. Reeves BC, Wood JM, Hill AR, Vistech VCTS. 6500 charts within and between session reliability. Optom Vis Sci. 1991;68(9):728–737. doi:10.1097/00006324-199109000-00010
47. Elliott DB, Bullimore MA. Assessing the reliability, discriminative ability, and validity of disability glare tests. Invest Ophthalmol Vis Sci. 1993;34(1):108–119.
48. Yotsukura E, Ayaki M, Nezu N, et al. Changes in patient subjective happiness and satisfaction with cataract surgery. Sci Rep. 2020;10(1):17273. doi:10.1038/s41598-020-72846-2
49. Ishii K, Kabata T, Oshika T. The impact of cataract surgery on cognitive impairment and depressive mental status in elderly patients. Am J Ophthalmol. 2008;146(3):404–409. doi:10.1016/j.ajo.2008.05.014
50. Feeny S, Posso A, McDonald L, et al. Beyond monetary benefits of restoring sight in Vietnam: evaluating well-being gains from cataract surgery. PLoS One. 2018;13(2):e0192774. doi:10.1371/journal.pone.0192774
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.