Back to Journals » Clinical Ophthalmology » Volume 14
A Review of Advancements and Evidence Gaps in Diabetic Retinopathy Screening Models
Authors Pearce E, Sivaprasad S
Received 12 June 2020
Accepted for publication 6 August 2020
Published 14 October 2020 Volume 2020:14 Pages 3285—3296
DOI https://doi.org/10.2147/OPTH.S267521
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Elizabeth Pearce,1 Sobha Sivaprasad1,2
1Department of Ocular Biology, Institute of Ophthalmology, University College London, London, UK; 2Medical Retina Department, NIHR Moorfields Biomedical Research Centre, Moorfields Eye Hospital, London, UK
Correspondence: Sobha Sivaprasad
NIHR Moorfields Biomedical Research Centre, Moorfields Eye Hospital, NHS Foundation Trust, 162 City Road, London EC1V 2PD, UK
Tel +44 20 7253 3411
Email [email protected]
Abstract: Diabetic retinopathy (DR) is a microvascular complication of diabetes with a prevalence of ∼ 35%, and is one of the leading causes of visual impairment in people of working age in most developed countries. The earliest stage of DR, non-proliferative DR (NPDR), may progress to sight-threatening DR (STDR). Thus, early detection of DR and active regular screening of patients with diabetes are necessary for earlier intervention to prevent sight loss. While some countries offer systematic DR screening, most nations are reliant on opportunistic screening or do not offer any screening owing to limited healthcare resources and infrastructure. Currently, retinal imaging approaches for DR screening include those with and without mydriasis, imaging in single or multiple fields, and the use of conventional or ultra-wide-field imaging. Advances in telescreening and automated detection facilitate screening in previously hard-to-reach communities. Despite the heterogeneity in approaches to fit local needs, an evidence base must be created for each model to inform practice. In this review, we appraise different aspects of DR screening, including technological advances, identify evidence gaps, and propose several studies to improve DR screening globally, with a view to identifying patients with moderate-to-severe NPDR who would benefit if a convenient treatment option to delay progression to STDR became available.
Keywords: telescreening, non-proliferative diabetic retinopathy, risk-stratification, systematic, opportunistic
Plain Language Summary
Diabetic retinopathy is a common complication of diabetes and is one of the leading causes of blindness in adults of working age.
Regular screening and early detection, before diabetic retinopathy progresses to the sight-threatening stage, is needed to provide treatment to prevent sight loss.
The increasing number of patients with diabetes means there are major challenges to carrying out accurate, cost-effective screening on a large scale, including:
- A lack of agreement on the best screening methods and how often they should be used
- Limited resources and infrastructure in some cases because many countries do not have country-wide healthcare systems or diabetic retinopathy care plans
- Patients with diabetes not attending their screening appointments
We reviewed current diabetic retinopathy screening methods and found that telescreening, whereby ophthalmologists visit communities or digital pictures are taken and graded later by an expert, combined with artificial intelligence (AI) to automatically detect diabetic retinopathy, may be a solution:
- Telescreening cost savings increase when carried out on a larger scale
- AI automated detection has been developed for handheld cameras, unmanned kiosks, and smartphones, increasing accessibility
- Telescreening programs and patient education improve screening attendance
To provide the evidence needed to adopt these new techniques, future studies should focus on developing telescreening methods that are cost-effective across all healthcare systems. Other studies should investigate the reliability of AI automated detection and the ease of use of handheld devices and other new technologies.
Introduction
Diabetes is a global problem, afflicting more than 425 million people worldwide, which could rise to 629 million by 2045.1 Diabetic retinopathy (DR) is a microvascular complication of diabetes, with an average prevalence of about 35% among people with diabetes, and is one of the leading causes of blindness in people of working age in most developed countries.1 The earliest stage of DR is non-proliferative DR (NPDR). NPDR may progress from mild through moderate, then severe stages, to sight-threatening DR (STDR), such as proliferative DR (PDR) and diabetic macular edema (DME).2 Approximately one-third of patients with DR have STDR,2 so regular active screening of patients with diabetes and early detection of DR are necessary for early intervention to prevent sight loss and blindness. For example, after the introduction of national systematic screening programs in England and Wales, inherited retinal disorders accounted for more cases of certified blindness than DR in 2009–2010.3
Optimization of glycemic control, blood pressure, and serum lipid control are recommended to reduce the risk or slow the progression of DR. Nevertheless, even with optimal systemic control, a substantial proportion of patients with diabetes will develop DME or proliferative changes requiring intervention.4 Currently, treatment options that specifically target NPDR and DME are limited to panretinal photocoagulation, intravitreal corticosteroids, and intravitreal vascular endothelial growth factor (VEGF) inhibitors.5–7 While these treatments are effective for many patients, they may be inconvenient, uncomfortable, and in some cases, associated with permanent eye damage.5,8 An effective systemic therapy delivered as an oral formulation would provide a more convenient treatment option that could be administered to patients with moderate-to-severe NPDR identified through active screening to delay progression to STDR.
Although the incidence of DR development is higher for patients with type one diabetes (T1D) compared with type two diabetes (T2D),9,10 T2D is more prevalent than T1D, accounting for 90–95% of all diabetes cases and the majority of DR cases.10,11 One of the biggest challenges in managing DR is the prevalence of undiagnosed diabetes because DR may progress to STDR before a diagnosis of diabetes is established, resulting in people presenting with symptomatic complications of diabetes, both because the onset of T2D is usually slow and because the presentation may involve a long pre-detection period.1,2
Table 1 shows the estimated prevalence of diabetes globally and illustrates the gravity of the problem of undiagnosed diabetes – the prevalence of diabetes worldwide is 9.3%, rising to 13.3% in North America and the Caribbean.1 Another challenge faced in most countries with no DR care pathway is that as patients are asymptomatic, they are reluctant to present themselves for treatment, or they cannot afford out-of-pocket expenses for treatment.
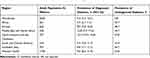 |
Table 1 Global Diabetes Prevalence in Adults Aged 20−79 (2019)1 |
In this review, we aim to identify the research required to improve DR screening globally, with a view to detecting patients with moderate-to-severe NPDR who would benefit if a convenient treatment option to delay progression to STDR became available in the near future.
DR Screening
As opposed to other branches of medicine where patients receive tests when a disease is suspected, DR screening seeks to identify a previously undetected complication of diabetes in otherwise healthy individuals.12 Patients with diabetes who do not receive DR screening are at four-fold higher risk of STDR;13 therefore, the broad goal of DR screening is to prevent progression to STDR. Screening for DR is cost effective compared with the costs of vision loss from undetected DR,14 and further cost savings can be made if high-risk groups are screened at shorter intervals than low-risk groups.15
DR screening is instrumental in disease management, including making treatment decisions; for example, early intervention in moderate-to-severe NPDR before it develops into PDR or DME may reduce both the disease burden for patients and societal costs.16 The benefit could be even more substantial after the introduction of an oral therapy for moderate-to-severe NPDR. From a holistic perspective, DR screening can also offer a further advantage in the detection of retinal and microvascular conditions other than DR.17,18 While there is broad agreement about the need for DR screening programs and currently several different approaches, there is a lack of consensus on the optimal approach in terms of cost effectiveness and/or logistical options in different healthcare systems.
Types of DR Screening
International and national guidelines recommend annual screening for DR for all patients with diabetes,19,20 and this is performed in some countries such as the UK, Iceland, and Hong Kong using systematic national screening programs.3,21,22 Systematic screening for DR involves the selective identification of all individuals at risk of DR (ie any patients with diabetes) and uses quality-assured predetermined screening processes to ensure adequate coverage of the chosen patient population.22 Systematic screening is probably the most effective way of detecting STDR; however, it is difficult to perform in many healthcare systems where there are multiple healthcare providers without a centralized database of patients with diabetes. Hence, in most other countries, opportunistic methods, such as local hospital-based projects or community-based screening programs, are used if any screening is performed and tend to cover fewer patients and be less cost effective in the long term than systematic screening. Opportunistic screening is much more common;22 this may be offered by a healthcare professional, requested by a patient, or occur as a result of an assessment for another complaint, but it is not offered to all individuals at risk of DR.
DR Screening Methodology
Various methods of screening can be used to diagnose and monitor DR provided that the recommended sensitivity and specificity levels are met. The National Institute for Health and Care Excellence (NICE) guidelines propose that any screening program for DR should have at least 80% sensitivity and 95% specificity, with a technical failure rate of <5%.19
Mydriasis in DR Screening
Mydriatic retinal photography was traditionally believed to be the most effective DR screening strategy;23 however, mydriasis needs to be performed by a qualified professional and is relatively time-consuming because the eye drops need at least 20 minutes to take effect, thus creating an administrative burden. New approaches to DR screening often omit mydriasis to improve the screening experience and overall acceptance by patients – by not dilating the pupil, the time in the clinic can be minimized and the screening efficiency improved (by taking fewer photographs and not having to wait for the dilating drops to take effect), allowing larger numbers of patients to be screened more quickly than traditional surveillance techniques.24 A 2015 meta-analysis showed that although diagnostic accuracy was higher with mydriasis, adequate levels of sensitivity and specificity can be reached without mydriasis.25 Different instruments can be used for screening (eg a direct or indirect ophthalmoscope, slit lamp, photographic film, scanning laser, or digital photography). The number of photographic fields, mydriatic status, and the experience or qualifications of the grader can vary.26 For example, different numbers of photographic fields can be used for detecting retinopathy, trading ease of execution and cost for sensitivity.
Imaging in Single or Multiple Fields
The gold-standard DR detection method is 30° stereoscopic color fundus photography in seven standard fields;27 however, this method is time-consuming and may be uncomfortable for the patient, as well as impractical for large-scale screening programs.22 The use of digital fundus photography allows for a greater viewing angle, with most screening programs currently using 45°, enables the use of fewer fields, and is more convenient as it is quicker, requires less light exposure, and is often performed without mydriasis; however, sensitivity and specificity are reduced.28 Compared with mydriatic ophthalmoscopy, the sensitivity and specificity for detecting DR with one-, two-, three-, and five-field non-mydriatic 45° color photography is 71–88% and 76–99%; 94% and 69%; 100% and 79%; and 85% and 99%, respectively.29,30 The American Academy of Ophthalmology reported that there is sufficient evidence to suggest that single-field fundus photography with interpretation by trained readers can serve as a screening tool to identify patients with DR, without the need for mydriasis in the majority of cases;28 however, sensitivity and specificity values are diminished (non-mydriatic 45°: 61–78% and 85–86%; dilated 45°: 72–74% and 88%, respectively),28 and it produces a higher number of unreadable images that require further referral31 compared with seven-standard field photography.
In the Comparison Among Methods of Retinopathy Assessment (CAMRA) study, the sensitivity and specificity of non-mydriatic three-field fundus photography (45° foveal, nasal, and temporal) for detecting any DR was 81% and 94%, respectively, and 54% and 99%, respectively, for detecting STDR.32 A cross-sectional study carried out in a Thai hospital compared single-field (45° central posterior) and five-field (45° central posterior, temporal, nasal, superior, and inferior) digital non-mydriatic fundus photography and found that both were acceptable for the detection of any DR by a primary care physician (sensitivity and specificity were 70.7% and 99.3%, respectively, for single-field fundus photography, and 84.5% and 98.6%, respectively, for five-field fundus photography), although the single-field approach occasionally missed peripheral retinal lesions and underestimated the DR grade.30 Moreover, a report suggested that although single-field 45° digital non-mydriatic imaging can detect the presence of DR (sensitivity and specificity 71% and 96%), three 45° fields may be necessary for grading (sensitivity and specificity 82% and 92%),33 representing a good compromise on sensitivity, specificity, and ease.34
Digital Imaging
Digital modalities have largely superseded traditional fundoscopy and are a current focus for development in retinal screening technology. The introduction of digital technology allows fundus photography to be performed by non-ophthalmologists, with images sent to ophthalmologists or trained graders; digital copies of the images are retained and can be remotely reviewed and subsequently graded. Using smartphone-based retinal cameras with specialized adaptors, skilled operators can capture high-quality, wide-field fundus images; furthermore, these embedded systems are capable of acquisition, storage, and even analysis of images.35 However, mydriasis is necessary for optimizing sensitivity with this approach and therefore it is not feasible in all circumstances. In the CAMRA study, the sensitivity and specificity for smartphones to detect any DR was 50% and 94%, respectively, and 59% and 100%, respectively, for detecting STDR.32 However, artificial intelligence (AI)-based automated software in conjunction with a smartphone-based device has demonstrated a sensitivity and specificity for the detection of any DR of 96% and 80%, respectively, and 99% and 80%, respectively, for the detection of STDR.36 Another novel technique for retinal imaging is the miniaturized non-mydriatic wide-field fundus camera, which uses dual light sources − near infrared (for retinal guidance) and white (for color retinal imaging) − to successfully achieve reflection-free and artefact-free fundus photography; furthermore, these cameras are constructed from off-the-shelf components37 so may become an affordable solution. The FDA-approved, handheld Pictor portable LED camera offers another non-mydriatic approach for obtaining high-quality retinal images (with minimal training) from which STDR could be identified by graders with a broad level of experience.38 Unlike smartphone-based imaging, these novel approaches do not require mydriasis and are potentially the next generation of telemedicine and point-of-care assessment devices for eye diseases. Although currently available non-mydriatic cameras tend to be expensive and bulky,39 a current research focus includes the development of smaller, handheld retinal cameras to obtain fundus images without mydriasis37,38,40 and allow screening in underserved hard-to-reach communities, as demonstrated in urban slum populations.41 Another approach is through the use of healthcare kiosks located in public places, such as supermarkets and pharmacies, that already offer automated vision tests42 or screening for several chronic diseases, including diabetes.43,44 Including fully automated non-mydriatic fundus cameras in pre-existing or new, dedicated healthcare kiosks may encourage patients with diabetes to initiate opportunistic screening. This raises the question of who should fund such an initiative. Existing kiosks have been sponsored by healthcare companies, supermarkets and pharmacies, but often at a local level,42 or by employers via health insurance coverage,45 so access may be sporadic.
Screening Based on the Posterior Pole vs the Entire Retina
It was estimated that up to 15% of DR lesions and 27% of PDR lesions may lie outside of the area covered by a standard 45° field image.23 Increasing a single field of view to 60° covers 60% of the area covered by seven 30° fields and may increase the chance of detecting early retinopathy; however, the wider angle reduces magnification.46 Ultra-wide-field (UWF) imaging devices, such as the Optos P200MA/P200C47 or Optos Daytona48 (Optos Plc, Dunfermline, UK), address the limitations imposed by conventional fundus photography by broadening the view of the retina from 30° up to 200° in a single image, with a high level of sensitivity.47 The ungradable image rate per patient is lower using UWF imaging than with conventional fundus photography, leading to a reduction in the number of ungradable images overall.48 Furthermore, peripheral lesions that would not have been identified using standard Early Treatment of Diabetic Retinopathy Study (ETDRS) fields may have prognostic significance; they are suggestive of more severe DR in ~10% of patients,48 and their predominance outside the standard ETDRS field is associated with a 4.7-fold increased risk of progression to PDR.49 Using a smartphone, a lens adaptor, and a high-definition television, self-monitoring UWF retinal photography (“retinal selfie”) is currently being investigated, highlighting the improved accessibility and cost effectiveness brought by technological advances.50
Other Diagnostic Tools for DR
Retinal Fundus-Related Electrophysiological Responses
Aspects of retinal function, such as fundus-related electrophysiological responses, can vary at different stages of DR. RETeval-DR™ (LKC Technologies, Inc., Gaithersburg, MD, USA; Welch Allyn, Inc., Skaneateles Falls, NY, USA), a new handheld device for measuring oscillatory potentials,51,52 has demonstrated accuracy in detecting DR once the operator has undergone minimal training.52 The performance of RETeval-DR™ has been compared with standard seven-field fundus photography and found to be highly accurate (99%), with a very short testing time (2.3 minutes),52 and RETeval-DR™ can differentiate STDR from non-STDR quickly, without mydriasis.51,52 Furthermore, 63.5% of patients preferred RETeval-DR™ screening over other imaging techniques, compared with 22.8% who preferred digital fundus photography, which could positively impact patient adherence and aid patient management.51,52 Nevertheless, the cost of these devices is likely to be problematic for some providers.
Pupillary Light Reflexes
The pupillary light response can be used as an index of intrinsically sensitive retinal ganglion cell function, which in turn may provide insight into inner retina dysfunction in patients with diabetes. A study investigating the effects of diabetes on the various pupillary measures showed that patients with diabetes at all stages of NPDR can have abnormalities in pupil responses, such as decreased pupillary light response elicited by flashes of light under melanopsin-mediated conditions, and for patients with moderate-to-severe NPDR, under cone-mediated conditions.53 Furthermore, mean dark-adapted steady-state pupil size was significantly reduced at all stages of NPDR (p<0.001), whereas the mean light-adapted steady-state pupil size was only significantly reduced for patients with moderate-to-severe NPDR (p=0.008).53 Significant changes in mean dark-adapted pupillary re-dilation velocity were detected in patients with diabetes without DR and in those with mild and moderate NPDR and PDR (p≤0.05).54 Another study reported that reduced pupillary dilatation amplitude was detected in hyperglycemic patients with DR,55 which may assist in patient diagnosis and stratification by severity. Smartphone LEDs have been used as stimuli in combination with infrared video pupillometry,56 and now entirely iPhone-based pupillometry can provide similar results to infrared pupillometry.57 Further studies are required to determine the relative accuracy, costs, and ease of these pupillary light response tests, or a combination thereof, for sensitivity and specificity for diagnosing DR and determining its severity. Smartphone approaches are promising as they permit patients to detect DR themselves, without the need for ophthalmologists or optometrists, and instead, pupillary response recordings can be sent to an expert for interpretation.
Developments in DR Screening: Telescreening and AI
Telescreening, whereby ophthalmologists visit communities and/or digital pictures are taken and graded later by an expert, represents the single most promising innovation in DR screening for large populations. Meta-analysis suggests that telescreening reduces clinic workload, is cost effective, and can increase patient compliance when provided free of charge to remote communities.58 Telescreening approaches may include temporary mobile DR screening services whereby teams visit communities for short periods, centralized image analysis, or a combination of both.59–62 Telescreening is usually cheaper and preferred by patients compared with traditional surveillance techniques.63 Telescreening has been used in different screening programs, including the OPHDIAT® program in France;59 the Remote Outreach DR Screening Service in Australia, which increased screening rates four-fold;64 and the Sankara Nethralaya Teleophthalmology Project (SNTOP) and Aravind Teleophthalmology Network (ATN) in India, which estimated that 150 patients could be screened per day, with a single ophthalmologist making the final diagnoses remotely.65 In China, the “Lifeline Express” initiative, which consists of custom-built trains and eye centers nationwide, has successfully extended its initial service beyond cataract surgery treatment to large-scale DR screening.60
Another transformative advance in DR screening is the use of automated DR detection and AI, including automated machine learning and deep learning algorithms that are capable of recognizing DR lesions.66–68 After “training” with data sets that may include several thousand images, deep learning systems have achieved a sensitivity and specificity of ≥80%.67,69 AI has been successfully integrated into smartphone-based systems and on-site systems such as the FDA-approved IDx-DR system.36,70–72 Cheaper and accessible handheld cameras with incorporated AI will lead to a reduction in DR screening costs in a similar manner to the outsourcing and streamlining of blood tests and diagnosis, and this may be the key to the rapid assessment of large numbers of retinal images. The capturing and sharing of digital fundus photographs may also be useful in other conditions: Google AI can predict the risk of stroke using fundus photographs, suggesting that this approach may have the ability to provide standardized measurements.73
To improve access for the majority of patients with DR, telescreening is likely to be the basis of most DR screening programs in the future; however, imaging and analysis depend on equipment and training, which can be cost prohibitive, especially in communities that are not supported by centralized healthcare systems or governments.74
Strategies to Improve the Uptake of DR Screening
Despite the wealth of evidence supporting the effectiveness of DR screening, coverage is inconsistent and may be below recommended levels in certain groups, such as younger patients, those with T1D, or those in deprived areas, even in countries where systematic screening is employed.75 Screening non-attendance is not only a missed opportunity for detecting STDR, but can also result in financial consequences through the treatment of more advanced retinopathy.76 The use of telescreening presents an immense opportunity to manage the steadily increasing demand for eye care; however, challenges remain in the delivery of practical, viable, and clinically proven solutions. The cost savings of telescreening approaches are more significant when carried out on a greater scale;77 therefore, cooperation and agreement on screening approaches within nations is required to organize screening over greater areas, to ensure high standards and cost savings. The lack of DR awareness and its potential impact on sight, in addition to poor delivery of DR screening services and their associated costs, have been reported as important barriers to accessing treatment in both developing and developed countries.78–81 The following section explores how DR screening uptake could be improved.
Patient Education and Engagement
Health literacy in diabetes and its complications may be insufficiently developed for optimal participation in DR screening. Studies of the provisions of DR screening and treatment have identified a lack of awareness of the relationship between diabetes and DR until after vision is affected; furthermore, this was acknowledged by physicians as a key barrier that impacts outcomes of adults with DR.82 Improved patient education and access to clinics may increase DR screening rates and attendance at follow-up appointments, and therefore should be included in public health programs.79,80 Various studies show that educational interventions (both targeted at DR and diabetes in general) improve DR screening rates: a 2018 meta-analysis (including studies in the USA, Canada, Australia, China, and Europe) demonstrated a 5% improvement in DR screening rates after DR-specific and general diabetes educational intervention;83 an educational intervention study performed in the USA doubled the rate of ophthalmic examination achieved with a routine medical care group (from 27.3% to 54.7%);84 another study in the USA revealed that patients receiving an educational intervention and personalized letter compared with usual care (schedule letter and automated phone call) were more likely to arrange (63% vs 40%; p<0.0001) and attend their appointment (48% vs 30%; p<0.0001);85 and a study in Tanzania showed that an educational intervention and a referral for free screening improved uptake from 29% to 47%.86 Tailoring health education to high-risk subgroups, for example younger people,87,88 is a valid strategy, although the effectiveness of targeting populations based on baseline demographics remains unclear.83 Studies have shown that perceptions of barriers to DR screening can differ between patients and healthcare providers, and as such, active patient community engagement should be considered when formulating new educational programs.89 For instance, intervention mapping using patient interviews and surveys has been used to develop leaflets targeting young people with T2D,87 and direct telephone engagement with patients has been shown to increase DR screening attendance by 74% in patients with diabetes in an urban healthcare setting in the USA.90
Changes to DR Screening Service Delivery
Patients with inconvenient journeys to screening appointments are associated with delayed DR screening;91 screening and health checks performed in more conveniently located healthcare settings, such as high street dental surgeries and community pharmacy settings, may offer a solution. Community-based screening programs for various non-communicable diseases, including osteoporosis, cardiovascular disease, peripheral arterial disease, and diabetes have shown promising results for this type of intervention;92 furthermore, stakeholders were in broad support of this approach. Using their unique position, pharmacists can identify candidates for DR screening based on their medication histories and can use the screenings as an opportunity to encourage patients to seek DR care from their physicians.92 Community settings may also facilitate effective interventions, such as on-the-spot counselling and friendly reminders, that could be effective for motivating patients to self-manage their conditions. DR screening in a primary care setting by trained non-physician/ophthalmologist photographic graders may offer a further solution,93,94 provided adequate levels of sensitivity and specificity are met.19 Trained photographers can acquire the images, which can be saved and analyzed at a future date, and the uptake of automated diagnostic systems and AI may add efficiency and value to existing telescreening programs.70 Other aspects of task-sharing in DR management − such as carrying out regular follow-up appointments for those not currently showing signs of DR − could also reduce the burden on ophthalmologists.95 Adequate training underpins the success of this approach; ophthalmic personnel generally outperform non-ophthalmic personnel in DR grading, so referral to ophthalmologists must be an option when necessary.96 Infrastructure improvements, focused on increased collaboration and information sharing between providers, have the potential to increase screening uptake by reaching more patients.97 For instance, bespoke software produced by the Portuguese Diabetes Association (APDP [APDPSoft]) integrates with the Portuguese Ministry of Health systems to track screening requests and appointments, and also manages clinical data, fundus photography, and retinography reports.98,99 Automated interrogation and extraction of electronic primary care data may identify additional candidates for screening.100
Financial Incentives and Reimbursement for Screening Systems
Deprivation remains a factor in non-attendance for DR screening, even in countries with a systematic approach, such as the UK.101,102 High-income countries such as Australia and Canada report significantly lower DR screening rates and inadequate diabetes care in their remote Indigenous populations;103,104 therefore, a concerted effort is needed to screen hard-to-reach communities.105 Reimbursement of retinal screening can be complex and extra considerations such as patient selection, camera utilization, and use of non-mydriatic cameras may affect reimbursement claims.106,107 A study in Trinidad and Tobago revealed that private sector ophthalmologists performed 80% of all eye care, but only 19.3% of the adult population had private healthcare insurance, leading to significant out-of-pocket expenditure.108
Studies have investigated the impact of DR costs (real and perceived), as well as the impact of incentivizing DR screening, and identified significant predictors of decreased adherence, including when participants believed their medical insurance did not sufficiently cover the costs of diabetic eye exams, had poorly controlled blood glucose, or had only recently been diagnosed with diabetes.109 In a UK study, methods for encouraging patient engagement with DR screening were studied and it was revealed that financial incentives attracted fewer patients to screening than standard invites.110 Nevertheless, screening practices that detect DR early offer longer-term cost savings by avoiding the costs of preventable sight loss and blindness, including disability grants that could be avoided with early treatment;111 an Australian pilot telescreening program for early DR was effective and costs were competitive with Medicare reimbursement costs for eye examinations.112
Recommendations for Future Studies
The studies presented here highlight the necessity of DR screening for preventing blindness due to escalating global diabetes prevalence. Given the exponential rise of diabetes globally, the manpower needed for DR screening is likely to be outpaced, and telescreening undoubtedly has the greatest potential to transform screening. Public health programs and population-based interventions should provide appropriate levels of diagnostic accuracy within the context of cost-effective evidence-based care. The findings reported herein suggest that telescreening for DR can be successful while also reducing travel time and costs for patients with diabetes, and despite higher referral numbers owing to ungradable images, patients appear to prefer this approach, thus improving patient adherence and engagement.
To plan and feasibly implement DR screening in public health policies globally, we propose several studies to assess the extent of DR and screening best practice. To employ successful DR screening programs that are cost effective and efficient, the best approach needs to be determined; incorporating the recent advances in technology and telescreening could impact DR screening, while balancing cost, practicality, and patient preference, as well as patient outcomes. Studies should focus on developing a telescreening methodology that can be applied on a large scale and across different regions. For example, a non-mydriatic or staged mydriatic methodology that would allow evaluation of the predictive accuracy of digital imaging in different populations using digital fundus photography in three fields may offer an acceptable compromise on sensitivity and ease of execution. Other studies should include the evaluation of AI automated detection versus traditional approaches and aim to standardize the second-tier referral process for patients requiring treatment and ungradable images. Research projects exploring whether the use of handheld devices, advanced optics, and newer technology (including UWF imaging and retinal function measurements) are feasible for future large-scale telescreening would be particularly helpful in terms of ease of use, reliability, and costs. The impact of patient-driven approaches such as smartphone pupillometry and automated non-mydriatic fundus cameras situated in public places should also be studied as a means to increase patient-driven screening.
Conclusions
This review is limited to the published data available; however, it is clear that great attempts are being made worldwide in the fields of telescreening, automated detection using AI, and patient-initiated testing with smartphones and unmanned kiosks to diagnose and manage the escalating problem of diabetes and DR, despite the immense challenges with resources and infrastructure. However, despite these efforts, evidence gaps remain. Telescreening approaches and equipment need to be compared and ideally standardized, and AI and smartphone technologies need to be rigorously tested to ensure adequate sensitivity and specificity. We believe that a more standardized and collaborative approach would lead to the establishment of the best approach to DR screening practice, as well as data sharing for research purposes and cost efficiency.
In countries with inadequate primary care systems, a holistic approach to screening for diabetes is highly recommended to prevent end-organ damage in the absence of a routine screening program. This, at a minimum, should include retinal screening, as well as foot examinations, blood pressure monitoring, and urine albumin, HbA1c, and lipid testing. A collateral benefit of DR screening, which may be underappreciated, is that it can also identify other conditions, including retinal disease and other microvascular conditions.
To protect the sight of the millions of patients at risk of DR, significant investment is required. Determining the best way forward is a challenge, especially with respect to funding initiatives such as healthcare kiosks and smartphone telescreening. Whether pharmaceutical companies, supermarkets and pharmacies, insurance companies, or healthcare authorities should contribute and/or collaborate is unclear, but doing nothing is more costly, both economically and to society. It is likely that DR-related visual disabilities will increase in the coming years; therefore, an organized public health approach must be adopted, with all stakeholders cooperating to control severe visual disabilities caused by DR.
Acknowledgments
Medical writing support was provided by Aisling Koning, PhD, and Tom Priddle, DPhil, of OPEN Health Medical Communications (Choice, London, UK), funded by Boehringer Ingelheim. The research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
Funding was provided by Boehringer Ingelheim. Boehringer Ingelheim did not have a role in study design; in the analysis or interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
Disclosure
Miss Pearce is now an employee of Boehringer Ingelheim but was not when the manuscript was written. Professor Sivaprasad reports grants, non-financial support, and personal fees from Bayer grants and personal fees from Novartis, grants and personal fees from Allergan, grants and personal fees from Roche, grants and personal fees from Boehringer Ingelheim, personal fees from Heidelberg, personal fees from Oxurion, grants and personal fees from Optos, and personal fees from Apellis, outside of the submitted work. The authors report no other conflicts of interest in this work.
References
1. International Diabetes Federation. IDF Diabetes Atlas.
2. Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010;376(9735):124–136. doi:10.1016/S0140-6736(09)62124-3
3. Liew G, Michaelides M, Bunce C. A comparison of the causes of blindness certifications in England and Wales in working age adults (16–64 years), 1999–2000 with 2009–2010. BMJ Open. 2014;4(2):e004015. doi:10.1136/bmjopen-2013-004015
4. Solomon SD, Chew E, Duh EJ, et al. Diabetic retinopathy: a position statement by the American diabetes association. Diabetes Care. 2017;40(3):412–418. doi:10.2337/dc16-2641
5. Deschler EK, Sun JK, Silva PS. Side-effects and complications of laser treatment in diabetic retinal disease. Semin Ophthalmol. 2014;29(5–6):290–300. doi:10.3109/08820538.2014.959198
6. Campochiaro PA, Brown DM, Pearson A, et al. Sustained delivery fluocinolone acetonide vitreous inserts provide benefit for at least 3 years in patients with diabetic macular edema. Ophthalmology. 2012;119(10):2125–2132. doi:10.1016/j.ophtha.2012.04.030
7. Lu Q, Lu L, Chen B, Chen W, Lu P. Efficacy comparison of intravitreal injections of conbercept and ranibizumab for severe proliferative diabetic retinopathy. Can J Ophthalmol. 2019;54(3):291–296. doi:10.1016/j.jcjo.2018.06.010
8. Bolinger MT, Antonetti DA. Moving past anti-VEGF: novel therapies for treating diabetic retinopathy. Int J Mol Sci. 2016;17(9):
9. Romero-Aroca P, Navarro-Gil R, Valls-Mateu A, Sagarra-Alamo R, Moreno-Ribas A, Soler N. Differences in incidence of diabetic retinopathy between type 1 and 2 diabetes mellitus: a nine-year follow-up study. Br J Ophthalmol. 2017;101(10):1346–1351. doi:10.1136/bjophthalmol-2016-310063
10. Thomas RL, Dunstan FD, Luzio SD, et al. Prevalence of diabetic retinopathy within a national diabetic retinopathy screening service. Br J Ophthalmol. 2015;99(1):64–68. doi:10.1136/bjophthalmol-2013-304017
11. CDC. National Diabetes Statistics Report, 2020: estimates of diabetes and its burden in the United States; 2020. Available from: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf.
12. Scanlon PH. The English National Screening Programme for diabetic retinopathy 2003–2016. Acta Diabetol. 2017;54(6):515–525. doi:10.1007/s00592-017-0974-1
13. Fung MM, Yap MK, Cheng KK. Community-based diabetic retinopathy screening in Hong Kong: ocular findings. Clin Exp Optom. 2011;94(1):63–66. doi:10.1111/j.1444-0938.2010.00552.x
14. Jones S, Edwards RT. Diabetic retinopathy screening: a systematic review of the economic evidence. Diabet Med. 2010;27(3):249–256. doi:10.1111/j.1464-5491.2009.02870.x
15. Scanlon PH, Aldington SJ, Leal J, et al. Development of a cost-effectiveness model for optimisation of the screening interval in diabetic retinopathy screening. Health Technol Assess. 2015;19(74):1–116. doi:10.3310/hta19740
16. Royle P, Mistry H, Auguste P, et al. Pan-retinal photocoagulation and other forms of laser treatment and drug therapies for non-proliferative diabetic retinopathy: systematic review and economic evaluation. Health Technol Assess. 2015;19(51):
17. Owsley C, McGwin G
18. Nielsen N, Jackson C, Spurling G, Cranstoun P. Nondiabetic retinal pathology - prevalence in diabetic retinopathy screening. Aust Fam Physician. 2011;40(7):529–532.
19. National Institute for Health and Care Excellence (NICE). Type 2 diabetes in adults: management. Clinical Guideline; 2019. Available from: https://www.nice.org.uk/guidance/ng28.
20. American Diabetes Association. Standards of medical care in diabetes – 2014. Diabetes Care. 2014;37(Suppl 1):S14–S80. doi:10.2337/dc14-S014
21. Aspelund T, Thornorisdottir O, Olafsdottir E, et al. Individual risk assessment and information technology to optimise screening frequency for diabetic retinopathy. Diabetologia. 2011;54(10):2525–2532. doi:10.1007/s00125-011-2257-7
22. Gangwani RA, Lian JX, McGhee SM, Wong D, Li KK. Diabetic retinopathy screening: global and local perspective. Hong Kong Med J. 2016;22(5):486–495. doi:10.12809/hkmj164844
23. Klein R, Klein BE, Neider MW, Hubbard LD, Meuer SM, Brothers RJ. Diabetic retinopathy as detected using ophthalmoscopy, a nonmydriatic camera and a standard fundus camera. Ophthalmology. 1985;92(4):485–491. doi:10.1016/S0161-6420(85)34003-4
24. Mansberger SL, Gleitsmann K, Gardiner S, et al. Comparing the effectiveness of telemedicine and traditional surveillance in providing diabetic retinopathy screening examinations: a randomized controlled trial. Telemed J E Health. 2013;19(12):942–948. doi:10.1089/tmj.2012.0313
25. Shi L, Wu H, Dong J, Jiang K, Lu X, Shi J. Telemedicine for detecting diabetic retinopathy: a systematic review and meta-analysis. Br J Ophthalmol. 2015;99(6):823–831. doi:10.1136/bjophthalmol-2014-305631
26. Pasquel FJ, Hendrick AM, Ryan M, Cason E, Ali MK, Narayan KM. Cost-effectiveness of different diabetic retinopathy screening modalities. J Diabetes Sci Technol. 2016;10(2):301–307. doi:10.1177/1932296815624109
27. Early Treatment Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs -an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology. 1991;98(5 Suppl):786–806. doi:10.1016/S0161-6420(13)38012-9
28. Williams GA, Scott IU, Haller JA, Maguire AM, Marcus D, McDonald HR. Single-field fundus photography for diabetic retinopathy screening: a report by the American Academy of Ophthalmology. Ophthalmology. 2004;111(5):1055–1062. doi:10.1016/j.ophtha.2004.02.004
29. Lee JC, Nguyen L, Hynan LS, Blomquist PH. Comparison of 1-field, 2-fields, and 3-fields fundus photography for detection and grading of diabetic retinopathy. J Diabetes Complications. 2019;33(12):107441. doi:10.1016/j.jdiacomp.2019.107441
30. Srihatrai P, Hlowchitsieng T. The diagnostic accuracy of single- and five-field fundus photography in diabetic retinopathy screening by primary care physicians. Indian J Ophthalmol. 2018;66(1):94–97. doi:10.4103/ijo.IJO_657_17
31. Martinez J, Hernandez-Bogantes E, Wu L. Diabetic retinopathy screening using single-field digital fundus photography at a district level in Costa Rica: a pilot study. Int Ophthalmol. 2011;31(2):83–88. doi:10.1007/s10792-010-9413-9
32. Ryan ME, Rajalakshmi R, Prathiba V, et al. Comparison Among Methods of Retinopathy Assessment (CAMRA) Study: smartphone, nonmydriatic, and mydriatic photography. Ophthalmology. 2015;122(10):2038–2043. doi:10.1016/j.ophtha.2015.06.011
33. Vujosevic S, Benetti E, Massignan F, et al. Screening for diabetic retinopathy: 1 and 3 nonmydriatic 45-degree digital fundus photographs vs 7 standard early treatment diabetic retinopathy study fields. Am J Ophthalmol. 2009;148(1):111–118. doi:10.1016/j.ajo.2009.02.031
34. Aptel F, Denis P, Rouberol F, Thivolet C. Screening of diabetic retinopathy: effect of field number and mydriasis on sensitivity and specificity of digital fundus photography. Diabetes Metab. 2008;34(3):290–293. doi:10.1016/j.diabet.2007.12.007
35. Maamari RN, Keenan JD, Fletcher DA, Margolis TP. A mobile phone-based retinal camera for portable wide field imaging. Br J Ophthalmol. 2014;98(4):438–441. doi:10.1136/bjophthalmol-2013-303797
36. Rajalakshmi R, Subashini R, Anjana RM, Mohan V. Automated diabetic retinopathy detection in smartphone-based fundus photography using artificial intelligence. Eye (Lond). 2018;32(6):1138–1144. doi:10.1038/s41433-018-0064-9
37. Toslak D, Liu C, Alam MN, Yao X. Near-infrared light-guided miniaturized indirect ophthalmoscopy for nonmydriatic wide-field fundus photography. Opt Lett. 2018;43(11):2551–2554. doi:10.1364/OL.43.002551
38. Zhang W, Nicholas P, Schuman SG, et al. Screening for diabetic retinopathy using a portable, noncontact, nonmydriatic handheld retinal camera. J Diabetes Sci Technol. 2017;11(1):128–134. doi:10.1177/1932296816658902
39. Chen M, Swinney C, Chen M, Bal M, Nakatsuka A. Comparing the utility of the non-mydriatic fundus camera to the direct ophthalmoscope for medical education. Hawaii J Med Public Health. 2015;74(3):93–95.
40. Shen BY, Mukai S. A portable, inexpensive, nonmydriatic fundus camera based on the raspberry Pi(R) computer. J Ophthalmol. 2017;2017:4526243. doi:10.1155/2017/4526243
41. Wadhwani M, Vashist P, Singh SS, et al. Diabetic retinopathy screening programme utilising non-mydriatic fundus imaging in slum populations of New Delhi, India. Trop Med Int Health. 2018;23(4):405–414. doi:10.1111/tmi.13039
42. Primary Care Optometry News. Software-based vision kiosks help generate new patients; 2009. Available from: https://www.healio.com/news/optometry/20120225/software-based-vision-kiosks-help-generate-new-patients.
43. Pursuant Health. American Diabetes Association and Pursuant Health announce multi-year agreement to include diabetes risk test in national health kiosk network at pharmacies nationwide; 2016. Available from: https://pursuanthealth.com/diabetes-risk-test/.
44. Ng G, Tan SW, Tan NC. Health outcomes of patients with chronic disease managed with a healthcare kiosk in primary care: protocol for a pilot randomised controlled trial. BMJ Open. 2018;8(3):e020265. doi:10.1136/bmjopen-2017-020265
45. Kaiser Health News. Your doctor will see you in this telemedicine kiosk; 2016. Available from: https://www.medscape.com/viewarticle/865164.
46. von Wendt G, Rönnholm P, Heikkilä K, Summanen P. A comparison between one- and two-field 60 degree fundus photography when screening for diabetic retinopathy. Acta Ophthalmol Scand. 2000;78(1):14–20. doi:10.1034/j.1600-0420.2000.078001014.x
47. Silva PS, Cavallerano JD, Tolls D, et al. Potential efficiency benefits of nonmydriatic ultrawide field retinal imaging in an ocular telehealth diabetic retinopathy program. Diabetes Care. 2014;37(1):50–55. doi:10.2337/dc13-1292
48. Silva PS, Horton MB, Clary D, et al. Identification of diabetic retinopathy and ungradable image rate with ultrawide field imaging in a national teleophthalmology program. Ophthalmology. 2016;123(6):1360–1367. doi:10.1016/j.ophtha.2016.01.043
49. Silva PS, Cavallerano JD, Haddad NM, et al. Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 years. Ophthalmology. 2015;122(5):949–956. doi:10.1016/j.ophtha.2015.01.008
50. Lai KHW, Lee RPW, Yiu EPF. Ultrawide-field retinal selfie by smartphone, high-definition television, and a novel clip-on lens. Ophthalmology. 2018;125(7):1027. doi:10.1016/j.ophtha.2018.03.027
51. Al-Otaibi H, Al-Otaibi MD, Khandekar R, et al. Validity, usefulness and cost of RETeval system for diabetic retinopathy screening. Transl Vis Sci Technol. 2017;6(3):3. doi:10.1167/tvst.6.3.3
52. Maa AY, Feuer WJ, Davis CQ, et al. A novel device for accurate and efficient testing for vision-threatening diabetic retinopathy. J Diabetes Complications. 2016;30(3):524–532. doi:10.1016/j.jdiacomp.2015.12.005
53. Park JC, Chen YF, Blair NP, et al. Pupillary responses in non-proliferative diabetic retinopathy. Sci Rep. 2017;7:44987. doi:10.1038/srep44987
54. Jain M, Devan S, Jaisankar D, Swaminathan G, Pardhan S, Raman R. Pupillary abnormalities with varying severity of diabetic retinopathy. Sci Rep. 2018;8(1):5636. doi:10.1038/s41598-018-24015-9
55. Sdobnikova SV, Dorokhina N, Gupalo OD, Krivosheeva NV. Pupillary reactions and eye hemodynamics in patients with diabetes mellitus with different glycemic levels. Vestn Oftalmol. 2010;126(4):10–14.
56. Chang LY, Turuwhenua J, Qu TY, Black JM, Acosta ML. Infrared video pupillography coupled with smart phone LED for measurement of pupillary light reflex. Front Integr Neurosci. 2017;11:6. doi:10.3389/fnint.2017.00006
57. McAnany JJ, Smith BM, Garland A, Kagen SL. iPhone-based pupillometry: a novel approach for assessing the pupillary light reflex. Optom Vis Sci. 2018;95(10):953–958. doi:10.1097/OPX.0000000000001289
58. Ullah W, Pathan SK, Panchal A, et al. Cost-effectiveness and diagnostic accuracy of telemedicine in macular disease and diabetic retinopathy: a systematic review and meta-analysis. Medicine (Baltimore). 2020;99(25):e20306. doi:10.1097/MD.0000000000020306
59. Schulze-Döbold C, Erginay A, Robert N, Chabouis A, Massin P. Ophdiat®: five-year experience of a telemedical screening programme for diabetic retinopathy in Paris and the surrounding area. Diabetes Metab. 2012;38(5):450–457. doi:10.1016/j.diabet.2012.05.003
60. Wong IYH, Ni MY, Wong IOL, Fong N, Leung GM. Saving sight in China and beyond: the Lifeline Express model. BMJ Glob Health. 2018;3(4):e000766. doi:10.1136/bmjgh-2018-000766
61. Melles RB, Conell C, Siegner SW, Tarasewicz D. Diabetic retinopathy screening using a virtual reading center. Acta Diabetol. 2020;57(2):183–188. doi:10.1007/s00592-019-01392-9
62. Kalogeropoulos D, Kalogeropoulos C, Stefaniotou M, Neofytou M. The role of tele-ophthalmology in diabetic retinopathy screening. J Optom. 2020. doi:10.1016/j.optom.2019.12.004
63. Li Z, Wu C, Olayiwola JN, Hilaire DS, Huang JJ. Telemedicine-based digital retinal imaging vs standard ophthalmologic evaluation for the assessment of diabetic retinopathy. Conn Med. 2012;76(2):85–90.
64. Glasson NM, Crossland LJ, Larkins SL. An innovative australian outreach model of diabetic retinopathy screening in remote communities. J Diabetes Res. 2016;2016:1267215. doi:10.1155/2016/1267215
65. Bai VT, Murali V, Kim R, Srivatsa SK. Teleophthalmology-based rural eye care in India. Telemed J E Health. 2007;13(3):313–321. doi:10.1089/tmj.2006.0048
66. Bellemo V, Lim G, Rim TH, et al. Artificial intelligence screening for diabetic retinopathy: the real-world emerging application. Curr Diab Rep. 2019;19(9):72. doi:10.1007/s11892-019-1189-3
67. Ramachandran N, Hong SC, Sime MJ, Wilson GA. Diabetic retinopathy screening using deep neural network. Clin Exp Ophthalmol. 2018;46(4):412–416. doi:10.1111/ceo.13056
68. Heydon P, Egan C, Bolter L. et al. Prospective evaluation of an artificial intelligence-enabled algorithm for automated diabetic retinopathy screening of 30 000 patients. Br J Ophthalmol. 2020. doi:10.1136/bjophthalmol-2020-316594
69. Ting DSW, Cheung CY, Lim G, et al. Development and validation of a deep learning system for diabetic retinopathy and related eye diseases using retinal images from multiethnic populations with diabetes. JAMA. 2017;318(22):2211–2223. doi:10.1001/jama.2017.18152
70. van der Heijden AA, Abramoff MD, Verbraak F, van Hecke MV, Liem A, Nijpels G. Validation of automated screening for referable diabetic retinopathy with the IDx-DR device in the Hoorn Diabetes Care System. Acta Ophthalmol. 2018;96(1):63–68. doi:10.1111/aos.13613
71. Natarajan S, Jain A, Krishnan R, Rogye A, Sivaprasad S. Diagnostic accuracy of community-based diabetic retinopathy screening with an offline artificial intelligence system on a smartphone. JAMA Ophthalmol. 2019;137(10):1182–1188. doi:10.1001/jamaophthalmol.2019.2923
72. Bhaskaranand M, Ramachandra C, Bhat S, et al. The value of automated diabetic retinopathy screening with the eyeart system: A study of more than 100,000 consecutive encounters from people with diabetes. Diabetes Technol Ther. 2019;21(11):635–643. doi:10.1089/dia.2019.0164
73. Peng L. Assessing cardiovascular risk factors with computer vision; 2018. Available from: https://ai.googleblog.com/2018/02/assessing-cardiovascular-risk-factors.html.
74. James M, Turner DA, Broadbent DM, Vora J, Harding SP. Cost effectiveness analysis of screening for sight threatening diabetic eye disease. BMJ. 2000;320(7250):1627–1631. doi:10.1136/bmj.320.7250.1627
75. Millett C, Dodhia H. Diabetes retinopathy screening: audit of equity in participation and selected outcomes in South East London. J Med Screen. 2006;13(3):152–155. doi:10.1258/096914106778440608
76. Waqar S, Bullen G, Chant S, Salman R, Vaidya B, Ling R. Cost implications, deprivation and geodemographic segmentation analysis of non-attenders (DNA) in an established diabetic retinopathy screening programme. Diabetes Metab Syndr. 2012;6(4):199–202. doi:10.1016/j.dsx.2012.08.009
77. Bjørvig S, Johansen MA, Fossen K. An economic analysis of screening for diabetic retinopathy. J Telemed Telecare. 2002;8(1):32–35. doi:10.1258/1357633021937433
78. Al-Shakarchi FI. Blindness in iraq: leading causes, target patients, and barriers to treatment. Middle East Afr J Ophthalmol. 2011;18(3):199–203. doi:10.4103/0974-9233.84044
79. Keenum Z, McGwin G
80. Lewis K, Patel D, Yorston D, Charteris D. A qualitative study in the United Kingdom of factors influencing attendance by patients with diabetes at ophthalmic outpatient clinics. Ophthalmic Epidemiol. 2007;14(6):375–380. doi:10.1080/09286580701375195
81. Cavan D, Makaroff LE, da Rocha Fernandes J, et al. Global perspectives on the provision of diabetic retinopathy screening and treatment: survey of health care professionals in 41 countries. Diabetes Res Clin Pract. 2018;143:170–178. doi:10.1016/j.diabres.2018.07.004
82. Cavan D, Makaroff L, da Rocha Fernandes J, et al. The Diabetic Retinopathy Barometer Study: global perspectives on access to and experiences of diabetic retinopathy screening and treatment. Diabetes Res Clin Pract. 2017;129:16–24. doi:10.1016/j.diabres.2017.03.023
83. Lawrenson JG, Graham-Rowe E, Lorencatto F, et al. Interventions to increase attendance for diabetic retinopathy screening. Cochrane Database Syst Rev. 2018;1:CD012054.
84. Basch CE, Walker EA, Howard CJ, Shamoon H, Zybert P. The effect of health education on the rate of ophthalmic examinations among African Americans with diabetes mellitus. Am J Public Health. 1999;89(12):1878–1882. doi:10.2105/AJPH.89.12.1878
85. Zangalli CS, Murchison AP, Hale N, et al. An education- and telephone-based intervention to improve follow-up to vision care in patients with diabetes: a prospective, single-blinded, randomized trial. Am J Med Qual. 2016;31(2):156–161. doi:10.1177/1062860614552670
86. Mumba M, Hall A, Lewallen S. Compliance with eye screening examinations among diabetic patients at a Tanzanian referral hospital. Ophthalmic Epidemiol. 2007;14(5):306–310. doi:10.1080/09286580701272079
87. Lake AJ, Browne JL, Abraham C, et al. A tailored intervention to promote uptake of retinal screening among young adults with type 2 diabetes - an intervention mapping approach. BMC Health Serv Res. 2018;18(1):396. doi:10.1186/s12913-018-3188-5
88. Orton E, Forbes-Haley A, Tunbridge L, Cohen S. Equity of uptake of a diabetic retinopathy screening programme in a geographically and socio-economically diverse population. Public Health. 2013;127(9):814–821. doi:10.1016/j.puhe.2013.04.015
89. Lu Y, Serpas L, Genter P, Anderson B, Campa D, Ipp E. Divergent perceptions of barriers to diabetic retinopathy screening among patients and care providers, Los Angeles, California, 2014–2015. Prev Chronic Dis. 2016;13:E140. doi:10.5888/pcd13.160193
90. Walker EA, Schechter CB, Caban A, Basch CE. Telephone intervention to promote diabetic retinopathy screening among the urban poor. Am J Prev Med. 2008;34(3):185–191. doi:10.1016/j.amepre.2007.11.020
91. Macon C, Carrier H, Janczewski A, Verger P, Casanova L. Effect of automobile travel time between patients’ homes and ophthalmologists’ offices on screening for diabetic retinopathy. Telemed J E Health. 2018;24(1):11–20. doi:10.1089/tmj.2016.0271
92. Law MG, Komura S, Murchison AP, Pizzi LT. Pharmacy staff opinions regarding diabetic retinopathy screenings in the community setting: findings from a brief survey. Am Health Drug Benefits. 2013;6(9):548–552.
93. Rosses APO, Ben AJ, Souza CF, et al. Diagnostic performance of retinal digital photography for diabetic retinopathy screening in primary care. Fam Pract. 2017;34(5):546–551. doi:10.1093/fampra/cmx020
94. Daskivich LP, Vasquez C, Martinez C
95. Shah M, Noor A, Deverell L, Ormsby GM, Harper CA, Keeffe JE. Task sharing in the eye care workforce: screening, detection, and management of diabetic retinopathy in Pakistan. A case study. Int J Health Plann Manage. 2018;33(3):627–636. doi:10.1002/hpm.2508
96. Facey K, Cummins E, MacPherson K, Morris A, Reay L, Slattery J. Organisation of services for diabetic retinopathy screening. Health Technology Assessment Report 1. Glasgow: Health Technology Board for Scotland; 2002.
97. Strutton R, Du Chemin A, Stratton IM, Forster AS. System-level and patient-level explanations for non-attendance at diabetic retinopathy screening in Sutton and Merton (London, UK): a qualitative analysis of a service evaluation. BMJ Open. 2016;6(5):e010952. doi:10.1136/bmjopen-2015-010952
98. Dutra Medeiros M, Mesquita E, Gardete-Correia L, et al. First incidence and progression study for diabetic retinopathy in Portugal, the RETINODIAB study: evaluation of the screening program for Lisbon region. Ophthalmology. 2015;122(12):2473–2481. doi:10.1016/j.ophtha.2015.08.004
99. Dutra Medeiros M, Mesquita E, Papoila AL, Genro V, Raposo JF. First diabetic retinopathy prevalence study in Portugal: RETINODIAB Study–evaluation of the screening programme for Lisbon and Tagus Valley region. Br J Ophthalmol. 2015;99(10):1328–1333. doi:10.1136/bjophthalmol-2015-306727
100. Scanlon PH, Provins EK, Craske S, et al. Updating diabetic retinopathy screening lists using automatic extraction from GP patient records. J Med Screen. 2013;20(3):111–117. doi:10.1177/0969141313505747
101. Leese GP, Boyle P, Feng Z, Emslie-Smith A, Ellis JD. Screening uptake in a well-established diabetic retinopathy screening program: the role of geographical access and deprivation. Diabetes Care. 2008;31(11):2131–2135. doi:10.2337/dc08-1098
102. Moreton RBR, Stratton IM, Chave SJ, Lipinski H, Scanlon PH. Factors determining uptake of diabetic retinopathy screening in Oxfordshire. Diabet Med. 2017;34(7):993–999. doi:10.1111/dme.13350
103. Moynihan V, Turner A. Coordination of diabetic retinopathy screening in the Kimberley region of Western Australia. Aust J Rural Health. 2017;25(2):110–115. doi:10.1111/ajr.12290
104. Oster RT, Virani S, Strong D, Shade S, Toth EL. Diabetes care and health status of First Nations individuals with type 2 diabetes in Alberta. Can Fam Physician. 2009;55(4):386–393.
105. Spurr S, Bullin C, Bally J, Trinder K, Khan S. Nurse-led diabetic retinopathy screening: a pilot study to evaluate a new approach to vision care for Canadian Aboriginal peoples. Int J Circumpolar Health. 2018;77(1):1422670. doi:10.1080/22423982.2017.1422670
106. Phan AD, Koczman JJ, Yung CW, Pernic AA, Doerr ED, Kaehr MM. Cost analysis of teleretinal screening for diabetic retinopathy in a county hospital population. Diabetes Care. 2014;37(12):e252–253. doi:10.2337/dc14-0929
107. French DD, Behrens JJ, Jackson KL, et al. Payment reform needed to address health disparities of undiagnosed diabetic retinopathy in the City of Chicago. Ophthalmol Ther. 2017;6(1):123–131. doi:10.1007/s40123-016-0072-4
108. Braithwaite T, Winford B, Bailey H, et al. Health system dynamics analysis of eyecare services in Trinidad and Tobago and progress towards Vision 2020 Goals. Health Policy Plan. 2018;33(1):70–84. doi:10.1093/heapol/czx143
109. Sheppler CR, Lambert WE, Gardiner SK, Becker TM, Mansberger SL. Predicting adherence to diabetic eye examinations: development of the Compliance with Annual Diabetic Eye Exams Survey. Ophthalmology. 2014;121(6):1212–1219. doi:10.1016/j.ophtha.2013.12.016
110. Judah G, Darzi A, Vlaev I, et al. Financial disincentives? A three-armed randomised controlled trial of the effect of financial Incentives in Diabetic Eye Assessment by Screening (IDEAS) trial. Br J Ophthalmol. 2018;102(8):1014–1020. doi:10.1136/bjophthalmol-2017-311778
111. Khan T, Bertram MY, Jina R, Mash B, Levitt N, Hofman K. Preventing diabetes blindness: cost effectiveness of a screening programme using digital non-mydriatic fundus photography for diabetic retinopathy in a primary health care setting in South Africa. Diabetes Res Clin Pract. 2013;101(2):170–176. doi:10.1016/j.diabres.2013.05.006
112. Lee SJ, McCarty CA, Taylor HR, Keeffe JE. Costs of mobile screening for diabetic retinopathy: a practical framework for rural populations. Aust J Rural Health. 2001;9(4):186–192. doi:10.1046/j.1038-5282.2001.00356.x
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
