Back to Journals » International Journal of Women's Health » Volume 15
A Study on the Psychological Experience and Influential Factors of Pregnant Women Who Decided Elective Caesarean Section After Public Health Emergencies – A Cross-Sectional Survey
Authors Dai C, Wang X, Xu C, Bai L, Li Y
Received 27 April 2023
Accepted for publication 13 October 2023
Published 9 November 2023 Volume 2023:15 Pages 1713—1725
DOI https://doi.org/10.2147/IJWH.S418959
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
Chunye Dai,1,* Xuelu Wang,1,* Chenying Xu,1 Lina Bai,1 Yuehong Li2
1Operating Room, Shanghai Key Laboratory of Maternal Fetal Medicine, Shanghai Institute of Maternal-Fetal Medicine and Gynecologic Oncology, Shanghai First Maternity and Infant Hospital, School of Medicine, Tongji University, Shanghai, People’s Republic of China; 2Nursing Department, Shanghai Key Laboratory of Maternal Fetal Medicine, Shanghai Institute of Maternal-Fetal Medicine and Gynecologic Oncology, Shanghai First Maternity and Infant Hospital, School of Medicine, Tongji University, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Chenying Xu, Tel +86 021-20261099, Email [email protected]
Background: The COVID-19 pandemic used to be a major public health emergency which affected people worldwide, and it affected individuals’ body, mood, work and lifestyle to some extent. The pregnant woman affected by the unstable hormone will be more sensitive than normal ones. Long-term depression and anxiety could feedback on their body and lead to a host of pregnancy complications. Because pregnant women who choose cesarean section are awake during the perioperative period, to ensure safety, the degree of cooperation about psychology and behavior is relatively high, so we should know the psychological state of such a group of people.
Objective: This study aims to explore psychological experience and influential factors of pregnant women who decided elective caesarean section after the COVID-19 pandemic.
Methods: This is a cross-sectional study carried out in a hospital in Shanghai, according to the inclusion and exclusion criteria, we selected pregnant women who selected elective cesarean section as the study objects, all participants provided informed consent and completed questionnaires, including sociodemographic questionnaire, Generalized Anxiety Disorder scale (GAD-7) and General Well-Being Schedule (GWBS). Software SPSS 23.0 was used to analyze and explore the influencing factors.
Results: Eligible 595 questionnaires were included in the study, the mean score of GAD-7 was 4.855 ± 3.254 and 90.699 ± 13.807 of GWBS. Generalized linear regression analysis revealed several factors that were statistically significant with the two scales, including birthplace, average monthly income, number of abortion and pregnancy complication (p < 0.01).
Conclusion: The COVID-19 infection status and symptoms around infection have no statistical difference in anxiety level and general well-being after they experience the COVID-19 pandemic. However, through this study, we found some influencing factors that worth further exploration. In the future, we will expand the sample size to explore the different situation of multi-center, and we hope provide psychological nursing interventions based on existing results to offer a better delivery experience.
Keywords: public health emergency, cesarean section, pregnant woman, psychological experience
Introduction
The COVID-19 pandemic used to be a major public health emergency which affected people worldwide.1 The hazard of disease and the protection from national level made a change in the social operation,2 and also affected individuals’ work, study and life to some extent, which challenged the emotional and mental stability of residents.3 Some studies4,5 have pointed out that the proportion of residents’ anxiety and stress increased during the COVID-19 pandemic, mainly due to the following reasons: feeling uncertainty about the future direction of life and work, worrying about the impact of COVID-19 on the health of themselves and family members, unable to pay for family expenses anymore and lack of care from family and friends. After a period of effective control, China decided to implement the “Class B and B management program” for the COVID-19 infection domestically from January 2023.6 According to the survey data released by many provinces around the New Year, the positive infection rate in many provinces has reached more than 50%.7 As the disease brought physical changes, such as cough, fever, limb pain, insomnia, loss of taste and smell, loss of appetite and so on,8 not only affects people’s health status and quality of life in a period of time9, but also lacking knowledge for these diseases made people feel anxiety, panic and depression.10
It was found anxiety is common among pregnant women. Firstly, during early pregnancy, hormones like estrogen and progesterone increase, which could easily affect emotional fluctuations.11 Secondly, during middle pregnancy, fear of childbirth and lack of knowledge would make them hard to adapt to the physical changes, which would easily increase the risk of anxiety.12 Thirdly, during late pregnancy, they concerned about their physical appearance, complications, and the safety of their child during delivery, which would also increase anxiety and depression level.5 As a harmful teratogen which affects the fetal development, pregnancy stress and anxiety can increase the risk of pregnancy complications by the hypothalamic–pituitary–adrenal cortex system and the sympathetic-adrenal medullary system. For pregnant women, the response of the heart and nervous system to stress can increase the risk of hypertension, diabetes, postpartum depression, and infection.13 For newborns, stress during pregnancy can lead to abnormal nervous system development, preterm birth, high incidence of growth restriction, and low Apgar scores after birth.14 Therefore, the mental health of pregnant women needs to be emphasized and intervened. In 2020, a study in Shanghai found that during the COVID-19 pandemic, 94.6% of pregnant women were concerned about being infected, 14.7% thought they needed psychological decompression services, and 87.7% requested “appointment services to avoid crowded places”15 In the same year, a Canadian study found that before the outbreak of the COVID-19 pandemic, pregnant women had significantly lower rates of depression, anxiety symptoms, separation symptoms, and post-traumatic stress disorder symptoms than pregnant women during the COVID-19 pandemic.16 Compared with women who were not infected with COVID-19, women with COVID-19 were more likely to have significant clinical levels of depression and anxiety symptoms.17 This suggests that COVID-19 and the changes to life had a significant impact on the emotional well-being of pregnant women.10 So the COVID-19 pandemic has increased pregnant women’s anxiety risk to some extent.
It is important to pay attention to the psychological experience of pregnant women who decided to undergo elective caesarean section with combined epidural anesthesia. Caesarean section is appropriate for pregnant women with severe complication or those who cannot give birth vaginally.18,19 Combined epidural anesthesia is often used for elective caesarean section surgery because it works quick and provides good pain relief and muscle relaxation. However, since the patient remains awake throughout the surgery, their emotional control and cooperation with preoperative anesthesia are critical to ensuring successful anesthesia and surgery.20,21 This makes higher demands on the psychological resilience of pregnant women undergoing caesarean section with lumbar spinal anesthesia compared to other surgeries.22 Nervousness and anxiety during the surgery may increase the heart rate and blood pressure, muscle tremors, and oxygen consumption of the heart muscle, which affect the surgical procedure, especially in pregnant women with complications during pregnancy.23 Anxiety and excitement can also reduce the concentration of immune factors in the blood, leading to decreased immune function after surgery and increased incidence of chronic pain.24 Also, it might increase the level of catecholamines in pregnant women, which would increase the risk of postpartum hemorrhage.25
This article aims to explore the impact of public health emergencies on the psychological experience of pregnant women and get knowledge of the recovery situation of pregnant women’s traumatic experiences due to public health infectious events, and then we hope it can lead us to provide a better nursing plan about preventive psychological care for pregnant women who choose cesarean section finally.
Methods
Study Design and Procedure
This is a cross-sectional study, which was designed to explore the anxiety situation and general well-being status of pregnant women who decided to choose Caesarean Section as their delivery mode after COVID-19 pandemic.
Study Population
This study was carried out in Shanghai first maternity and infant hospital from 10th February to 15th September 2023. The pregnant women who choose Caesarean Section would be selected to have an interview based on questionnaires. The inclusion criteria of this study population were as follows: 1) gestational weeks ≥ 37 weeks; 2) age ≥18 years old; 3) the participant informed and consented to participate; 4) the participant had normal expressive ability. Exclusion criteria were as follows: 1) the participant had serious diseases before pregnant, including physically and mentally; 2) the participant had severe pregnancy complications, including malignant hypertension, severe intrahepatic cholestasis syndrome, abruptio placentae, hyperemesis gravidarum, etc.
Ethical Considerations
This study protocol has been reviewed and approved by the Institutional Review Board of Shanghai first maternity and infant hospital (Ref. number: KS2316). The study complied with the Declaration of Helsinki. All participants will learn about the study from the informed consent and sign after agreeing to participate.
Instruments
Sociodemographic Questionnaire
This was designed by the study team, which was meant to consist of as many as possible relevant factors to the study including three parts: 1) General information: age, birthplace, live in Shanghai, education level, career, average monthly income, reimbursement for hospitalization, and live with husband most time during pregnancy. 2) Hospitalization information: gestational weeks, pregnancy order for this time, single/twin, number of abortion, cesarean section experience, surgical history, pre-pregnant health situation, pregnancy complications, Body Mass Index (BMI). 3) COVID-19 infection: The situation of COVID-19 infection and symptoms around infection.
The Generalized Anxiety Disorder Scale (GAD-7)
This questionnaire is designed to measure the level of anxiety experienced over the past two weeks. It comprises seven items, each with a four-point rating scale: 0 = not at all, 1 = several days, 2 = more than a week, 3 = nearly every day. The total scores range from 0 to 21. The questionnaire evaluates anxiety levels as follows: score 0–4 indicate no or minimal anxiety, score 5–9 indicate mild anxiety, score 10–14 indicate moderate anxiety, score 15–21 indicate severe anxiety. The Cronbach's alpha coefficient of the scale is 0.8–0.9. It can be used to measure social stress, post-traumatic stress disorder, and other conditions.26
The General Well-Being Schedule (GWBS)
This questionnaire is designed to assess an individual’s subjective sense of happiness.27 In 1996, Jianhua Duan revised the scale,28 which includes six dimensions with a total of 18 items: care for health (item 10,15), energy (item 1,9,14,17), Life satisfaction (item 6,11), pleasant environment (item 4,12,18), emotional control (item 3,7,13), relaxandtension (item 2,5,8,16). The total score range from 0 to 120, score 0–24 indicate low overall happiness, score 25–48 indicate relatively low overall happiness, score 49–72 indicate moderate overall happiness, score 73–96 indicate relatively high overall happiness, and score 97–120 indicate high overall happiness. The Cronbach’s alpha coefficient for the scale is 0.950, and the test–retest reliability is 0.850.29
Data Collection
The interview time that the study team chose was after the pregnant women admitted to hospital, and before the day of surgery, the interview place were conducted in the ward in order to ensure consistency throughout the study, the study team assign specific two persons to explain the purpose of the study, signed informed consent for the participant and help them to spent 10–15 minutes to fill out the three questionnaires. Participants self-reported general information and COVID-19 infection parts. Specific research persons filled out hospitalization information parts according to medical electronic records.
Data Analysis
Two researchers entered data into Excel 972003 and the third researcher checked the accuracy to make sure all data is right. Statistical analysis was performed by IBM SPSS Statistics version 23.0. Continuous data were presented as mean and standard deviation (mean ± SD), categorical data were presented as frequency (n) and percentage (%). For two groups comparison, if the data variance was equal, Independent t-test was used, and if not equal, the rank sum test was used. For more than two groups comparison, one-way ANOVA was used. Multiple-factor analysis was performed by generalized linear regression analysis. The significance level was set at α = 0.05, and all tests were two-sided. p ≤ 0.05 was considered statistically significant.
Results
Participant Characteristics and Description of Scale Information
Eligible 595 questionnaires were included in the study, with a mean age of 32.67 ± 3.808, ranging from 23 to 44 (Table 1). The total mean score of Generalized Anxiety Disorder Scale (GAD-7) was 4.855 ± 3.254, ranging from 0 to 18.0, which indicated no or minimal anxiety, and the mean score of General Well-Being Schedule (GWBS) was 90.699 ± 13.807, ranging from 61.0 to 120.0, which indicated indicate relatively high overall happiness. The proportion of stage scores of GAD-7 and GWBS was outlined in the context (Table 2 and Table 3).
 |
Table 1 Description and Scores of Demographic Data (n = 595) |
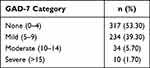 |
Table 2 The Score of Generalized Anxiety Disorder Scale (n = 595) |
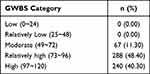 |
Table 3 The Score of General Well-Being Schedule (n = 595) |
Single Factor Analysis of the Generalized Anxiety Disorder Scale (GAD-7)
Birthplace (t = 7.287, p < 0.001), education level (p < 0.001), career (p < 0.001), average monthly income (p < 0.001), reimbursement for hospitalization (p < 0.001), live with husband most time during pregnancy (t = 11.451, p < 0.001), gestational weeks (p < 0.05), pregnancy order for this time (F = 9.012, p < 0.001), number of abortion (p < 0.001), cesarean section experience (t = −2.787, p < 0.05), pregnancy complications (t = −4.072, p < 0.001), body Mass Index (BMI) (p < 0.001). These factors above was considered statistically significant with GAD-7 (Table 1).
Single Factor Analysis of the General Well-Being Schedule (GWBS)
Birthplace (t = −9.653, p < 0.001), live in Shanghai (t = −3.900, p < 0.001), education level (p < 0.001), career (p < 0.001), average monthly income (p < 0.001), reimbursement for hospitalization (p < 0.001), live with husband most time during pregnancy (t = −4.912, p < 0.001), gestational weeks (F = 6.179, p < 0.05), pregnancy order for this time (p < 0.001), number of abortion (p < 0.001), cesarean section experience (t = 5.161, p < 0.05), pregnancy complications (t = 2.841, p < 0.05), body mass index (BMI) (F = 15.274, p < 0.001). The factors above were statistically significant with GAD-7 (Table 1).
The Results of Generalized Linear Regression Analysis of Influencing Factors of Generalized Anxiety Disorder Scale (GAD-7)
The results of the generalized linear regression analysis show that birthplace (B = −0.644), education level (B = −2.466, B = −2.532, B = −2.308), average monthly income (B = −1.603, B = −0.646), live with husband most time during pregnancy (B = −3.544), number of abortion (B = 2.202), pregnancy complications (B = 0.737). These factors above was considered statistically significant with GAD-7 (p < 0.05) (Table 4).
 |
Table 4 Generalized Linear Regression Analysis of Influencing Factors of Anxiety (GAD-7) |
The Results of Generalized Linear Regression Analysis of Influencing Factors of General Well-Being Schedule (GWBS)
The results of the generalized linear regression analysis show that birthplace (B = 5.074), live in Shanghai (B = 6.581), average monthly income (B = 5.857, B = 10.718), reimbursement for hospitalization (B = 4.208), pregnancy order for this time (B = −4.702), number of abortion (B = −5.420), pregnancy complications (B = −2.609), body mass index (B = 3.423). These factors above were statistically significant with GWBS (p < 0.05) (Table 5).
 |
Table 5 Generalized Linear Regression Analysis of Influencing Factors of General Well-Being Schedule (GWBS) |
Discussion
This study investigated the mental status of pregnant women who decided to choose Caesarean Section as their delivery mode after COVID-19 epidemics in Shanghai, China. Among the 595 questionnaires, 92.6% participants stated they had no and mild generalized anxiety, and 88.7% participants have relatively high level of general well-being feeling.
Our generalized linear regression analysis revealed several factors were statistically significant with Generalized anxiety disorder, including birthplace, education level, average monthly income, live with husband most time during pregnancy, number of abortion and pregnancy complication. However, the factors that affect general well-being status were slightly different, including birthplace, live in Shanghai, average monthly income, reimbursement for hospitalization, pregnancy order for this time, number of abortion, pregnancy complication, Body Mass Index (BMI).
Common factors with significant differences between the two scales including birthplace, average monthly income, number of abortion and pregnancy complication.
The birthplace in Shanghai was negative related with anxiety and positively correlated with general wellbeing. The factors affecting happiness include external environmental factors and internal factors. External environmental factors including economic environment, institutional environment, cultural and social environment. Internal factors refer to a series of joyful and pleasant emotions based on people‘s sense of satisfaction and security. Shanghai is China‘s municipality. Its geographical location is superior, urban planning is pleasant, historical and cultural diversity, social atmosphere is more open, democratic, which made a strong social security and economic growth for them.30,31 The increasingly sufficient material conditions also make the Shanghai people pay more attention to the improvement of spiritual life and pay more attention to explore the meaning of life, have more hobbies and wider interests in life. Moreover, local residents have more relatives, wider interpersonal relationships.32 These are why the local people have higher happiness and less anxiety level than non-locals above so does the people live in Shanghai.
Average monthly income was negatively related to anxiety and positively correlated with general wellbeing. Family social economy is one of the important factors affecting maternal anxiety. Studies33,34 showed that external stimuli cannot have a direct impact on individuals under normal circumstances, while anxiety is perceived by their self-system feedback. The internal cognize plays a decisive role. The higher family‘s social and economic status is, the more support and resources during pregnancy they would get, which makes the pregnant women see themselves more confident and positive. On the contrary, pregnant women with lower monthly family income have less resources but also face more risks and challenge.
More abortions made higher anxiety and lower happiness. There was a statistically significant difference in anxiety between pregnant women with abortion ≥3 times and pregnant women without abortion experience. With the opening of sexual concepts, environmental pollution and other factors, the rate of repeated abortion has been on the rise recently. The main causes of abortion include the mother‘s own reluctance to continue pregnancy, and some diseases makes it inappropriate to continue pregnancy. At present, painless abortion is used clinically to terminate pregnancy. Although most of the operations can be carried out smoothly and safely, the complications caused by the operation, such as pelvic inflammatory disease, intrauterine adhesions and placental implantation will threaten the safety of mother and fetus during pregnancy in the future.35,36
Pregnancy complications were positively correlated with anxiety and negatively correlated with general well-being. Pregnancy is a special physiological process. On the one hand, it will cause physiological changes in pregnant women37 such as cardiovascular disease, physiological anemia, gestational diabetes mellitus, gestational hypertension, kidney infection, immune system disorder, and so on. These physiological changes will affect the psychological experience and emotions of pregnant women. Long-term continuous tension and changes in living habits will reverse the body. For example, the uterine artery resistance index is positively correlated with the anxiety score. The resistance of the uterine artery to blood flow is enhanced, and the fetus is prone to intrauterine growth and preeclampsia.38
The higher education level, the less anxiety. The higher education level determines the wider range of thinking, the longer field of vision, the larger controllable space, and the advantages and disadvantages of thinking way from multiple dimensions.39,40 They are willing and able to learn about pregnancy knowledge in many ways, such as indications for cesarean section, main points of observation in perioperative period and care of newborns, and also they will find ways to get comfort and support from family and society to make themselves to cope with physiological and physical changes during their pregnancy. Although some studies have pointed out that people with master’s degree or above have higher self-definition and demands on the outside world and are prone to have mental illness, the proportion of people with higher education included in this study is low, which has not proven it.41
The anxiety level of pregnant woman living with their spouse for a long time during pregnancy was significantly lower than that of pregnant woman separated from their spouse. Pregnant women‘s body shape, body hormone changes, role changes, and concerns about maternal and fetal safety in the middle and late stages of pregnancy can easily aggravate anxiety and depression. Family support is a key factor in the process of maternal perinatal role change adaptation.42 On the one hand, good family support provides protection for pregnant women under stress, and on the other hand, it can improve the stress ability of pregnant women in the face of major events, helping them to control emotions. The spouse gradually accepts the role change with the pregnant woman through the companionship of the pregnant woman throughout the pregnancy. The spouse actively care for and help the pregnant woman to share the pressure, become the dependence of the pregnant woman, meet the needs of love and belonging in the emotional needs of the pregnant woman, help to regulate the emotions of the pregnant woman, and bring positive effects.43
Reimbursement for hospitalization is one of the factors that affect the happiness of pregnant women. The survey showed that there was a significant difference in happiness between pregnant women at their own expense and those with medical insurance. There are two kinds of own expense ways in our hospital. One is pregnant women who choose to stay in VIP ward for delivery, and the other is pregnant women who come to Shanghai for medical treatment without local medical insurance. Their common point is that pregnant women and their families are willing to choose institutions with more comfortable conditions and more reliable quality of diagnosis and treatment and are willing to bear the costs. The VIP wards in our hospital are set up to meet the high-demand patients. The ward environment is beautiful, and the medical staff also have more time to provide patients with more high-quality, efficient and personalized nursing services. With such a nursing care, the puerpera can enjoy more comprehensive car.44,45 Feeling a pleasant environment and all-round patient care during hospitalization are also one of the important factors to enhance happiness. For pregnant women who have come to Shanghai for medical treatment and delivery, they chose our hospital among comparison of several hospitals. During the whole process of prenatal examination during pregnancy, the communication with doctors and the understanding of the disease are also constantly improving. From successful conception to full-term delivery, the correctness of this choice and the increase of trust are also the main factors of high happiness.
In addition, the impact of the COVID-19 epidemic on maternal anxiety and general well-being was also included, and the results showed no statistical difference. It shows that although the prevention, control and regulation during the epidemic have affected people‘s living environment and habits and people‘s material and spiritual needs have not been balanced and met for a certain period of time, the resilience of pregnant women after this public health event was still good, which does not affect the degree of anxiety and happiness.
The Clinical Implication of This Study
This study allows us to understand the psychological status of pregnant women undergoing elective cesarean section and the influencing factors of anxiety and general well-being. This study provides guidance to the improvement of clinical work in the future; based on the results, we can imagine improving patients’ knowledge of cesarean section, extending perioperative family time, and improving communication skills and nursing behaviors to build a good relationship with patients were good choices to improve patients’ cooperation and psychological preparation during perioperative cesarean section, reduce physical discomfort caused by tension and anxiety, and increase patients’ happiness during childbirth. Moreover, this study is more conducive to the career development of our operating room nurses. It makes up for the part of patient psychological care where we have little contact with patients, and made us pay attention to the underlying psychological state of patient, evaluating the patient’s situation from multiple dimensions, and assisting doctors and patients to communicate and make appropriate decisions.
Limitations
This study has limitations in research design and methodology. Firstly, this study was conducted in a single center in Shanghai. Although the sample size was large, the results only represent the psychological status of pregnant women undergoing elective cesarean section in one obstetrics and gynecology hospital in Shanghai; it was not a multi-center study, so the reliability of the results is not strong, which cannot reflect in national level. Secondly, the study was a cross-sectional study in a group of people which use single-factor analysis and generalized linear regression analysis as statistical methods, lacking horizontal control so does the statistical method is simple. Thirdly, the purpose of this study was to explore the psychological state of pregnant women after the COVID-19 epidemic, and we chose GAD-7 and GWBS as our study questionnaires.
Now, we have a preliminary understanding of the general situation from the results of this study. Considering the limitations above, we will make the following changes in the future research. Firstly, we conducted a longitudinal study, setting up different follow-up time points during pregnancy to explore the psychological changes at different times during pregnancy. Secondly, based on the current results, a randomized controlled study will be conducted to compare the results after the implementation of intervention programs among different groups to explore the impact of different nursing programs on pregnant women’s psychology. Thirdly, we can further understand the maternal psychological questionnaire and increase the investigation dimension of psychological state. In addition, we can also carry out multiple forms of research, such as qualitative interviews based on the influencing factors of the current results, in order to relieve the anxiety of pregnant women.
Conclusion
The study showed that the COVID-19 infection status and symptoms around infection have no statistical difference in anxiety level and general well-being after they experience the COVID-19 pandemic. However, through cross-sectional study, we knew the psychological and emotional status and their impact factors of the women who chose cesarean section delivery in our hospital. In the future, we will expand the sample size to explore the different situation of multi-center. We hope to provide psychological nursing interventions based on existing results to give them a better delivery experience.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study has no funding assistance.
Disclosure
Chunye Dai and Xuelu Wang are co-first authors for this study. The authors report no conflicts of interest in this work.
References
1. Chew NWS, Lee GKH, Tan BYQ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID‑19 outbreak. Brain Behav Immun. 2020;88:559–565. doi:10.1016/j.bbi.2020.04.049
2. Li Z, Ge J, Yang M, et al. Vicarious traumatization in the general public, members, and non‑members of medical teams aiding in COVID‑19 control. Brain Behav Immun. 2020;88:916–919. doi:10.1016/j.bbi.2020.03.007
3. Schwatz DA, Grahan AL. Potential maternal and infant outcomes from coronavirus 2019-nCoV (SARS-CoV-2) infecting pregnant women: lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020;12(2):194. doi:10.3390/v12020194
4. Purgato M, Gastaldon C, Papola D, et al. Psychological therapies for the treatment of mental disorders in low- and middle-income countries affected by humanitarian crises. Cochrane Database Syst Rev. 2018;7(7):CD011849. doi:10.1002/14651858.CD011849.pub2
5. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi:10.3390/ijerph17051729
6. The Joint Prevention and Control Mechanism Comprehensive Group. The joint prevention and control mechanism comprehensive group of the state council for novel coronavirus infection, on the issuance of the overall plan for the implementation of “Class B and B Management” for novel coronavirus infection, joint prevention and control mechanism comprehensive [2022] No. 144; 2022.
7. The latest! Experts: the epidemic in Beijing and other places is coming to an end. Available from: https://m.163.com/dy/article/HQ02SPG00519D3V1.html.
8. Zambrano LD, Ellington S, Strid P, et al. Update: characteristics of symptomatic women of reproductive age with LaboratoryConfirmed SARS- CoV-2 infection by pregnancy status — United States, January 22- October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1641–1647. doi:10.15585/mmwr.mm6944e3
9. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi:10.1016/S0140-6736(20)30460-8
10. Salem D, Katranji F, Bakdash T. COVID-19 infection in pregnant women: review of maternal and fetal outcomes. Int J Gynaecol Obstet. 2021;152(3):291–298. doi:10.1002/ijgo.13533
11. Lebel C, MacKinnon A, Bagshawe M, et al. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. 2020;277:5–13. doi:10.1016/j.jad.2020.07.126
12. Lee DT, Sahota D, Leung TN, et al. Psychological responses of pregnant women to an infectious outbreak: a case-control study of the 2003 SARS outbreak in Hong Kong. J Psychosom Res. 2006;61(5):707–713. doi:10.1016/j.jpsychores.2006.08.005
13. Street ME, Bernasconi S. Endocrine-Disrupting Chemicals in Human Fetal Growth. Int J Mol Sci. 2020;21(4):1430. doi:10.3390/ijms21041430
14. Cardwell MS. Stress: pregnancy considerations. Obstet Gynecol Surv. 2013;68(2):119–129. doi:10.1097/OGX.0b013e31827f2481
15. Du L, Gu YB, Cui MQ, et al. Investigation on demands for antenatal care services among 2002 pregnant women during the epidemic of COVID-19 in Shanghai. Zhonghua Fu Chan Ke Za Zhi. 2020;55(3):160–165. Chinese. doi:10.3760/cma.j.cn112141-20200218-00112
16. Berthelot N, Lemieux R, Garon-Bissonnette J, et al. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet Gynecol Scand. 2020;99(7):848–855. doi:10.1111/aogs.13925
17. Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi:10.1016/j.jaut.2020.102433
18. Yaofen S, Qiuyuan H, Yang M. Effects of Family Collaborative nursing Model on delivery outcome and postpartum recovery of primipara. J Adv Nurs. 2016;31(5):4. doi:10.16821/j.cnki.hsjx.2016.05.023
19. Shao H, Jin Y, Fang S, et al. Analysis of Influencing Factors on Cognition and choice of delivery mode in patients with cicatricial uterus repregnancy. Nurs Rehabil. 2017;16(8):4. doi:10.3969/j.issn.1671-9875.2017.08.006
20. Huang L, Wenjing L, Yang W, et al. Analysis on the Clinical Problems of older childbearing after the universal two-child Policy. Chin Mater Child Health Res. 2017;28(12):1780–1782. doi:10.3969/j.issn.1673-5293.2017.12.090
21. Xiao Q, Chen Q, Zheng Y. Analysis of influencing factors of cesarean section after the implementation of “two-child policy”. Pract Prevent Med. 2018;25(6):3.
22. Li C. Application value of lumbar puncture and epidural anesthesia in different parts of cesarean section. Med Theory Pract. 2023;36(07):1177–1179. doi:10.19381/j.issn.1001-7585.2023.07.035
23. Tang S, Hu H, Wan Z. Effects of combined epidural anesthesia on serum LncRNA FOXD2-AS1 miR-206 and inflammatory cytokines in pregnant women who were delivered by cesarean section with hypertensive diseases. Mater Child Health Care Chin. 2022;37(21):3929–3932. doi:10.19829/j.zgfybj.issn.1001-4411.2022.21.014
24. Jie M. Application effect and safety of combined lumbar and epidural anesthesia in elderly primipara cesarean section. Clin Med (Northfield Il). 2022;42(07):38–40. doi:10.19528/j.issn.1003-3548.2022.07.013
25. Wang Y, Liu J, Tian W. Effect of epidural anesthesia and combined lumbar epidural anesthesia in cesarean delivery and hemodynamic analysis. Syst Med. 2022;7(19):79–82. doi:10.19368/j.cnki.2096-1782.2022.19.079
26. Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
27. Fazio AF. A concurrent validational study of the NCHS general well-being schedule. Vital Health Stat. 1977;2(73):1–53.
28. Duan JH. The trial results and analysis of the overall wellbeing scale in Chinese college students. Chin J Clin Psychol. 1996;4(1):56–57.
29. Meng Y, Zhang X, Zhang X. Analysis of influencing factors of subjective well-being of nurses of different nursing ages in general surgery based on partial correlation and structural equation model. Hebei Pharmaceut. 2016;38(023):3654–3657. doi:10.3969/j.issn.1002-7386.2016.23.042
30. Qun ZCC. Vice mayor of shanghai: actively promoting the construction of high-level learning city. Shanghai Educ. 2021; 34:16.
31. Wang Y, Zhang J, Yu H. The effect of health status on social support and subjective well-being of floating population in shanghai. Med Soc (Berkeley). 2021;34(11):83–86. doi:10.13723/j.yxysh.2021.11.017
32. Ma S. Promote economic and social development, improve people’s happiness index. Qilian Mountain News. 2023. doi:10.28628/n.cnki.nqlsb.2023.000083
33. Almeida-Filho N, Lessa I, Magalhães L, et al. Social inequality and depressive disorders in Bahia, Brazil: interactions of gender, ethnicity, and social class. Soc Sci Med. 2004;59(7):1339–1353. doi:10.1016/j.socscimed.2003.11.037
34. Yesiltepe D, Pepping R, Ling FCM, et al. A tale of two cities: understanding children’s cycling behavior from the socio-ecological perspective. Front Public Health. 2022;10:864883. doi:10.3389/fpubh.2022.864883
35. Zhang Y, Chen H, Liu Y. Safety analysis of different aged pregnant women under the new birth policy. Chin General Med. 2023;21(04):629–631+636. doi:10.16766/j.cnki.issn.1674-4152.002947
36. Tang X, Zhu Y, Wang Z, et al. Analysis of Factors related to postpartum hemorrhage in women with placenta previa. Advan Mod Obstet Gynecol. 2023;32(02):118–122. doi:10.13283/j.cnki.xdfckjz.2023.02.006
37. Fei Y. Analysis of perinatal hematological test index and pregnancy outcome of elderly and eligible pregnant women. Med Inform. 2017;30(2):2. doi:10.3969/j.issn.1006-1959.2017.02.201
38. Zoli SI, Baiti MA, Alhazmi AA, et al. Factors affecting awareness of pregnancy screening for group B streptococcus infection among women of reproductive age in Jazan Province, Saudi Arabia. J Multidiscip Healthc. 2023;7(26):2109–2116. doi:10.2147/JMDH.S421412
39. Dubber S, Reck C, Müller M, et al. Postpartum bonding: the role of perinatal depression, anxiety and maternal-fetal bonding during pregnancy. Arch Womens Ment Health. 2015;18(2):187–195. doi:10.1007/s00737-014-0445-4
40. Huang X, Yang J, Liu Y, et al. The Effects of Anxiety and depression and life events on pregnancy outcomes in pregnant women. J Med Coll Qingdao Univer. 2016;52(1):21–24. doi:10.13361/j.qdyxy.201601008
41. An L, Yeh KC, Liu Y, et al. An online structured diabetes self-management education and support programme improves glycaemic control in young adults with type 1 diabetes. J Multidiscip Healthc. 2023;16(9):2641–2654. doi:10.2147/JMDH.S414102
42. Sahin E, Seven M. Depressive symptoms during pregnancy and postpartum: a prospective cohort study. Perspect Psychiatr Care. 2019;55(3):430–437. doi:10.1111/ppc.12334
43. Karaçam Z, Çoban A, Akbaş B, et al. Status of postpartum depression in Turkey: a meta-analysis. Health Care Women Int. 2018;39(7):821–841. doi:10.1080/07399332.2018.1466144
44. Stokke R, Wibe T, Sogstad M. Forming nursing home practices that support quality of care for residents. A qualitative observational study. J Multidiscip Healthc. 2023;16(9):2667–2680. doi:10.2147/JMDH.S426913
45. Shen L, Hon Y, Hu Y. Construction of hospital management culture based on the concept of value transfer. J Tradit Chin Med Manag. 2021;29(12):238–239. doi:10.16690/j.cnki.1007-9203.2021.12.115
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
