Back to Journals » Risk Management and Healthcare Policy » Volume 14
Accessing Healthcare Services for People with Physical Disabilities in Hawassa City Administration, Ethiopia: A Cross-Sectional Study
Authors Tesfaye T, Woldesemayat EM , Chea N , Wachamo D
Received 13 May 2021
Accepted for publication 9 September 2021
Published 24 September 2021 Volume 2021:14 Pages 3993—4002
DOI https://doi.org/10.2147/RMHP.S317849
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Tagel Tesfaye,1 Endrias Markos Woldesemayat,2 Nana Chea,2 Demelash Wachamo3
1Department of Public Health, Adare General Hospital, Hawassa, Sidama Regional State, Ethiopia; 2School of Public Health, College of Medicine and Health Sciences, Hawassa University, Hawassa, Sidama Regional State, Ethiopia; 3Department of Public Health, Hawassa College of Health Sciences, Hawassa, Sidama Regional State, Ethiopia
Correspondence: Demelash Wachamo
Department of Public Health, Hawassa College of Health Sciences, Hawassa, Sidama Regional State, Ethiopia
Tel +251 91 686 6654
Email [email protected]
Background: Persons with disabilities experience significant barriers to accessing health care. These barriers may be more serious in countries such as Ethiopia. In this study, we aimed to assess the prevalence of accessibility and associated factors among physically disabled people visiting physical disability associations in Hawassa.
Methods: A cross-sectional study was conducted among 345 randomly selected physically disabled people who visited disability associations in Hawassa. Data were collected from February 1 to 28, 2020 through face-to-face interview using a semi-structured questionnaire. Data analysis was done by SPSS version 23. Statistically significant test was declared using statistical cut-off point of P-value < 0.05.
Results: Accessibility to healthcare services among respondents was 83 (25.4%). About three-quarters of these respondents (74.6%) experienced at least one access barrier to healthcare services; 61.5% experienced physical barriers, 62.7% reported barriers related to medical equipment and 59.3% had communication barriers. Male participants (AOR = 3.19, 95% CI: 1.70, 6.99), married individuals (AOR = 2.95, 95% CI: 1.59, 5.49), people whose costs for healthcare services was covered by NGOs (AOR = 3.23, 95% CI: 1.39, 7.51) and participants with no experience of discrimination when accessing healthcare services (AOR = 5.84, 95% CI: 3, 11, 10.95) had more access to healthcare services.
Conclusion: Accessibility to healthcare services among people with disabilities was poor in the study. It is related with various factors. Therefore, it is important to strengthen inter-sectoral collaboration, promote community health insurance and strengthen the economic capacity of persons with physical disabilities in order to overcome barriers.
Keywords: physical disability, healthcare service, access, barriers
Background
The United Nations Convention on The Rights of Persons with Disabilities (UNCRPD) has precisely given a broad definition that encompasses all forms of disabilities. Physical accessibility is a condition of the physical environment that determines the use of services. It is how accessible physical structures such as hospital buildings, door entrances, toilets and scales are to Persons with Physical Disabilities (PWPD). It also includes the accessibility of roads to healthcare facilities, and sidewalks, corridors and parking spaces intended for PWPD within the healthcare facility.1 It can be affected by factors such as physical barriers, information and communication, financial barriers and attitude-related barriers.2 It can be affected by factors such as physical barriers, information and communication, financial barriers and attitude related barriers.2
The UNCRPD addresses areas such as physical, mental, intellectual or sensory impairments and the environmental factors which include negative attitudes, inaccessible transportation and inaccessible public buildings and limited social supports.3 PWPD remain at the margins of society and belong to the most impoverished groups.4 Negative imagery and language, stereotypes, and stigma with deep historic roots persist for people with disabilities around the world.4,5
Based on the World Report on Disability, over 1 billion people, or 15% of the world’s population, are living with some form of disability.4 Between 110 million (2.2%) and 190 million (3.8%) people aged 15 years and older have significant difficulties in functioning.6 However, rates of disability are increasing, due to population aging and the global increase in chronic health conditions.7
PWPD report seeking more health care than people without disability and have greater unmet needs.6,8 Today, only 1 in 10 people in need have access to assistive products. Affordability of health services and transportation are two main reasons why PWPD do not receive their required health care in low-income countries; 32–33% of people without disability are unable to afford health care compared with 51–53% of people with disability.9
The combination of high needs and low capacity to pay for health care is a major policy concern and a serious global challenge for providing available, accessible and affordable healthcare for PWPD.7,10 A study in India showed that PWPD had significantly less access to healthcare services than those without disability, and the barriers reported most often were lack of information, transport and physical inaccessibility.11 These problems are particularly common among PWPD in Africa and most developing countries, and widen the access gap between them and their counterparts in the developed world.10 A study in Ghana reported that inaccessible healthcare facilities and equipment, specifically absence of ramps and elevators, narrow corridors, absence of toilets and lack of sidewalks were among the biggest barriers to access healthcare services.12
The barriers to accessing healthcare services increase with age and severity of disability, and reduce with increasing level of education and with increasing number of members in the household.13 In addition to this are being single and unemployed, and lack of family support.14
In Ethiopia, a majority are facing a unique challenge to access basic social services and service providers may lack knowledge about disability issues, and misinformed or discriminatory attitudes of health workers can lead to impacts on access to healthcare services.15 As long as this disastrous situation is not addressed and inclusive strategies are not implemented, the global and national goals of poverty reduction and human rights will not be achieved.16 As a result, the need for empirical evidence on barriers to PWPD in accessing healthcare services becomes very important. Although disability as one socio-economic problem has received the attention of many scholars, information on the healthcare services accessibility barriers of PWPD is limited in Ethiopia. Moreover, although this issue has been investigated in the study area,16 this was not adequate for any decision making. This study therefore aimed to examine the prevalence of barriers and associated factors among physically disabled people in Hawassa city.
Methods
Study Setting and Study Population
This study was conducted in Hawassa city administration, in Sidama National Regional State which is located in the southern part of Ethiopia. Hawassa city is located at 275 km distance from Addis Ababa, Ethiopia. The city administration has 8 sub-cities with 20 urban and 12 rural kebeles. Due to lack of available information, it is difficult to obtain accurate figures on the prevalence of PWPD. Based on the 2013 CSA population projection report, the total number of PWPD in 2017 was 8088 (1.78% of the population).17
The source population of the study was all PWD residing in Hawassa city administration. While, all randomly selected individuals who are members of six physical disability associations in Hawassa city, namely: Ethiopian National Association of the Deaf (ENAD), Ethiopian National Association of Persons Affected by Leprosy (ENAPAL), Ethiopian National Association of the Blind (ENAB), Cheshire Service Ethiopia, “Salu Meredadat” PWPD Development and “Birhan Le Ethiopia” PWPD Association and available during the study period were considered as the study population. All randomly selected PWPD with age greater than 18 years old (adults) who were enrolled as members of the physical disability associations, could give informed consent and visited associations from February 1 to 28, 2020 were included in the study. Those individuals with intellectual/mental impairments, those with multiple disabilities and those PWPD who were not members of the physical disability associations were excluded from the study.
Variables
Access to healthcare service status was determined from the sum of variables such as availability of services, and individual and social related characteristics. Availability of services refers to resource allocation, financial incentives, the availability of transportation, suitable methods of service delivery, and favorable healthcare settings such as corridors and door entrances, toilet, ramps and elevators. Individual and social related characteristics are factors such as help-seeking behaviour, previous experiences, demand for formal care, social support. Organizational related factors include registration, opening times, waiting times, admission beds setting, information provision, costs of care, building design, and availability of different assistive devices such as stretchers and chairs for those with a disability. Regarding the sum of score of the questions to examine healthcare service accessibility which participants were expected to answer, participants who scored above the mean were categorized as “good access” and those who scored below the mean were categorized as “poor access”.18
Exposure variables include socio-demographic characteristics of the participants such as age, residence, gender, marital status, education status, occupational status, household monthly income. Physical barriers include infrastructure, transportation accessibility, distance, medical equipment and assisting devices. Financial barriers include income level, transportation cost, amount of healthcare service cost, insurance coverage. Communication and Information barriers include unavailability of visual signs, disability assistants, sign language interpreters and assistive devices in healthcare facility, knowledge on available services. Finally, other related barriers include type of disability, healthcare providers, perceived quality of care, discrimination, lack of compassion and respect (Figure S1).
Sample Size and Sampling Procedures
The sample size (n) was calculated using the following single population proportion formula and corrected for finite source population based on the following assumptions: (p) 50%, 95% Confidence interval (CI) (1.96), 5% margin of error (d), and adding 10% contingency.
 = (1.96)2(0.5) (0.5)/ 0.052) = 384, then corrected as by; Finite population correction formula, Therefore, nf=
= (1.96)2(0.5) (0.5)/ 0.052) = 384, then corrected as by; Finite population correction formula, Therefore, nf= = 384/ ((1+((383))/ 1712)) = 313.8 + 10% (31.38) =345 ≈ 345
= 384/ ((1+((383))/ 1712)) = 313.8 + 10% (31.38) =345 ≈ 345
Therefore, the required sample size was n = 345 included in the study.
The selection of the study participants was included in the sampling frame which prepared from registries of the associations that work with people with physical impairments in Hawassa city. The sample size was allocated proportionally to each association based on the number of PWPD registered on their institutions. Finally, 422 study participants were selected using a lottery method.
Data Collection Tools and Procedures
The data were collected through an interview by pre-tested and structured questionnaires. Socio-demographic characteristics and other determinants were assessed. The questionnaire was developed after a thorough literature review.2,19,20 The questionnaires were translated into the local language. The questionnaires were pretested and validated on 5% of the PWPD before two weeks in the study time at “Kuyera, Shashemene” outside the study area. Then some modifications on sequence and arrangement of the multiple answer questionnaire were done based on the findings. A total of six data collectors, nurses (including a sign language translator) and one supervisor were selected, trained and carried out the data collection process for 5 consecutive days. The data from participants with hearing impairment was obtained by a data collector who had knowledge and skill of sign language interpretation. Furthermore, the data collection process was supervised closely by the principal investigator and the supervisor to ensure information were properly collected and recorded.
Data Analysis
Data entry, cleaning, and analysis were done by SPSS V. 23. Descriptive analysis including frequency distribution and percentage was made to determine the access to healthcare service status, to describe socio-demographic and other determinants. Bivariate logistic regression analysis was conducted for crude odds ratio (COR) and all factors with a p-value < 0.25 were included in a multivariable logistic regression to control confounding effects. The Hosmer-Lemeshow goodness-of-fit statistic was used to assess whether the necessary assumptions for the application of multiple logistic regression are fulfilled. Adjusted odds ratios (AOR) with 95% confidence intervals (CI) were used to measure strength of the association between outcome variables and its determinant factors. Finally, p-value < 0.05 indicated a significant association.
Operational Definitions
Disability refers to difficulties encountered for persons with hearing, visual and mobility impairments in any or all three areas of functioning.
Person with physical disability was defined as a person with disability in vision, hearing and/or mobility.
Physical barriers: refers to the condition of the physical environment that determines the use of services and how accessible physical structures such as infrastructure, transportation, distance, medical equipment and assisting devices are to PWPD.
Healthcare access was defined as the opportunity to reach and obtain appropriate healthcare services in situations of perceived need for care. Access also described as: the possibility to identify healthcare needs, to seek healthcare services, to reach the healthcare resources, to obtain or use healthcare services, and to actually be offered services appropriate to the needs for care. Finally, we conceptualize five dimensions of accessibility of services as represented in the upper part of Figure S1: (1) Approachability; (2) Acceptability; (3) Availability and accommodation; (4) Affordability; (5) Appropriateness.18
The access to health service status was the sum of score of the questions to assess health access and participants who were able to score above the mean (3.5) out of 7 questions were categorized under “good access” and those who scored below the mean were categorized under “poor access”.
Communication and information barriers: are defined as anything that prevents PWPD from receiving and understanding the messages that health personnel use to convey their information at health facility.
Hearing impairment: is considered when a person faces a total inability to hear and may occur in one or both ears.
Reduced mobility: refers to the inability of a person to use one or more of his/her extremities, or a lack of strength to walk, grasp, or lift objects. The use of a wheelchair, crutches, or a walker may be utilized to aid in mobility.
Visual impairment: refers to a person with partial or total inability to see and may occur in one or both eyes.
Discrimination while accessing healthcare services: any act or practice inconsistent with the PWD, for example: facing discrimination in participation or consenting in their medical procedures, repeatedly asking about their disability, insulting or using culturally embarrassing words, calling by their disability, waiting for a long time to get service due to their disability.
Results
Socio-Demographic Characteristics
A total of 327 study participants were included, providing a response rate of 94.8%. The mean and standard deviation (±SD) age of PWPD was 30.5 (± 9.07) years, with 120 (36.7%) respondents being between 25 and 35 years of age. The majority, 230 (70.3%) of the study participants were urban dwellers. More than half, 186 (56.9%) of the respondents were men and 156 (47.7%) were married. Regarding the educational status of study participants, 86 (26.3%) had no formal schooling, 77 (23.5%) had primary schooling and 164 (50.2%) had secondary and higher education. Only 37 (11.3%) of the study participants were employed in government organizations, while 107 (32.7%) were employed in private companies. One hundred and sixty-four (50.2%) of respondents earned a monthly household income of 1051–3342 ETB. Regarding type of disability, out of 327 study participants, the proportion of persons with reduced mobility, visual and hearing impairments were 145 (44.3%), 112 (34.3%) and 70 (21.4%), respectively (Table 1).
 |
Table 1 Bivariable and Multivariable Logistic Regression Analysis to Access Healthcare Service by Persons with Physical Disability, Hawassa City, Southern Ethiopia, June 2020 |
Respondent’s Experience and Perceptions of Healthcare Service Visit
Almost all 326 (99.7%) of the respondents visited healthcare services in the last 12 months. Of these, 243 (74.3%) respondents visited healthcare facilities mainly to seek treatment, 46 (14.1%) visited for regular check-ups and 36 (11.0%) visited for laboratory tests. The majority of respondents, 247 (75.5%) had visited public hospitals or health centers. Concerning the regular source of funding for respondents to cover healthcare costs, 145 (44.3%) were covered by community health insurance (CBHI), 112 (34.3%) out of pocket expenses and 70 (21.4%) by NGOs (Table S1).
Healthcare Service Access and Its Barriers
The overall level of access to the healthcare services among PWPD clients was 83 (25.4%) [95% CI: 20.9–30.3]. Regarding the barriers that respondents faced when they accessed healthcare facilities, 244 (74.6%) participants reported at least one access barrier to healthcare services, 201 (61.5%) had physical barriers, 205 (62.7%), had barriers related to medical equipment and 194 (59.3%) had communication barriers (Figure 1). Regarding the physical barriers, 73 (46.5%) study participants with reduced mobility and 72 (45.9%) with visual impairment reported that poor road network and absence of disability friendly public transport were the two main challenges to reach healthcare facilities. In addition, 61 (44.2%) and 64 (46.4%) respectively, reported they faced narrow corridors and door entrances during their previous visit of healthcare services. Regarding barriers related to medical equipment, 62 (56.9%) and 51 (72.9%) experienced uncomfortable patient admission beds and uncomfortable stretchers and chairs, respectively, among those with reduced mobility. Regarding the communication barriers; 40 (76.9%) and 41 (75.9%) persons with hearing impairment reported these, more than other disability groups (Table 2).
 |
Table 2 The Major Barriers to the Accessibility of Healthcare Services for Persons with Physical Disability in Hawassa City, Southern Ethiopia, June 2020 |
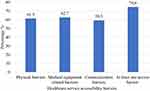 |
Figure 1 Types of barriers to access healthcare services by persons with physical disability in Hawassa city, Southern Ethiopia in June, 2020 (n=327). |
Experience of Discrimination
The majority of the respondents, 198 (60.6%) reported experience of discrimination from health service providers. Of these, 63 (31.2%) reported being discriminated against by nurses, 54 (26.7%) faced discrimination by pharmacy professionals and 43 (21.3%) faced discrimination by laboratory professionals. Regarding the respondents’ perception of the reasons for discrimination, 193 (95.5%) considered that their disability was the only cause of discrimination by healthcare providers. Among these, 99 (49.0%) respondents experienced delay in the process of health service delivery. In addition, a total of 225 (68.8%) respondents reported that healthcare providers had not allocated enough time to meet their healthcare needs during the treatment process. Moreover, 211 (64.5%) of the respondents indicated that their ideas were not fully understood by healthcare providers (Table S2).
Factors Associated with Access to Healthcare Services
In the bivariable logistic regression model, the analysis factors that had an association with access to healthcare services were residence, sex, age, marital status, education level, monthly household income, source of coverage for health costs and discrimination in accessing health services. In the multivariate logistic regression analysis model,males [AOR = 3.19, 95% CI: 1.70, 6.99] were approximately three times more privileged to access healthcare services compared with females. In addition, married PWPD [AOR = 2.95, 95% CI: 1.59, 5.49], participants in the study whose health costs were covered by NGOs [AOR = 3.23, 95% CI: 1.39, 7.51] and those with no experience of discrimination in accessing health services [AOR = 5.84, 95% CI: 3.11, 10.95] had more access to healthcare services than their counterparts (Table 1).
Discussions
The findings of this study showed that a low proportion of PWPD access healthcare facilities. A high proportion of the study participants experienced discrimination from healthcare service providers. Moreover, accessing healthcare services by PWPD was associated with being male, being married, having healthcare costs covered by NGOs and PWPD with no experience of discrimination in accessing health services were considered to have association with good access to healthcare service compared with their counterparts.
In this study, only 25.4% of PWPD had good access to healthcare services, while 74.6% had poor access to healthcare services. This finding is higher than a study report in which 65.6% reported at least one access barrier to healthcare in Ghana.1 The finding in the current study was higher compared with study reports from Brazil (37.3%),21 and South Africa22 indicated that 11% of adult PWPD had experienced several challenges in accessing healthcare services. This difference also could be associated with technological advancement and economic ability to afford access to assistive products between study participants. This implies that PWPD in developing countries like Ethiopia, particularly in our study area, are confronting a huge difficulty in accessing healthcare services.
In this study 74.6% of PWPD had faced at least one access barrier to healthcare services, a large proportion of them (61.5%) had experienced physical barriers to access healthcare facilities and 62.7% had experienced barriers related to medical equipment. This finding was higher than a study in Syria and Lebanon in which only 19% of respondents reported physical barriers to access healthcare services faced by PWPD23 and 37.3% of the patients reported inadequate physical access infrastructure (including doors, hallways, waiting rooms, and offices) in Fortaleza, Ceara, Brazil.21 The difference might be due to the economic conditions of these countries, which allow them to develop healthcare infrastructure and medical equipment comfortable to PWPD. The main physical barriers of the finding were absence of elevators or ramps, uncomfortable toilets and transportation difficulties. This indicated that construction companies failed to address disability issues intheir construction designs and institutions who are responsible to improve the rights of PWPD are not fulfilling the UNCRPD conventions and the GTP.24 It is suggested that, the government needs to revisit existing building regulations to re-design buildings to ensure disability friendly infrastructure.
The study revealed that 59.3% of PWPD faced barriers that made it difficult to communicate with healthcare providers during their visit in health facilities. This was consistent with 56.2% in Fortaleza, Ceara, Brazil.21 This may be because most persons with hearing impairment could not effectively communicate with healthcare providers by using verbal language. It is suggested that healthcare providers have training in some basic sign language or employ those who can translate sign language. In addition to this it is better to develop strategies like translator software of signs at health facilities.
The study participants who had no experience of discrimination in accessing health services had high odds to access health service compared with their counterparts. They claim mainly discrimination in participation or consenting in their medical procedures, ignorance about their disability, being insulted or using embarrassing cultural words, calling by their disability, waiting for a long time to get service due to their disability. Our finding was in line with the report on discrimination, social exclusion, isolation and barriers to accessing healthcare services in Mpumalanga Province of South Africa.25 This may be partly due to the perceived beliefs of PWPD towards their own disability or maybe failure of healthcare providers to effectively communicate with their clients. This may due to the norms of the local community dictating the access for health care that PWPD have, in that most of PWPD do not want to show their disability to the community to get help and they afraid to are ask and not be discriminated due to their disability. They cannot dare to ask or know they have equal rights, and due to different challenges like transportation, location, communication and assisting devices, the social support still lacking. Providing capacity building training on Compassionate, Respectful and Caring (CRC) for healthcare providers and assigning trained disability assistants in healthcare facilities are suggested to minimize discrimination.
In this study findings revealed that being male, being married and having healthcare costs covered by NGOs allowed more privilege in accessing healthcare services compared with their counterparts. This finding was consistent with a study in Iran,26 Tanzania27 and Ghana.1 This might be because married PWPD had better chances from their partners including being accompanied by them during their visit to healthcare facilities, and financial and emotional support. This suggests the need to strengthening institutions responsible for improving the rights of women. In addition to this, strengthening CBHI, enhancing the purchasing capacity of PWPD through capacity building and providing disability grants are important strategies in order to address these barriers.
This study has implications to target better health access and health-seeking behaviour among persons with disabilities who experience significant barriers to accessing health care. These barriers can be particularly severe for developing countries such as Ethiopia, and includephysically inaccessible medical clinics and hospitals, lack of appropriate transport to enable PWPD to seek medical care or rehabilitation services; lack of or poor communication and accommodation in healthcare settings, untrained personnel and inadequate staffing, negative attitudes of healthcare providers, particularly in relation to denial of treatment on grounds of disability.
This study had some potential limitations that might have led to information bias on the part of the respondents. Although we collect on 1-year data health service utilization to minimize the recall bias, it is still possible to have some recall bias. The study was limited to members of PWPD associations, and does not consider the children. Furthermore, the chicken-egg dilemma may be considered as the main limitation. The study may not establish a causal relationship as we have implemented a cross-sectional study design.
Conclusions
In this study, we found a high proportion of the study participants had inadequate access to healthcare services. Physical barriers, medical equipment’s related barriers, communication and discrimination barriers were the most important challenges. Mainly reported as a reason for inaccessibility, physical barriers include difficulty of getting transportation due to poor road network, inaccessible door entrances, absence of elevators, ramps and toilets. Being male, being married, having healthcare costs covered by NGOs and having no experience of discrimination in accessing healthcare services had significant association to having good access to healthcare services. Hence, it is important to strengthen intersectoral collaboration, promote community health insurance and strengthen the economic capacity of persons, considering the PWPD during the construction of the health facilities, setting different furniture for those with physical disabilities in order to overcome the barriers.
Abbreviations
AOR, adjusted odds ratio; COR, crude odds ratio; CBHI, Community Based Health Insurance; CRC, Compassionate, Caring and Respectful; ETB, Ethiopian Birr; FDRE, Federal Democratic Republic of Ethiopia; PWPD, Persons with Physical Disability; SPSS, Statistical Package for Social Science; UNCRPD, The United Nations Convention on the Rights of Persons with Disabilities; WHO, World Health Organization.
Data Sharing Statement
The datasets used in this study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from Hawassa University College of Medicine and Health sciences and conducted in accordance with the Declaration of Helsinki and was approved by an institutional review board or ethics committee. Support letter was obtained from the Hawassa city health department. All participants were informed about the purpose, risks, benefit and confidentiality issues related to the study. Participation was on a voluntary basis and written informed consent (verbal consent for who cannot read and write) was obtained from each participant. No one other than investigators had access to data.
Acknowledgments
The authors would like to thank Hawassa University for providing funds for the study. The authors are grateful to all data collectors and study participants for their valuable contributions.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Hawassa University provided fund for the study. The funder had no role in designing the study and conducting the analysis.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Badu E, Agyei-Baffour P, Opoku MP. Access barriers to health care among people with disabilities in the Kumasi Metropolis of Ghana. Can J Disabil Stud. 2016;5(2):131–151. doi:10.15353/cjds.v5i2.275
2. Visagie S, Eide AH, Dyrstad K, et al. Factors related to environmental barriers experienced by persons with and without disabilities in diverse African settings. PLoS One. 2017;12(10):e0186342. doi:10.1371/journal.pone.0186342
3. United Nations. United Nations Convention on the Rights of Persons with Disabilities (UNCRPD); 2006. Available from: http://www.un.org/disabilities/convention.
4. World Health Organization, Regional Office for South-East Asia and World Bank. World Report on Disability 2011. Geneva: World Health Organization; 2011.
5. Tuakli-Wosornu YA, Haig AJ. Implementing the World Report on Disability in West Africa: challenges and opportunities for Ghana. Am J Phys Med Rehabil. 2014;93(1 Suppl 1):S50–S57. doi:10.1097/PHM.0000000000000023
6. World Health Organization, Regional Office for South-East Asia. WHO Global Disability Action Plan 2014–2021: Better Health for All People with Disability. World Health Organization; 2015.
7. World Health Organization. Regional Office for the Western, P. Health Care Utilization of Persons with Disabilities in Cambodia: Based on the Cambodia Demographic and Health Survey 2014. Manila: WHO Regional Office for the Western Pacific; 2017.
8. World Health Organization. Disability and Health: Key Facts. World Health Organization; 2018.
9. Heaslip V. Health and disability in adults: definitions and models. In: Human Growth and Development in Adults: Theoretical and Practice Perspectives. Policy Press; 2020:179.
10. Mitra S, Posarac A, Vick B. Disability and poverty in developing countries: a multidimensional study. World Dev. 2013;41:1–18. doi:10.1016/j.worlddev.2012.05.024
11. Gudlavalleti MVS, John N, Allagh K, et al. Access to health care and employment status of people with disabilities in South India, the SIDE (South India Disability Evidence) study. BMC Public Health. 2014;14(1):1125. doi:10.1186/1471-2458-14-1125
12. Ganle JK, Otupiri E, Obeng B, et al. Challenges women with disability face in accessing and using maternal healthcare services in Ghana: a qualitative study. PLoS One. 2016;11(6):e0158361. doi:10.1371/journal.pone.0158361
13. Vergunst R, Swartz L, Hem K-G, et al. Access to health care for persons with disabilities in rural South Africa. BMC Health Serv Res. 2017;17(1):741. doi:10.1186/s12913-017-2674-5
14. Moses AL. Factors Influencing Access to Healthcare Service Delivery in West Pokot County, Kenya. University of Nairobi; 2017.
15. ILO/International Labour Organisation. Inclusion of People with Disabilities in Ethiopia: Fact Sheet. ILO/Irish Aid Partnership Programme. ILO/International Labour Organisation; 2013.
16. Alemu Y. Impact of Rehabilitation Centre on the Psycho-Social Condition of Children with Physical Impairment. Addis Ababa University; 2014.
17. Hawassa City Administrative Health Department. Health Sector Growth and Transformation Plan (GTP II), 2012 E.C. 2019, A.M. Hawassa, Ethiopia: Printing Press; 2019.
18. Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12(1):18. doi:10.1186/1475-9276-12-18
19. Wright A, Roberts R, Bowman G, et al. Barriers and facilitators to physical activity participation for children with physical disability: comparing and contrasting the views of children, young people, and their clinicians. Disabil Rehabil. 2019;41(13):1499–1507. doi:10.1080/09638288.2018.1432702
20. Alkawai FM, Alowayyed AS. Barriers in accessing care services for physically disabled in a hospital setting in Riyadh, Saudi Arabia, cross-sectional study. J Commun Hosp Intern Med Perspect. 2017;7(2):82–86. doi:10.1080/20009666.2017.1324237
21. Rocha LL, de Lima Saintrain MV, Vieira-Meyer AP. Access to dental public services by disabled persons. BMC Oral Health. 2015;15:35. doi:10.1186/s12903-015-0022-x
22. Mutwali R, Ross E. Disparities in physical access and healthcare utilization among adults with and without disabilities in South Africa. Disabil Health J. 2019;12(1):35–42. doi:10.1016/j.dhjo.2018.07.009
23. Baroud M, Mouheildine O. Healthcare needs and barriers of persons with disabilities: an exploratory study among Syrian refugees, Palestine Refugees from Syria, and Lebanese. In: Issam Fares Institute for Public Policy and International Affairs. Mazraa, Beirut, Lebanon: American University of Beirut; 2018:46.
24. Tadele F. Towards a More Inclusive Economic Growth and Social Development in Ethiopia: the State of Vulnerable Social Groups and Social Protection.
25. Neille J, Penn C. Beyond physical access: a qualitative analysis into the barriers to policy implementation and service provision experienced by persons with disabilities living in a rural context. Rural Remote Health. 2015;15(3):3332.
26. Matin BK, Kamali M, Williamson HJ, Moradi F, Solatni S. The predictors of access to health services for people with disabilities: a cross sectional study in Iranian context. Med J Islam Repub Iran. 2019;33:125.
27. Mshana G, Dotchin CL, Walker RW. ‘We call it the shaking illness’: perceptions and experiences of Parkinson’s disease in rural northern Tanzania. BMC Public Health. 2011;11:219. doi:10.1186/1471-2458-11-219
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
