Back to Journals » Risk Management and Healthcare Policy » Volume 16
A Study on Influencing Factors of Physicians’ Suboptimal Health Status in Primary Healthcare Institutions
Received 17 May 2023
Accepted for publication 4 July 2023
Published 6 July 2023 Volume 2023:16 Pages 1241—1257
DOI https://doi.org/10.2147/RMHP.S417277
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Haotao Li, Yuankai Huang,* Xiaoyu Xi*
The Research Center of National Drug Policy & Ecosystem, China Pharmaceutical University, Nanjing, 211198, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yuankai Huang; Xiaoyu Xi, The Research Center of National Drug Policy & Ecosystem, China Pharmaceutical University, Nanjing, 211198, People’s Republic of China, Tel +86 134-0414-2338 ; +86 138-5229-7573, Email [email protected]; [email protected]
Purpose: This study aims to investigate the current health status of Chinese physicians in primary healthcare institutions (PHI) and the effects of personal characteristics, lifestyle, work-related environment and life-related environment on the subhealth status (SHS) of them.
Methods: A conceptual framework of various influencing factors was constructed with reference to the concept of health-related quality of life before the convenience sampling. Self-administered questionnaires are distributed to acquire the cross-sectional information of nationwide PHI physicians. A logit regression model was constructed to investigate the influence of various factors on the SHS of PHI physicians.
Results: Among 682 valid cases included in the logit regression, 457 physicians were in SHS, with an SHS rate of 67%. The regression results (R2=0.3934, chi-square=337.07, p< 0.0001) showed that long working hours (p< 0.05), personal income (p< 0.05) and life stress (p< 0.05) were protective factors for subhealth. The frequency of alcohol consumption (p< 0.01), smoking (p< 0.05), fear of making mistakes at work (p< 0.001), tension with colleagues (p < 0.0001), and job satisfaction (p < 0.05) were all risk factors. Other factors such as education (p < 0.1) also had an effect on the SHS of primary care physicians.
Conclusion: A large proportion of PHI physicians in China are in SHS and many of them are not aware that they are in a poor health state. The logit regression model showed that factors including worries about the occurrence of accidents, strained relationships with colleagues, job satisfaction, and frequency of smoking and drinking negatively influence the SHS of PHI physicians, which should be paid more attention. Meanwhile, annual personal income, long working hours and life stress are protective factors, which means that these factors need to be encouraged.
Keywords: physician, primary healthcare institution, sub-optimal health, influencing factors, China
Introduction
The WHO Charter, proposed at the time of its establishment in 1948, defines health as a favorable state in physical, mental and social dimensions instead of just being away from physical defects and diseases. And between the healthy state and the disease state, another state exists called the subhealth state.1 Subhealth is a state of reduced vitality and reduced functional and adaptive capacity for a certain period of time.2 And if not managed in time, the body may develop further into a disease state due to the long-term low quality of health.3 Current research suggests that sub-health status (SHS) can be used to measure the health status of a population and prevent the occurrence of disease.4 In China, studies have been conducted on SHS of hospital personnel, community health workers, midwives, civil servants and university students.5–9 Internationally, studies have been conducted on the SHS of pregnant women, young people and university students.10–12 In all the mentioned studies, the SHMSV1.0 scale is the most commonly used instrument to measure SHS and the influencing factors are various for the different characteristics of different occupations, however, variables like exercising frequency, diet condition and eating condition are frequently mentioned in studies. Besides, studies have also shown that subhealth is significantly associated with the shortening of chromosomal telomeres, which can be used as a predictor of physiological aging.13 There is also a study combining SHS with indicators of endothelial dysfunction to predict the risk of cardiovascular disease.14 However, there are no studies on the SHS of physicians working in PHI.
Primary healthcare institutions (PHI) are the basic units of China’s three-tier healthcare system, which includes community health service stations, street health centers, township health centers, village health offices, outpatient clinics and clinics (infirmaries), accounting for more than 93% of the total number of health care institutions.15 PHIs are responsible for basic health care services such as medical treatment, maternal and child health care, health education, and infectious disease prevention, control and reporting. By the end of November 2021, China had 978,000 primary care institutions. However, China’s primary care physicians still have a heavy task and are under tremendous pressure due to China’s large population and the huge gap in per capita medical resources compared to developed countries. In 2013, the concept of “hierarchical medical system” was proposed by the central committee to regulate the conflicts between the service pressure of hospital and people’s tendency to seek medical treatment, solve the problem of insufficient utilization of primary hospitals and improve the two-way referral collaboration among medical institutions, which further increased the pressure on the medical personnel in PHIs.16 Physicians in PHIs, facing patients, often require more meticulousness and attention than other occupations. In the context of COVID-19, the intensity of their work increases the possibility to feel tired, nervous and other emotions related to SHS. The SHS of PHI physicians in China requires urgent attention.
By studying the SHS of PHI physicians, we can have an overview of the proportion of them in SHS and better understand the complexity of the working environment and the enormity of the work pressure of PHI physicians by comparing the SHS of PHI physicians with the SHS of all physicians or other groups. Improvement measures can be proposed to prevent the health condition from deteriorating or even turning into a disease state.
In terms of public health care, in addition to continuously improving the number of PHIs and physicians and strengthening the equipment level of hardware facilities, it is imperative to stabilize and strengthen the current service protection capacity of the PHI physicians. The health level of PHI physicians affects their working hours and efficiency. And physicians in a healthy state can avoid absenteeism due to illness and provide efficient treatment for patients. This study collects data to find out the SHS level of PHI physicians in the context of COVID-19 in China and further investigates the influencing factors affecting the SHS of PHI physicians to provide scientific guidance for the relevant departments to take corresponding intervention measures for high-risk groups. This study also has certain significance for the optimization of service quality in PHIs, the prevention of physicians’ health problems, and the promotion of group health levels.
Conceptual Framework
Health-related quality of life is similar to the concept of subhealth, which can be converted to scores according to the scales to judge whether a person is in good condition.17 These two concepts can also both be divided into several dimensions for comprehensive evaluation. The dimensions of health-related quality of life include the physical, psychological and social dimensions of subhealth. Therefore, this study tries to establish a model of the influencing factors of subhealth based on the study related to health-related quality of life. As the work content and nature of PHI physicians is special and the concepts of subhealth and health-related quality of life are not identical, this study attempted to adapt the original model to suit this study for measuring physicians’ subhealth. This study used a self-administered questionnaire to solicit experts’ opinions on the model revision by single expert consultation method. There are eight PHI physicians with clinical practice experience and eight experts with research experience about physicians. The questionnaire was consisted of two questions: 1. whether you think the original model is applicable to this study; 2. if not, which part is not applicable and how it should be revised. This study employed a stratified interview method. Three of each group revised the first tier of influencing factors that directly affect subhealth and the remaining experts revised the second tier of influencing factors. The final model of the influencing factors of physicians’ SHS in PHI was determined. In this study, the influencing factors were also divided into two types: personal and environmental. The personal-related factors were divided into personal characteristics, living habits and work condition; the environmental-related factors were divided into social condition and material conditions. According to previous analyses, this study also included the following factors: gender, age, education, BMI, marital status, smoking frequency, drinking frequency, number of children, diet, exercise frequency, breakfast eating condition, number of personal hobbies, household location, interpersonal relationships, stress management, personal and family income, work environment satisfaction, long working hours, and health insurance coverage.2,18–27 In addition, this study included the employment form, stressful feelings of worrying about work accidents, whether the elder or children need care, and work and life stress according to the framework of influencing factors and the work characteristics of PHI physicians. The inclusion reasons are as follows. PHI physicians are generally divided into permanent workers and contract workers and permanent staff usually have higher salaries and job stability, which may contribute to higher quality of life and job satisfaction. Therefore, this study included the influencing factor of work type. PHI physicians are mainly 30–50 years old, which generally bear the responsibility of raising children and caring the elderly. The high life and work stress affect subhealth level. Therefore, whether the elderly or children need care, work pressure and life pressure were included. Since the work of PHI physicians is closely related to the health level of local residents and work mistakes can cause serious consequences, the fear of work accidents occurring was included. According to the characteristics, the influencing factors were categorized according to the theoretical framework (see Figure 1 and Table 1).
 |
Table 1 An Overview of Variables |
 |
Figure 1 The conceptual model of influencing factors of SHS (sub-optimal health status). |
Personal-Related Factors
Personal characteristics include three categories, namely, basic information, life habits and work condition. Basic information includes gender, age, BMI and diploma. Life habits include work and rest condition, dietary regularity, breakfast eating frequency, exercise frequency, smoking frequency and drinking frequency. Work situation includes frequency of long working hours, work experience, form of employment, and stress of worrying about accidents.
Environment-Related Factors
Environmental characteristics include two major categories: social relations and material conditions. Social relationships include marital status, number of children, relationships among colleagues, the number of elderly or children in need of care, and work and life stress. Material conditions include annual personal and family income, type of household registration, type of basic health insurance, and whether or not one participates in commercial health insurance.
Materials and Methods
Participants
To carry out a nation-wide study, the targeted population was PHI physicians in China. And only cases in physically healthy condition in the sample were included in the analysis. This study employed convenience sampling method and contacted PHIs across China that were easily accessible and not affected by the COVID-19 by telephone. Managers in institutions that agreed to participate recommended physicians. Potential respondents were contacted by telephone by the investigator to explain the purpose and content of the study and to ask for basic information about the respondents to ensure that they met the inclusion criteria. Ultimately an interview list of approximately 800 respondents was formed. The minimum sample size in this survey was calculated from Raosoft calculation.28 663 participants was needed to meet the estimated size of 479,000 with the setting of a 99% confidence level, ±5% margin of error, and 50% response distribution.29 As 682 physicians are included in the analysis, the response rate of the convenience sample exceeded that required for this analysis. Cities with more than 25 respondents were included and the inclusion and exclusion criteria of respondents are as follows.
Inclusion criteria: 1. Physicians in PHIs such as grassroots community health service centers that provide medical, preventive, health care, and rehabilitation services to their jurisdictions; 2. Physicians who were willing to accept the survey and filled out an informed consent form.
Exclusion criteria: 1. Those who had worked in their units for less than 1 month; 2. Those who suffering from acute or chronic diseases, major organic diseases or psychological diseases; 3. Those who scored as sick on the total subhealth score and scores from subscales. 4. Those whose questionnaire results with logical errors (eg contradictions in the number of children and children who need to go to school, personal income > family income), omissions, or indiscriminate answers are excluded.
Data Collection
From August to September in 2021, 60 trained researchers were sent to the research cities, collecting at least one questionnaire from each PHI. The researchers were also responsible for the neighboring cities. Researchers used cell phones or table computers to open the online survey system with respondents filling out the questionnaire and submitting it under the guidance of the researcher. During the research process, the researcher is not allowed to provide any comments about the questionnaire except the requirements or instructions for filling out the questionnaire. The researcher did not collect information outside of the questionnaire to ensure the anonymity of all respondents during the research process. After the questionnaires were completed, the results were recorded in the survey system and converted into electronic data, which were eventually uploaded to the database system by the researcher. To ensure the quality of the research, two data auditors were recruited to review the uploaded questionnaires in real-time. When there were data errors or data corruption problems, the auditors immediately contacted the researcher by phone to inform the problem and asked the researcher to make a return visit.
In order to ensure the sample size is enough, the researcher can contact other respondents who meet the criteria according to the convenience sampling principle or snowball recommendation if the respondents of an organization cannot participate in the research process. If the total number of respondents in a city does not meet the requirements, the researcher can communicate with the research designer, who will contact neighboring cities and dispatch the researcher to conduct a new survey after determination. By the sampling methods above, 537 medical institutions from all 31 provincial administrative units in mainland China were selected in this survey. Hong Kong, Macau, and Taiwan were excluded because the public health system of these three provincial administrative regions is distinctively different from the system applied in mainland China.
Research Instrument
In this study, a self-administered questionnaire called the Sub-Health Measurement Scale V1.0 (SHMS V1.0) designed by Xu Jun et al was used to measure the SHS of the population, which contains three subscales of physical sub-health (PS), mental sub-health (MS), and social sub-health (GS) and general item of sub-health (GS).18,30 The scale has nine dimensions: physical symptom, organic function, physical mobility function, vitality, positive emotion, psychosocial symptom, cognitive function, social adaptability, social resource and social support, containing 39 questions. The SHMS V1.0 is a 5-level Likert scale and all items except the overall self-assessment items can be summed up. The SHS is judged by the subhealth normative criteria divided by different genders and age groups.31 According to the scores of the total scale and the physical, psychological and social subscales, the body states are classified as disease, severe subhealth, moderate subhealth, mild subhealth and healthy in descending order. The validity and reliability of this scale have been tested and validated.32
Data Analysis
In this study, logit regression was performed using StataMP 17 to analyze the effect of each influencing factor on the total subhealth score. In order to further investigate in what ways each influencing factor affects the SHS of PHI physicians and to verify whether the influencing factor that is significant for the main scale score can also be significant for each subscale score, we further constructed a logit regression model using the subscales’ score as the dependent variable. In order to better analyze the influence of each factor on SHS, the total subhealth score and subscales’ scores were processed to reduce dimensions as follows.
Subhealth score: According to the normative study of subhealth scale, the disease population in the total scale and three subscales were excluded. The group scoring high was classified as a healthy population, while the mild, moderate and severe subhealth population was uniformly classified as the SHS population. Therefore, the original continuous numerical variables were processed into dichotomous variables measuring whether they were in SHS or not.
In this study, the regression results were tested for collinearity and robustness, respectively. Collin’s instruction showed that the average VIF value was 1.72 and the VIF values of all 32 explanatory variables were less than 5 with the tolerance value bigger than 0.1, therefore, there was no significant collinearity between the explanatory variables; Robust analysis is detailed in 3.4.
Results
There are 804 complete, error-free, and authentic questionnaire records from PHI physicians, among which 40 physicians self-reporting a disease and 82 cases of disease groups with low scores on the Subhealth Scale were excluded. Finally, 682 PHI physicians who reported that they were healthy were included in the analysis.
Demographic Characteristics
The mean age of the subjects was 40.53±8.68 years (see Table 2). The mean personal income was 8.2±4.96(w). The mean annual family income was 17.01±15.99(w). The gender ratio was relatively balanced (n=344,50.44%) and they are almost all married (n=612,89.74%). They mainly obtained college and bachelor degree (n=198, 29.03%; n=351, 51.47%) and their titles were mainly primary and intermediate (n=279, 40.91%; n=279, 40.91%).
 |
Table 2 Demographic Characteristics of Participants |
Descriptive Analysis
According to the descriptive analysis, there are more people in SHS in the younger group. Except for the group of 20–29, among which the subhealth rate in social dimension was lower than the subhealth rate in mental health, the subhealth rate in social dimension was higher than the rate in physical dimension and the mental dimension in all other age groups (see Table 3).
 |
Table 3 Results of the Descriptive Analysis of the Participants |
Regression Analysis
All variables in the conceptual model are considered to explore their relationships with SHS of PHI physicians (see Table 4). If the odds ratio (OR) of a variable is bigger than 1, this variable is a risk factor for SHS, otherwise, it is a protective factor.
 |
Table 4 Results of the Logistic Multivariate Regression Between the Variables and Total SHS Score |
Protective Factors
Protective factors for SHS of PHI physicians in China were annual personal income, long working hours and life stress. The odds ratio (OR) decreased to 0.904 (95% CI 0.823 to 0.993; p<0.05) for every 10,000 increase in annual personal income compared to the subhealth rate before the occurrence. The OR decreased to 0.229 (95% CI 0.058 to 0.903; p < 0.05) for 6–7 days a week working more than 10h compared to 0–1 days a week working more than 10h. The OR was reduced to 0.229 (95% CI 0.058 to 0.903; p < 0.05) with relatively high life stress compared to no life stress.
Risk Factors
Risk factors for sub-health conditions among PHI physicians in China were worries about the occurrence of accidents, strained relationships with colleagues, job satisfaction, and frequency of smoking and drinking. The OR increased to 3.59 (95% CI 1.85 to 6.96; p < 0.001) for occasional fear of work-related accidents compared to never fearing work-related accidents. The OR increased to 3.047 (95% CI 1.81 to 5.14; p<0.0001) for rarely having tension with coworkers compared to never having tension with co-workers. The OR increased to 4.04 (95% CI 1.27 to 12.81; p<0.05) for generally satisfied with the work environment compared to very dissatisfied with the work. The OR of occasional drinking increased to 2.13 (95% CI 1.20 to 3.77; p<0.05) compared to never drinking; p<0.01). The OR increased to 2.27 (95% CI 1.01 to 5.08; p < 0.05; p < 0.05) for occasional smoking compared to never smoking.
Robust Analysis
To verify the results of the logit model constructed by the variables and the total score of the scale, another three logit models are constructed by the variables and the scores of three sub-scales, namely, physical sub-health scale, mental sub-health scale and social sub-health scale (see Table 5).
 |
Table 5 Results of the Logit Regression of the Score of Sub-Scales and Variables |
In the subscale of physical health dimension, worries about the occurrence of accidents and tension with co-workers were risk factors, which were consistent with the results of the scale’s total score; in the subscale of psychological health dimension, the protective factors consistent with the results of the scale’s total score were personal annual income and long working hours with the risk factors of job satisfaction, worries of the occurrence of accidents, tension with co-workers, and frequency of drinking. In addition, the psychological subhealth subscale also indicated that the protective factors for psychological subhealth also include marital status and exercise frequency and the risk factors also include work stress and whether children were under pressure for further education and employment. In the social subhealth subscale, the protective factors supporting the result of the total score were long working hours and the risk factors were job satisfaction and worries of the occurrence of accidents. In addition, the subscales of social dimension indicated that the protective factors of social subhealth also include the number of hobbies, the type of health insurance and whether have purchased commercial insurance and the risk factors also include title and household registration. Seven of the eight influencing factors significant in the results of main score also appeared in the subscale regressions with same direction of influence. The influencing factor of worries of the occurrence of accident appeared in all three regressions of subscales. The results of the robustness analysis further validated the results of the regression analysis and explored the significant factors affecting each subscale to provide a reference for targeting the improvement of the subhealth condition of a specific group.
Discussion
This study investigated the current SHS of PHI physicians and the relationship between their subhealth levels and various influencing factors. The results of regression analysis showed that eight influencing factors had a significant effect on the level of subhealth, namely, annual personal income, long working hours, life stress, worries about the occurrence of accidents, tension with colleagues, job satisfaction, and frequency of smoking and drinking (see Figure 2). Among them, the effects of long working hours, life pressure and job satisfaction on subhealth are contrary to our perception, which will be discussed and analyzed combined with the extant literature.
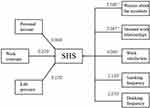 |
Figure 2 An influencing model of SHS (sub-optimal health status). Notes: *p<0.1; **p<0.05; ***p<0.01. |
May Long Working Hours Energize the Chinese Physicians?
The analysis showed that the OR of subhealth decreased to 0.295 (p < 0.05) when working more than 10h for 6–7 days per week compared to 0–1 days per week and to 0.568 (p < 0.1) when working more than 10h for 4–5 days per week compared to 0–1 days per week. We generally believed that the longer the working hours, the worse the physical condition. And there are existing studies on the effect of long working hours on subhealth both supporting and objecting to the results of this study.33–38 The work specificity of PHI physicians may contribute to this result. The unique culture and education in China praising hard work, efforts and dedication and the status of physicians offer PHI physicians a different identity from other professions. Long working hours will certainly cause physical and mental fatigue, however, the psychological achievement of self-realization will have a positive physical impact. From the perspective of social system, PHI physicians, as members of the system, are influenced by the Chinese social system. Working from 9:am to 9:pm for 6 days a week, namely “996”, is a phenomenon widely seen in many walks of life in China. Besides, the medical resource and personnel are tight. Therefore, long working hours is not a case that rarely happens to PHI physicians.39 They have a higher tolerance and adaptability to long working hours. From the perspective of lifestyle habits, it is possible that long working hours has reduced the incidence of crapulence and drinking at night, forcing PHI physicians to eat and rest regularly to cope with the high intensity of workloads.
More Life Pressure on Your Shoulder, the Healthier You Will Be?
Regarding the effect of life stress on subhealth, the analysis showed that the OR of subhealth was reduced to 0.229 (p < 0.05) with relatively high life stress compared to no life stress. And this phenomenon may be due to the fact that there are more middle-aged people in the group of PHI physicians. Although middle-aged people confront heavier life stress compared to older groups, their physical condition is better compared to the older group. Therefore, it is not that higher life stresses lead to better health, but that the stressed population group is still in a relatively good physical condition. And then this study constructs a regression model to analyze the correlation between life stress and subhealth in specific age groups, a conclusion that is more in line with common sense was reached, that is, the higher the stress, the more likely to lead to SHS.40
Do Not Mind Being a Grumbler at Work
The OR increased to 4.04 (p < 0.05) for those who were generally satisfied with their occupation compared to those who were very dissatisfied with their occupation, which is contradictory to the expected influence of psychology status on mental health. However, it was found that the rate of poor lifestyle habits was higher among the generally satisfied group than the non-satisfied group in the descriptive analysis. To further verify the result, logit regression was performed with whether or not they were generally satisfied with their jobs as the dependent variable and each lifestyle habit such as frequency of smoking and drinking, diet and rest conditions as the independent variables. It was found that the odds ratio of generally satisfied with their job for the groups of relatively regular diets and very regular diets were 0.20 and 0.14 respectively using relatively-disorder diet condition as a control. All evidence showed that more people who are generally satisfied with their jobs have irregular diet habits. As for the reason, it is suggested that maybe they choose a more relaxed lifestyle and attitude after being satisfied with their jobs, which has a negative impact on their SHS. However, there are also studies showing that low job satisfaction increases work stress, which affects health status.41,42 The impact of job satisfaction on SHS among PHI physicians needs to be further explored.
Limitations
There are also some shortcomings in this study. Firstly, the sample size of this study and certain subgroups were limited, which might affect the analysis results. The sample size should be expanded to further investigate and verify the influence of each influencing factor on subhealth. Next, although the questionnaire has been tested for reliability and validity in the Chinese population, future studies are expected to have better solutions to this problem. In addition, the data in this study were collected from July to August in 2021, which is time-based. The SHS of PHI physicians may change with the development of the epidemic and economy in China.
Conclusion
A large proportion of PHI physicians in China are in SHS and many of them are not aware that they are in a poor health state. The logit regression model showed that factors including worries about the occurrence of accidents, strained relationships with colleagues, job satisfaction, and frequency of smoking and drinking negatively influence the SHS of PHI physicians, which should be paid more attention and avoided. Meanwhile, annual personal income, long working hours and life stress are protective factors, which means that these factors need to be encouraged. However, further studies need to be conducted to evaluate the effect of long working hours and life stress on physicians’ SHS in PHI.
Considerations
In order to improve the subhealth level of PHI physicians in China, the influencing factors of their SHS should be adjusted reasonably. Specifically, government agencies and medical institutions should increase the income of PHI physicians, reasonably adjust physicians’ work time and stress, and pay attention to the relationship between colleagues. PHI physicians should avoid excessive worrying about accidents that do not occur, reduce the frequency of smoking and drinking, and pay attention to their own health issues. Although moderate working overtime has a protective effect on subhealth for the PHI physicians’ tolerance and the boost in work and emotion brought by the stress, prolonged stress may still have adverse effects on physicians’ health. Further research is warranted to balance the protective effects and the stress from working overtime. In addition, this study only showed that the subhealth rate was relatively lower with relatively high life stress compared with no life stress, however, there was no sufficient evidence that the higher the life stress, the lower the subhealth rate. The descriptive statistical analysis found that the higher the life stress and the lower the job satisfaction, the higher the subhealth rate. Future studies about the effects and mechanics of life stress and job satisfaction on SHS are needed.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the China Pharmaceutical University (approval no. CPU2019015). The participants provided their written informed consent to participate in this study.
Acknowledgments
The authors are very grateful to all the investigators for their efforts and all participants for their cooperation in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work received no specific funding.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Li G, Xie F, Yan S, et al. Subhealth: definition, criteria for diagnosis and potential prevalence in the central region of China. BMC Public Health. 2013:13446. doi:10.1186/1471-2458-13-446
2. Chen J, Cheng J, Liu Y, et al. Associations between breakfast eating habits and health-promoting lifestyle, suboptimal health status in Southern China: a population based, cross sectional study. J Transl Med. 2014:12348. doi:10.1186/s12967-014-0348-1
3. Wessely S, Chalder T, Hirsch S, Wallace P, Wright D. The prevalence and morbidity of chronic fatigue and chronic fatigue syndrome: a prospective primary care study. Am J Public Health. 1997;87(9):1449–1455. doi:10.2105/ajph.87.9.1449
4. Liu YY, Wan CC, Xi XY. Measurement properties of the EQ-5D-5L in sub-health: evidence based on primary health care workers in China. Health Qual Life Outcomes. 2023;21(1):22. doi:10.1186/s12955-023-02105-1
5. Chen Xiaoqian JX, Huang X, Zheng J, Liu G, Pan Y. Establishment of the norms of Sub-Health Measurement Scale for midwives and the influencing factors. J Nursing Sci. 2020;35(24):67–70.
6. He G. Analyzing The Status of Sub-health of Civil Servants in Zhejiang Provincial Government Departments and Its Influencing Factors. Chine Health Service Management. 2020;38(02):151–154.
7. Lan Dazhi LZ, Zhou S, Wei H. Analysis of the current situation and the affecting factors of subhealth of medical staff in public hospitals in Nanning. J Guangxi Univ Chine. 2022;25(04):91–95.
8. Meihong SZZ. Status of sub-health and its influencing factors in community health care workers in Hongkou District, Shanghai. Shanghai J Preventive Med. 2018;33(02):151–156.
9. Xiaoyu WPZ. Investigation on Sub-health Status of College Students and Analysis of Its Influencing Factors. Value Engineering. 2020;39(21):219–221.
10. Ahmad F, Munawar M, Alam MA, Sadiq MS, Anwaar A, Dayar J. Assessment of Suboptimal Health Status among Young Adults and Its Association with Their Demographic Factors. Pakistan J Med Health Sci. 2021;15(9):2460–2463. doi:10.53350/pjmhs211592460
11. Anto EO, Coall DA, Addai-Mensah O, et al. Early gestational profiling of oxidative stress and angiogenic growth mediators as predictive, preventive and personalised (3P) medical approach to identify suboptimal health pregnant mothers likely to develop preeclampsia. Epma J. 2021;12(4):517–534. doi:10.1007/s13167-021-00258-x
12. Jairoun A, Shahwan M. Assessment of University Students’ Suboptimal Health and Social Media Use: implications for Health Regulatory Authorities. J Community Health. 2021;46(4):653–659. doi:10.1007/s10900-020-00929-2
13. Alzain MA, Asweto CO, Zhang J, et al. Telomere Length and Accelerated Biological Aging in the China Suboptimal Health Cohort: a Case-Control Study. Omicsa J Integrative Biol. 2017;21(6):333–339. doi:10.1089/omi.2017.0050
14. Kupaev V, Borisov O, Marutina E, Yan Y-X, Wang W. Integration of suboptimal health status and endothelial dysfunction as a new aspect for risk evaluation of cardiovascular disease. Epma J. 2016;719. doi:10.1186/s13167-016-0068-0
15. Niu Yadong ZY. Ye Ting Development and Current Situation of Service Capacity in Primary Medical Institutions in China. Chine Hospital Manage. 2017;38(06):
16. He Sizhang ZD, Zhang R, Sun BCY. Practical Situation and Consideration of Classified Diagnosis and Treatment in China. Modern Hospital Manage. 2015;13(02):20–22.
17. Ferrans CE, Zerwic JJ, Wilbur JE, Larson JL. Conceptual model of health-related quality of life. J Nursing Scholarship. 2005;37(4):336–342. doi:10.1111/j.1547-5069.2005.00058.x
18. Bi J, Huang Y, Xiao Y, et al. Association of lifestyle factors and suboptimal health status: a cross-sectional study of Chinese students. BMJ Open. 2014;4(6):e005156. doi:10.1136/bmjopen-2014-005156
19. Chen J, Xiang H, Jiang P, et al. The Role of Healthy Lifestyle in the Implementation of Regressing Suboptimal Health Status among College Students in China: a Nested Case-Control Study. Int J Environ Res Public Health. 2017;14(3):240. doi:10.3390/ijerph14030240
20. Li Yao GX, Jiang H, Li M, Wang K, Nie S. Study on the risk factors of sub-health status among people in Qianjiang City. Chine J Dis Control Prevention. 2015;2016(20):374–378.
21. Li YAo GX, Jiang H. Prevalence of sub-health among adult residents of Qianjiang municipality Hubei province. Chine J Public Health. 2017;33(01):149–152.
22. Lolokote S, Hidru TH, Li X. Do socio-cultural factors influence college students’ self-rated health status and health-promoting lifestyles? A cross-sectional multicenter study in Dalian, China. BMC Public Health. 2017;17478. doi:10.1186/s12889-017-4411-8
23. Tian M, Zhang Q, Zhang Z, Meng J, Liu L. Prevalence of Suboptimal Health Status and Its Influencing Factors among Chinese Software Programmers. Iran J Public Health. 2021;50(7):1361–1371.
24. Wu S, Xuan Z, Li F, et al. Work-Recreation Balance, Health-Promoting Lifestyles and Suboptimal Health Status in Southern China: a Cross-Sectional Study. Int J Environ Res Public Health. 2016;13(3):66.
25. Xie Juan LH, Hong Z. Prevalence and influence factors of sub-health among urban residents in Tianjin. Chine J Public Health. 2016;32(01):76–80.
26. Xue Y, Huang Z, Liu G, et al. Association analysis of Suboptimal health Status: a cross-sectional study in China. Peerj. 2020:8e10508. doi:10.7717/peerj.10508
27. Zhou Zhaoxia LJ, Li G, Huang X. Analysis on sub-health status and risk factors of Zhuhai residents. Chinese J Public Health Manage. 2017;33(02):217–219.
28. Raosoft. An online sample size calculator. Available from: http://www.raosoft.com/samplesize.html.
29. COMMISSION NH. Statistical Bulletin on the Development of Health Care in China in 2018 [Online]; 2018.
30. Xu Jun FL, Ren L, Jincai Q, Jinhua Z, Xiaoshan Z, Qian W. Assessment of the reliability and validity of the Sub-health Measurement Scal Version 1.0. J Southern Med Univ. 2011;31(01):33–38.
31. Xu J, Xue Y, Liu G, et al. Establishment of the norms of Sub-Health Measurement Scale Version 1.0 for Chinese urban residents. J Southern Med Univ. 2019;39(3):271–278. doi:10.12122/j.issn.1673-4254.2019.03.03
32. Miao JM, Liu J, Wang Y, Zhang YL, Yuan HX. Reliability and validity of SHMS v1.0 for suboptimal health status assessment of Tianjin residents and factors affecting sub-health A cross-sectional study. Medicine. 2021;100(17):e25401. doi:10.1097/md.0000000000025401
33. Cui Zhouguo XJ, Wu W, Zhang Y, Su S, Huang X. Study of Status and its impacting factors of sub-health in young and middle-aged intellectuals in Guangzhou. China Med Herald. 2015;12(30):12–16.
34. Shan Shuling CD, ying F, Junran H, Guochang X. Subhealth status and influencing factors of female civil servants in perimenopausal. Chine J Gerontol. 2017;37(09):2284–2286.
35. Wu Wei XJ, Qian X, Jinhua Z, Zhouguo C, Xiaowei H. Sub-health Status of Urban Residents in Three Regions in China and Influencing Factors. Chine General Practice. 2016;19(22):2651–2655.
36. Zhang Qingyun WR, Sun D, Kang J, Zhou J, Xue J, Wang Z. Present status on sub-health of nurses from cardiovascular department and analysis on its influencing factors. J Nursing Rehabilitation. 2019;18(07):25–28.
37. Zhang Zhirong RR, Jinxin Z. The State of Sub-health of Medical Personnel in Grade 3 Hospital in Foshan City. China Health Standard Manage. 2019;10(07):8–11.
38. Zhi Yiyu YX. Investigation and analysis of sub-health status in young and middle-aged intellectuals in Guangxi. Modern Clin Nursing. 2017;16(06):5–10.
39. Zhang Hanbing LJ, Li J. Analysis of physicians’ working hours and their influencing factors. Shanxi Med J. 2016;45(23):2743–2744.
40. Xu T, Liu J, Zhu G, Han S. Prevalence and Associated Lifestyle Factors of Suboptimal Health Status among Chinese Children Using a Multi-Level Model. Int J Environ Res Public Health. 2020;17(5):1497. doi:10.3390/ijerph17051497
41. Liang Y-Z, Chu X, Meng S-J, Zhang J, L-J W, Yan Y-X. Relationship between stress-related psychosocial work factors and suboptimal health among Chinese medical staff: a cross-sectional study. BMJ Open. 2018;8(3):e018485. doi:10.1136/bmjopen-2017-018485
42. Sehlen S, Vordermark D, Schaefer C, et al. Job stress and job satisfaction of physicians, radiographers, nurses and physicists working in radiotherapy: a multicenter analysis by the DEGRO Quality of Life Work Group. Radiation Oncol. 2009:46. doi:10.1186/1748-717x-4-6
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
