Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 17
ACE Gene Mutations (rs577350502) in Early-Onset and Recurrent Myocardial Infarction: A Case Report and Review
Authors Deng X, Guo X, Chen X, Zeng X, Guo J, Bai X, Zhang P, Wang Y
Received 19 December 2023
Accepted for publication 4 April 2024
Published 20 April 2024 Volume 2024:17 Pages 163—169
DOI https://doi.org/10.2147/PGPM.S455740
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Martin H Bluth
Xiaoxi Deng,1,* Xiaofei Guo,1,* Xiaojie Chen,2 Xinyu Zeng,1 Jiamin Guo,1 Xin Bai,1 Ping Zhang,1 Yuan Wang1
1Department of Pathology, Wangjing Hospital, China Academy of Chinese Medical Sciences, Beijing, 100102, People’s Republic of China; 2Department of Emergency, Wangjing Hospital, China Academy of Chinese Medical Sciences, Beijing, 100102, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yuan Wang, Ping Zhang, Department of Pathology, Wangjing Hospital, China Academy of Chinese Medical Sciences, 6 Wangjing Zhonghuan South Road, Chaoyang District, Beijing, 100102, People’s Republic of China, Tel +86 010-84739040, Email [email protected]; [email protected]
Background: Acute myocardial infarction (AMI) is a severe acute coronary syndrome, demonstrating a trend toward affecting younger individuals in recent years. The association between early-onset myocardial infarction and single nucleotide polymorphism necessitates further exploration and evaluation.
Case description: We present a case of a patient experiencing early-onset and recurrent myocardial infarction. The patient underwent stent implantation for myocardial infarction at the age of 53 and subsequently encountered two more myocardial infarctions within a span of 16 years. Following interventional therapy, genetic testing was conducted to assess the efficacy of subsequent anti-heart failure medications, with the aim to preemptively address heart failure risks. Genetic testing revealed a mutation in the angiotensin-converting enzyme (ACE) gene (rs577350502, g.63488533C>A), characterized by an intron-deletion single nucleotide variant.
Conclusion: While this variant has not been previously reported to be associated with any specific disease, we hypothesize that it may contribute to the susceptibility and risk of myocardial infarction and coronary heart disease in the patient under consideration. This observation underscores the significance of investigating the insertion/deletion polymorphisms of the ACE gene in the context of AMI and emphasizes the necessity for further validation of this variant and other genetic markers associated with AMI in related diseases.
Keywords: ACE, case reports, gene mutations, myocardial infarction, SNV
Introduction
Acute myocardial infarction (AMI) is a serious complication of coronary heart disease (CHD) primarily arising from severe stenosis or occlusion of coronary arteries, resulting in ischemic necrosis of the corresponding myocardial supply region. It represents a critical pathophysiological consequence within the spectrum of CHD. However, not all patients with CHD experience an AMI, and there might be some certain gene polymorphisms that contribute to the progression of coronary artery disease (CAD) into AMI.1 Consequently, single nucleotide polymorphisms (SNPs) linked to AMI episodes warrant careful consideration. Early-onset AMI is defined by its occurrence in males under the age of 55 and females under the age of 60.2 In this report, we present a case of a patient with early-onset and recurrent myocardial infarction, experiencing the initial episode at 53 years of age and subsequently enduring two more attacks over the next 16 years. Blood leukocyte DNA testing was conducted utilizing polymerase chain reaction (PCR) and Sanger sequencing, adhering to the ethical principles outlined in the Declaration of Helsinki.
Case Description
A 69-year-old male was transported to our hospital by ambulance following a heart attack, presenting with symptoms such as chest tightness, breathlessness, and vomiting of stomach contents. An emergency electrocardiogram (ECG) conducted en route revealed sinus rhythm with ST elevation in leads II, III, and AVF. Subsequent coronary angiography revealed coronary atherosclerotic heart disease, manifesting as double-vessel disease affecting the anterior descending artery and the right coronary artery (see Figure 1). The patient’s blood test is shown in detail in Table 1. As per established diagnostic criteria,3 the patient was diagnosed with acute inferior myocardial infarction. Emergency intervention was conducted, involving stent implantation for the right posterior descending coronary artery and the right posterior lateral coronary artery.
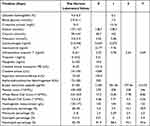 |
Table 1 Blood Test Indexes of the Patient |
 |
Figure 1 Coronary angiography. |
Remarkably, the patient’s medical history revealed that this marked the third occurrence of such a procedure. The initial diagnosis of coronary atherosclerotic heart disease was made 16 years ago, leading to coronary stent implantation for myocardial infarction at the ages of 53 and 58, resulting in a total of 3 stents being implanted. Postoperatively, the patient consistently took enteric-coated aspirin tablets; however, this was later discontinued due to gastrointestinal bleeding. The patient, a long-term smoker of over 50 years averaging 30 cigarettes per day, reported no family history of genetic disease and no previous history of hypertension. Considering the potential risk of heart failure associated with myocardial infarction, our treatment plan included the administration of anti-heart failure medications, along with relevant genetic testing.
PCR testing, in this case, utilized the TIANLONG TL 988 Real-Time PCR System along with Angiotensin Converting Enzyme (ACE) insertion/deletion (I/D) detection kit (Lot.HY221107, Wuxi Ruiqi Gene Biotechnology Co., Ltd.). The detection methodology involved the use of the PCR dissolution curve method, with the positive control DD type exhibiting a melting temperature (Tm) of 51.5°C, and the type II Tm measured at 58.5°C. The proband in this case exhibited ACE D/D genotype, as depicted by the dissolution peak curve illustrated in Figure 2.
 |
Figure 2 PCR solubility peak curve results. |
Sanger sequencing revealed a C>A mutation at the 7th base preceding the I/D mutation point (see Figure 3). The identified mutation was cross-referenced and assessed through three distinct databases: dbSNP (http://www.ncbi.nlm.nih.gov/projects/SNP/), 1000 Genomes (http://www.1000genomes.org/), ExAC (http://exac.broadinstitute.org/), and gnomAD (http://gnomad.broadinstitute.org/). The mutation site was identified as rs577350502, positioned at chr17:63488533 (GRCh38.p14), and characterized as a single nucleotide variant (SNV). It is noteworthy that, since 2019, this mutation has only been documented in two patients in Japan, as recorded in the dbSNP database. However, detailed clinical descriptions of this mutation were not provided by the recorder. In this case, the advanced age of the proband made it impractical to trace the ACE genotype of his parents. Additionally, his wife and daughter declined to participate in genetic testing at our hospital.
 |
Figure 3 Sequencing results of the proband. The arrow points to the position of the SNP. |
Given the patient’s ACE gene being of the D/D type, which could potentially influence the efficacy of ACE inhibitors (ACEI) and β-receptor antagonists, the patient was administered spironolactone and furosemide instead of ACEI to alleviate cardiac workload. The patient responded positively to this alternative treatment regimen and was discharged with grade I cardiac function (Killip). Upon returning to our hospital two months later, the patient reported no significant discomfort.
Discussion
AMI is an acute coronary syndrome characterized by high global mortality and morbidity, representing a severe consequence of CHD. It is estimated that nearly half of American adults with CHD also encountered AMI4 in their life. Early-onset myocardial infarction, occurring before the age of 55 years, is more concerned now,2 while the related genetic investigation of is far less than CHD.1,5,6
The patient experienced the first AMI at the age of 53 and subsequently endured two additional attacks over the next 16 years. Emergency coronary angiography revealed double-vessel disease affecting the anterior descending artery and the right coronary artery. The patient was found to have a high level of IL-6,CRP,NT-proBNP and a D/D type of the ACE gene with a rare mutation (rs577350502). Then, he was diagnosed with AMI and underwent stent implantation. Cardiac load was relieved by administration of spironolactone and furosemide. The patient exhibited a positive recovery trajectory post-discharge.
Carrying the ACE D allele has been linked to an elevated risk of coronary artery disease, hypertension, diabetes mellitus, dyslipidemia, and increased mortality associated with COVID-19.7 The rs577350502 mutation is situated within the genomic region encompassed by rs1799752. The rs1799752 variant signifies an ACE (I/D) polymorphism, which influences the clinical efficacy of captopril. Moreover, rs1799752 is associated with susceptibility8 and cardiac autonomic modulation9 in patients with CAD. Approximately 50% of the variation in blood ACE levels is attributed to ACE gene (I/D) polymorphisms,10 widely acknowledged as a risk factor for CAD.11 Particularly noteworthy is the association between ACE I/D polymorphisms and the degree of coronary atherosclerosis in males with elevated total cholesterol levels (≥200 mg/dl).12 ACE gene polymorphisms (I/D) influence enzyme activity, consequently impacting the risk of CAD.13
Studies have demonstrated a close association between ACE gene polymorphisms, specifically the deletion type (D/D), and early-onset cardiovascular diseases. ACE gene polymorphisms have been linked to early-onset cardiovascular disease in the Iranian population.14 Additionally, SNPs of ACE (rs4646994) as well as those of MTHFR and PON1 have been identified associated with early-onset CAD.15 AMI, a condition primarily resulting from myocardial ischemic necrosis due to coronary artery narrowing or spasm, involves the angiotensin-converting enzyme encoded by the ACE gene. The ACE gene, encoding angiotensin-converting enzyme, plays a role in catalyzing the conversion of angiotensin I to the physiologically active peptide angiotensin II, thereby regulating blood pressure and electrolyte balance. ACE activity can contribute to sodium and water retention, increased cardiac load, and heightened vasoconstriction. These effects may aggravate coronary artery stenosis and potentially lead to spasms, providing a plausible explanation for the association between ACE gene mutations and the onset of AMI. The application of ACEI can inhibit this activity.
The patient had elevated levels of IL-6, CRP, NT-proBNP. The elevation in plasma IL-6 levels after cardiac surgery could be inhibited in long-term ACEI.16 The presence of D allele was also associated with higher IL-6.17 IL-6 can enhance the activity of CD4+T cells through STAT3 pathway.18 This might be how AMI induces rapid influx of CD4+T cells into the myocardium, which participates in promoting the process of ventricular remodeling and progressive heart failure.19 Besides, taking ACEI can also reduce CRP after COVID-19 infection and NT-proBNP levels in heart failure patients.20,21 AMI patients had a low proportion of CD73 on CD4+T cells, while CD73 is negatively correlated with serum NT-proBNP, decreasing tissue tropism and immunosuppressive function, while disrupting myocardial repair.22 This may be the mechanism for how ACE decreases repair of myocardial damage, by increasing the amount of CD4+ T-cells and decreasing CD73 phenotype delayed myocardium healing and ventricle remolding.19,23
The identification of the rs577350502 SNV indicating the ACE (D/D) genotype in a patient experiencing early-onset myocardial infarction holds significance, particularly in the absence of a history of hypertension. This contradictory manifestation suggests the existence of other underlying mechanisms contributing to the occurrence of early-onset and recurrent myocardial infarction in such patients, warranting further research and exploration. However, in the case of this patient, timely genetic testing proved instrumental in avoiding the potentially ineffective use of ACEI and consequently reducing the risk of heart failure post-myocardial infarction. This highlights the significance of genetic testing in clinical diagnosis and treatment (see Figure 4). The findings emphasize the need for clinicians to integrate genetic testing into clinical practice, enhancing the efficiency and effectiveness of treatment strategies.
 |
Figure 4 Summary or prospect description of this study. The figure was drawn by Figdraw. |
Study Limitations
Due to the disagreement of patients’ families, we did not collect their gene mutation and related medical history. The mutation is extremely rare, so it is necessary to further verify its influence on the early-onset and recurrence of myocardial infarction. We look forward to addressing the issue of confounding factors in the occurrence and development of AMI related to gene mutations in the future.
Conclusion
SNVs have garnered increasing attention in medical research, and the detection of rs577350502SNV in the blood of patients with early-onset and recurrent myocardial infarction represents a significant contribution. The timely identification of this SNV enables prompt adjustment in medical interventions, which is of great significance for the prevention and treatment of early-onset and recurrent myocardial infarction.
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
This study was conducted with approval from the Ethics Committee of Wangjing Hospital, China Academy of Chinese Medical Sciences (WJEC-KT-2022-065-P001). This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from the participant.
Consent for Publication
Consent for the publication of the case was obtained from the patient.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
National Natural Science Foundation of China (No.82174415). Science and technology innovation project of Chinese Academy of Traditional Chinese Medicine (No. CI2021A05054).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Lu X, Liu Z, Cui Q. et al. A polygenic risk score improves risk stratification of coronary artery disease: a large-scale prospective Chinese cohort study. Eur Heart J. 2022;43(18):1702–1711. doi:10.1093/eurheartj/ehac093
2. Tonstad S, Westheim A. Implementation of guidelines to screen relatives of patients with premature coronary heart disease in a hospital setting. Am j Cardiol. 2002;90(11):1211–1214. doi:10.1016/S0002-9149(02)02836-9
3. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–177. doi:10.1093/eurheartj/ehx393
4. Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics—2018 update: a Report From the American Heart Association. Circulation. 2018;137:12.
5. Buniello A, MacArthur JAL, Cerezo M, et al. The NHGRI-EBI GWAS Catalog of published genome-wide association studies, targeted arrays and summary statistics 2019. Nucleic Acids Res. 2019;47(D1):D1005–D1012. doi:10.1093/nar/gky1120
6. Jeon Y, Jeon S, Choi W-H, et al. Genome-wide analyses of early-onset acute myocardial infarction identify 29 novel loci by whole genome sequencing. Hum Genet. 2023;142(2):231–243. doi:10.1007/s00439-022-02495-0
7. Aladag E, Tas Z, Ozdemir BS, et al. Human Ace D/I polymorphism could affect the clinicobiological course of COVID-19. J Renin Angiot Aldoster Sys. 2021;2021:5509280. doi:10.1155/2021/5509280
8. Fawzy MS, Toraih EA, Aly NM, et al. Atherosclerotic and thrombotic genetic and environmental determinants in Egyptian coronary artery disease patients: a pilot study. BMC Cardiovasc Disorders. 2017;17(1):26. doi:10.1186/s12872-016-0456-3
9. Dias‐Filho CAA, Soares NDJS, Bomfim MRQ, et al. The effect of family history of hypertension and polymorphism of the ACE gene (rs1799752) on cardiac autonomic modulation in adolescents. Clin Exp Pharmacol Physiol. 2021;48(2):177–185. doi:10.1111/1440-1681.13426
10. Rigat B, Hubert C, Alhenc-Gelas F, et al. An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. J Clin Investig. 1990;86(4):1343–1346. doi:10.1172/JCI114844
11. Zintzaras E, Raman G, Kitsios G, et al. Angiotensin-converting enzyme insertion/deletion gene polymorphic variant as a marker of coronary artery disease: a meta-analysis. Arch Int Med. 2008;168(10):1077–1089. doi:10.1001/archinte.168.10.1077
12. Borzyszkowska J, Stanislawska-Sachadyn A, Wirtwein M, et al. Angiotensin converting enzyme gene polymorphism is associated with severity of coronary artery disease in men with high total cholesterol levels. J Appl Genet. 2012;53(2):175–182. doi:10.1007/s13353-012-0083-3
13. Klashami ZN, Roudbordeh MG, Asadi M, et al. Association of ACE gene polymorphisms with in-stent restenosis by stent type (biomime, supraflex, xience). Mole Biol Rep. 2023;50(8):6445–6455. doi:10.1007/s11033-023-08554-7
14. Poorzand H, Fazeli B, Khajavi O, et al. Association of polymorphisms of renin angiotensin system and endothelial nitric oxide synthase genes with premature cardiovascular disease in an Iranian population. BMC Cardiovasc Disorders. 2023;23(1):254. doi:10.1186/s12872-023-03276-x
15. Masud R, Anjum A, Anwar M, et al. The risk stratification of coronary vascular disease as linked to homocysteine, its modulating genes, genetic polymorphisms, conventional predictors, and with antihypertensive medicaments. Chin J Physiol. 2021;64(6):298. doi:10.4103/cjp.cjp_71_21
16. Presta P, Bolignano D, Coppolino G, et al. Antecedent ACE-inhibition, inflammatory response, and cardiac surgery associated acute kidney injury. Rev Cardiovasc Med. 2021;22(1):207–213. doi:10.31083/j.rcm.2021.01.288
17. Dai S, Ding M, Liang N, et al. Associations of ACE I/D polymorphism with the levels of ACE, kallikrein, angiotensin II and interleukin-6 in STEMI patients. Sci Rep. 2019;9(1):19719. doi:10.1038/s41598-019-56263-8
18. Valença-pereira F, Fang Q, Marié IJ, et al. IL-6 enhances CD4 cell motility by sustaining mitochondrial Ca2+ through the noncanonical STAT3 pathway. Proc Natl Acad Sci USA. 2021;118(37):e2103444118. doi:10.1073/pnas.2103444118
19. Kumar V, Prabhu SD, Bansal SS. CD4+ T-lymphocytes exhibit biphasic kinetics post-myocardial infarction. Front Cardiovasc Med. 2022;9:992653. doi:10.3389/fcvm.2022.992653
20. Yang G, Tan Z, Zhou L, et al. Effects of Angiotensin II Receptor Blockers and ACE (Angiotensin-Converting Enzyme) inhibitors on virus infection, inflammatory status, and clinical outcomes in patients with COVID-19 and hypertension: a single-center retrospective study. Hypertension. 2020;76(1):51–58. doi:10.1161/HYPERTENSIONAHA.120.15143
21. Tutarel O, Meyer GP, Bertram H, et al. Safety and efficiency of chronic ACE inhibition in symptomatic heart failure patients with a systemic right ventricle. Int J Cardiol. 2012;154(1):14–16. doi:10.1016/j.ijcard.2010.08.068
22. Zhuang R, Meng Q, Ma X, et al. CD4+FoxP3+CD73+ regulatory T cell promotes cardiac healing post-myocardial infarction. Theranostics. 2022;12(6):2707–2721. doi:10.7150/thno.68437
23. Kumar V, Rosenzweig R, Asalla S, et al. TNFR1 contributes to activation-induced cell death of pathological CD4+ T lymphocytes during ischemic heart failure. JACC. 2022;7(10):1038–1049. doi:10.1016/j.jacbts.2022.05.005
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
