Back to Journals » Drug Design, Development and Therapy » Volume 16
A Real-World Study on the Effect of Imrecoxib for Patients with Axial Spondyloarthritis
Authors Zong HX, Xu SQ , Wang JX , Chu YR, Chen K , Wang C, Tong WQ, Wang XL
Received 30 May 2022
Accepted for publication 13 August 2022
Published 22 August 2022 Volume 2022:16 Pages 2755—2765
DOI https://doi.org/10.2147/DDDT.S376406
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Tuo Deng
He-xiang Zong, Sheng-qian Xu, Jian-xiong Wang, Yi-ran Chu, Ke-ming Chen, Cong Wang, Wan-qiu Tong, Xi-le Wang
Department of Rheumatology and Immunology, The First Affiliated Hospital of Anhui Medical University, Hefei, People’s Republic of China
Correspondence: Sheng-qian Xu, Department of Rheumatology and Immunology, The First Affiliated Hospital of Anhui Medical University, No. 218, Ji-xi Road, Hefei, Anhui, 230022, People’s Republic of China, Tel +86 551 62922261, Fax +86 551 62923040, Email [email protected]
Purpose: Non-steroidal anti-inflammatory drugs (NSAIDs) have generally been viewed as first-line therapy for axial spondyloarthritis (axSpA). Imrecoxib is a selective COX-2 inhibitor developed independently in China. At present, only one single-center RCT trial has shown that imrecoxib is equally effective as celecoxib in treating axSpA. Based on real-world data, our study aims to explore the efficiency of imrecoxib and TNF inhibitor (TNFi) combined with imrecoxib in treating axSpA.
Patients and Methods: A total of 163 patients with axSpA who had more than two follow-up records in 6 months and treated with imrecoxib/celecoxib/TNFi combined with imrecoxib/TNFi combined with celecoxib from the First Affiliated Hospital of Anhui Medical University SpA Real World Database (AHSpA) were selected for analysis of our study. The linear mixed model was used to compare efficacy indexes before and after treatment and between different groups, adjust baseline measurement value and follow-up time. The Kaplan–Meier survival analysis was used to identify the differences in cumulative clinical remission rates between groups with different treatment at the follow-up period.
Results: Results showed that after treatment ASDAScrp was slightly improved in imrecoxib group and celecoxib group within 6 months (p < 0.05). CRP, ESR, BASDAI, ASDAScrp, BASFI, occiput to wall distance and finger floor distance all significantly improved in TNFi combined with imrecoxib group and TNFi combined with celecoxib group within 6 months (all p < 0.05). According to the Kaplan–Meier survival curve and Log rank test analysis, the clinical remission rate was not significantly different between different treatment during 24-month follow-up (all p > 0.05).
Conclusion: ASDAScrp improved slightly within 6 months after treatment with imrecoxib, and TNFi combined with imrecoxib significantly improved multiple effect indexes in axSpA patients. The efficacy of imrecoxib and celecoxib in the treatment of axSpA is equivalent. Also, they have the same efficacy after being combined with TNFi.
Keywords: axial spondyloarthritis, imrecoxib, celecoxib, TNF inhibitor
Introduction
Spondyloarthritis (SpA) was a chronic inflammatory rheumatic disease consisting of different phenotypic subgroups with standard genetic, radiological, and clinical features, including ankylosing spondylitis (AS), psoriatic arthritis (PsA), juvenile-onset spondyloarthritis (JSpA), inflammatory bowel disease (IBD)-associated arthritis, reactive arthritis and undifferentiated spondyloarthritis.1 Based on the patients’ clinical presentation, SpA was classified as axial spondyloarthritis (axSpA) or peripheral spondyloarthritis (pSpA). The International Society for the Assessment of Spondyloarthritis (ASAS) definition of axSpA included SpA that had developed bony structural damage (radiographic axSpA), detectable in the sacroiliac joint, and SpA that has not yet formed structural damage noticeable by X-ray scanning (non-radiographic axial SpA, or nr-axSpA).1
The symptoms of axSpA generally appear between the ages of 20 and 30.2 The global prevalence of axSpA has been estimated to range from 0.3% to 1.4% in various surveys.3,4 In China, Liao et al5 found that the prevalence rate of axSpA was 0.78% in the Chinese Han population, while Tong et al6 found that the frequency of axSpA was 0.34% in a university in southern China. More than 4 million Chinese citizens, primarily young and middle-aged males, were affected by axSpA, putting a significant medical load on China’s limited economic resources.7
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen, diclofenac, and celecoxib were shown to be particularly efficient in relieving back pain and stiffness in axSpA patients and were thus suggested as first-line treatment.8 Traditional disease-modifying anti-rheumatic medications (DMARDs) failed to treat axial involvement in axSpA. Treatment with biologic DMARDs (bDMARDs) was indicated for individuals with active disease who had not responded to NSAIDs.9 The results demonstrated that bDMARD treatment successfully attained long-term control and reduced complications in individuals with axSpA.10 Celecoxib was a selective COX-2 inhibitor that had been proven to decrease radiographic development in spine imaging changes,11 and imrecoxib was a new, moderately selective COX-2 inhibitor which works similarly to celecoxib, developed by a Chinese pharmaceuticals firm and authorized in 2011. Its analgesic efficacy in osteoarthritis has been verified. Currently, only one single-center RCT study has shown that Imrecoxib has comparable efficacy to celecoxib in treating SpA.12 Based on real-world data, this study aimed to investigate the effectiveness of the combination of Imrecoxib and a TNF inhibitor (TNFi) for axSpA.
Patients and Methods
Patients
This was a retrospective observational cohort study investigating a cohort of axSpA patients from “the First Affiliated Hospital of Anhui Medical University SpA Real World Database (AHSpA)” from April 2020 to October 2020. This is a large teaching hospital in a city in the South of China, with a population of approximately 9000,000, which also receives referrals from other centres. Medical practices in the hospital are representative of hospitals in the same class in China. Once patients are initiated on treatment they are monitored at regular intervals during therapy by a team of Rheumatologist. To minimize the selection bias, all patients fulfilled the 2009 ASAS classification criteria for axSpA,1 and were treated with imrecoxib/celecoxib/TNFi combined with imrecoxib/TNFi combined with celecoxib (n=163) with more than 2 follow-up records during 6 months, were considered eligible for the study. Exclusion criteria included patients over 60 years old, patients with other rheumatic diseases, such as rheumatoid arthritis (RA), systemic vasculitis, system lupus erythematosus (SLE), other diffuse connective tissue diseases, and so on, patients using anticoagulants or antiplatelet aggregation drugs, patients with abnormal liver function, renal function, coagulation function, or anemia, patients to be allergic to painkillers and NSAIDs, patients with a history of drug, alcohol abuse, and mental illness, any investigational drug used within one month of screening.
The dosage of imrecoxib or celecoxib was 0.2g qn or 0.4g qn. TNFi treatment comprised etanercept subcutaneous injection, 50 mg/w, or adalimumab subcutaneous injection, 40 mg/2w. The study methodology was approved by Committee of the First Affiliated Hospital of Anhui Medical University, and signed informed permission was acquired from all individuals before participation, in accordance with the Declaration of Helsinki principles.
Clinical Data Collection
Patients’ baseline characteristics included age, sex, body mass index (BMI), calculated as the ratio of body weight (kg) to the square of height (m), smoking history (yes or no), presenting history of SpA, family history of SpA, and human leucocyte antigen B27. C-reactive protein (mg/L) and erythrocyte sedimentation rate (mm/h) were measured and recorded as biological markers of inflammation at baseline and subsequent treatment visits. Ankylosing Spondylitis Disease Scores based on CRP (ASDAScrp), the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), Functional Index (BASFI), Modified Schöber’s Test (cm), finger floor distance (cm), chest expansion (cm), and occiput to wall distance (cm) were used to assess disease activity, core symptoms, functions, and mobility (cm). In addition, ASDAScrp was calculated according to the “0.12 * Back Pain + 0.06 * Duration of Morning Stiffness + 0.11 * Patient Global + 0.07 * Peripheral Pain/Swelling + 0.58 * Ln (CRP+1)” formula.
Follow-Up Data
The effect of different treatments on clinical outcomes was defined during the follow-up period using the ASDAScrp computation. Clinical remission was defined as ASDAScrp < 1.3, whereas clinical non-remission was classified as ASDAScrp ≥ 1.3. At baseline, 3, 6, 9, 12, 18, and 24 months, remission status was assessed. We extracted data about disease duration (month) from clinical non-remission to remission, date of stopping visiting, or April 2022.
Statistical Analysis
Results were analyzed using SAS 9.4 and Graph Pad Prism 8. Continuous data with a normal distribution were described as mean and standard deviation (SD), skewed data was expressed using the median and quartile method, and nominal variables were represented as frequencies (percentage). The Shapiro–Wilk test was used to determine if the distribution was normal. A linear mixed model was employed to adjust baseline measurement value and follow-up time to evaluate efficacy indices before and after treatment and between different groups. The Kaplan–Meier survival analysis determined the differences in cumulative clinical remission rates between groups with different treatments during the follow-up period. Statistical significance was defined as a P value less than 0.05.
Results
Patient Characteristics
Of 900 patients with 1761 follow-up notes, 163 fulfilled entry criteria and were treated with imrecoxib/celecoxib/TNFi combined with imrecoxib/TNFi combined with celecoxib with more than 2 follow-up records during 6 months. In addition, 141 patients in clinical no-remission at baseline and treated with imrecoxib/celecoxib/TNFi combined with imrecoxib/TNFi combined with celecoxib were included in the survival analysis (Figure 1).
Patient Demographics and Clinical Characteristics
The patients’ demographics and clinical characteristics are shown in Table 1. Out of 163 patients, 19 cases were treated with imrecoxib, 39 with celecoxib, 45 with TNFi combined with imrecoxib, and 60 with TNFi combined with celecoxib. Of these patients, 77.3% (n = 126) were male, and the median duration of disease was 3.0 (1.0–6.0) years. Age ranged from 13 to 56 years, with a median age of 27.0 (22.0–35.0), BMI (22.27 ± 4.51) kg/m2, 62 patients (38.0.0%) had a history of smoking, 23 patients (14.1%) had a family history of SpA, 136 patients (83.4%) were HLA-B27 positive, and 26 patients (16.0%) under clinical remission.
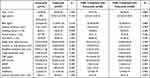 |
Table 1 Clinical Characteristics at Baseline |
There were no significant differences in patients’ demographics and clinical characteristics between the imrecoxib and celecoxib groups (P>0.05). At the same time, there were no significant differences in patient demographics and clinical characteristics between the TNFi combined with imrecoxib and TNFi combined with celecoxib groups (P>0.05) (Table 1).
Comparison of Effect Changes of Four Groups Before and After Treatment Within 6 Months
After treatment, ASDAScrp in imrecoxib group and celecoxib group was slightly improved than those before treatment (P<0.05), chest expansion in celecoxib group and TNFi combined with imrecoxib were higher than those before treatment (P<0.05), and modified Schöber’s test in TNFi combined with celecoxib were higher than those before treatment (P<0.05). CRP, ESR, BASDAI, ASDAScrp, BASFI, occiput to wall distance and finger floor distance all significantly improved than those before treatment in TNFi combined with imrecoxib group and TNFi combined with celecoxib group within 6 months (all P<0.05) (Table 2).
 |
Table 2 The Curative Effect Changes of Four Groups Within 6 Months |
Comparison of Effect Changes Between the Four Groups Within 6 Months
Result between different treatment showed that there was no significant difference in the improvement of efficacy indexes (ESR, CRP, BASDAI, ASDAScrp, BASFI, occiput to wall distance, finger floor distance) between imrecoxib group and celecoxib group within 6 months of treatment (all P>0.05) (Figure 2A), and there was no significant difference in the improvement of efficacy indexes (ESR, CRP, BASDAI, ASDAScrp, BASFI, occiput to wall distance, finger floor distance) between TNFi combined with imrecoxib group and TNFi combined with celecoxib group within 6 months (all p>0.05) (Figure 2B).
Comparison of Cumulative Clinical Remission Rates Among Different Treatment Groups
A total of 141 patients were censored as being in “clinical no-remission”. According to the Kaplan–Meier survival curve and Log rank test analysis, the clinical remission rate was not significantly different between patients treated with imrecoxib and celecoxib (long-rank p=0.980) (Figure 3), imrecoxib and TNFi combined with imrecoxib (long-rank p=0.057) (Figure 4), TNFi combined with imrecoxib and TNFi combined with celecoxib (long-rank p=0.137) (Figure 5), celecoxib and TNFi combined with celecoxib (long-rank p=0.296) (Figure 6) during 24 month follow-up.
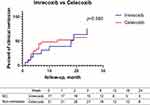 |
Figure 3 Kaplan–Meier curve comparing the probability of clinical remission between patients treated with imrecoxib and celecoxib during 24 month follow-up. |
 |
Figure 4 Kaplan–Meier curve comparing the probability of clinical remission between patients treated with imrecoxib and TNFi combined with imrecoxib during 24 month follow-up. |
 |
Figure 5 Kaplan–Meier curve comparing the probability of clinical remission between patients treated with TNFi combined with imrecoxib and TNFi combined with celecoxib during 24 month follow-up. |
 |
Figure 6 Kaplan–Meier curve comparing the probability of clinical remission between patients treated with celecoxib and TNFi combined with celecoxib during 24 month follow-up. |
Discussion
AxSpA was a chronic progressive, systemic inflammatory rheumatic disease affecting the axial skeleton and peripheral joints, entheses, and internal organs. In early adulthood, the disease presented with an insidious onset of back pain, morning stiffness and loss of physical function along with disease progression.13,14 Its pathological characteristics were synovial hyperplasia, lymphoid infiltration, and pannus formation, which would lead to bone erosion and cartilage destruction, eventually cause bone ankylosis, and seriously affect the daily life of patients. This was an important reason for the decline and disability of young and middle-aged male labor force in China. The fundamental pathogenesis of axSpA included axial inflammation, bone degradation, and new bone development; therefore, inhibiting new bone formation was crucial to therapy.15 Inflammation, fat deposition, and osteophyte in axSpA patients were interrelated, interactive, and relatively independent processes. Inflammation was the most important initial damage feature, which might lead to either bone destruction or new bone development.16 Therefore, anti-inflammatory analgesia was also the main direction of axSpA treatment.17
In recent years, international organizations had provided updated management recommendations to define the aims of axial SpA treatment as improving quality of life through control of symptoms and inflammation, preventing structural deterioration, and maintaining function and social participation.18,19 NSAIDs were highly recommended as the first-line therapy for symptom management in patients with active axSpA by the Asia Pacific League of Associations for Rheumatology (APLAR) in 2018.10 NSAIDs have the potential to enhance the outcome of axSpA, including pain alleviation, disease activity, and physical function, as well as to delay the progression of imaging.11 However, the effects of different NSAIDs might be different. In terms of mechanism, NSAIDs’ anti-inflammatory effects are due to an inhibitory impact on cyclooxygenase (COX) activity. COX is primarily classified as COX-1 and COX-2; NSAIDs inhibit COX-2 at the site of inflammation, resulting in therapeutic benefits, and COX-1 in the gastric mucosa, resulting in gastric damage.20–22 Imrecoxib, a new and moderately selective COX-2 inhibitor, reduces inflammation and discomfort by inhibiting the expression of COX-2 messenger ribonucleic acid (mRNA).23 Imrecoxib has a selective inhibitory impact on COX-1 and COX-2 in vitro, with the inhibitory effect on COX-2 stronger than COX-1.21 Compared with traditional NSAIDs drugs, imrecoxib has significantly fewer side effects on the digestive and cardiovascular systems. Celecoxib was one of the most generally used selective COX-2 inhibitor in the world for the treatment of axSpA, with good efficacy. Previous studies show that imrecoxib has non-inferior pain-relieving efficacy compared to celecoxib in arthropathy patients and oral surgical patients,12,21,24 meanwhile the proportions of patients who experienced gastrointestinal complication, cardiovascular events, or new-onset hypertension were lower in imrecoxib patients than in celecoxib patients.22
Imrecoxib was the first COX-2 selective inhibitor with independent intellectual property rights of Chinese pharmaceutical enterprises which played an important role in the treatment of axSpA. At present, there were few international reports on the therapeutic efficacy of imrecoxib in axSpA, only one RCT study confirmed that the efficacy of imrecoxib and celecoxib was equivalent.12 According to this randomized, double-blind, prospective study, both imrecoxib and celecoxib might considerably improve axSpA patients’ pain, disease activity, and function, as well as lower MRI sacroiliac joint inflammation. These findings showed that imrecoxib had similar analgesic and anti-inflammatory effects to celecoxib. It enhanced patient function and quality of life and perhaps delayed disease progression as revealed on imaging. In patients with axSpA, the effectiveness of imrecoxib and celecoxib was equivalent, according to the findings of our real-world investigation. A linear mixed model was utilized to compare efficacy indicators before and after treatment, as well as between groups, and to adjust baseline measurement indexes and follow-up duration. The findings revealed that ASDAScrp improved slightly in both groups after 6 months of treatment, with no statistically significant differences.
In a 6-week randomized, double-blind, placebo-controlled trial in France, the celecoxib groups showed greater reductions in pain (VAS) and functional impairment (BASFI) than the placebo group (mean changes in pain and functional impairment were −27 ± 30 [P = 0.0068] and −12 ± 22 [P = 0.0006, respectively). For pain intensity, the ratio of celecoxib effect to ketoprofen was 1.30 (95% CI 0.98–1.62), and for functional impairment, it was 1.98 (95% CI 0.80–3.96). The percentage of patients in the celecoxib group who improved by at least 50% (48%) was very near to the predicted (50%) and substantially different from the placebo (20%) (P = 0.001).25 In 2006, another 12-week randomized, double-blind, placebo-controlled study showed that celecoxib 200 mg qd and 400 mg qd were efficacious in treating signs and symptoms of AS. The results in the celecoxib group were significantly different from those in the placebo group (improvements in least-squares mean pain intensity (VAS), disease activity (VAS), and BASFI scores [P ≤ 0.001]) at Week 12 and the interim timepoints, Weeks 1, 3, and 6.26 However, different from previous studies, ESR, CRP, BASDAI, BASFI, occipital wall distance, and finger ground distance were not significantly improved before and after treatment with imrecoxib and celecoxib, which might be related to the short follow-up time and the small number of cases. It was necessary to further expand the sample size, prolong the observation time, and conduct multi-center clinical research.
Biological DMARDs (bDMARDs) are strongly recommended by both the 2016 ASAS/EULAR and the 2018 APLAR in patients with active disease who have failed to respond to two different NSAIDs. bDMARDs were specifically suggested for active disease described by BASDAI and ASDAScrp.10,19 The American Society of Rheumatology (ACR), the Spondylitis Association of America (SAA), and the Spondyloarthritis Research and Treatment Network (SPARTAN) published updated recommendations in 2019 that strongly recommended TNFi treatment over non-TNFi treatment in adults with active AS who were taking NSAIDs[9]. Because many patients stopped using NSAIDs after starting TNF inhibitors due to improved symptom control,27 there was no evidence of the effect of combination treatment on axSpA. In this 6-month, real-world study, TNFi combined with imrecoxib and TNFi combined with celecoxib were efficacious in improving the signs and symptoms of axSpA, as assessed by disease activity (ASDAScrp, BASDAI), physical function (BASFI) scores, and inflammatory indicators (ESR, CRP). And there was no significant difference in the improvement of efficacy indexes (ESR, CRP, BASDAI, ASDAScrp, BASFI, occiput to wall distance, finger floor distance) between two groups. The addition of NSAIDs to TNFi in patients with AS was linked with considerably reduced radiographic development in a dose-related manner at four years, according to results presented at EULAR 2018. For no NSAID, low dosage NSAID, and high dose NSAID, the mean difference in mSASSS between TNFi usage and no TNFi use after four years was 0.50 (P=0.38), −1.24 (P<0.001), and −3.31 (P<0.001), respectively. In conjunction with TNFi usage, celecoxib was linked with the highest decrease in radiographic progression, which was meaningful at both two and four years. At two and four years, the mean difference in mSASSS between TNFi and no TNFi usage for celecoxib was −3.98 (P<0.001) and −4.69 (P<0.001), respectively.28 Therefore, our and Gensler L’s studies suggested that TNFi and NSAIDs might have synergistic therapeutic effects, whether in reducing disease activity or delaying radiographic progress.
Treat-to-target (T2T) was a new management approach for SpA that was endorsed by an international task committee in 2012 and modified in 2017.17,29 Clinical remission should be the treatment objective in this strategy, while low disease activity might be an option. AS Disease Activity Score Inactive Disease (ASDAS-ID), low BASDAI with normal C-reactive protein (CRP) level, or ASAS partial remission (ASAS-PR) were the most common indicators of clinical remission.29,30 Inactive disease (ASDAS-ID, ASDAS < 1.3), moderate disease activity (1.3 ≤ ASDAS ≤ 2.1), high disease activity (2.1 ≤ ASDAS ≤ 3.5), and very high disease activity (ASDAS > 3.5) were the ASDAS cut-offs for disease activity stages.31 This real-world study defined ASDAScrp < 1.3 as clinical remission and ASDAScrp ≥ 1.3 as clinical non-remission. In order to explore the difference of clinical remission rate of axSpA patients with different treatment (imrecoxib/celecoxib/ TNFi combined with imrecoxib/TNFi combined with celecoxib), we conducted a survival analysis for 24 months on 141 patients with active disease at baseline. Our result showed that the clinical remission rate were not significantly different between patients treated with imrecoxib and celecoxib, imrecoxib and TNFi combined with imrecoxib, TNFi combined with imrecoxib and TNFi combined with celecoxib, celecoxib and TNFi combined with celecoxib. Therefore, imrecoxib and celecoxib, TNFi combined with imrecoxib and imrecoxib had similar effects on clinical remission.
Some limitations need to be taken into account when interpreting the results of our study. First, we focused on effectiveness rather than safety outcomes, this results thus provide no direct safety assessment from within the same study population. Second, because this was a real-world study, the size of our study population was relatively small, and there were some data missing and cases lost to follow-up, therefore, selection bias may be present. In the future, we need to expand the sample size, prolong the observation time, and add the research on the radiology progress and safety of imrecoxib and celecoxib in patients with AS.
Conclusion
This study demonstrated that ASDAScrp improved slightly within 6 months after treatment with imrecoxib, and TNFi combined with imrecoxib significantly improved multiple effect indexes in axSpA patients. The efficacious in disease activity, physical function, inflammatory indicators, and clinical remission rate of imrecoxib and celecoxib in the treatment of axSpA was equivalent. Also, the efficacy of TNFi combined with imrecoxib and TNFi combined with celecoxib in the treatment of axSpA was equivalent.
Acknowledgments
We would like to thank all the patients with axial spondyloarthritis and professionals who participated in this study.
Funding
The work received financial supports from the Wu Jieping Medical Foundation (Grant No.320.6750. 2020-03-4).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Rudwaleit M, van der Heijde D, Landewé R, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68(6):777–783. doi:10.1136/ard.2009.108233
2. Poddubnyy D, Sieper J, Akar S, et al. Characteristics of patients with axial spondyloarthritis by geographic regions: PROOF multicountry observational study baseline results. Rheumatology. 2021;4:keab901.
3. Sieper J, Poddubnyy D. Axial spondyloarthritis. Lancet. 2017;390(10089):73–84. doi:10.1016/S0140-6736(16)31591-4
4. Bohn R, Cooney M, Deodhar A, Curtis JR, Golembesky A. Incidence and prevalence of axial spondyloarthritis: methodologic challenges and gaps in the literature. Clin Exp Rheumatol. 2018;36:263–274.
5. Liao ZT, Pan YF, Huang JL, et al. An epidemiological survey of low back pain and axial spondyloarthritis in a Chinese Han population. Scand J Rheumatol. 2009;38(6):455–459. doi:10.3109/03009740902978085
6. Tong F, Lv Q, Li A, et al. An epidemiological study of the prevalence rate of inflammatory back pain and axial spondyloarthritis in a university in the south of China. Clin Rheumatol. 2018;37(11):3087–3091. doi:10.1007/s10067-018-4175-2
7. Man S, Ji X, Wang Y, et al. Add-on effects of conventional synthetic disease-modifying anti-rheumatic drugs in ankylosing spondylitis: data from a real-world registered study in China. Med Sci Monit. 2020;26:e921055. doi:10.12659/MSM.921055
8. Braun J, van den Berg R, Baraliakos X, et al. 2010 update of the ASAS/EULAR recommendations for the management of ankylosing spondylitis. Ann Rheum Dis. 2011;70:896–904. doi:10.1136/ard.2011.151027
9. Ward MM, Deodhar A, Gensler LS, et al. 2019 update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and treatment network recommendations for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritis. Arthritis Rheumatol. 2019;71(10):1599–1613. doi:10.1002/art.41042
10. Tam LS, Wei JC, Aggarwal A, et al. 2018 APLAR axial spondyloarthritis treatment recommendations. Int J Rheum Dis. 2019;22(3):340–356. doi:10.1111/1756-185X.13510
11. Wanders A, Heijde D, Landewé R, et al. Nonsteroidal antiinflammatory drugs reduce radiographic progression in patients with ankylosing spondylitis: a randomized clinical trial. Arthritis Rheum. 2005;52(6):1756–1765.
12. Gao GM, Li YM, Zheng XL, et al. The efficacy of imrecoxib and celecoxib in axial spondyloarthritis and their influence on serum dickopff-related Protein 1 (DKK-1) levels. Med Sci Monit. 2017;23:2985–2992. doi:10.12659/MSM.901727
13. Bal S, Bal K, Turan Y, et al. Sexual functions in ankylosing spondylitis. Rheumatol Int. 2011;31(7):889–894. doi:10.1007/s00296-010-1406-5
14. Webers C, Essers I, Ramiro S, et al. Gender-attributable differences in outcome of ankylosing spondylitis: long-term results from the outcome in Ankylosing Spondylitis international study. Rheumatology. 2016;55(3):419–428. doi:10.1093/rheumatology/kev340
15. Navarro-Compán V, Sepriano A, El-Zorkany B. Axial spondyloarthritis. Ann Rheum Dis. 2021;80(12):1511–1521. doi:10.1136/annrheumdis-2021-221035
16. Dougados M, Demattei C, van den Berg R, et al. Rate and predisposing factors for sacroiliac joint radiographic progression after a two-year follow-up period in recent-onset spondyloarthritis. Arthritis Rheumatol. 2016;68(8):1904–1913. doi:10.1002/art.39666
17. Smolen JS, Schöls M, Braun J, et al. Treating axial spondyloarthritis and peripheral spondyloarthritis, especially psoriatic arthritis, to target: 2017 update of recommendations by an international task force. Ann Rheum Dis. 2018;77(1):3–17. doi:10.1136/annrheumdis-2017-211734
18. Ward MM, Deodhar A, Akl EA, et al. American College of Rheumatology/Spondylitis Association of America/ Spondyloarthritis Research and Treatment Network 2015 recommendations for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritis. Arthritis Rheumatol. 2016;68:282–298. doi:10.1002/art.39298
19. van der Heijde D, Ramiro S, Landewé R, et al. 2016 update of the ASAS‐EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis. 2017;76(6):978–991. doi:10.1136/annrheumdis-2016-210770
20. Mitchell JA, Warner TD. Cyclo-oxygenase-2: pharmacology, physiology, biochemistry and relevance to NSAID therapy. Br J Pharmacol. 1999;128(6):1121–1132. doi:10.1038/sj.bjp.0702897
21. Jiang Y, Qi L, Liu J, et al. Analgesic efficacy of imrecoxib for postoperative pain following oral surgery: a prospective randomized, active-controlled, non-inferiority trial. Ann Transl Med. 2021;9(6):469. doi:10.21037/atm-21-264
22. Meng Q, Zhang Z, Li F, et al. The prescription patterns and safety profiles of oral non-steroidal anti-inflammatory drugs in China: an 8-year real-life analysis. Ann Palliat Med. 2021;10(2):2224–2237. doi:10.21037/apm-20-2356
23. Chen XH, Bai JY, Shen F, et al. Imrecoxib: a novel and selective cyclooxygenase 2 inhibitor with anti-inflammatory effect. Acta Pharmacol Sin. 2004;25(7):927–931.
24. Sun X, Zhen X, Hu X, et al. Cost-utility analysis of imrecoxib compared with celecoxib for patients with osteoarthritis. Ann Transl Med. 2021;9(7):575. doi:10.21037/atm-21-290
25. Dougados M, Béhier JM, Jolchine I, et al. Efficacy of celecoxib, a cyclooxygenase 2-specific inhibitor, in the treatment of ankylosing spondylitis: a six-week controlled study with comparison against placebo and against a conventional nonsteroidal antiinflammatory drug. Arthritis Rheum. 2001;44(1):180–185. doi:10.1002/1529-0131(200101)44:1<180::AID-ANR24>3.0.CO;2-K
26. Barkhuizen A, Steinfeld S, Robbins J, et al. Celecoxib is efficacious and well tolerated in treating signs and symptoms of ankylosing spondylitis. J Rheumatol. 2006;33(9):1805–1812.
27. Dougados M, Wood E, Combe B, et al. Evaluation of the nonsteroidal anti-inflammatory drug-sparing effect of etanercept in axial spondyloarthritis: results of the multicenter, randomized, double-blind, placebo-controlled SPARSE study. Arthritis Res Ther. 2014;16:481. doi:10.1186/s13075-014-0481-5
28. Gensler L, Reveille J, Lee M, et al. High dose nonsteroidal AntiInflammatory drugs (NSAIDs) and tumor necrosis factor inhibitor use results in less radiographic progression in ankylosing spondylitis – a longitudinal analysis [abstract]. Arthritis Rheumatol. 2016;68(Suppl 10):2481–2482.
29. Smolen JS, Braun J, Dougados M, et al. Treating spondyloarthritis, including ankylosing spondylitis and psoriatic arthritis, to target: recommendations of an international task force. Ann Rheum Dis. 2014;73:6–16. doi:10.1136/annrheumdis-2013-203419
30. Nam EJ, Lee WK. Early improvements in disease activity indices predict long-term clinical remission suggested by the treat-to-target strategy in patients with ankylosing spondylitis receiving TNF-α inhibitor treatment. J Clin Med. 2021;10(18):4279. doi:10.3390/jcm10184279
31. Machado PM, Landewe R, Heijde DV. Assessment of SpondyloArthritis international S. Ankylosing Spondylitis Disease Activity Score (ASDAS): 2018 update of the nomenclature for disease activity states. Ann Rheum Dis. 2018;77:1539–1540. doi:10.1136/annrheumdis-2018-213184
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


