Back to Journals » International Medical Case Reports Journal » Volume 15
Ab Interno Goniotomy with the Kahook Dual Blade in a Monocular Patient with Mucous Membrane Pemphigoid and Refractory Open Angle Glaucoma: A Case Report
Authors Kounatidou NE, Filippopoulos T, Palioura S
Received 18 July 2022
Accepted for publication 29 September 2022
Published 11 October 2022 Volume 2022:15 Pages 563—568
DOI https://doi.org/10.2147/IMCRJ.S382810
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Nefeli Eleni Kounatidou,1 Theodoros Filippopoulos,2 Sotiria Palioura3
1National and Kapodistrian University of Athens Medical School, Athens, Greece; 2Glaucoma Division, Athens Vision Eye Institute, Athens, Greece; 3Department of Ophthalmology, University of Cyprus Medical School, Nicosia, Cyprus
Correspondence: Sotiria Palioura, 7 Lampsa Str, Athens, 11524, Greece, Tel +30 698 580 2355, Email [email protected]
Purpose: To describe the case of a monocular patient with ocular mucous membrane pemphigoid (MMP) and open angle glaucoma refractory to medical treatment, who was successfully managed with ab interno goniotomy at the time of cataract surgery.
Methods: A 63-year-old woman with a history of severe MMP presented with exacerbation of the disease in both eyes. Vision was 20/80 in the right eye and light perception in the left eye. Symblepharon formation, trichiasis and forniceal foreshortening were present in the right eye, while the cornea of the left eye was completely conjunctivalized. Following aggressive systemic immunosuppressive therapy with corticosteroids and cyclophosphamide, the disease was brought under control. However, the patient developed a mature cataract and high intraocular pressure (IOP) of 28 mmHg on maximal medical therapy. Due to the high risk of ocular MMP exacerbation with glaucoma filtration surgery, the decision was made to proceed with cataract extraction combined with ab interno goniotomy with the Kahook Dual Blade.
Results: There were no intraoperative complications. The IOP has remained in the 12– 14 mmHg range without any topical glaucoma medications over a total follow up of 3.5 years.
Conclusion: Ab interno goniotomy using the Kahook Dual Blade can significantly reduce IOP and medication burden in MMP cases, where any type of conjunctival incisional surgery could induce disease flare up. In this case, it represented a safe and effective surgical procedure for ocular MMP with concomitant refractory open angle glaucoma.
Keywords: ocular cicatricial pemphigoid, MIGS, KDB goniotomy, phaco-KDB, ab interno goniotomy
Introduction
Ocular mucous membrane pemphigoid (MMP) presents as a bilateral relapsing-remitting cicatrizing conjunctivitis with conjunctival hyperemia, as well as with symblepharon and ankyloblepharon formation as the disease progresses.1 Cataract and glaucoma often coexist in patients with ocular MMP.2 Secondary open angle glaucoma occurs as a side-effect of corticosteroid therapy or because of the disease itself,2 given that scleral and episcleral scarring results in impaired aqueous outflow and increased intraocular pressure (IOP).3
Clear cornea phacoemulsification has been reported safe and effective in ocular MMP,4 but the management of glaucoma remains challenging. Anti-glaucomatous therapy is often ineffective, due to conjunctival foreshortening and epiphora, which limits the efficacy of topical drops. At the same time, eye drops, and glaucoma filtering surgeries can trigger MMP progression, by compromising the conjunctival basement membrane and by traumatizing the conjunctiva, respectively.5,6 Moreover, filtering surgeries, such as trabeculectomy and insertion of glaucoma drainage devices, are subject to increased rates of failure due to post-operative inflammation and conjunctival scarring.
Minimally invasive glaucoma surgery (MIGS) procedures offer a conjunctival-sparing alternative, thus minimizing the risk of ocular MMP exacerbation. Ab interno excisional goniotomy with the Kahook Dual Blade (KDB, New World Medical Inc., Rancho Cucamonga, CA, USA) is a MIGS procedure, that targets the trabecular meshwork, which is the main site of aqueous outflow resistance.7 It has been effective in mild to moderate primary open-angle glaucoma (POAG),8–10 uncontrolled glaucoma,11 angle closure12 and secondary glaucoma,13 and can be performed as a stand-alone procedure7,9,10,14,15 or in combination with cataract surgery.7,8,12,15–18
The purpose of this report is to present the case of a monocular patient with ocular MMP and open angle glaucoma refractory to medical treatment, that was managed successfully with ab interno KDB goniotomy at the time of cataract surgery.
Materials and Methods
A 63-year-old woman was referred to the Athens Vision Eye Institute Cornea Clinic for management of severe mucous membrane pemphigoid in both eyes. Medical history was significant for diabetes mellitus and a positive skin biopsy for pemphigoid 1.5 years prior to presentation. The patient was being managed with methylprednisolone 16 mg per os once a day. Over the 6 months prior to presentation, significant redness developed in both eyes along with a persistent epithelial defect in the left eye.
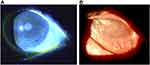
Upon examination of the right eye, best-corrected visual acuity was 20/80 and IOP was 20 mmHg by Goldmann applanation tonometry. For the left eye, best-corrected visual acuity was light perception and IOP readings were unreliable. Slit lamp examination was significant for entropion and trichiasis, extensive symblepharon formation and forniceal foreshortening in both eyes as well as ankyloblepharon in the left eye. Severe conjunctival injection and ocular surface dryness was present in both eyes (Figure 1A), while the cornea of the left eye was completely conjunctivalized (Figure 1B).
A cataract (2+ nuclear sclerosis) was also seen in the right eye. Dilated fundus examination of the right eye revealed macular drusen and cupping of the right optic nerve with a cup to disc ratio of 0.5. We were unable to obtain reliable results on static automated perimetry despite several attempts. The conjunctivalized surface of the left eye impeded examination of the fundus and, for this reason, a B-scan ultrasound was performed, which did not reveal any abnormalities.
Given the severe ocular surface inflammation and the monocular status of the patient, aggressive treatment was initiated to preserve vision in the right eye. Monthly intravenous cyclophosphamide (25 mg/kg) infusions were administered for 6 months along with a slow oral steroid taper and topical preservative-free dexamethasone drops. The patient was subsequently transitioned to oral mycophenolate mofetil 2 g daily. At the 8 month follow up visit the ocular surface was white and quiet (Figure 2A) but the cataract had matured significantly with a nuclear sclerotic and a posterior subcapsular component (Figure 2B). Vision in the right eye had dropped to 20/200 and IOP had increased to 35 mmHg. Despite cessation of oral and topical steroids and maximum medical therapy with oral acetazolamide 250 mg 3 times daily, topical preservative-free dorzolamide/timolol, brimonidine and latanoprost eye drops, IOP remained high at 28 mmHg.
Decision was made to proceed with clear cornea cataract surgery combined with ab interno goniotomy using the Kahook Dual Blade (phaco-KDB) in the patient’s right eye. Because of the significant forniceal foreshortening and the ankyloblepharon a pediatric lid speculum was used during the procedure and an assistant was manually retracting the patient’s lower lid as needed during otherwise standard clear cornea phacoemulsification via a 2.6 mm main incision. Following insertion of a single piece intraocular lens (Acrysoft IQ SN60WF 24.0 D, Alcon Laboratories, Fort Worth, TX, USA) and before removal of the cohesive viscoelastic the head of the patient and the head of the operating microscope were rotated, a Swan Jacob direct goniolens was applied on the cornea and 3–4 clock hours of pigmented trabecular meshwork were removed with the Kahook dual blade. Reflux of blood from collector channels into the anterior chamber was observed and the majority of the viscoelastic was removed with the irrigation aspiration handpiece. Postoperatively the patient was started on preservative-free topical dexamethasone eye drops, topical moxifloxacin and nepafenac.
Results
On the first post-operative day, the IOP was 14 mmHg and there was no layering hyphema in the anterior chamber (Figure 3). The patient’s corneal surface appeared very dry and within a few days a corneal epithelial defect developed, which was managed with a bandage contact lens and use of serum tears 30% and resolved by the 6th post-operative week. Intraocular pressure was 12 mmHg at 3 months post-operatively without any topical glaucoma medications and has remained in the 12–14 mm Hg range over a total follow up of 3.5 years. The patient’s visual acuity in the right eye at the last follow up visit was 20/40.
Discussion
In ocular MMP, the incidence of cataract-induced vision loss and glaucoma has been reported at 40% and 30%, respectively.2 In the case of our patient, the aggressive systemic immunosuppressive therapy, initiated to preserve vision in the right eye, resulted in significant cataract progression and IOP elevation, which remained high at 28 mmHg despite maximum tolerated medical therapy.
Although cataract surgery has an inherent IOP lowering effect, this is not sufficient in cases of uncontrolled glaucoma.19 Additionally, glaucoma patients undergoing cataract surgery show an increased incidence of post-operative IOP spikes with IOP >30 mmHg, which poses a significant risk in eyes with pre-existing glaucoma.20–22 However, IOP spikes are reduced when cataract surgery is combined with a MIGS procedure.23–25 For this reason, we decided to perform a combined procedure and more specifically an ab interno KDB goniotomy at the time of phacoemulsification (phaco-KDB).
Phaco-KDB results in an average IOP reduction of 12–32.1% with pressures in the mid-teens along with glaucoma medication requirements reduction of 21–89.1% over a follow-up period of 6–24 months.7,8,15–18,26–28 This IOP lowering effect is associated with the pre-operative IOP level.8,9 However, most trabecular by-passing or ablating procedures cannot achieve an IOP at the level of episcleral venous pressure as they do not address all sources of resistance to aqueous outflow.
In our case, the patient’s IOP decreased from 28 mmHg preoperatively to 14 mmHg after phaco-KDB and remained in the 12–14 mmHg range over the course of 3.5 years with elimination of essentially 4 classes of medications. This drop in IOP may appear impressive, but it needs to be acknowledged, that due to conjunctival foreshortening the eyedrops may not have remained in the conjunctival cul-de-sac long enough to be effective.
Our decision to proceed with phaco-KDB, instead of another MIGS procedure, was related to the unavailability in Greece of the Hydrus Microstent (Ivantis, Inc, Irvine, CA, USA), the lower cost of the KDB over the Trabectome (NeoMedix Corporation, Tustin, CA) and the i-Stent (Glaukos, Laguna Hills, CA), and KDB’s apparent superior efficacy to the i-Stent when combined with cataract surgery.7,15,16,26 We also decided to stay away from gonioscopy assisted transluminal trabeculotomy (GATT) out of fear of a significant hyphema that would delay visual rehabilitation.29 Nevertheless, randomized clinical trials comparing different types of MIGS are scarce25 and data are mainly derived from retrospective studies.17
Conclusions
To our knowledge this is the first reported case of phaco-KDB in a patient with cicatrizing ocular MMP. This combined phaco-MIGS procedure resulted in significant IOP and medication burden reduction without any intraoperative complications. This case may provide some insight into a viable treatment option for patients with cicatrizing ocular surface disorders, where traditional filtration surgeries are contraindicated due to the risk of inducing disease exacerbation and are likely to fail in the long term due to proliferation of subconjunctival fibrous tissue.
Abbreviations
MMP, Mucous membrane pemphigoid; IOP, Intraocular pressure; KDB, Kahook Dual Blade; MIGS, Minimally invasive glaucoma surgery; POAG, primary open-angle glaucoma; phaco-KDB, Cataract surgery combined with ab interno goniotomy using the Kahook Dual Blade; GATT, Gonioscopy assisted transluminal trabeculotomy.
Availability of Materials and Data
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Ethics Statement
Institutional approval was not required for the publication of this case.
Consent for Publication
Informed written consent was obtained from the patient for publication of this case report and accompanying images.
Acknowledgments
This paper was presented at the 40th Congress of the European Society of Cataract and Refractive Surgery as an abstract presentation with interim findings.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding or grant support.
Disclosure
Dr. Palioura is a consultant for Alcon. The authors declare no other conflict of interest related to this work.
References
1. Schmidt E, Zillikens D. Pemphigoid diseases. Lancet. 2013;381(9863):320–332. doi:10.1016/S0140-6736(12)61140-4
2. Miserocchi E, Baltatzis S, Roque MR, Ahmed AR, Foster CS. The effect of treatment and its related side effects in patients with severe ocular cicatricial pemphigoid. Ophthalmology. 2002;109(1):111–118.
3. Tsai JH, Derby E, Holland EJ, et al. Incidence and prevalence of glaucoma in severe ocular surface disease. Cornea. 2006;25:530–532. doi:10.1097/01.ico.0000220776.93852.d9
4. Sangwan VS, Gupta S, Das S. Cataract surgery in ocular surface diseases: clinical challenges and outcomes. Curr Opin Ophthalmol. 2018;29(1):81–87.
5. Noecker RJ, Herrygers LA, Corneal AR. Conjunctival changes caused by commonly used glaucoma medications. Cornea. 2004;23:490–496.
6. Feizi S, Ocular Manifestations RD. Management of autoimmune bullous diseases. J Ophthalmic Vis Res. 2019;14(2):195–210. doi:10.4103/jovr.jovr_86_18
7. Sieck EG, Epstein RS, Kennedy JB, et al. Outcomes of kahook dual blade goniotomy with and without phacoemulsification cataract extraction. Ophthalmol Glaucoma. 2018;1(1):75–81. doi:10.1016/j.ogla.2018.06.006
8. Dorairaj SK, Seibold LK, Radcliffe NM, et al. 12-month outcomes of goniotomy performed using the kahook dual blade combined with cataract surgery in eyes with medically treated glaucoma. Adv Ther. 2018. doi:10.6084/m9.figshare.6756638
9. Berdahl JP, Gallardo MJ, ElMallah MK, et al. Six-month outcomes of goniotomy performed with the kahook dual blade as a stand-alone glaucoma procedure. Adv Ther. 2018:2093–2102. doi:10.6084/m9.figshare.7145831
10. Salinas L, Chaudhary A, Berdahl JP, et al. Goniotomy using the kahook dual blade in severe and refractory glaucoma: 6-month outcomes. J Glaucoma. 2018;27(10):849–855. doi:10.1097/IJG.0000000000001019
11. ElMallah MK, Berdahl JP, Williamson BK, et al. Twelve-month outcomes of stand-alone excisional goniotomy in mild to severe glaucoma. Clin Ophthalmol. 2020;14:1891–1897. doi:10.2147/OPTH.S256423
12. Dorairaj S, Tam MD, Balasubramani GK. Twelve-month outcomes of excisional goniotomy using the kahook dual blade in eyes with angleclosure glaucoma. Clin Ophthalmol. 2019;13:1779–1785. doi:10.2147/OPTH.S221299
13. Miller VJ, Young CEC, Soohoo JR, et al. Efficacy of goniotomy with kahook dual blade in patients with uveitis-associated ocular hypertension. J Glaucoma. 2019;28(8):744–748. doi:10.1097/IJG.0000000000001298
14. Seibold LK, Soohoo JR, Ammar DA, Kahook MY. Preclinical investigation of ab interno trabeculectomy using a novel dual-blade device. Am J Ophthalmology. 2013;155(3):524–529.e2. doi:10.1016/j.ajo.2012.09.023
15. Arnljots TS, Economou MA. Kahook dual blade goniotomy vs istent inject: long-term results in patients with open-angle glaucoma. Clin Ophthalmol. 2021;15:541–550. doi:10.2147/OPTH.S284687
16. Dorairaj SK, Kahook MY, Williamson BK, Seibold LK, Elmallah MK, Singh IP. A multicenter retrospective comparison of goniotomy versus trabecular bypass device implantation in glaucoma patients undergoing cataract extraction. Clin Ophthalmol. 2018;12:791–797. doi:10.2147/OPTH.S158403
17. Ventura-Abreu N, García-Feijoo J, Pazos M, Biarnés M, Morales-Fernández L, Martínez-de-la-Casa JM. Twelve-month results of ab interno trabeculectomy with Kahook Dual Blade: an interventional, randomized, controlled clinical study. Graefes Arch Clin Exper Ophthalmol. 2021;259(9):2771–2781. doi:10.1007/s00417-021-05213-0
18. Al Habash A, Nagshbandi AA. Quality of life after combined cataract and minimally invasive glaucoma surgery in glaucoma patients. Clin Ophthalmol. 2020;14:3049–3056. doi:10.2147/OPTH.S276124
19. Iancu R, Corbu C. Intraocular pressure after phacoemulsification in patients with uncontrolled primary open angle glaucoma. J Med Life. 2014;7(1):11–16.
20. Shingleton BJ, Rosenberg RB, Teixeira R, et al. Evaluation of intraocular pressure in the immediate postoperative period after phacoemulsification. J Cataract Refract Surg. 2007;33(11):1953–1957.
21. Shingleton BJ, Laul A, Nagao K, et al. Effect of phacoemulsification on intraocular pressure in eyes with pseudoexfoliation. Single-surgeon series. J Cataract Refract Surg. 2008;34(11):1834–1841.
22. Kim JY, Jo MW, Brauner SC, et al. Increased intraocular pressure on the first postoperative day following resident-performed cataract surgery. Eye. 2011;25(7):929–936.
23. Zebardast N, Zheng C, Jampel HD. Effect of a Schlemm’s canal microstent on early postoperative intraocular pressure after cataract surgery: an analysis of the HORIZON randomized controlled trial. Ophthalmology. 2020;127:1303–1310.
24. Weiner Y, Severson ML, Weiner A. Intraocular pressure 3 to 4 hours and 20 hours after cataract surgery with and without ab interno trabeculectomy. J Cataract Refract Surg. 2015;41(10):2081–2091.
25. Ahmed IIK, Fea A, Au L, et al. A prospective randomized trial comparing Hydrus and iStent microinvasive glaucoma surgery implants for standalone treatment of open-angle glaucoma: the COMPARE study. Ophthalmology. 2020;127(1):52–61.
26. ElMallah MK, Seibold LK, Kahook MY, et al. 12-month retrospective comparison of Kahook dual blade excisional goniotomy with I-stent trabecular bypass device implantation in glaucomatous eyes at the time of cataract surgery. Adv Ther. 2019;2019:2515–2527.
27. Al Habash A, Albuainain A. Long term outcome of combined phacoemulsification and excisional goniotomy with the Kahook Dual Blade in different subtypes of glaucoma. Sci Rep. 2021;11(1):10660. doi:10.1038/s41598-021-90223-5
28. Chihara E, Chihara T. Turn back elevation of once reduced IOP after trabeculotomy ab externo and Kahook Dual Blade surgeries combined with cataract surgery. Clin Ophthalmol. 2020;14:4359–4368. doi:10.2147/OPTH.S287090
29. Qiao Y, Tan C, Chen X, et al. Gonioscopy-assisted transluminal trabeculotomy versus goniotomy with Kahook dual blade in patients with uncontrolled juvenile open-angle glaucoma: a retrospective study. BMC Ophthalmol. 2021;21(1):1.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.