Back to Journals » International Medical Case Reports Journal » Volume 17
A Young Woman with Fulminant Myocarditis with Cardiogenic Shock – Management with Assist Devices: A Case Report
Authors Hu F , Luo B, Yuan X, Zhang L, Chen L
Received 15 October 2023
Accepted for publication 5 December 2023
Published 7 February 2024 Volume 2024:17 Pages 93—100
DOI https://doi.org/10.2147/IMCRJ.S440590
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Feng Hu,1– 3,* Ben Luo,1,* Xun Yuan,1– 3 Linlin Zhang,1– 3 Lianglong Chen1– 3
1Department of Cardiology, Provincial Institute of Coronary Disease, Fujian Medical University Union Hospital, Fuzhou, Fujian, 350001, People’s Republic of China; 2Department of Cardiology, Heart Center of Fujian Medical University, Fuzhou, Fujian, 350001, People’s Republic of China; 3Department of Cardiology, Cardiovascular Medicine Center of Fujian Province, Fuzhou, Fujian, 350001, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xun Yuan; Lianglong Chen, Department of Cardiology, Provincial Institute of Coronary Disease, Fujian Medical University Union Hospital, Fuzhou, Fujian, 350001, People’s Republic of China, Email [email protected]; [email protected]
Background: Severe heart failure or cardiogenic shock might arise as a consequence of fulminant myocarditis if it manifests and advances swiftly. The effective implementation of an immunological modulation regimen and mechanical circulatory support has proven instrumental in preserving the lives of individuals experiencing hemodynamic disturbance.
Case Presentation: The current report described a severe instance of fulminant myocarditis in an 18-year-old young woman who presented with severe hypoxemia and hemodynamic instability. The patient was treated with a combination of optimal medical therapy, immunological modulation, extracorporeal membrane oxygenation (ECMO), and an intra-aortic balloon pump (IABP) to support him through his critical period of hemodynamic collapse.
Conclusion: The case presented herein underscored the prompt reversal of life-threatening fulminant myocarditis subsequent to a comprehensive treatment regimen encompassing optimal medical therapy and aggressive mechanical circulatory support.
Keywords: fulminant myocarditis, cardiogenic shock, comprehensive treatment regimen, mechanical circulatory support
Introduction
Fulminant myocarditis, frequently precipitated by viral infections or autoimmune disorders, presents as a clinical syndrome marked by hemodynamically unstable states accompanied by symptoms of acute heart failure and cardiogenic shock.1,2 In real-world scenarios, individuals afflicted with fulminant myocarditis faced an elevated likelihood of mortality or necessitating heart transplantation.2,3 In order to manage hemodynamic collapse, early implementation of Venous-arterial extracorporeal membrane oxygenation (VA-ECMO) and intra-aortic balloon pump (IABP) could be employed for cardiopulmonary support.1 This case report detailed the condition of a young female patient experiencing severe fulminant myocarditis with hemodynamic instability.
Case Presentation
Clinical Manifestation
A 18-year-old previously healthy female (165 cm, 65 kg, body mass index (BMI) 23.9), without pre-existing comorbidities or a family history for cardiac pathologies, was admitted to the cardiac care unit (CCU) at nine o’clock with cold-like symptoms and progressive dyspnea after five days of cold-like symptoms (fever, cough and expectoration). She had shortness of breath, palpitation (Heart rate: 156 beats per minute), and hypotension [Blood pressure (BP): 98/58 mmHg without vasoactive drugs usage]. Upon examination at an external hospital, a pulmonary computerized tomography (CT) revealed indications of cardiogenic pulmonary edema and moderate pulmonary inflammation. The patient presented upon admission in an alert and coherent state, but with a diminished overall condition, exhibiting sinus tachycardia at a rate of 150–160 beats per minute and experiencing oxygenation impairment. Due to hypoxia, the patient necessitated supplemental oxygen administration through both nasal cannula (at a flow rate of 3 L per minute) and mask inhalation (at a flow rate of 6 L per minute) to maintain a transcutaneous pulse oxygen saturation (SPO2) level of approximately 93%. The arterial blood gas analysis revealed a pH value of 7.44, a partial pressure of oxygen of 93 mmHg, and a partial pressure of carbon dioxide of 32 mmHg following the administration of oxygen.
The patient reported no history of smoking or alcohol consumption. Additionally, there was no evidence of illicit drug use, immune-checkpoint inhibitor usage, or anti-tuberculosis medication intake. The patient received two doses of the Coronavirus Disease 2019 (COVID-19) vaccine on July 26th and August 17th, 2021, respectively. The patient contracted COVID-19 infection three months prior as a result of the implementation of a “herd immunity” policy.
Laboratory results on admission showed an increased aspartic transaminase (AST) level of 56 IU/L, creatine kinase (CK) level of 373 IU/L, creatine kinase-MB (CK-MB) level of 36.5 IU/L, troponin I (TnI) level of 4.1 ng/mL (reference range: < 0.02 pg/mL), N-terminal pro brain natriuretic peptide (NT-proBNP) levels of 14,100 pg/mL, and serum creatinine levels of 119 umol/L. The lactate value was 1.7 mmol/L. The D-dimer was in the normal range (1.590mg/L). In addition, the inflammatory markers of white blood cell count, absolute neutrophil count, serum C-reactive protein (CRP), serum procalcitonin, amyloid A and interleukin 6 were 8.27×10^9/L, 6.26×10^9/L, 124.05 mg/L, 0.768ng/mL, 1114.5mg/L and 6235.0pg/mL, respectively. Thyroid function test suggested that hypersensitive thyrotropin (TSH) was decreasing (0.39 mIU/L), but triiodothyronine (T3) and tetraiodothyronine (T4) were normal.
Twelve lead electrocardiogram (ECG) admitted to hospitalization (April 13th, 2023) demonstrated sinus tachycardia. ECG showed QS complex only in V1-V3 leads and 1–2 mm ST-segment depression in II, III, aVF, V4-V6 leads (Figure 1A). Chest radiograph showed bilateral pulmonary scattered inflammatory changes and possible pulmonary oedema after IABP implantation (Figure 1B). After a period of treatment, the ECG findings on April 18th revealed flat or inverted T waves in leads V1-V6 (Figure 1C). On April 19th, chest radiograph showed no signs of pulmonary congestion or inflammation (Figure 1D).
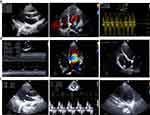
The transthoracic echocardiography (TTE) revealed a severely impaired left ventricular ejection fraction (LVEF ~35.7%), a moderately reduced right ventricular function [tricuspid annular plane systolic excursion (TAPSE) =12 mm)], moderate to severe regurgitation of the mitral valve and tricuspid valve (the estimated pulmonary artery systolic blood pressure was 49 mmHg) (Figure 2A). The inferior vena cava was widened and its’ respiratory collapse rate was less than 50%. The patient was admitted with a diagnosis of fulminant myocarditis: acute heart failure, cardiac function Grade III (New York Heart Association classification system); pulmonary infection; upper respiratory tract infection.
Due to the patient’s hemodynamic instability caused by acute heart failure, a continuous intravenous treatment regimen was administered. This included furosemide (4.1 ug/kg/min), dopamine (2.5 ug/kg/min), and metaraminol bitartrate injection (0.2 ug/kg/min) using microinjection pumps. Additionally, methylprednisolone sodium succinate (320 mg daily) was intravenously administered for five consecutive days to inhibit myocardial inflammation, while being protected by intravenous human immunoglobulin (PH4, 20 mg daily). Pulmonary infection was managed through transvenous administration of cefuroxime sodium every eight hours.
Drug and Instrumental Treatment
Three hours after admission, the patient exhibited a gradual progression into cardiogenic shock, specifically reaching the classic stage as defined by the cardiogenic shock staging of the American Society for Angiocardiography and Intervention. This was characterized by hypotension (blood pressure: 97/50 mmHg with the use of vasoactive drugs) and severely impaired oxygen saturation (SPO2 80%) at twelve o’clock. The patient’s heart rate was measured at 148 beats per minute, and the lactate value was recorded as 2.9 mmol/L at that time. Despite the administration of dopamine and metaraminol bitartrate to stabilize the patient’s vital signs, the cardiogenic shock remained uncorrected.
Thus, an IABP was initially used for cardiogenic shock management in cardiac catheterization room in hospital day one. An IABP device (Impella cardiac power, IAB-06840-U; Teleflex®, Arrow International LLC, USA) was placed to decrease afterload and improved diastolic BP in order to increase pulsatility and improve coronary perfusion. Because of reduced vigilance and ongoing hemodynamic instability, the patient was intubated and ventilated. Subsequently, on the first day of hospitalization in the evening, femoro-femoral veno-arterial extracorporeal membrane oxygenation (VA-ECMO) was administered using the Cardiohelp device (Getinge AB, Göteborg, Sweden). Following initiation, there was a partial reduction in aortic valve opening, leading to the discontinuation of metaraminol bitartrate. Additionally, a daily administration of human blood albumin (10 g) was implemented to enhance colloid osmotic pressure. Furthermore, fresh frozen plasma was administered to improve coagulation function and minimize the risk of bleeding associated with the instrumentation.
On the first day following the initiation of IABP (Counterpulsation pressure: 110 mmHg) and VA-ECMO (Rotation speed: 3495 RPM/min; Flow: 2.62 L/min), TTE still indicated a decrease in myocardial contractility, with an LVEF of 36.6% (Figure 2B). High dose of dopamine combined with furosemide were continued as treatment, while the invasive radial arterial BP was measured at 95/56 mmHg. By the third day after instrument implantation, there was an improvement in myocardial contractility and hemodynamic stabilization was achieved, resulting in a gradual reduction in vasopressor levels to 1.5 ug/kg/min. Thus, extracorporeal membrane oxygenation (ECMO) was discontinued on the fourth day after implantation, resulting in arterial blood pressure (BP) of 112/72 mmHg without the use of dopamine. Due to the patient’s hemodynamic stability, the intra-aortic balloon pump (IABP) was removed on the fifth day after implantation, resulting in arterial BP of 114/74 mmHg. The patient experienced a rapid recovery, as mechanical ventilation was discontinued the following day and arterial BP remained at 112/72 mmHg.
Eight days after she was admitted, TTE revealed that the patient had a normalized cardiac function with no sign of persisting heart failure (left ventricular end diastolic diameter (LVEDD), 42.5 mm; interventricular septum thickness (IVS), 10.5 mm; LVEF, 50.8%) (Figure 2C). We stopped using diuretics because of almost normal cardiac function.
Etiology
Coronary angiography revealed no artery stenosis in hospital day one (Figure 3). Fulminant myocarditis may be caused by a variety of factors, including viral, bacterial, toxic, and autoreactive. In this patient, legionella pneumophila A IgM antibody, mycoplasma and chlamydia IgM antibody, adenovirus IgM antibody, respiratory syncytial virus IgM antibody, influenza virus A and B IgM antibody, and parainfluenza virus antibody were negative. The laboratory test of toxoplasmosis, cytomegalovirus, rubivirus, herpes simplex virus type 1 and 2, parvovirus B19 IgM antibody showed negative but IgG antibody revealed positive. In addition, SARS-CoV-2 RNA was negative through the throat swab test.
 |
Figure 3 The Coronary angiography. Coronary angiography revealed that there was no stenosis or obstructive lesions in the coronary artery April 13th. |
The antinuclear antibody (ANA) was weakly positive (Spotty type 1:100), anti-mitochondrial antibody M2 was positive, anti-Ro-52 antibody and anti-SS-A antibodies were strongly positive. Both myeloperoxidase-ANCA (MPO-ANCA) and proteinase 3-ANCA (PR3-ANCA) were negative. Anti-double-stranded DNA and other autoimmunity anti-body were negative. We considered the patient might suffer from with Sjogren’s syndrome but the labial gland biopsy data were lacking.
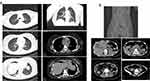
Fever and Depressive State
On hospital day 8, the patient developed fever, with body temperature fluctuating between 38 and 39 degrees. In addition, the inflammatory markers of white blood cell count, absolute neutrophil count, serum CRP and procalcitonin were 23.91×10^9/L, 20.69×10^9/L, 11.04 mg/L and 0.62 ng/mL, respectively. Serological tests for tuberculosis (T-SPOT, TB test), Widal reaction and blood cultures were negative. On the eighth day of hospitalization, a lung CT scan exhibited dispersed streaks in the lower right lung (Figure 4A), prompting a modification in the antibiotic regimen to piperacillin sulbactam (4.5g intravenous every eight hours). Nevertheless, by the tenth day of hospitalization, the patient’s temperature did not show any signs of reduction, raising doubts regarding the association between the fever and the progression of pneumonia. Subsequently, on the eleventh day of hospitalization, a comprehensive abdominal CT scan revealed colorectal dilatation, necessitating heightened awareness for the possibility of paralytic intestinal obstruction (Figure 4B). Following the administration of warm saline retention enema, the patient’s body temperature rapidly declined the following day.
Moreover, the patient exhibited notable levels of anxiety, depression, and suicidal inclinations on the ninth day of hospitalization. To address these concerns, psychological counseling therapy and the administration of sertraline hydrochloride tablets were implemented. Over time, the patient experienced a gradual recovery, leading to their transfer to the intermediate care unit on the thirteenth day and eventual discharge on the fourteenth day. The chronological sequence of events subsequent to the clinical intervention is depicted in Figure 5. Follow-up for seven month after discharge showed the patient had no chest tightness and shortness of breath after activity and the cardiac function was maintained at grade I (New York Heart Association classification system).
Discussion
The condition is characterized by a sudden onset of severe congestive heart failure, followed by a decrease in hemodynamics or the development of severe arrhythmia in the context of acute fulminant myocarditis.4 The progression was notably rapid, with an initial mortality rate ranging from 50% to 70%.4 Etiological factors encompassed infection, autoimmune disease, and toxin/drug toxicity, with viral infection being the primary cause.4 Wang et al5 introduced a novel life support-based comprehensive treatment regimen, incorporating mechanical support through the use of VA-ECMO and IABP, aggressive medical therapy with sufficient doses of glucocorticoids and immunoglobulins.
In this particular case, the patient demonstrated optimal clinical outcomes by employing immunological modulation, promptly escalating mechanical support through the utilization of IABP and VA-ECMO. Adequate quantities of human immunoglobulins were administered to enhance immune response, while appropriate glucocorticosteroids were administered to suppress myocardial inflammatory reactions upon admission. The early initiation of steroid therapy significantly enhances clinical outcomes, prognoses, and long-term survival rates.6
After administering high-dose oral steroids with a gradual tapering regimen, three cases demonstrated complete recovery and normalization of cardiac contractility.7 Subsequently, an IABP device was promptly inserted to reduce afterload, enhance coronary perfusion, increase pulsatility, and unload the left ventricle posterior pressure. Additionally, VA-ECMO was actively provided on the first night. By the third day of combined implantation, the patient’s myocardial contractility improved, leading to stabilized hemodynamics and a reduced dosage of vasopressors.1,5 This combined mechanical circulatory support approach has proven successful in facilitating the recovery of patients with acute myocarditis.
Naturally, it was imperative to acknowledge a sequence of issues that arose in the patient subsequent to the cessation of the aircraft, including the manifestation of fever on the eighth day of hospitalization and the conspicuous display of symptoms associated with depression on the ninth day. These circumstances underscored the necessity for a comprehensive approach to patient care, encompassing prompt psychological counseling interventions. The etiology of the fever was presumed to be linked to the presence of paralytic ileus, as evidenced by the patient’s rapid decline in body temperature following the administration of a warm saline retention enema.
The potential association between paralytic ileus and the administration of sedative drugs (midazolam, propofol, and remifentanil) for mechanical ventilation analgesia was suggested.8 This implied that healthcare professionals should enhance the surveillance of adverse reactions to general anesthetic agents and remain vigilant regarding the possibility of paralytic intestinal obstruction when utilizing remifentanil hydrochloride for injectable analgesia. The occurrence of a dual cardiac condition in the young patient could be attributed to the unfamiliar and anxiety-inducing environment in the intensive care unit, as well as the presence of intricate tubes affixed to their body. Therefore, we should pay more attention to the comprehensive management of patients’ physical and mental problems under the modern medical model.9
Histological and immune-histological specimens can be obtained through biopsies for clinical diagnosis purposes.10,11 Nevertheless, the patient in question was unable to undergo myocardial biopsy and cardiac magnetic resonance (CMR) due to cardiogenic shock during the initial stages of the disease and the excessively cautious healthcare environment prevalent in China. Ultimately, based on the patient’s medical history, clinical presentation, and supplementary examinations, viral myocarditis emerged as the principal consideration.
Conclusions
The case presented herein underscored the prompt reversal of life-threatening fulminant myocarditis subsequent to a comprehensive treatment regimen encompassing optimal medical therapy and aggressive mechanical circulatory support.
Ethical Statement
With the written consent of the patient, we summarized the case data from the hospital’s internal documentation. The patient provided the consent for the publication of this case. This disclosure of the case detail was approved by the Clinical Research Ethics Committee of Fujian Medical University Union Hospital.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by grants from the talent start-up capital program of Fujian Medical University Union Hospital (2023XH027), the Education and Research Project (Science and Technology) for Young and Middle-aged Teachers of Fujian Province (JAT200164).
Disclosure
The authors have no conflicts of interest to declare in this work.
References
1. Vishram-Nielsen JKK, Foroutan F, Rizwan S, et al. Patients with fulminant myocarditis supported with veno-arterial extracorporeal membrane oxygenation: a systematic review and meta-analysis of short-term mortality and impact of risk factors. Heart Fail Rev. 2023;28(2):347–357. doi:10.1007/s10741-022-10277-z
2. Kanaoka K, Onoue K, Terasaki S, et al. Features and outcomes of histologically proven myocarditis with fulminant presentation. Circulation. 2022;146(19):1425–1433. doi:10.1161/CIRCULATIONAHA.121.058869
3. Baritussio A, Schiavo A, Basso C, et al. Predictors of relapse, death or heart transplantation in myocarditis before the introduction of immunosuppression: negative prognostic impact of female gender, fulminant onset, lower ejection fraction and serum autoantibodies. Eur J Heart Fail. 2022;24(6):1033–1044. doi:10.1002/ejhf.2496
4. Section of Precision Medical of Chinese Society of Cardiology of Chinese Medical Association; Editorial Board of Chinese Journal of Cardiology; Working Group on Adult Myocarditis. 中国成人暴发性心肌炎临床诊治专家共识声明 [Chinese expert consensus statement on clinical diagnosis and treatment of fulminant myocarditis in adults]. Zhonghua Xin Xue Guan Bing Za Zhi. 2017;45(9):742–752. Chinese. doi:10.3760/cma.j.issn.0253-3758.2017.09.004
5. Wang D, Li S, Jiang J, et al. Chinese society of cardiology expert consensus statement on the diagnosis and treatment of adult fulminant myocarditis. Sci China Life Sci. 2019;62(2):187–202. doi:10.1007/s11427-018-9385-3
6. Yanagisawa T, Inomata T, Watanabe I, et al. Clinical significance of corticosteroid therapy for eosinophilic myocarditis. Int Heart J. 2011;52(2):110–113. doi:10.1536/ihj.52.110
7. Wong CW, Luis S, Zeng I, Stewart RA. Eosinophilia and coronary artery vasospasm. Heart Lung Circ. 2008;17(6):488–496. doi:10.1016/j.hlc.2008.06.003
8. Alcaraz Lorente PJ, Aguayo Albasini JL, Parrilla Paricio P, et al. [Influence of general anesthetic agents on postoperative paralytic ileus. Experimental study in dogs]. Rev Esp Anestesiol Reanim. 1987;34(2):108–114. Spanish.
9. Ono R, Kitagawa I. Double Heart-Shaped Silhouette. Gastroenterology. 2021;161(2):427–428. doi:10.1053/j.gastro.2021.04.072
10. Jiang L, Wang L, Zhao C, et al. Atrial-His bundle pacing in fulminant myocarditis with ventricular arrhythmia: a case report. BMC Cardiovasc Disord. 2022;22(1):497. doi:10.1186/s12872-022-02936-8
11. Mavrogeni S, Papadopoulos G, Hussain T, Chiribiri A, Botnar R, Greil GF. The emerging role of cardiovascular magnetic resonance in the evaluation of Kawasaki disease. Int J Cardiovasc Imaging. 2013;29(8):1787–1798. doi:10.1007/s10554-013-0276-9
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.