Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 16
A Review of the Pharmacokinetic Characteristics of Immune Checkpoint Inhibitors and Their Clinical Impact Factors
Received 29 September 2022
Accepted for publication 6 January 2023
Published 20 January 2023 Volume 2023:16 Pages 29—36
DOI https://doi.org/10.2147/PGPM.S391756
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Jun-Chen Liu, Hong-Jing Yu
Department of Clinical Pharmacy, The First People’s Hospital of Jiande, Jiande, People’s Republic of China
Correspondence: Hong-Jing Yu, Department of Medical Oncology, The First People’s Hospital of jiande, No. 599 Yanzhou Avenue, Xin’anjiang street, Jiande, Zhejiang, 311600, People’s Republic of China, Tel +86 15869196365, Fax +86-571-64721520, Email [email protected]
Abstract: Immune checkpoint inhibitors (ICIs) have been shown to be significant in improving the overall survival rate in certain malignancies with poor prognoses. However, only 20– 40% of patients achieve long-term benefits, highlighting the relevance of the factors that influence the treatment, which can help clinicians improve their results and guide the development of new immune checkpoint therapies. In this study, the current pharmacokinetic aspects associated with the ICIs and the factors influencing clinical efficacy were characterised, including in terms of drug metabolism, drug clearance, hormonal effects and immunosuppressive effects.
Keywords: immune checkpoint inhibitors, pharmacokinetics, influencing factors
Background
Cancer is one of the major threats to human health.1–3 Cancer cells can bypass the immune system in a variety of ways, including through the signal molecules expressed by tumour cells combining with the immune checkpoint on the surface of T-cells to jointly inhibit the function of these cells and cause immune escape.2–4 Immune checkpoints (ICs) are upregulated during immune cell activation and play a negative regulatory role in the immune response.5,6 Following IC activation, the activity of the immune cells is suppressed to prevent excessive damage to the peripheral tissues. It is important to have IC proteins to maintain the balance between autoimmunity and self-tolerance; however, the checkpoints can help cancer cells keep out of the way of the body’s defences, helping them to avoid the cellular destruction that occurs when the immune system attacks.5 To date, more than 10 types of ICs have been identified, with cytotoxic T lymphocyte-associated antigen-4 (CTLA-4) and programmed cell death-1/programmed death-ligand-1 (PD-1/PDL-1) the most widely studied.
The development of immune checkpoint inhibitors (ICIs) marked a watershed moment in the field of cancer treatment.7,8 The ICIs reactivate cancer cell immune responses by blocking the co-inhibitory pathways. Meanwhile, CTLA-4 is a transmembrane protein expressed in activated CD4+ and CD8+ T-cells and can competitively bind the ligands CD80 and CD86 with CD28. Its affinity for CD80 and CD86 is greater than that of CD28, replacing the latter and inducing an inhibitory signal to the T-cells. In fact, CTLA-4 is present in the cytoplasm of the cell, and when the T-cell receptors are activated, the CTLA-4 is phosphorylated and transported to the outer membrane of the cell. The CTLA-4 that has been phosphorylated can compete with its homologue, CD28, for the ligands CD80 and CD86, preventing the CD28 from acting as an activator of T-cells. Based on this rationale, the following inhibitors based on the CTLA-4 site were developed: ipilimumab (Yervoy®, Bristol-Myers Squibb) and tremelimumab (AstraZeneca).9,10 These two inhibitors counteract the inhibitory effect of CTLA-4, allowing the CD28 to bind to the CD80/CD86 and activate T-cells, thereby boosting the immune response.
In addition to CTLA-4, the PD-1/PD-L1 pathway is another IC pathway that has attracted some attention. In fact, PD-1 is an important immunosuppressive transmembrane protein expressed on the surface of T-cells, and its main ligand is PD-L1.11 Other co-stimulatory and co-inhibitory receptors, such as glucocorticoid-induced tumour necrosis factor receptor, OX40, 4–1BB, immune inhibitory receptor lymphocyte-activation gene 3, and T-cell immunoglobulin and mucin-domain containing-3, are also used as targets in clinical trials.12 However, despite the importance of ICIs in the treatment of various cancers, including leukaemia, melanoma and non-small-cell lung cancer, little attention has been paid to the therapeutic optimisation and individualisation of ICIs due to the individualised differences in drug therapy treatments, and addressing the attendant pharmacological issues could help to improve the treatment accuracy and lower the healthcare costs. Therefore, this study summarises the pharmacokinetic (PK) and potential clinical influencing factors to provide guidance for individualised clinical treatment.
Pharmacokinetic Characteristics
Primarily, ICIs are humanised or human immunoglobulin G 1 (IgG1) and IgG4 antibodies with similar PK characteristics to other therapeutic monoclonal antibodies (mAbs). They have little or no effect on the renal and hepatic function, and are characterised by a low clearance, a small volume of distribution, extravascular diffusion, a long half-life and an equal timing of receptor-mediated linear and nonlinear combined clearance.13 These mAbs have a distribution volume comparable to that of plasma, and it has been demonstrated that mAbs administered via any route can reach the peripheral tissues.14 The drug receptor’s binding affinity and conjugation-dissociation kinetic characteristics are important in the drug distribution process.15 Nonlinear and linear elimination occurs primarily through specific (target-mediated) and non-specific (constant fragment-mediated) routes of elimination. The linear and non-specific elimination pathways predominate following saturation of the target receptor, resulting in a half-life of three to four weeks for these drugs.14,16
The PK parameters of the majority of currently approved ICIs are based on a two-compartment model with linear elimination, which includes atezolizumab, avelumab and ipilimumab (but not durvalumab, which has both linear and nonlinear characteristics).17–19 The mean maximum reduction (coefficient of variation) was found to have increased from 17.1% (40.6%) at baseline (atezolizumab) to 41.7% (40.0%) (avelumab) in previous studies.17–19 These changes in clearance rate are generally considered not to affect the clinical treatment of the drug. However, recent PK modelling analyses conducted by various research institutions suggest that the clearance rate changes correlate with the efficacy.20–23 It has been reported that the improved aspects of tumour response and overall survival (OS) in patients effectively treated with nivolumab, pembrolizumab or atezolizumab are associated with reduced clearance rates, while tumour shrinkage via durvalumab is also associated with reduced clearance rates.22,23 One interpretation of this finding is that as the patient’s condition improves, a decrease in cachexia will lead to a decrease in catabolism, which will reduce the antibody clearance.22,23 The approved ICIs include anti-CTLA-4, anti-PD-1 and anti-PD-L1 agents, and most exhibit PK characteristics typical of mAbs, with a low clearance and long half-life (Table 1).24–31
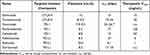 |
Table 1 Pharmacokinetic Data on Immune Checkpoint Inhibitors |
Typically, mAbs exhibit little variability in PK characteristics among the patient population, and the introduction of certain intrinsic and extrinsic factors into the population’s PK data can help explain part of the observed variation.32 It has been reported that the main intrinsic covariates include gender, age and various factors related to disease status (including parameters such as tumour type, tumour load and baseline, lactate dehydrogenase and albumin), and that the corresponding differences among the patients can result in a variation in PK characteristics.33–35 Most factors affecting drug clearance (including age, gender, race, tumour load, Eastern Cooperative Oncology Group and immunogenicity) appear to be independent of clinical efficacy since they do not affect the PK parameters by more than 30%.36 However, body weight and clearance have been found to be significantly associated with certain mAbs (eg ipilimumab, pembrolizumab and avelumab).
Since all the ICIs have been approved only recently, the data on the PK/PD relationship of ICIs remain limited, with most based on registration trials involving selected patient populations.37 As with other mAbs (eg bevacizumab, trastuzumab and cetuximab), years of clinical practice are required following approval for oncology treatment, specifically in terms of examining the PK factors and identifying biomarkers that can be used as predictors of the clinical outcomes.
Effect of Liver and Kidney Injury on Immune Checkpoint Inhibitors
The Food and Drug Administration (FDA) guidelines recommend assessing the effect of renal injury on drug PKs when the molecular weight of the drug is <69 kDa. Given that most mAbs have a molecular weight of 100–1000 kDa, renal impairment generally does not affect their PK.16 Renal function is a statistically significant covariate that affects the clearance of a number of approved ICIs, but its effect on their PK characteristics is only around 20%–30%. Accordingly, the PK characteristics of nivolumab, pembrolizumab and avelumab in patients with mild, moderate or severe renal impairment were found to have no clinically meaningful effects when compared to healthy patients in a population PK analysis.17,18,38,39 In other PK-based studies, the patients with renal impairment did not require dose adjustments, and there were no significant clinical differences in clearance between the patients with renal impairment and those with normal renal function.40,41 Elsewhere, neither atezolizumab nor durvalumab PKs were found to have an effect on mild or moderate renal impairment, but the effect on severe renal impairment remains unknown.19,21,42 According to current research, there is no need to adjust the dose of ICIs in patients with renal impairment.19,42
Given that mAbs are typically degraded by proteases, and hepatic cytochrome enzymes play no role in their metabolism, dedicated liver injury studies are rarely carried out. However, the liver plays an important role in proteolytic metabolism and can have an indirect impact on mAb PKs. Using markers such as aspartate aminotransferase, alanine aminotransferase, albumin and bilirubin as the covariates, population PK models are frequently used to compare the PK parameters and exposures among patients with normal and impaired liver function. Since the results of single markers are unreliable, the effect of liver damage on mAbs is generally assessed using a composite score (eg the Child–Pugh score).43 Mild hepatic impairment does not affect the PK characteristics of nivolumab, pembrolizumab, atezolizumab or durvalumab, meaning there is no need to adjust the dose in these cases. Most trials have excluded patients with moderate to severe liver injury, meaning the effect of mAbs among such patients remains unknown.17,19,38,42 A mild liver injury does not affect the PK characteristics of ipilimumab, which are similar to those of patients with normal liver function. Patients with moderate or severe hepatic function have not been studied in relation to ipilimumab. Meanwhile, avelumab has no clinically meaningful effect on PK characteristics in terms of either mild or moderate liver function, and its effect on severe liver damage is unknown.18,33 Therefore, ICI dose adjustment is also not recommended for patients with hepatic insufficiency.
Effect of Hormones on the Metabolism of Immune Checkpoint Inhibitors
Many immune-related adverse events (irAEs) can occur with the use of IC drugs. Diarrhoea, rash, hepatitis and hypophysitis are the most common irAEs. Researchers have learned to recognise these tumour complications early and treat them with immunosuppressive drugs, most commonly corticosteroids.44 Corticosteroids are used to treat and prevent excessive inflammation, which could jeopardise the therapeutic mechanisms of ICIs. Lymphopenia and impaired T-cell responses to antigens are two mechanisms of action for corticosteroids, which lead to inflammation and reduced immune activity.45 Many chemotherapy patients require corticosteroids before, during or after ICI treatment. Furthermore, most of the negative effects of ICIs, primarily autoimmune toxicity, are due to the inhibition of immunomodulatory checkpoints that induce tolerance. Corticosteroids are commonly used to treat these irAEs. In studies related to ipilimumab treatment for melanoma patients, high-dose steroid therapy was found to have long-lasting antitumour effects in patients with irAEs without compromising the drug efficacy.46,47 In contrast, whether hormones affect the initial antitumour response to immunotherapy remains unclear. According to a 2018 study, almost one-third of patients with non-small-cell lung cancer treated with nivolumab while receiving concomitant corticosteroids had fewer total treatment cycles, implying a lower clinical benefit and shorter OS time.48 In 2018 and 2019, two different study groups found that using more than 10 mg of a corticosteroid prednisone-equivalent affected the immunotherapy outcomes in patients with non-small-cell lung cancer. Elsewhere, Arbour et al found that the use of corticosteroid prednisone-equivalents attenuated immune T-cell activity and further weakened the immune efficacy in 640 patients with non-small-cell lung cancer treated with a PD-L1 blockade, and the authors recommend using glucocorticoids with caution when commencing a PD-L1 blockade.49 The same results were obtained by Fucà et al, whose clinical data indicated that the administration of high-dose corticosteroid prednisone-equivalents in 151 clinical patients significantly reduced the lymphocyte counts, resulting in a negative effect on the ICI therapy.50 However, the 2019 JCO defended hormones, arguing that the condition of the patient’s organism influenced the OS time, independent of hormone use. However, until PD-1 antibodies are used, it is recommended not to use hormones if there is no indication for their use. In cases of cerebral oedema and respiratory distress, glucocorticoids can be used according to the conventional regimen. Meanwhile, the use of topical, oral or intravenous hormones to control immunotoxicity was found not to affect the OS time, meaning patients with immunotoxicity should still be treated aggressively with hormones. The rational use of hormones to control the side effects does not affect the efficacy.51 Similarly, new evidence suggests that treating irAEs with glucocorticoids has no negative impact on the efficacy.52–54
In conclusion, it is unlikely that steroid hormone therapy will affect the efficacy since it is only used for a short time before and after chemotherapy. The relationship between the timing and duration of steroid administration should be investigated in future studies. The brief use of corticosteroids during chemotherapy with a PD-L1 blockade will not likely be as detrimental as the effect of long-term corticosteroid use on the PD-L1 blockade. At the same time, the influence of other factors on the disease should be excluded.
Effect of Immunosuppressants on the Efficacy of Immune Checkpoint Inhibitors and the Possibility of Rejection in Transplant Patients
In some cases, glucocorticoids alone are insufficient for treating immune-related side effects, and additional immunosuppressive drugs, such as antitumour necrosis factor (anti-TNF) mAbs, are required. According to one study, 30% of the patients given systemic high-dose corticosteroids failed to completely control their adverse events, necessitating additional immunosuppressive therapy. The majority of patients only require a single dose of infliximab, while some may require a second dose. Long-term treatment with high-dose corticosteroids is preferable to early treatment with infliximab.55 Generally, if the symptoms do not improve significantly during the first few weeks of high-dose systemic corticosteroid therapy, continued treatment is unlikely to be beneficial, and the patients will most likely require infliximab. Whether the use of the drug also has a corresponding effect on the efficacy of PD-1. The FDA currently approves the combination regimen of CTLA-4 and anti-PD-1 antibodies for a variety of cancers, including melanoma, renal cell carcinoma and colorectal cancer; however, this combination can lead to serious irAEs.
In animal studies, it was found that if TNF inhibitors were given prophylactically at the beginning of the treatment, instead of reducing the effect of the immune combination therapy, the effect of the immunotherapy was improved.56 It is believed that the short-term use of immune agents does not affect PD-1 efficacy; however, given that there exist few relevant studies, especially on the effect of the long-term use of immunosuppressive agents on PD-1 efficacy, more evidence from clinical studies is needed.
In another case, a patient with stage-IV small-cell lung cancer treated with cyclosporine and corticosteroid prednisone who received three doses of nabumetinumab was reported to experience severe rejection.54 There is also evidence that CTLA-4 results in less graft rejection than PD-1 in renal transplant oncology patients.33,57,58 Renal transplant recipients have a higher risk of skin cancer, urologic malignancies and other cancers than the general population, and it is worth exploring whether this is linked to immunosuppressive therapy. The T-cells activated by PD-1 inhibitors do not only attack malignant tumour cells but also the donor alloantigens of the transplanted kidney. Furthermore, in transplant patients, PD-1/PD-L1 is required for the induction and maintenance of peripheral allograft tolerance. In addition, this pathway is involved in the induction of regulatory T-cells, which plays an important role in suppressing T-cell activation in renal transplant recipients following exposure to alloantigens.59 As a result, even with the use of immunosuppressive anti-rejection drugs, there appears to be a risk of rejection with PD-1 treatment in renal transplant oncology patients.
Impact of Vaccines on Immune Checkpoint Inhibitors
By affecting the number and quality of long-lived plasma cells, PD-1 inhibitors may affect the humoral response to vaccines.60 Infection with the influenza virus is linked to a high morbidity and mortality rate in cancer patients.61,62 As such, an influenza vaccination is recommended for such patients, especially those receiving antineoplastic therapy.63,64 Various studies on vaccine-induced humoral immune responses in patients receiving traditional cytotoxic chemotherapy have found that, in general, a concomitant seasonal influenza vaccination is safe for cytotoxic chemotherapy patients; however, most of these studies have found that increasing the vaccine dose reduces the effectiveness of serum protective antibody titers.65–67 While the humoral immune responses are reduced in patients receiving cytotoxic chemotherapy, the response in patients undergoing a checkpoint blockade for cancer is unknown. The relationship between ICIs and influenza vaccinations was investigated by Chong et al, and the results indicated that among the 370 patients receiving an influenza vaccination within 65 days of ICI treatment, the incidence of irAEs was not affected.68 Similarly, a study on trivalent inactivated influenza vaccinations in lung cancer patients receiving ICIs (nivolumab or pembrolizumab) revealed that the influenza vaccine induced similar serum antibody titers in these patients as in the healthy population. However, the seroconversion rate was significantly higher in the oncology patients than in the healthy population, and it was clear that the influenza vaccination in the oncology patients receiving ICIs could cause immune overstimulation in response, leading to an increased risk of an ICI-induced irAE.69 However, the findings of a large observational study conducted by Wijn et al70 involving lung cancer patients only (n = 127) cast some doubt on these findings, with the authors finding no difference in irAEs between the vaccinated and unvaccinated non-small-cell lung cancer patients receiving anti-PD-1 and concluding that influenza vaccinations should not be discouraged in this patient group. Similarly, Chong et al71 found a similar rate of irAEs in clinical ICI trials, implying that the co-administration of influenza vaccines with FDA-approved ICIs is both safe and effective. In summary, most studies conclude that vaccinations are safe and effective for oncology patients receiving ICIs, while attention should still be paid to the possibility of adverse effects.
Conclusion
At present, various ICIs are on the market, and the focus is on improving the molecular target affinity and clinical efficacy without a complete understanding of the rationale for PK modelling. Unlike with chemical drugs, the dose selection, especially for mAbs with complex PKs and pharmacodynamics, is a major challenge in the development of targeted therapies. However, as previously noted, mAb-related PK studies have revealed significant inter-patient variability, with many factors found to influence the patients’ uptake distribution of mAbs. With this in mind, this study examined the potential PK factors as well as the current clinical issues, providing useful evidence for further investigation into the therapeutic drug monitoring of these mAbs. In this study, it was confirmed that there is no need to adjust the ICI dose in patients with renal damage, with the ICIs of patients with mild liver injury not requiring a dosage adjustment, while the medication for patients with moderate and severe liver damage requires further research. At present, hormones may not affect the efficacy of ICIs, but it is important to study the relationship between the administration time and the duration of hormone drugs. Furthermore, more clinical evidence is needed to determine whether combined immunosuppressants or vaccines have an impact on ICIs (Table 2). Future research should focus on improving the dosage and dosing regimens of these mAbs, as well as gradually developing personalised drug treatment regimens through therapeutic drug monitoring to improve the success rate of the clinical treatments.
 |
Table 2 Effects of Liver and Kidney Injury, Hormones, Immunosuppressants, and Vaccines on ICIs |
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Research and Publication Ethics
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of The First People’s Hospital of jiande.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Zhejiang Province Medical and Health Science and Technology Program[Grant NO.:2020KY808].
Disclosure
All of the authors had no any personal, financial, commercial or academic conflicts of interest separately.
References
1. Alexandrov LB, Kim J, Haradhvala NJ, et al. The repertoire of mutational signatures in human cancer. Nature. 2020;578(7793):94–101. doi:10.1038/s41586-020-1943-3
2. Vishwakarma M, Piddini E. Outcompeting cancer. Nat Rev Cancer. 2020;20(3):187–198. doi:10.1038/s41568-019-0231-8
3. Brown AJ, Chua NK, Yan N. The shape of human squalene epoxidase expands the arsenal against cancer. Nat Commun. 2019;10(1):888. doi:10.1038/s41467-019-08866-y
4. Hausman DM. What is cancer? Perspect Biol Med. 2019;62(4):778–784. doi:10.1353/pbm.2019.0046
5. Nakamura K, Smyth MJ. Myeloid immunosuppression and immune checkpoints in the tumor microenvironment. Cell Mol Immunol. 2020;17(1):1–12. doi:10.1038/s41423-019-0306-1
6. Pérez-Ruiz E, Melero I, Kopecka J, Sarmento-Ribeiro AB, García-Aranda M, De Las Rivas J. Cancer immunotherapy resistance based on immune checkpoints inhibitors: targets, biomarkers, and remedies. Drug Resistance Updates. 2020;53:100718. doi:10.1016/j.drup.2020.100718
7. Tundo GR, Sbardella D, Lacal PM, Graziani G, Marini S. On the horizon: targeting next-generation immune checkpoints for cancer treatment. Chemotherapy. 2019;64(2):62–80. doi:10.1159/000500902
8. Affolter T, Llewellyn HP, Bartlett DW, et al. Inhibition of immune checkpoints PD-1, CTLA-4, and IDO1 coordinately induces immune-mediated liver injury in mice. PLoS One. 2019. doi:10.1371/journal.pone.0217276
9. Rotte A. Combination of CTLA-4 and PD-1 blockers for treatment of cancer. J Exp Clin Cancer Res. 2019;38(1):255. doi:10.1186/s13046-019-1259-z
10. Toor SM, Nair VS, Decock J, Elkord E. Immune checkpoints in the tumor microenvironment. Semin Cancer Biol. 2020;65:1–12. doi:10.1016/j.semcancer.2019.06.021
11. Iwai Y, Ishida M, Tanaka Y, Okazaki T, Honjo T, Minato N. Involvement of PD-L1 on tumor cells in the escape from host immune system and tumor immunotherapy by PD-L1 blockade. Proc Natl Acad Sci U S A. 2002;99(19):12293–12297. doi:10.1073/pnas.192461099
12. Marin-Acevedo JA, Dholaria B, Soyano AE, Knutson KL, Chumsri S, Lou Y. Next generation of immune checkpoint therapy in cancer: new developments and challenges. J Hematol Oncol. 2018;11(1):39. doi:10.1186/s13045-018-0582-8
13. Wang W, Wang EQ, Balthasar JP. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84(5):548–558. doi:10.1038/clpt.2008.170
14. Zhao L, Ren TH, Wang DD. Clinical pharmacology considerations in biologics development. Acta Pharmacol Sin. 2012;33(11):1339–1347. doi:10.1038/aps.2012.51
15. Deng R, Jin F, Prabhu S, Iyer S. Monoclonal antibodies: what are the pharmacokinetic and pharmacodynamic considerations for drug development. Expert Opin Drug Metab Toxicol. 2012;8(2):141–160. doi:10.1517/17425255.2012.643868
16. Mould DR, Meibohm B. Drug development of therapeutic monoclonal antibodies. BioDrugs. 2016;30(4):275–293. doi:10.1007/s40259-016-0181-6
17. KEYTR UDA (pembrolizumab) [package insert]. Whitehouse Station, NJ: Merck & Co. Inc; 2017. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/125514s016lbl.pdf.
18. BA VENCIO (avelumab) [package insert]. Rockland, MA: EMD Serono, Inc; 2017. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761049s000lbl.pdf.
19. IMFINZI (durvalumab) [package insert]. Wilmington, DE: AstraZeneca Pharmaceuticals LP; 2017. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761069s000lbl.pdf.
20. Center for Drug Evaluation and Research. TECENTRIQ Clinical pharmacology and biopharmaceutics review; 2016. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2016/761041Orig1s000ClinPharmR.pdf.
21. Baverel P, Dubois V, Jin C, et al. Population pharmacokinetics of durvalumab and fixed dosing regimens in patients with advanced solid tumors. J Clin Oncol. 2017;35(suppl):2566. doi:10.1200/JCO.2017.35.15_suppl.2566
22. European Medicines Agency. Keytruda extension of indication assessment report; 2016. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Assessment_Report_-_Variation/human/003820/WC500212039.pdf.
23. Liu C, Yu J, Li H, et al. Association of time-varying clearance of nivolumab with disease dynamics and its implications on exposure response analysis. Clin Pharmacol Ther. 2017;101(5):657–666. doi:10.1002/cpt.656
24. Feng Y, Masson E, Dai D, Parker SM, Berman D, Roy A. Model-based clinical pharmacology profiling of ipilimumab in patients with advanced melanoma. Br J Clin Pharmacol. 2014;78(1):106–117. doi:10.1111/bcp.12323
25. Wang E, Kang D, Bae K-S, Marshall MA, Pavlov D, Parivar K. Population pharmacokinetic and pharmacodynamic analysis of tremelimumab in patients with metastatic melanoma. J Clin Pharmacol. 2014;54(10):1108–1116. doi:10.1002/jcph.309
26. Bajaj G, Wang X, Agrawal S, Gupta M, Roy A, Feng Y. Model-based population pharmacokinetic analysis of nivolumab in patients with solid tumors. CPT Pharmacometrics Syst Pharmacol. 2017;6(1):58–66. doi:10.1002/psp4.12143
27. Freshwater T, Kondic A, Ahamadi M, et al. Evaluation of dosing strategy for pembrolizumab for oncology indications. J Immunother Cancer. 2017;5:43. doi:10.1186/s40425-017-0242-5
28. Libtayo. FDA drug label. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761097s001lbl.pdf.
29. Patel R, Bock M, Polotti CF, Elsamra S. Pharmacokinetic drug evaluation of atezolizumab for the treatment of locally advanced or metastatic urothelial carcinoma. Expert Opin Drug Metab Toxicol. 2017;13(2):225–232. doi:10.1080/17425255.2017.1277204
30. Kim ES. Avelumab: first global approval. Drugs. 2017;77(8):929–937. doi:10.1007/s40265-017-0749-6
31. Imfinzi. FDA drug label. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761069s002lbl.pdf.
32. Bai S, Jorga K, Xin Y, et al. A guide to rational dosing of monoclonal antibodies. Clin Pharmacokinet. 2012;51(2):119–135. doi:10.2165/11596370-000000000-00000
33. Feng Y, Masson E, Dai D, Parker SM, Berman D, Roy A. Model-based clinical pharmacology profiling of ipilimumab in patients with advanced melanoma. Br J Clin Pharmacol. 2014;78(1):106–117. doi:10.1111/bcp.12323
34. Bajaj G, Wang X, Agrawal S, et al. Model-based population pharmacokinetic analysis of nivolumab with solid tumors. CPT Pharmacometrics Syst Pharmacol. 2017;6(1):58–66. doi:10.1002/psp4.12143
35. Ahamadi M, Freshwater T, Prohn M, et al. Model-based characterization of the pharmacokinetics of pembrolizumab: a humanized anti-PD-1 monoclonal antibody in advanced solid tumors. CPT Pharmacometrics Syst Pharmacol. 2017;6(1):49–57. doi:10.1002/psp4.12139
36. Desnoyer A, Broutin S, Delahousse J, et al. Pharmacokinetic/pharmacodynamic relationship of therapeutic monoclonal antibodies used in oncology: part 2, immune checkpoint inhibitor antibodies. Eur J Cancer. 2020;128:119–128. doi:10.1016/j.ejca.2020.01.003
37. Ji H, Tang X, Dong Z, Song L, Jia YT. Adverse event profiles of anti-CTLA-4 and anti-PD-1 monoclonal antibodies alone or in combination: analysis of spontaneous reports submitted to FAERS. Clin Drug Investig. 2019;39(3):319–330. doi:10.1007/s40261-018-0735-0
38. OPDIVO (nivolumab) [package insert]. Princeton, NJ: BristolMyers Squibb Company; 2017. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/125554s031lbl.pdf.
39. Center for Drug Evaluation and Research. BA VENCIO clinical pharmacology and biopharmaceutics review; 2017. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2017/761049orig1s000clinpharmr.pdf.
40. Rizvi S, Wang J, El-Khoueiry AB. Liver cancer immunity. Hepatology. 2020;73:86–103. doi:10.1002/hep.31416
41. YER VOY (ipilimumab) [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2015. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/125377s074lbl.pdf.
42. TECENTRIQ (atezolizumab) injection, for intravenous use[package insert]. South San Francisco, CA: Genentech, Inc; 2017. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761034s001lbl.pdf.
43. US Food and Drug Administration. Guidance for Industry.Pharmacokinetics in patients with impaired hepatic function: study design, data analysis, and impact on dosing and labeling; 2003. Available from: https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm072123.pdf.
44. Griewing LM, Schweizer C, Schubert P, et al. Questionnaire-based detection of immune-related adverse events in cancer patients treated with PD-1/PD-L1 immune checkpoint inhibitors. BMC Cancer. 2021;21(1):1–10. doi:10.1186/s12885-021-08006-0
45. Greaves MW. Anti-inflammatory action of corticosteroids.Postgrad. Med J. 1976;52:631–633. doi:10.1136/pgmj.52.612.631
46. Downey SG, Klapper JA, Smith FO, et al. Prognostic factors related to clinical response in patients with metastatic melanoma treated by CTL-associated antigen-4 blockade. Clin Cancer Res. 2007;13:6681–6688. doi:10.1158/1078-0432.CCR-07-0187
47. Harmankaya K, Erasim C, Koelblinger C, et al. Continuous systemic corticosteroids do not affect the ongoing regression of metastatic melanoma for more than two years following ipilimumab therapy. Med Oncol. 2011;28:1140–1144.
48. Scott SC, Pennell NA. Early use of systemic corticosteroids in patients with advanced NSCLC treated with nivolumab. J Thorac Oncol. 2018;13(11):1771–1775. doi:10.1016/j.jtho.2018.06.004
49. Arbour KC, Mezquita L, Long N, et al. Impact of baseline steroids on efficacy of programmed cell death-1 and programmed death-ligand 1 blockade in patients with non-small-cell lung cancer. J Clin Oncol. 2018;36(28):2872–2878. doi:10.1200/JCO.2018.79.0006
50. Fucà G, Galli G, Poggi M, et al. Modulation of peripheral blood immune cells by early use of steroids and its association with clinical outcomes in patients with metastatic non-small cell lung cancer treated with immune checkpoint inhibitors. ESMO open. 2019;4(1):e000457.
51. Kahn AM, Blenman KRM, Sonis ST, Lustberg MB. Strategies to mitigate the toxicity of cancer therapeutics. Adv Cancer Res. 2022;155:215–244. doi:10.1016/bs.acr.2022.02.006
52. Postow MA, Sidlow R, Hellmann MD. Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med. 2018;378:158–168. doi:10.1056/NEJMra1703481
53. Santini FC, Rizvi H, Wilkins O, et al. Safety of retreatment with immunotherapy after immunerelated toxicity in patients with lung cancers treated with anti-PD(L)-1 therapy. J Clin Oncol. 2017;(suppl 35):9012. doi:10.1200/JCO.2017.35.15_suppl.9012
54. Horvat TZ, Adel NG, Dang TO, et al. Immunerelated adverse events, need for systemic immunosuppression, and effects on survival and time to treatment failure in patients with melanoma treated with ipilimumab at Memorial Sloan Kettering Cancer Center. J Clin Oncol. 2015;33:3193–3198. doi:10.1200/JCO.2015.60.8448
55. Weber JS, Larkin JMG, Schadendorf D, et al. Management of gastrointestinal (GI) toxicity associated with nivolumab (NIVO) plus ipilimumab (IPI) or IPI alone in Phase II and III trials in advanced melanoma (MEL). J Clin Oncol. 2017;(suppl 35):9523. doi:10.1200/JCO.2017.35.15_suppl.9523
56. Schadendorf D, Wolchok JD, Hodi FS, et al. Efficacy and safety outcomes in patients with advanced melanoma who discontinued treatment with nivolumab and ipilimumab because of adverse events: a pooled analysis of randomized phase II andIII trials. J Clin Oncol. 2017;35:3807–3814. doi:10.1200/JCO.2017.73.2289
57. Boils CL, Aljadir DN, Cantafio AW. Use of the PD-1 pathway inhibitor nivolumab in a renal transplant patient with malignancy. Am J Transplant. 2016;16(8):2496–2497. doi:10.1111/ajt.13786
58. Regalla DKR, Williams GR, Paluri RK. Immune checkpoint inhibitors in the management of malignancies in transplant recipients. Postgrad Med J. 2018;94:704–708. doi:10.1136/postgradmedj-2018-136081
59. Lipson EJ, Bodell MA, Kraus ES, Sharfman WH. Successful administration of ipilimumab to two kidney transplantation patients with metastatic melanoma. J Clin Oncol. 2014;32:e69–e71. doi:10.1200/JCO.2013.49.2314
60. De Bruyn P, Van Gestel D, Ost P, et al. Immune checkpoint blockade for organ transplant patients with advanced cancer: how far can we go? Curr Opin Oncol. 2019;31(2):54–64. doi:10.1097/CCO.0000000000000505
61. Kean LS, Turka LA, Blazar BR. Advances in targeting co-inhibitory and co-stimulatory pathways in transplantation settings: the Yin to the Yang of cancer immunotherapy. Immunol Rev. 2017;276:192–212. doi:10.1111/imr.12523
62. Good-Jacobson KL, Szumilas CG, Chen L, Sharpe AH, Tomayko MM, Shlomchik MJ. PD-1 regulates germinal center B cell survival and the formation and affinity of long-lived plasma cells. Nat Immunol. 2010;11(6):535–542. doi:10.1038/ni.1877
63. Treanor JJ. CLINICALPRACTICE. influenza vaccination. N Engl J Med. 2016;375(13):1261–1268. doi:10.1056/NEJMcp1512870
64. Robin C, Beckerich F, Cordonnier C. Immunization in cancer patients: where we stand. Pharmacol Res. 2015;92:23–30. doi:10.1016/j.phrs.2014.10.002
65. Choi DK, Fuleihan RL, Walterhouse DO. Serologic response and clinical efficacy of influenza vaccination in children and young adults on chemotherapy for cancer. Pediatr Blood Cancer. 2016;63(11):2011–2018. doi:10.1002/pbc.26110
66. Nakashima K, Aoshima M, Ohfuji S, et al. Immunogenicity of trivalent influenza vaccine in patients with lung cancer undergoing anticancer chemotherapy. Hum Vaccin Immunother. 2017;13(3):543–550. doi:10.1080/21645515.2016.1246094
67. Waqar SN, Boehmer L, Morgensztern D, et al. Immunogenicity of influenza vaccination in patients with Cancer. Am J Clin Oncol. 2018;41(3):248–253. doi:10.1097/COC.0000000000000257
68. Chong CR, Park VJ, Cohen B, et al. Safety of inactivated influenza vaccine in cancer patients receiving immune checkpoint inhibitors. Clin Infect Dis. 2020;70(2):193–199. doi:10.1093/cid/ciz202
69. Hakim H, Allison KJ, Van de Velde LA, et al. Immunogenicity and safety of high-dose trivalent inactivated influenza vaccine compared to standard-dose vaccine in children and young adults with cancer or HIV infection. Vaccine. 2016;34(27):3141–3148. doi:10.1016/j.vaccine.2016.04.053
70. Wijn DH, Groeneveld GH, Vollaard AM, et al. Influenza vaccination in patients with lung cancer receiving anti–programmed death receptor 1 immunotherapy does not induce immune-related adverse events. Eur J Cancer. 2018;104:182–187. doi:10.1016/j.ejca.2018.09.012
71. Chong CR, Park V, Harding JJ, et al. Safety of influenza vaccination in patients undergoing immunotherapy treatment for advanced cancer. J Clin Oncol. 2018;36(15_suppl):e15073–e15073. doi:10.1200/JCO.2018.36.15_suppl.e15073
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
