Back to Journals » ClinicoEconomics and Outcomes Research » Volume 14
A US Retrospective Claims Analysis Comparing Healthcare Costs of Patients Transitioning from Immediate-Release Oxycodone to Two Different Formulations of Extended-Release Oxycodone: Xtampza ER or OxyContin
Authors Olatoke O, Zah V , Stanicic F , Vukicevic D , Yfantopoulos P, Thompson C, DeGeorge MK, Passik S
Received 1 October 2021
Accepted for publication 23 February 2022
Published 3 March 2022 Volume 2022:14 Pages 119—128
DOI https://doi.org/10.2147/CEOR.S340290
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Samer Hamidi
Oluwadara Olatoke,1 Vladimir Zah,1 Filip Stanicic,1 Djurdja Vukicevic,1 Platonas Yfantopoulos,1 Christy Thompson,2 Michael K DeGeorge,2 Steven Passik2
1HEOR Department, ZRx Outcomes Research, Mississauga, Ontario, Canada; 2Medical Department, Collegium Pharmaceutical Inc., Stoughton, MA, USA
Correspondence: Oluwadara Olatoke, HEOR Department, ZRx Outcomes Research Inc., 3450 Cawthra Road, Mississauga, ON, L5A 2X7, Canada, +1 416 953 4427, Email [email protected]
Purpose: Opioid therapy for managing chronic pain remains a challenge, as providers must weigh the medical benefit to the patient with the risk of adverse events. Manipulation of many extended-release (ER) opioid formulations may lead to increased serious medical outcomes or death. The economic burden of opioid use disorders due to opioid misuse and abuse may vary depending on which abuse deterrent opioid formulation is prescribed. The study aimed to compare demographic and clinical characteristics and healthcare costs of chronic pain patients treated with two different abuse-deterrent opioid formulations, Xtampza ER and reformulated OxyContin.
Methods: The source of data was IBM® MarketScan® Commercial Claims and Encounters Medicare Supplemental database, from January 2016 through February 2020. Patients with chronic pain were assigned to either the Xtampza ER or the OxyContin cohort based on the initial ER opioid prescription set as the index date. Continuous healthcare coverage was required during a minimum 3-month pre-index and 9-month post-index periods. Pre-index patients’ characteristics were analyzed. Healthcare costs of Xtampza ER vs OxyContin were assessed in the post-index period.
Results: After applying selection criteria, 464 patients were observed in the Xtampza ER cohort versus 1927 patients in the OxyContin cohort. In unmatched patients, ER opioid costs were lower for Xtampza ER than OxyContin ($2645 vs $3141; p< 0.001), which ultimately led to lower total prescription costs for the Xtampza ER cohort compared to the OxyContin cohort ($7492 vs $8754; p=0.016). In matched patients, the total healthcare costs were significantly lower in the Xtampza ER cohort than in the OxyContin cohort, $22,630 vs $28,386 (p=0.005), respectively.
Conclusion: This study suggests that Xtampza ER may result in lower healthcare costs than OxyContin for a population of chronic pain patients switching from immediate release oxycodone based on real-world data.
Keywords: chronic pain, opioids, abuse-deterrent, short-acting, long-acting, cost
Introduction
Chronic pain represents the most common reason for patients to seek medical care in the US1 and is found to be one of the most common causes of the general health degradation impacting patients’ quality of life, daily activities, and employment status.2,3 It accounts for an estimated $635 billion yearly in medical costs and decreased work productivity.1
Opioids have been described as effective drugs for relieving moderate-to-severe pain, though they all carry substantial risk.4 Immediate release (IR) opioids are indicated for short-term relief of moderate-to-severe pain beneficial for patients with temporary pain.5 ER opioids are recommended for the management of pain severe enough to require daily, around-the-clock, long-term treatment and for which alternate treatments are inadequate.6 The use of opioids may become necessary as they remain a part of the armamentarium for managing chronic pain for patients who do not respond to non-opioid and other therapies. However, inherent risks exist in the clinical choice for opioid treatment, including the risks of misuse, abuse, diversion, and overdose, which can result in serious life-threatening consequences, consumption of healthcare resources, prolonged hospital stay, and symptomatic treatment.5,7 Tailoring pain treatment based on the needs and characteristics of an individual patient and their risk of abuse, misuse, diversion, or overdose represents an essential part of pain management, with the choice of appropriate opioid therapy coming after a careful clinical judgment of every patient.5
Opioid abuse and misuse often involve manipulation of the product to obtain greater plasma levels more quickly than taking the intact oral formulation. Manipulation of most ER opioid formulations can result in greater exposure to the drug than intended, leading to an increase in the risk of serious medical outcomes or death compared to abuse of intact oral formulations.8 In 2015, the Food and Drug Administration (FDA) released Guidance for Industry regarding the development of abuse-deterrent opioid formulations (ADFs). Their stated goal was to create opioid formulations designed to deter abuse by making the formulation more resistant to manipulation and making abuse of the manipulated product less attractive or less rewarding.9 Industry responded by developing formulations aimed at targeting known or expected routes of abuse, such as crushing for oral use or insufflation, or dissolving to inject.10
Initial in vitro, pharmacokinetic, and human abuse potential studies have demonstrated that ADFs differ in the degree to which they are resistant to manipulation.10 More recent studies aimed at better understanding the real-world implications of ADFs (Real-World Evidence studies or RWE) support findings from these earlier studies. The large national studies demonstrated differences in misuse, abuse, and diversion rates among ADF ER opioids.11,12 Still, the economic implications of these findings have not been further elaborated. There is also a lack of studies directly comparing different formulations of the same medication, and this may be the most accurate way to measure the impact of ADF formulations.
The analysis of healthcare costs related to the treatment of chronic pain with ADF medications in the real-world setting would help provide essential evidence on the cost-effectiveness of these drugs among chronic pain patients. Therefore, the primary aim of the current analysis was to compare the economic outcomes of the two ADF ER opioids, Xtampza ER vs OxyContin, among non-cancer chronic pain patients who transitioned from IR to ER oxycodone treatment.
Methodology
Data Source
The retrospective study was conducted on US insurance claims data from the IBM® MarketScan® Commercial Claims and Encounters Medicare Supplemental Databases. These databases represent the largest de-identified US patient data collection with approximately 240 million covered lives from over 300 employers and health plans across the US. The study databases comply with the Health Insurance Portability and Accountability Act of 1996, protecting the privacy and ensuring the confidentiality of personal data. The study used only de-identified data, thus Institutional Review Board approval to conduct this study was not required.
Study Design
A retrospective cohort analysis was conducted using commercially insured patients’ claims, employing data from June 01, 2015, through February 29, 2020. The patient selection process was performed between June 01, 2016, and May 31, 2019 (see Figure 1).
Patients 18–64 years old and prescribed Xtampza ER or OxyContin during the selection window were included in the analysis. Based on the initial prescription, patients were assigned to the Xtampza ER cohort or OxyContin cohort. The date of the initial prescription was set as the index date. The observational period covered the timeframe from 3 months before to 9 months after the index date. Patients were required to have continuous healthcare and pharmacy coverage during the observational period. To select patients with long-lasting pain, patients were required to have had at least a 90-day supply of the initially prescribed ER opioid. Additionally, at least one claim with ICD-10 codes related to chronic pain was required within the pre-index period. The National Drug Codes (NDCs) extracted from the corresponding Redbook were used to identify IR opioids, Xtampza ER, and OxyContin (see Appendix Tables A1 & A2).
Patients were excluded from the study due to the following reasons:
- for having diagnostic/procedural codes for cancer or palliative care within the observational period (see Appendix Table A3),
- for having a diagnosis of diabetic neuropathy or fibromyalgia within the pre-index period (see Appendix Table A4),
- if concomitantly using other ER opioids in the 9-month follow-up period,
- for having a gap in the health plan or pharmaceutical coverage during the observational period.
Patients’ demographic characteristics were captured on the index date, and clinical characteristics were observed during the pre-index period, while outcomes were measured during the post-index period. Patients’ characteristics and healthcare costs were observed and compared between Xtampza ER and OxyContin treatment cohorts.
Outcomes
Healthcare costs were measured during the 9-month follow-up period. All-cause and opioid use disorders (OUD)-related costs were reported for the following categories: total cost, inpatient, outpatient, emergency department (ED), and outpatient prescription cost. The OUD-related costs were calculated as the sum of costs of all claims associated with opioid abuse, opioid dependence, opioid-induced disorders, poisoning by opioids, and adverse effects of opioids, and captured in the outpatient or inpatient settings (Appendix Table A5), while the OUD-related prescription costs were determined based on the NDCs for OUD-related drug prescriptions (buprenorphine, naloxone, naltrexone, and methadone). Healthcare costs represent the amount paid by the health plan and were evaluated on a per-member basis. The cohorts of XtampzaER- and OxyContin-treated patients were adjusted for their baseline characteristics using the propensity-score matching process. The healthcare costs were presented for the non-matched and matched cohorts of the Xtampza ER- and OxyContin-treated patients.
Statistical Analysis
The differences between the cohorts were tested using the independent t-test for continuous variables and the chi-square test for categorical variables. Results were validated using bootstrapping analysis to account for the uncertainty of the estimates. P-values less than 0.05 were considered statistically significant.
To minimize study selection bias and adjust for confounders, patients in the Xtampza ER cohort were propensity score-matched to those treated with OxyContin in the 1:4 matching ratio. Propensity scores were retrieved from the multivariable logistic regression, with all relevant confounders included.
All analyses were performed in the IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY.
Results
Characteristics of the Non-Matched Study Population
The mean age of the patients in both cohorts was approximately 50 years. Patients were equally distributed in sub-groups by the health plan, and there were no significant differences between the cohorts. A substantially higher proportion of patients treated with OxyContin resided in the North East region (10.3% vs 18.5%, p<0.001), while a higher proportion of Xtampza ER-treated patients were located in the South region (59.3% vs 53.0%, p=0.016), see Table 1.
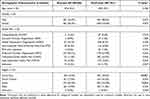 |
Table 1 Demographic Characteristics of the Non-Matched Study Population |
Observing clinical characteristics within the non-matched sample of patients, the cohorts showed significant differences in terms of the mean Charlson Comorbidity score (CCI) score (Xtampza ER=0.3 vs OxyContin=0.4, p=0.004) and CCI sub-groups (see Table 2). However, no significant differences were seen among components of CCI score apart from diabetes with chronic complication (Xtampza ER=0.2% vs OxyContin=1.3%, p=0.046). Regarding the mental health disorders and conditions causing chronic pain, no significant differences were noted except for disorders of the spine where a higher proportion of patients was noted in the Xtampza ER cohort (94.4% vs 88.9%, p<0.001).
 |
Table 2 Clinical Characteristics in the Non-Matched Study Population |
Economic Outcomes in the Non-Matched Study Sample
The all-cause and OUD-related healthcare costs stratified by service setting in the non-matched study sample are listed in Table 3. Significantly higher outpatient prescription costs were observed in the OxyContin cohort of patients ($7492 vs $8754, p=0.016). The difference in the outpatient prescription costs stems from the higher ER opioid costs in the OxyContin cohort than in the Xtampza ER cohort ($2645 vs $3141, p<0.001). Total healthcare costs were substantially higher for the OxyContin- than the Xtampza ER-treated patients ($22,630 vs $28,386, p=0.005). Additionally, statistical differences among the cohorts were noted in the OUD-related inpatient and OUD-related total costs (Xtampza ER=$91 vs OxyContin=$388, p=0.001; Xtampza ER=$322 vs OxyContin=$604, p=0.048, respectively).
 |
Table 3 Healthcare Costs in the Non-Matched Study Sample |
Propensity-Score Matching
Patients were matched based on the pre-index characteristics using the propensity score (PS) matching technique with matching ratio 1:4 and 0.001 caliper. Variables used in the PS matching process were selected based on Pearson’s correlation matrix, logistic and linear regression. The following variables were controlled: region of the patients’ residence, CCI score, and spine disorders. After the PS matching process, 463 Xtampza ER-treated patients were successfully matched to 1573 OxyContin-treated patients. Demographic characteristics between the matched groups were well balanced (see Appendix Table A6). After PS matching, no significant differences were found in either the CCI score or its components. Also, no differences were noted in the components of mental health or chronic pain conditions between the treatment cohorts (Appendix Table A7).
Cost-Analysis in the Matched Sample
All-cause and OUD-related healthcare costs stratified by service setting in the matched study sample are presented in Table 4. Substantially higher total healthcare costs were demonstrated in OxyContin-treated than Xtampza ER-treated patients ($22,575 vs $26,986, p=0.034). A significant difference between the treatment cohorts was observed in terms of the ER opioid and OUD-related inpatient healthcare costs, which were consistently lower in the Xtampza ER cohort ($2645 vs $3056, p<0.001; $92 vs $330, p=0.014, respectively).
 |
Table 4 Healthcare Costs in the Matched Study Sample |
In contrast to the non-matched study population, outpatient prescription costs did not significantly differ between the treatment cohorts (Xtampza ER=$7502 vs OxyContin=$8189, p=0.247), despite the substantially higher ER opioid costs in the OxyContin cohort.
The results obtained by the bootstrapping analysis confirmed the results of the independent t-test, demonstrating that the uncertainty of the outcome estimates did not impact the study conclusions.
Discussion
The adoption of ADF opioids represents an approach to manage abuse, misuse, and diversion of opioids while providing pain control for people who suffer from chronic moderate-to-severe pain. To our knowledge, this is the first study that provides real-world insight into the comparative healthcare costs of two ADF opioids with the same active compound but different abuse-deterrent properties.
While OxyContin and Xtampza ER are both ADF formulations of ER oxycodone, their technologies differ, as does their FDA-approved labeling. OxyContin is a hard tablet formulation that uses INTAC technology to impart a hard shell, along with a compound that gels upon exposure to liquid. Xtampza ER is a microsphere-in-capsule formulation that uses DETERx technology to impart both ER and ADF properties to each individual microsphere (~300 microns in diameter). Both Xtampza ER and OxyContin have FDA-approved labeling stating in vitro data demonstrate that they have physicochemical properties expected to make abuse by injection difficult as well as language around in vitro studies demonstrating resistance to certain types of manipulation. They also have labeling stating that Human Abuse Potential studies demonstrate the formulations are expected to reduce abuse via the intranasal route. Their labeling differs, however, in that Xtampza ER is also expected to reduce abuse via the oral route. Further, in human pharmacokinetic studies, when crushed or chewed, Xtampza ER does not dose dump (ie, it is bioequivalent to Xtampza ER intact), whereas OxyContin, when crushed or chewed, exhibits dose-dumping (ie, is bioequivalent to IR oxycodone).13,14 The differences in formulation and, thus, labeling may have implications for abuse in the real world.
Postmarketing, RWE data have begun to elucidate how manipulation-resistance demonstrated within the FDA-approved labeling (in vitro, pharmacokinetic, and Human-Abuse Potential studies) is reflected in real-world abuse, misuse, and diversion. Postmarketing studies have reported continued manipulation of OxyContin for abuse. In one study, one-third of people who abuse OxyContin managed to manipulate the drug and circumvent the ADF formulation.15 In a separate study, one-fifth of patients continued intravenous abuse of OxyContin after reformulation.16
Two additional studies have demonstrated data in support of continued OxyContin abuse, misuse, and diversion. One recent analysis used the National Addictions Vigilance Intervention and Prevention Program (NAVIPPRO) Addiction Severity Index–Multimedia Version (ASI-MV) to understand rates of past 30-day non-medical use (NMU) in individuals entering substance abuse treatment. The researchers found lower rates of NMU for Xtampza ER compared with other ER ADF oxycodone (99% ADF OxyContin and Authorized Generic). This was true at both the population and drug utilization levels and was maintained over a 3.5-year time period ending Q4 2019. Further, Xtampza ER had lower rates of non-oral manipulation, including insufflation and injection, than did the other ER ADF oxycodone group.11
A second postmarketing RWE study collected abuse, misuse, and diversion data over a 3-year time period (ending Q2 2019) from the Researched Abuse, Diversion and Addiction-Related Surveillance (RADARS®) System. This system utilizes a mosaic approach to detect multiple different misuse, abuse, and diversion signals. Across nearly all systems, the researchers found lower rates of abuse and misuse of Xtampza ER compared with other ADF ER opioids (Reformulated OxyContin represented 88% of the utilization among this group during the study period). In addition, rates of diversion of Xtampza ER were lower than for other ADF ER opioids.12 Although it was not a specific aim of this study, future research might help to uncover additional medical utilization costs associated with formulations more attractive for diversion by those who might seek to borrow, buy or steal opioids that are prescribed to the person with pain. For example, clinical experience has shown that having one’s medication stolen could lead to withdrawal in the person for whom the prescription was intended. This could, in turn, lead them to an emergency Department to seek treatment and might even require inpatient admission. Undoubtedly there are other complications that could arise in the wake of people with pain finding themselves unexpectedly missing their supply of medications.
Numerous studies have explored the economic impact and cost-effectiveness of ADFs. A hypothetical 2-year model analyzed the budget impact of the introduction of an ADF morphine formulation, incorporating real-world evidence on misuse/abuse rates, healthcare resource use, and costs. Based on the model conclusions, adding the ADF morphine formulation to formulary resulted in decreased abuse-related healthcare costs by over half-million dollars over 2 years. The savings offset the initially higher cost of the ADF drug prescription.17
Similar findings were presented in a real-world retrospective analysis of insurance claims that found that the implementation of ADFs resulted in a substantial reduction in all-case and OUD-related hospitalizations and ED visits. The healthcare cost reduction offsets the increased pharmacy costs for the novel formulations.18
In 2017, the Institute for Clinical and Economic Review assessed the clinical effectiveness and cost-effectiveness of 10 ADF opioids. Based on the report, limited evidence existed at the time on the incremental value of ADFs in reducing opioid abuse. The report emphasized that expenditures for the use of ADF formulations are substantially higher, even when accounting for the effect on preventing opioid misuse and abuse.19 However, this report did not include Xtampza ER or currently available real-world evidence, and is therefore not reflective of the currently marketed ADF products, of which there are only three.
The current study compared healthcare costs of two distinct ADF ER oxycodone formulations that differ in their underlying technology. The possible bias in study outcomes has been minimized as the active compound in both medications is the same. Additionally, the cohorts have been matched based on the list of thoroughly examined confounding characteristics to lower the possibility of selection bias and confounding effect.
Analysis of insurance claims showed that Xtampza ER represents a cost-saving option for treating long-lasting chronic pain compared to OxyContin. The mean total healthcare costs for patients treated with Xtampza ER were substantially lower than the mean costs for OxyContin-treated patients in a real-world setting ($22,630 vs $28,386, p=0.005) primarily due to the lower ER opioid prescription cost in the Xtampza ER cohort ($2645 vs $3141, p<0.001). Notable differences were also observed in OUD-related inpatient and OUD-related total costs. Additionally, the difference remained significant when outcomes were adjusted for confounders in the PS matching-controlled environment ($22,575 vs $26,986, p=0.034). Specifically, the ER opioid costs and OUD-related inpatient costs remained higher in the OxyContin cohort, while there was no significant difference in OUD-related total costs ($323 vs $525, p=0.336). This observation can be explained by statistical factors that may affect the comparison, such as sample size and the variable standard deviation characteristic for cost variables.
Strengths and Limitations
Database research provides a valuable insight into real-world clinical practice and healthcare costs across the US. Therefore, we aimed to overcome database limitations (discussed below) by employing data cleaning, careful patient selection, and various methods to control confounders, such as propensity score matching. Limitations of the study may stem from limits of the RWE analysis, database characteristics, and coding system disadvantages. As retrospective claims data are primarily created for billing purposes, there are pitfalls related to this study type, including data entry errors and miscoding, gaps in insurance coverage, duplicate or negative-cost claims. Administrative databases are limited to prescribed opioid claims, so we could not track the use of opioids not prescribed by a healthcare practitioner or for purposes not intended by a prescriber. The use of medication for purposes other than indicated was not captured. An additional limitation is a lack of data related to chronic pain severity. Also, the history of OUD in the claims data was not assessed due to the relatively short pre-index period. Finally, the retrospective analysis was conducted in the commercially insured sample of adult patients. There was a limited representation of adolescents, older adults (≥65 years of age), the Medicare population, and Medicaid beneficiaries in the database. Hence, our findings may not be generalizable to those populations.
Conclusions
Our retrospective study demonstrated the significant benefits in regard to healthcare costs of one ADF ER oxycodone formulation, Xtampza ER, over another, OxyContin, in the management of non-cancer chronic pain patients. Although both medications were developed as ER oxycodone ADF formulations, this analysis reported potential significant cost advantages with the Xtampza ER formulation. To confirm and further elucidate our findings, further studies should consider patients’ baseline risk of abuse and chronic pain severity.
Abbreviations
ADF, abuse-deterrent formulation; ASI-MV, addiction severity index-multimedia version; CCI, Charlson comorbidity score; CDHP, consumer-driven health plan; ED, emergency department; ER, extended release; EPO, exclusive provider organization; FDA, Food and Drug Administration; HDHP, high deductible health plan; HMO, health maintenance organization; IR, immediate release; NAVIPPRO, national addictions vigilance intervention and prevention program; NDC, national drug codes; NMU, non-medical use; Non-CapPOS, non-capitated point-of-service; OUD, opioid use disorders; PPO, preferred provider organization; PS, propensity score; RADARS®, researched abuse, diversion and addiction-related surveillance system.
Data Sharing Statement
The data used in the analysis were extracted from the IBM MarketScan® Commercial and Medicare Supplemental Databases. The MarketScan® Research Databases are under the license of the IBM and are available from Vladimir Zah ([email protected]) upon reasonable request and with permission of the IBM and Endo Pharmaceutical Inc.
Ethics Approval and Informed Consent
Researchers confirmed they have obtained permission from the dataset owner to use the information in databases/repositories for the purposes of this research. The study was exempted from requiring ethical approval as all the data were de-identified and compliant with the US Health Insurance Portability and Accountability Act (HIPAA).
All patient data used in the current study were deidentified in compliance with the HIPAA. As such, there was no requirement for institutional review board approval and this aligns with ZRx Outcomes Research Inc., internal policies to waive the need for IRB review for these type of studies.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by Collegium Pharmaceutical, Inc. The source of funding had no influence on the study design, analysis, or interpretation of data.
Disclosure
OO, VZ, FS, DV, and PY are employees of ZRx Outcomes Research. VZ reports grants and/or personal fees from Glympse Bio, HutchMed Pharmaceuticals, Endo Pharmaceuticals, Stealth Biotherapeutics, RedHill Pharmaceuticals, and Collegium Pharmaceuticals, outside the submitted work. FS reports grants from Collegium Pharmaceutical Inc., during the conduct of the study. DV reports grants from Collegium Pharmaceutical, Inc., during the conduct of the study. CT, MKDG, and SP are employees of Collegium Pharmaceutical, Inc. The authors’ competing interests had no influence on study design, interpretation of the results or impose a censoring of the obtained results. The authors declare no other competing interest.
References
1. Moorman-Li R, Motycka CA, Inge LD, Congdon JM, Hobson S, Pokropski B. A review of abuse-deterrent opioids for chronic nonmalignant pain. P T. 2012;37(7):412–418.
2. Clauw DJ, Essex MN, Pitman V, Jones KD. Reframing chronic pain as a disease, not a symptom: rationale and implications for pain management. Postgrad Med. 2019;131(3):185–198. doi:10.1080/00325481.2019.1574403
3. Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain. 2015;16(8):769–780. doi:10.1016/j.jpain.2015.05.002
4. Lowinson JH. Substance Abuse: A Comprehensive Textbook. Lippincott Williams & Wilkins; 2005.
5. Fine PG, Mahajan G, McPherson ML. Long-acting opioids and short-acting opioids: appropriate use in chronic pain management. Pain Med. 2009;10(Suppl 2):S79–88. doi:10.1111/j.1526-4637.2009.00666.x
6. McCarberg BH, Barkin RL. Long-acting opioids for chronic pain: pharmacotherapeutic opportunities to enhance compliance, quality of life, and analgesia. Am J Ther. 2001;8(3):181–186. doi:10.1097/00045391-200105000-00006
7. Chung CP, Callahan ST, Cooper WO, et al. Individual short-acting opioids and the risk of opioid-related adverse events in adolescents. Pharmacoepidemiol Drug Saf. 2019;28(11):1448–1456. doi:10.1002/pds.4872
8. Green JL, Bucher Bartelson B, Le Lait MC, et al. Medical outcomes associated with prescription opioid abuse via oral and non-oral routes of administration. Drug Alcohol Depend. 2017;175:140–145. doi:10.1016/j.drugalcdep.2017.01.039
9. Food and Drug Administration Center for Drug Evaluation and Research. Abuse-deterrent opioids —evaluation and labeling. Available from: https://www.fda.gov/files/drugs/published/Abuse-Deterrent-Opioids-Evaluation-and-Labeling.pdf.
10. Carinci AJ. Abuse-deterrent opioid analgesics: a guide for clinicians. Pain Manag. 2020;10(1):55–62. doi:10.2217/pmt-2019-0052
11. Green JL, Robbins RS, Dailey-Govoni T, Butler SF. Nonmedical use of Xtampza(®) ER and other oxycodone medications in adults evaluated for substance abuse treatment: real-world data from the Addiction Severity Index-Multimedia Version (ASI-MV(®)). J Pain Res. 2021;14:1773–1783. doi:10.2147/JPR.S304805
12. Geoffrey Severtson S, Kreider SED, Amioka EC, Margolin ZR, Iwanicki JL, Dart RC. Postmarketing analysis of misuse, abuse, and diversion of Xtampza ER. Pain Med. 2020;21(12):3660–3668. doi:10.1093/pm/pnaa272
13. Food and Drug Administration. Product Information - XTAMPZA ER. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/208090s000lbl.pdf.
14. Food and Drug Administration. Product information - Oxycontin. Available from: https://www.fda.gov/media/131026/download.
15. Cicero TJ, Ellis MS. Abuse-deterrent formulations and the prescription opioid abuse epidemic in the United States: lessons learned from OxyContin. JAMA Psychiatry. 2015;72(5):424–430. doi:10.1001/jamapsychiatry.2014.3043
16. Cicero TJ, Ellis MS, Kasper ZA. A tale of 2 ADFs: differences in the effectiveness of abuse-deterrent formulations of oxymorphone and oxycodone extended-release drugs. Pain. 2016;157(6):1232–1238. doi:10.1097/j.pain.0000000000000511
17. Rossiter LF, Kwong WJ, Marrett E. Healthcare resource use and cost: the impact of adopting an abuse-deterrent formulation of extended release Morphine. Clinicoecon Outcomes Res. 2020;12:35–44. doi:10.2147/CEOR.S226607
18. Green T, Perkins M, Kwong J, Jones B. Impact of abuse-deterrent formulation opioid utilization on healthcare resource use among managed medicaid patient.
19. Institute for Clinical and Economic Review. Opioid epidemic: abuse deterrent opioids. Available from: https://icer.org/assessment/opioids-abuse-deterrent-2017/.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

