Back to Journals » International Medical Case Reports Journal » Volume 15
A Rare Case of Intestinal Tuberculosis with Chronic Partial Small Bowel Obstruction in a 37-Year-Old Ethiopian Man
Authors Aregawi AB , Alem AT , Girma A
Received 6 September 2022
Accepted for publication 3 December 2022
Published 14 December 2022 Volume 2022:15 Pages 725—733
DOI https://doi.org/10.2147/IMCRJ.S388269
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Ronald Prineas
Alazar Berhe Aregawi,1 Alemwosen Teklehaimanot Alem,2 Abdulkerim Girma3
1Department of Surgery, Hawassa University Comprehensive Specialized Hospital, Hawassa University, Hawassa, Sidama, Ethiopia; 2Department of Pathology, Hawassa University Comprehensive Specialized Hospital, Hawassa University, Hawassa, Sidama, Ethiopia; 3Department of Radiology, Yanet Internal Medicine Specialized Centre, Hawassa, Sidama, Ethiopia
Correspondence: Alazar Berhe Aregawi, Tel +251911914624, Email [email protected]; [email protected]
Abstract: Tuberculosis (TB) is a chronic granulomatous inflammatory disease that affects any part of our body. TB is a significant problem in developing countries. Intestinal TB accounts for 2% of TB cases worldwide. Terminal ileum and cecum are the two commonly affected regions because of abundant lymphoid tissue, physiologic stasis, limited digestive activity and increased fluid and electrolyte absorption rate. Intestinal obstruction is the leading complication of intestinal TB, and it occurs because of intestinal luminal narrowing, multiple strictures or adhesions. The clinical presentation of patients with intestinal TB and post-TB intestinal obstruction is non-specific. It can be acute, chronic, or acute on chronic. Uncomplicated cases of intestinal TB can be managed medically. Surgery is reserved for complicated cases of intestinal TB, which includes peritonitis, intestinal obstruction and perforations. Here, we present a 37-year-old man who presented with long-standing, intermittent crampy abdominal pain and vomiting. He was diagnosed with chronic partial small bowel obstruction secondary to possibly small bowel carcinoma. We did segmental ileal resection and end-to-end ileo-ileal anastomosis. Postoperatively, the histopathology result turned out to be intestinal TB. This case report aims to make physicians aware of the rare condition of small bowel obstruction secondary to intestinal TB. Clinicians need to have a high index of suspicion in any patient with long-standing symptoms of partial obstruction and consider surgery and anti-TB once diagnosed.
Keywords: intestinal TB, abdominal TB, gastrointestinal TB, granulomatous inflammation
Introduction
Tuberculosis (TB) is a chronic granulomatous inflammatory disease that affects any part of our body. The lungs, bones, intestine, and lymphatic tissue are commonly affected regions. TB is a significant problem in developing countries.1,2 The incidence of TB has been on the rise in the developed world in the past decade due to the surge of HIV infection, the influx of immigrants from the developing world and the increasing use of Immunosuppressive therapy.1–4
Abdominal TB is the sixth most common form of extra-pulmonary TB after lymphatic, genitourinary, bone and joints, miliary and meningeal TB. It accounts for 0.6–0.8% of all forms. Relative to pulmonary TB, extra-pulmonary TB, particularly gastrointestinal TB, is a neglected problem.2,6–8 A report from Ethiopia found that abdominal TB is the most typical form of extra-pulmonary TB, only second to TB lymphadenitis.9 Abdominal TB refers to TB of the gastrointestinal tract, peritoneum, mesentery, abdominal lymph nodes, liver, spleen, and pancreas. The commonest sites of abdominal TB are the gastrointestinal tract/65–78%/, peritoneum and mesenteric lymph nodes.3,6,10–13
Intestinal TB accounts for 2% of TB cases worldwide. Intestinal TB is common in young individuals, like the other forms of TB. More than 70% of the cases are younger than 40 years.3,6,7,10,12,14,15 The Gastrointestinal involvement has declined to 25% after the advent of anti –TB treatment.16 Gastrointestinal TB can occur anywhere from the mouth to the anus. Terminal ileum and cecum are the two commonly affected regions because of abundant lymphoid tissue, physiologic stasis, limited digestive activity and increased fluid and electrolyte absorption rate.10,11,13,15,17,18 On gross appearance, there are three types of lesions of intestinal TB: ulcerative (60%), hypertrophic/hyperplastic (10%), and ulcero-hypertrophic types (30%). The hypertrophic type is the less frequent form that causes luminal narrowing and intestinal obstruction.5,6,12,15,19
Severe complications of gastrointestinal TB include intestinal strictures, obstruction, perforation and bleeding. Intestinal obstruction is the leading complication of intestinal TB, and it occurs because of intestinal luminal narrowing, multiple strictures or adhesions. Intestinal obstruction secondary to intestinal TB is an uncommon cause of mechanical obstruction.2,3,8,14,19
The clinical presentation of patients with intestinal TB and post-TB intestinal obstruction is non-specific. It can be acute, chronic, or acute on chronic. The presentation can range from mere abdominal pain to features of peritonitis or intestinal obstruction. This makes clinical diagnosis very difficult. Preoperative diagnosis of intestinal TB is challenging, particularly in resource-limited settings.1,3,6,11,13,16,17,19
Uncomplicated cases of intestinal TB can be managed medically.1,8,15,16 Moreover, surgery is reserved for complicated cases of intestinal TB, which includes peritonitis, intestinal obstruction and perforations. However, the decision is challenging because of high morbidity and mortality.1,9,11 Intestinal obstruction is the most common complication, often due to multiple and long strictures which do not respond to medical treatment.9,12 The type of surgery depends on the intraoperative findings, which include Stricturoplasty, perforation repair with or without a protective stoma, segmental small bowel resection, and a bypass as in ileotransversostomy, right hemicolectomy, the release of adhesions or simple ileostomy.8,9,17
This case report aims to make physicians aware of the rare condition of small bowel obstruction secondary to intestinal TB. Physicians need to have a high index of suspicion in any patient with long-standing symptoms of partial obstruction and consider surgery and anti-TB once diagnosed. Up to now, we did not find a single published case report of similar case in our country.
Case Description
We present a case of a 37-year-old male who came to Yanet internal medicine speciality centre, Hawassa, Sidama,Ethiopia. He presented with intermittent crampy abdominal pain of 3 months duration. He complained of occasional abdominal distension and intermittent vomiting of ingested matter occasionally with bilious content. He had constipation but had no failure to pass faeces or flatus. In addition, he had easy fatigability, loss of appetite and unquantified significant weight loss. The patient reported that he had the above symptoms for the last 3 years but the symptoms have worsened in the last 3 months prior to his current presentation.
He had no diarrhea or cough.
His past medical history is unremarkable.
On physical examination, he looked acutely sick.
On V/S (Vital Sign) PR (Pulse rate)-104 bpm RR (Respiratory rate)-20 bpm T (Temperature)-ATT (Afebrile to touch) BP (Blood pressure)-100/70 mmHg.
On HEENT- he had slightly pale conjunctiva.
On abdominal examination- the abdomen looked soft, which moved with respiration; there was no visible peristalsis, no area of tenderness, and DRE (Digital rectal examination)-normal.
On investigation.
Complete blood count (CBC)- White blood cell count (WBC)=6.5x103/uL Granulocyte=73% Lymphocyte=15%.
- Hemoglobin (Hgb)=8.4 g/dl Hematocrit (HCT)-27.9.
- Platelet (Plt)= 295×103/uL
Blood group and Rh= o+.
FBS (Fasting blood sugar), BUN (Blood urea nitrogen), Creatinine, ALP, AST, ALT are all normal.
Serum Na, K+, Cl− were in the normal limits.
On imaging.
CXR (Chest x ray) was normal.
Abdominal Ultrasound - There was a short segment of small bowel mass like asymmetric wall thickening measuring 4.5cm by 2.2 cm over the LUQ (Left upper quadrant) with a maximum wall thickness of 1.2cm. There were multiple adjacent mesenteric lymphadenopathies, the largest 1.1cm. The proximal small bowel was distended up to 5cm with collapsed distal bowel. The conclusion was, short segment small bowel wall thickening with luminal stenosis and features of partial SBO (Small bowel obstruction) and mesenteric lymphadenopathies, and small bowel carcinoma was considered as differential diagnosis, and Abdominal CT (Computed tomography) was recommended.
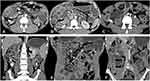
On Abdominal CT there were multi-focal short and long segment symmetric wall thickening of small bowel loops, which was marked in the left lower quadrant narrowing the lumen with proximal bowel loops dilatation and shouldering. There were also multi-focal luminal narrowing (constrictions) of the involved small bowel loops with associated focal wall thickening. Small mesenteric lymph nodes were noted in the left lower quadrant small bowel mesentery with adjacent mesenteric fat stranding and internal hypoattenuation in keeping with central necrosis (see Figure 1).
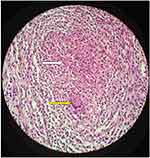
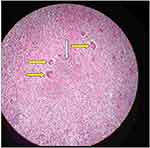
The patient was admitted with the consideration of Inflammatory bowel disease (IBD) and was given IV Ceftriaxone and Hydrocortisone and kept on maintenance fluid for 36hrs. After Small bowel Carcinoma was entertained, he was transferred to the surgical side. Because of a blood shortage, he was transfused with only 1 unit of X-matched blood and taken to OR (Operation room) for exploratory laparotomy. Under GA (General anesthesia) and ETT (Endotracheal tube) abdomen was cleaned and draped, then entered through a vertical midline incision, there was a distended small bowel about 200cms away from the ligamentum trietz, and the distended segment was about 100cm long, and there were three constrictions nearly obstructing the lumen which were a few centimeters apart. There were scant shooty mesenteric lymph nodes, there was no fat stranding, and the rest of the bowel looked normal. So we did segmental resection and end-to-end ileo-ileal anastomosis (See Figures 2 and 3). The site of anastomosis was about 100cm proximal to the ileocecal junction. After thorough lavage, the wound closed in layers, and the count was correct. The patient had a smooth postoperative course and was discharged on the third postoperative day. He returned to the outpatient clinic after 2 weeks with the pathology result. The microscopic description of the Pathology report stated: Sections from the intestinal lesions and mesenteric lymph nodes revealed nodular aggregates of epitheloid cells surrounded by mixed inflammatory cells and scattered Langhans type giant cells with areas of central caseous necrosis. That was histomorphologically consistent with Tuberculosis (See Figures 4–9). He was doing well and started on anti TB medication. He came to follow-up at two and seven months postoperatively and he was doing fine with all the symptoms resolved.
 |
Figure 2 The resected segment, the small artery forceps are pointing at the sites of constrictions. |
 |
Figure 3 The same picture with Figure 2 but a different view. |
 |
Figure 4 Gross picture 1: Resected segment of small bowel: grey white to grey brown outer surface with areas of constrictions (blue Arrows). |
 |
Figure 5 Gross Picture 2: Opened up bowel segment at the areas of constrictions to show areas of hypertrophic mucosa with near total lumen obstruction (blue arrows) and mucosal ulcer (white arrow). |
 |
Figure 6 Microphotograph 1: Low power view: Section taken from ulcerated mucosa showing intense inflammation and a granuloma (white arrows). |
 |
Figure 9 Microphotograph 4: Low power view: Section taken from mesenteric lymph node showing a granuloma (nodule indicated by the white arrow) with central necrosis (yellow arrow). |
Discussion
The most common location of intestinal TB is the ileocaecal region, accounting for about 52–85%.2,7,17 Intestinal TB resembles other inflammatory and neoplastic conditions in the intestine.18 Because of this, the rate of misdiagnosis reaches 50–70%, even in countries where TB is endemic.2–4,14,18 This would result in treating TB patients with steroids and biological agents, which has the potential to cause disease progression and causes increased morbidity and mortality. It is challenging to distinguish between intestinal TB and Crohn’s disease. They have similar characteristics in clinical presentation, radiologic appearances, operative findings, and histologic examinations.2,4,12,14,18,20 In our case, the patient was admitted with clinical impression of inflammatory bowel disease for which he was started on Hydrocortisone. However, after 48 hours of admission, an abdominal CT was done and the possibility of small bowel carcinoma was entertained then after.
Abdominal TB has an insidious course and lacks specific clinical, laboratory, or radiologic features, making its diagnosis challenging.2,7,20 Abdominal pain is the most common presentation, followed by nausea/vomiting.2,14,18,21 Our patient had long-standing intermittent abdominal cramps and vomiting. Moreover, proper treatment is delayed because the correct diagnosis is not established timely, which increases morbidity and mortality.7,21 In addition, our patient had repeated prior visits to nearby health facilities, but there was no improvement. According to many reports, the duration of symptoms of abdominal TB could last more than six months before the patient visits health facilities.2,22 Our patient presented with a 3 year symptom which worsened over the last 3 months. Intestinal obstruction resulting from tuberculosis accounts for 12–60%.13 In India, about 3–20% of all intestinal obstructions are due to abdominal TB.13,14
Routine laboratory investigations, like CBC, and ESR, have a minimal role in diagnosing abdominal TB. Clinical and laboratory findings only suggest the chronicity of the disease. Incidence of anemia reaches up to 80% in patients with TB.2,7,10,13 Our patient was as well anemic.
Classic imaging findings of abdominal TB are ascites, thickening of the peritoneum, mesentery, or bowel wall, and lymphadenopathy.1,7,23 Our case had an abdominal ultrasound and CT, but abdominal TB was not considered as a DDx even though there was a symmetric bowel wall thickening, luminal stenosis and mesenteric LAP on the description of the imaging report; instead small bowel tumor was entertained.
There are reports which suggest contrast studies of the gastrointestinal tract are beneficial in diagnosing intestinal TB.1,23 So, clinical decision and a high index of suspicion play a significant role in making the diagnosis of Intestinal TB.17,24
A definitive diagnosis of abdominal TB is made by identifying mycobacterium TB from tissue and/or depicting caseating granulomas at a histopathologic examination. Mycobacterial culture takes about six weeks, so histologic confirmation is crucial for the management.2,7,13,21 In Ethiopia, culture is available for research purpose and multidrug TB resistance centers.6 The rate of diagnosis of intestinal TB from a histopathologic specimen is 54%, and microbiologic confirmation has been made in 18–50% of cases.15 There are different ways of harvesting a specimen for histopathology. Diagnostic laparotomy can be done for clinically suspected cases of intestinal TB when endoscopy or laparoscopy is not feasible.8,9 In our case, a definitive diagnosis of intestinal TB was made on histopathology examination of the post-surgical specimen.
In the absence of complications, most patients with abdominal TB respond to the standard anti-TB medical treatment.13,15,16 However, according to many authors, surgery best manages intestinal obstruction secondary to intestinal TB. Because the Pathology in intestinal TB is often a hypertrophic lesion, the response to medical management is not very good. Moreover, surgery provides a specimen for confirmatory pathologic diagnosis.13 Ileocolostomy is one of the surgical options but it often complicates with blind loop syndrome. Right hemicolectomy or segmental resection of the small bowel combined with anti-TB medication are found to be safe and effective.13 The anti-TB treatment, the duration and regimen, are similar to Pulmonary TB patients. A six month treatment is usually sufficient.16 In our case, we did segmental ileal resection, and the patient was put on anti-TB medication postoperatively. The Anti-TB regimens were HRZE (isoniazid, rifampicin, pyrazinamide, ethambutol) for the 1st 2 months and HR for the subsequent 4 months.
Conclusion
Intestinal TB is a great mimicker of intestinal conditions like small bowel tumors and other inflammatory diseases like IBD. So, a high index of suspicion is vital in the diagnosis of Intestinal TB especially as a cause of partial chronic small bowel obstruction in populations where TB is common. Although anti-TB treatment remains the mainstay of therapy in Intestinal TB, surgery is often required on an emergency or elective basis, depending on the patient’s presentation, which in turn is determined by the presence of complications or not.
Data Sharing Statement
The data used to support the findings of this study will be available from the corresponding author upon reasonable request.
Ethical Review
Written informed consent was obtained from the patient for the publication of this case report after a letter of permission was gained from the Hawassa University Institutional Review Board (IRB).
Acknowledgments
The authors would like to acknowledge the patient, who allowed us to undertake this case report.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Mirza B, Ijaz L, Saleem M, Sheikh A. Surgical aspects of intestinal tuberculosis in children: our experience. Afr J Paediatr Surg. 2011;8(2):185–189.
2. Chalya PL, Mchembe MD, Mshana SE, Rambau P, Jaka H, Mabula JB. Tuberculous bowel obstruction at a university teaching hospital in Northwestern Tanzania: a surgical experience with 118 cases. World J Emerg Surg. 2013;8(1):1. doi:10.1186/1749-7922-8-12
3. Merino-Gallego E, Gallardo-Sánchez F, Gallego-Rojo FJ. Intestinal tuberculosis and Crohn’s disease: the importance and difficulty of a differential diagnosis. Rev Esp Enferm Dig. 2018;110(10):650–656.
4. Shaikh MS, Dholia KRAM, Jalbani MA, Shaikh SALI. Prevalence of intestinal tuberculosis in cases of acute abdomen. Pak J Surg. 2007;23(1):52–56.
5. Lowbridge C, Fadhil SAM, Krishnan GD, et al. How can gastro-intestinal tuberculosis diagnosis be improved? A prospective cohort study. BMC Infect Dis. 2020;20(1):1–8. doi:10.1186/s12879-020-04983-y
6. Arega B, Mersha A, Minda A, et al. Epidemiology and the diagnostic challenge of extra-pulmonary tuberculosis in a teaching hospital in Ethiopia. PLoS One. 2020;15(12December):1–15. doi:10.1371/journal.pone.0243945
7. Tan KK, Chen K, Sim R. The spectrum of abdominal tuberculosis in a developed country: a single institution’s experience over 7 years. J Gastrointest Surg. 2009;13(1):142–147. doi:10.1007/s11605-008-0669-6
8. Pattanayak S, Behuria S. Is abdominal tuberculosis a surgical problem? Ann R Coll Surg Engl. 2015;97(6):414–419. doi:10.1308/rcsann.2015.0010
9. Weledji EP, Pokam BT. Abdominal tuberculosis: is there a role for surgery? World J Gastrointest Surg. 2017;9(8):174. doi:10.4240/wjgs.v9.i8.174
10. Gonie A, Bekele K. Perforated tuberculous appendicitis: a rare case report. Int Med Case Rep J. 2018;11:129–131. doi:10.2147/IMCRJ.S158074
11. Park H, Kansara T, Victoria AM, Boma N, Hong J. Intestinal tuberculosis: a diagnostic challenge. Cureus. 2021;13(Iv):2–5.
12. Djaharuddin I, Hatta M, Tabri NA, Muis E, Safriadi S, Primaguna MR. Intestinal tuberculosis: case series of three patients. Respir Med Case Rep. 2020;29:100942.
13. Nguyen VH. Intestinal obstruction due to tuberculosis. Asian J Surg. 2002;25(2):145–148. doi:10.1016/S1015-9584(09)60163-9
14. Awasthi S, Saxena M, Ahmad F, Kumar A, Dutta S. Abdominal tuberculosis: a diagnostic dilemma. J Clin Diagn Res. 2015;9(5):EC01–EC03.
15. Kentley J, Ooi JL, Potter J, et al. Intestinal tuberculosis: a diagnostic challenge. Trop Med Int Health. 2017;22(8):994–999. doi:10.1111/tmi.12908
16. Eraksoy H. Gastrointestinal and abdominal tuberculosis. Gastroenterol Clin North Am. 2021;50(2):341–360. doi:10.1016/j.gtc.2021.02.004
17. Barot M, Yagnik VD, Patel K, Dawka S. Surgical management of abdominal tuberculosis: a prospective single-center study. Tzu Chi Med J. 2021;33(3):282–287. doi:10.4103/tcmj.tcmj_206_20
18. Dhali ADK, Das K, Dhali G, Ghosh R, Sarkar A, Misra D. Abdominal tuberculosis: clinical profile and outcome. Int J Mycobacteriol. 2021;10:414–420. doi:10.4103/ijmy.ijmy_195_21
19. Castellotti P, Riccardi N, Ferrarese M, et al. Intestinal tuberculosis versus inflammatory bowel diseases: a never-ending challenge. New Microbiol. 2020;43(3):139–143.
20. Uygur-Byramiçli O, Dabak G, Dabak R. A clinical dilemma: abdominal tuberculosis. World J Gastroenterol. 2003;9(5):1098–1101. doi:10.3748/wjg.v9.i5.1098
21. Merza MA, Jabrial FK, Hussein NR. Intestinal obstruction secondary to primary ileocecal tuberculosis: a case report. Int J Mycobacteriol. 2012;1(2):139–143. doi:10.1016/j.ijmyco.2012.05.001
22. Pejhan S. Surgical treatment for complications of Azizollah Abbasi, *MD; Mojtaba Javaherzadeh, MD; Mehrdad Arab, MD; 2015.
23. Ionescu S, Nicolescu AC, Madge OL, Marincas M, Radu M, Simion L. Differential diagnosis of abdominal tuberculosis in the adult—literature review. Diagnostics. 2021;11(12):1–17. doi:10.3390/diagnostics11122362
24. Sala ML, Verhage SM, Zijta F, Hirata T. Abdominal tuberculosis complicated by intestinal perforation. Case Rep Gastrointest Med. 2021;2021:1–3. doi:10.1155/2021/8861444
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.