Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
A Report of Eruptive Pruritic Papular Porokeratosis Treated with Abrocitinib
Received 5 June 2023
Accepted for publication 5 August 2023
Published 14 August 2023 Volume 2023:16 Pages 2223—2227
DOI https://doi.org/10.2147/CCID.S424310
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Jiali Xia, Guan Jiang
Department of Dermatology, The Affiliated Hospital of Xuzhou Medical University, Xuzhou, 221002, People’s Republic of China
Correspondence: Guan Jiang, Department of Dermatology, The Affiliated Hospital of Xuzhou Medical University, 99 West Huai Hai Road, Xuzhou, Jiangsu, 221002, People’s Republic of China, Tel +86 181 6877 7336, Email [email protected]
Abstract: Eruptive pruritic papular porokeratosis (EPPP) is a subtype of porokeratosis (PK). EPPP is characterized by intense itching and challenging to treat in some cases. Herein, for the first time, a case of successful relief of EPPP treated with abrocitinib was reported. A 75-year-old male with a 60-year history of PK suddenly experienced severe itching in the past 6 months. The patient’s use of antihistamines, prednisone, vitamin A derivatives, vitamin D derivatives, and tripterygium wilfordii showed poor efficacy. Abrocitinib is a highly selective JAK1 inhibitor, and JAK1 appears to play a crucial role in pruritic diseases. Abrocitinib can quickly relieve itching within 24 hours. Before abrocitinib treatment, the visual analog scale (VAS) score was 10, the 12-item pruritus severity scale (12-PSS) score was 19, and the dermatology life quality index (DLQI) score was 18. Abrocitinib (100 mg) was taken orally once a day. After 1 month of oral administration of abrocitinib, the skin lesions gradually subsided, pruritus was relieved, and no adverse side effects occurred. The VAS, 12-PSS, and DLQI scores of the patient decreased to 2, 3, and 4, respectively. This report suggests a potential therapeutic benefit of abrocitinib in managing EPPP. However further investigations with larger sample sizes and controlled studies are necessary to validate its efficacy as a clinical therapy.
Keywords: eruptive pruritic papular porokeratosis, porokeratosis, abrocitinib, pruritus, itch, JAK inhibitors
Introduction
Eruptive pruritic papular porokeratosis (EPPP) is a subtype of porokeratosis (PK). It manifests clinically in three distinct phases: years of asymptomatic PK rash, sudden exacerbation with severe itching, and eruptive papules that resolve after a few months. This condition, which is noted for its intense pruritus, poses significant treatment challenges for many patients. Herein, a case of successful relief of EPPP treated with abrocitinib was reported for the first time. Written informed consent was signed by the patient.
Case Presentation
The subject is a 75-year-old male diagnosed with EPPP, who has a 60-year history of PK. For the last 6 months, the rash deepened and increased in color, with intense pruritus. Several family members of the patient had PK. The patient’s face, neck, trunk, and extremities had densely keratinized papules measuring 2–5 mm in diameter, ranging from dark red to dark brown in color. These papules exhibited old central atrophy, and they were well-defined, slightly raised, and partially covered with thin scales (Figures 1a and b). The patient had no history of tumor disease. Skin biopsy demonstrated cornoid lamella formation, hypogranulosis, and vacuolation in keratinocytes. Moreover, lymphocyte infiltration was observed around dermal vessels (Figures 2a and b). After the patient’s medical history, skin lesions, and the results from skin pathology reports were evaluated, EPPP diagnosis was confirmed.
The patient was administered with various medications, including ketotifen fumarate, levocetirizine dihydrochloride, and ebastine. The dose of prednisone acetate was adjusted from 15, 20, and 30 mg to 40 mg once daily for 3 months. The patient was also prescribed tripterygium wilfordii (20 mg three times daily) or cyclosporine A (100 mg twice a day orally) for 3 months. He used glucocorticoids and vitamin D derivatives externally. Unfortunately, these treatments failed to alleviate the patient’s itching symptoms. The patient’s initial visual analog scale (VAS) score was 10, the 12-item pruritus severity scale (12-PSS) score was 19, and the dermatology life quality index (DLQI) score was 18. After informed consent was obtained from the patient and his family, a comprehensive series of tests and examinations was performed, including a complete blood routine, liver and kidney function, coagulation function, hepatitis B and C screening, tumor marker screening, a tuberculin test, and imaging of the chest and abdomen via computed tomography. No anomalies were detected in any of these evaluations.
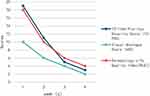
Subsequently, the patient was prescribed a daily dose of 100 mg abrocitinib, administered orally. The patient did not take any additional medications during this period. After 1-month oral administration of abrocitinib, the skin lesions gradually subsided (Figure 1c). In addition, the patient reported relief from pruritus, with no adverse side effects detected. The subsequent VAS, 12-PSS, and DLQI scores of the patient decreased to 2, 3, and 4, respectively (Figure 3). The patient was subsequently advised to attend follow-up appointments.
Discussion
Kanzaki1 in Japan first reported three cases of EPPP in 1992 and considered it a heteromorphic form of superficial disseminated type. Itch is one of the characteristic symptoms of EPPP. It is an unpleasant subjective sensation that stimulates the desire to scratch and one of the main symptoms of many skin diseases and systemic disorders. When itch becomes severe or chronic (>6 weeks) or occurs in the context of an underlying medical condition, it has a significant effect on the patient’s wellbeing. The chronicity of pruritus can affect sleep, mood, and personal relationships, thus significantly reducing quality of life. The current treatment modalities of EPPP include glucocorticoids, antihistamines, vitamin A derivatives, 5-fluorouracil, cryotherapy, and carbon dioxide laser, all demonstrating a certain degree of efficacy.2 However, some patients with severe pruritus experience unsatisfactory therapeutic outcomes.
The mechanism of pruritus in EPPP remains unclear. Immunofluorescent staining of patients with EPPP revealed a notable presence of IL-31 cells in the injured skin, heightened dermal deposition of periostin,3 enhanced epidermal expression of TSLP, and increased eosinophil and basophil infiltration4 compared with non-injured skin. IL-31, a known itch-inducing cytokine, binds to IL-31 receptor A and oncostatin M receptor, activating JAK (Janus kinases) 1 and 2 and STATs 1, 3, and 5 to continue the pruritic inflammatory response.5 Abnormal proliferating keratinocytes in the lesions of patients with EPPP can secrete large amounts of TSLP, promoting a Th2 immune response, which upregulates periostin and IL-31. This cascade of events could be a leading cause of intractable pruritus in this condition.3
Abrocitinib is a highly selective oral JAK1 inhibitor. The signaling cytokines mediated by JAK1 include IL-4, IL-13, IL-31, and TSLP. Abrocitinib inhibits IL-31 by up to 85%, reaches the peak of blood drug concentration within 1 hour, and is potent for rapidly relieving itching.6 Lymphocyte and eosinophil infiltration can be observed in EPPP. This lymphocytic inflammation and eosinophilic activity may be instrumental in the progression of skin injury. The possible rationale for employing abrocitinib in EPPP treatment lies in its ability to mitigate inflammation through immunomodulatory and its anti-inflammatory properties. Thus, JAK1 inhibitor represented by abrocitinib may be a better choice for treating EPPP.
The use of abrocitinib is off-label, which is only approved for atopic dermatitis at daily doses of either 200 or 100 mg. Abrocitinib is a highly selective JAK1 inhibitor, affecting the other three JAK subtypes to a lesser extent. This elevated selectivity reduces the effect on the normal physiological functions of other JAK subtypes, thus minimizing the off-target effects. Reports showed the use of tofacitinib in treating EPPP.7 However, considering that abrocitinib is a highly selective JAK1 inhibitor, whereas tofacitinib is a non-selective JAK inhibitor, the significant differences between these two generations of selective agents are safety and efficacy.8 Selective inhibitors are safer than nonselective inhibitors, and abrocitinib has a better safety profile than tofacitinib. Abrocitinib is known to block cytokine receptors that involve JAK1 as part of their signaling mechanism while does not appear to significantly affect cytokine receptors that use JAK2/JAK2 or TYK2/JAK2 combinations. Thus, the risk of adverse events (AEs), such as anemia/neutropenia, appears to be lower.9 In addition, JAK1 seems to play a crucial role in pruritic diseases. Abrocitinib can provide rapid relief from itching within 24 hours, and its speed of itch relief is superior to that of tofacitinib.
The safety of JAK inhibitors, such as abrocitinib, has been a subject of ongoing discussion. The most frequently observed treatment-related AEs include headaches, diarrhea, and nausea. A recent analysis of clinical trials involving abrocitinib indicated a notably low incidence of non-melanoma skin cancer, other malignancies, or cardiovascular events (less than 0.5 cases per 100 PY).2 This finding suggested that abrocitinib exhibits controllable long-term safety and tolerance over short-term oral administration at an appropriate dose. Abrocitinib has been successfully used to treat Hailey–Hailey disease,10 lichen sclerosus,11 primary cutaneous lichenoid amyloidosis,12 Lichen planus,13 and prurigo nodosum.14 One case reported a transient increase in platelet and total cholesterol, and three uncircumcised male patients reported erectile tension, which was then relieved after 4 weeks without any other AEs.
The precise mechanism by which abrocitinib ameliorates EPPP remains undetermined, and prior reports on EPPP treatment are scarce. This article delineates the efficacy of abrocitinib in treating EPPP, indicating the potential role of JAK1 in EPPP pathogenesis and the prospect of JAK1 inhibitors in EPPP treatment. While the findings are encouraging, further studies are warranted to validate them. This work represents the first case of using a JAK1 inhibitor to satisfactorily treat EPPP.
Conclusion
For the first time, abrocitinib was successfully used to treat an elderly male patient diagnosed with EPPP. Despite the absence of specific research elucidating the precise mechanism of abrocitinib in the management of EPPP, it serves to offer clinicians a novel option and perspective in terms of drug selection and therapeutic strategies.
Data Sharing Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Consent Statement
Written informed consent was obtained from the patient to have the case details and associated images published. Institutional approval was not required.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
No funding or sponsorship was received for this study or publication of this article.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kanzaki T, Miwa N, Kobayashi T, Ogawa S. Eruptive pruritic papular porokeratosis. J Dermatol. 1992;19(2):109–112. doi:10.1111/j.1346-8138.1992.tb03190.x
2. Simpson EL, Silverberg JI, Nosbaum A, et al. Integrated safety analysis of abrocitinib for the treatment of moderate-to-severe atopic dermatitis from the phase II and phase III clinical trial program. Am J Clin Dermatol. 2021;22(5):693–707. doi:10.1007/s40257-021-00618-3
3. Hashimoto T, Moriyama Y, Satoh T. Linear porokeratosis with severe itch accompanied by lesional upregulation of interleukin 31, thymic stromal lymphopoietin, and periostin. Eur J Dermatol. 2021;31(4):570–572. doi:10.1684/ejd.2021.4083
4. Awatani K, Hashimoto T, Satoh T. Eruptive pruritic papular porokeratosis accompanied by eosinophilic and basophilic infiltrate with upregulation of epidermal CCL26/eotaxin-3 and thymic stromal lymphopoietin. J Dermatol. 2021;48(8):e382–e383. doi:10.1111/1346-8138.15949
5. Furue M. Regulation of skin barrier function via competition between AHR axis versus IL-13/IL-4‒JAK‒STAT6/STAT3 axis: pathogenic and therapeutic implications in atopic dermatitis. J Clin Med. 2020;9(11):3741. doi:10.3390/jcm9113741
6. Gooderham MJ, Forman SB, Bissonnette R, et al. Efficacy and safety of oral janus kinase 1 inhibitor abrocitinib for patients with atopic dermatitis: a phase 2 randomized clinical trial. JAMA Dermatol. 2019;155(12):1371–1379. doi:10.1001/jamadermatol.2019.2855
7. Mu X, Li W, Zhang M, et al. Successful treatment of eruptive pruritic papular porokeratosis in the elderly with tofacitinib: a case report. Clin Cosmet Investig Dermatol. 2023;16:1741–1747. doi:10.2147/CCID.S412495
8. Shawky AM, Almalki FA, Abdalla AN, Abdelazeem AH, Gouda AM. A comprehensive overview of globally approved JAK inhibitors. Pharmaceutics. 2022;14(5):1001. doi:10.3390/pharmaceutics14051001
9. Akada H, Akada S, Hutchison RE, Sakamoto K, Wagner KU, Mohi G. Critical role of Jak2 in the maintenance and function of adult hematopoietic stem cells. Stem Cells. 2014;32(7):1878–1889. doi:10.1002/stem.1711
10. Li Y, Jiang Y, Sun J. Improvement of Hailey-Hailey disease with abrocitinib. Clin Exp Dermatol. 2023;48(5):532–533. doi:10.1093/ced/llad023
11. Bao C, Xu Q, Xiao Z, et al. Abrocitinib as a novel treatment for lichen sclerosus. Br J Dermatol. 2023;189(1):136–138. doi:10.1093/bjd/ljad129
12. Bai J, Su W, Fang H, Qiao J. Treatment of primary cutaneous lichenoid amyloidosis with abrocitinib: a pilot study in two cases. Int J Dermatol. 2023. doi:10.1111/ijd.16698
13. Solimani F, Mesas-Fernández A, Dilling A, et al. The Janus kinase 1 inhibitor abrocitinib for the treatment of oral lichen planus. J Eur Acad Dermatol Venereol. 2023;37. doi:10.1111/jdv.19069
14. Vander Does A, Yosipovitch G. Failure of dupilimab with severe prurigo nodularis that responded well to abrocitinib. Dermatitis. 2023. doi:10.1089/derm.2022.0065
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.