Back to Journals » International Medical Case Reports Journal » Volume 15
A Rare Case of Dandy-Walker Syndrome
Authors Oria MS, Rasib AR , Pirzad AF, Wali Ibrahim Khel F, Ibrahim Khel MI , Wardak FR
Received 23 November 2021
Accepted for publication 2 February 2022
Published 15 February 2022 Volume 2022:15 Pages 55—59
DOI https://doi.org/10.2147/IMCRJ.S350858
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Mohammad Sharif Oria,1 Aziz Rahman Rasib,2 Ahmad Fawad Pirzad,3 Fahima Wali Ibrahim Khel,4 Mohammad Ismael Ibrahim Khel,1 Fazel Rahim Wardak5
1Anesthesiology Department, Kabul University of Medical Sciences, Kabul, 1001, Afghanistan; 2Neuropsychiatry Department, Kabul University of Medical Sciences, Kabul, 1001, Afghanistan; 3Neurosurgery Department, Kabul University of Medical Sciences, Kabul, 1001, Afghanistan; 4Gynecology and Obstetrics Department, Malalai Maternity Hospital, Kabul, 1003, Afghanistan; 5Microbiology Department, Kabul University of Medical Sciences, Kabul, 1001, Afghanistan
Correspondence: Aziz Rahman Rasib, Department of Neuropsychiatry, Kabul University of Medical Sciences, Kabul, 1001, Afghanistan, Tel +93797089250, Email [email protected]
Abstract: Dandy-Walker syndrome (DWS) is a rare congenital malformation characterized by hypoplasia of the cerebellar vermis and its upward rotation and cystic enlargement of the fourth ventricle. The clinical manifestations include psychomotor retardation, ataxia and hydrocephalus. We report a case of 16-year-old female patient in Ali Abad Teaching Hospital who was suffering from unsteady gait, memory deterioration and urinary incontinence. A brain magnetic resonance imaging revealed enlarged cystic posterior fossa, dilated fourth ventricles and upward rotated cerebellar vermis which were indicating DWS. The patient prepared for planned surgical operation and a written informed consent was obtained from her parents for surgery and general anesthesia. A cystoperitoneal (CP) shunt was placed and then the patient transferred to recovery room. After recovery and hospital stay, the patient discharged with improved clinical symptoms.
Keywords: Dandy Walker syndrome, hydrocephalus, intubation challenge
Introduction
Dandy-Walker syndrome (DWS) or Dandy-Walker malformation is a developmental abnormality characterized by dilated posterior fossa, cystic enlargement of the fourth ventricle, hypoplasia of cerebellar vermis and its upward rotation. The affected person may suffer from psychomotor retardation, ataxia, apnea attacks, muscle weakness, occasional muscle spasm, seizures, nystagmus, and macrocephaly.1,2 However, half of the cases have normal intelligence.1
The etiology of DWS is less understood, however, the overlapping deletion of 3q24q25.1 has been reported in a limited number of patients. The heterozygous deficiency of ZIC1 and ZIC4 genes has been detected within the missed region and is said to be the cause of DWS in the mouse models.2 The frequency of DWS in the United States is approximately 1 per 30,000 live births,2 whereas the global occurrence is reported at 6.79 per 100,000 childbirths.3
DWS may be asymptomatic or associated with various diseases such as bipolar disorder, Acquired Immunodeficiency Syndrome, and kidney and liver diseases.4 Anesthetic management of DWS patients may be faced with severe challenges due to multi-organ association of craniofacial abnormalities, hydrocephalus, renal, and cardiac anomalies.5
Case Presentation
A 16-year-old female patient was brought to the Department of Neurosurgery of Ali Abad Teaching Hospital with intermittent episodes of nausea, vomiting, headache, seizure and urinary incontinence. On physical examination, she had movement disturbance, memory deterioration, paresthesia, and muscle weakness. The head circumference was 59 centimeters (cm). She was the second child of her family and did not have any significant family history of congenital disorders, additionally, her mother did not remember any exposure to drugs or infections during her pregnancy.
Brain computed tomography (CT) scan, which had been done before, showed cystic dilatation of the fourth ventricle with enlargement of the posterior fossa, evidence of hypoplastic cerebellar vermis and mild supratentorial hydrocephalus (Figure 1). The patient underwent magnetic resonance imaging (MRI) and it showed cystic dilatation of the fourth ventricle with enlargement of the posterior fossa (Figure 2A), evidence of hypoplastic cerebellar vermis with cephalad rotation of the vermian remnant (Figure 2B) and mild supratentorial hydrocephalus (Figure 2C). These findings confirmed the diagnosis of DWS. The patient was selected for a planned surgical operation, after obtaining informed consent from her parents. Before the procedure, a 22-gauge peripheral intravenous catheter was inserted and pre-oxygenation was performed for four minutes. Antibiotics and 1 mg midazolam and 0.5 mg morphine were administered as a premedication. To control postoperative nausea and vomiting, 4 mg IV ondansetron was administered immediately before anesthesia. Anesthesia induction was done with 2 mg/kg propofol. After adequate muscle relaxation with 1 mg/kg succinylcholine laryngoscopy was performed using a Macintosh size 3 blade with the patients’ head in sniffing position by anesthesiologists with more than three years’ experience in anesthesia. We recorded a Cormack and Lehane grade II view through the laryngoscopy. However, we could not intubate the patient with initial attempts to pass an endotracheal tube size 6.5 mm due to resistance of the vocal cords. The same resistance was observed with a smaller sized endotracheal tube. Then, a laryngeal mask airway (LMA) was inserted. Sufficient ventilation was established by auscultating the normal breathing sounds in both lungs. We elevated the head of the patient by 10 cm. Anesthesia was constantly maintained with sevoflurane during this time. The patient’s blood pressure and pulse rate remained stable at 110/80–120/70 mmHg and 65–85 beats/min, respectively, throughout the operation.
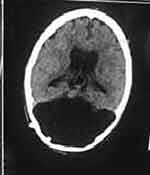 |
Figure 1 Brain CT scan; showing cystic dilatation of the fourth ventricle with enlargement of the posterior fossa, evidence of hypoplastic cerebellar vermis and mild supratentorial hydrocephalus. |
Once anesthetic management of the patient was ensured the operational procedure started. First, a curvilinear incision was performed at the Keen’s point (located 3 cm above and behind the pinna of the ear). Then, a small hole drilled in the skull (Burr hole). Subsequently, a small skin incision in the right upper quadrant of the abdomen was made for insertion of a tunneler. Finally, the cystoperitoneal shunt catheter was placed subcutaneously from the abdomen insertion point, to the Keen’s point, where it was connected to the valve. The operation continued for one hour and forty minutes. At the end, we decurarized the patient with 0.5 mg atropine, and 2.5 mg neostigmine. The LMA was removed without any complication. The patient was referred to recovery room where she was kept for 1 hr and then transferred to a ward, after an Aldrete score reading of 10. She was discharged from hospital after four days with significant improvement of her symptoms.
The patient’s parents provided written consent for the case details to be published.
Discussion
Dandy-Walker syndrome is a rare malformation defined as dilation of the posterior fossa, cystic enlargement of the fourth ventricle, hypoplasia of the cerebellar vermis and its upward dislocation. DWS is normally presented in childhood, however, rare cases are also reported in adulthood.6 This is the first report of DWS in a sixteen-year-old female from Afghanistan. The condition is linked to congenital cardiac anomalies, spina bifida or anencephaly, cleft lip, cleft palate and Hirschsprung’s disease in some cases.6 Predisposing factors of DWS are common congenital infections such as toxoplasmosis, cytomegalovirus and rubella, and drugs like, warfarin, retinol derivative (isotretinoin) and ethanol.7,8 However, we are not certain whether the mother of this patient had faced these factors or not.
Our case had recurrent nausea, vomiting, headache and seizure. These symptoms are comparable to a report by Ndu et al where the case had fever, headache, vomiting, seizure, continuous visual loss, unconsciousness and neck pain.8 In addition, the patient had development mental retardation, ataxia, paresthesia, muscle weakness, hydrocephalus and macrocephaly. Meanwhile, about 90% of individuals with DWS have hydrocephalus, 15.30% have seizure, 41.71% have poor intelligence development, increased head circumference, ataxia, muscle rigidity, and growth retardation at the time of diagnosis.7
The diagnosis of DWS is made by contemporary imaging tools such as ultrasonography, computed tomography and MRI.9 We observed cystic enlargement of the posterior fossa and a dilated fourth ventricle in MRI images of the patient.
Although the patient was assessed to have easy intubation before operation (Mallampati score 2), we encountered difficulty in intubation. The reason could be a number of anomalies associated with DWS such as craniofacial abnormalities, or renal, or cardiac anomalies.5 Moreover, macroglossia, crowding of the midfacial structures, high arched, narrow palate, micrognathia, short broad neck, and high frequency of tonsillar and adenoidal hypertrophy are the most prevalent morphologic abnormalities seen in DWS patients.10 Flattened nasal bridge, shallow hypopharyngeal dimensions, tracheal and congenital subglottic stenosis, airway malacia, pharyngeal muscle hypotonia, increased secretions, and frequent infections are also mentioned by other authors.11
An unexpectedly difficult intubation puts patients at a higher risk of complications.12 Soft tissue injury, trauma and subsequent airway edema, inessential surgical airway, failure to maintain tissue oxygenation, brain injury, cardiorespiratory arrest, and even death are all possible outcomes.13
Due to a higher occurrence of subglottic stenosis and recurrent respiratory tract infection (RTI) in patients with DWS, opinions on whether to employ endotracheal intubation or the supraglottic air device are continually discussed.11,14 According to Lewanda et al11 the employment of LMA is recommended for brief procedures. Though endotracheal intubations can cause chronic inflammation and scarring of the subglottic airway,15 if intubation is necessary, it is recommended to start with an endotracheal intubation which is at least two sizes smaller than what we would normally choose.11,16 Some clinicians employ a small cuffed tube that permits successful intubation while avoiding substantial air leak.11 In children with an upper RTI Tait et al17 recommended that LMA is as safe as endotracheal intubation in terms of perioperative airway problems.
We could not observe her airway with a bronchoscope to find out the exact cause of the challenge. Although skilled anesthesiologists are essential, the scarcity of important instruments is a big challenge during the airway management of patients with anatomic anomalies like Dandy Walker syndrome. The patient returned to hospital eight months after the surgery for a follow-up visit. Her status was satisfactory. The patient’s guardian was reluctant to do a follow up MRI due to financial restriction. However, her post-operative control X-ray showed the CP shunt inserted during the operation (Figure 3). This report highlights a rare case of symptomatic DWS which improved significantly after CP shunt placement. In addition, unexpected difficulty in intubation was found which signifies the importance of the skilled anesthesiologists and essential instruments during operation.
 |
Figure 3 Post-operative X-ray which illustrates the CP shunt inserted during the operation. |
Ethics Statement
This report was approved by the Ethics Committee of the Department of Anesthesiology, Kabul University of Medical Sciences under protocol no. (2021-60).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Grinberg I, Northrup H, Ardinger H, et al. Heterozygous deletion of the linked genes ZIC1 and ZIC4 is involved in Dandy-Walker malformation. Nat Genet. 2004;36(10):1053–1055. doi:10.1038/ng1420
2. Ferraris A, Bernardini L, Sabolic Avramovska V, et al. Dandy-Walker malformation and Wisconsin syndrome: novel cases add further insight into the genotype-phenotype correlations of 3q23q25 deletions. Orphanet J Rare Dis. 2013;8:75. doi:10.1186/1750-1172-8-75
3. Santoro M, Coi A, Barišić I, et al. Epidemiology of dandy-walker malformation in Europe: a EUROCAT Population-Based Registry Study. Neuroepidemiology. 2019;53(3–4):169–179. doi:10.1159/000501238
4. Jha VC, Kumar R, Srivastav AK, et al. A case series of 12 patients with incidental asymptomatic Dandy–Walker syndrome and management. Childs Nerv Syst. 2012;28(6):861–867. doi:10.1007/s00381-012-1734-8
5. Buget MI, Edipoglu IS, Cemaller E, et al. Anesthetic management of a patient with Dandy-Walker syndrome for orthopedic surgery. J Med Cases. 2015;6(9):403–405. doi:10.14740/jmc2255e
6. Zhang N, Qi Z, Zhang X, et al. Dandy-Walker syndrome associated with syringomyelia in an adult: a case report and literature review. J Int Med Res. 2019;47(4):1771–1777. doi:10.1177/0300060518808961
7. Hamid HA. Dandy-walker malformation. Egypt J Med Hum Genet. 2007;8(2):115–120.
8. Ndu I, Chinawa JM, Chikani M, et al. Dandy Walker malformation (variant): late presentation with childhood blindness. Niger J Paediatr. 2015;42(1):73–75. doi:10.4314/njp.v42i1.17
9. Tadakamadla J, Kumar S, Mamatha GP. Dandy-Walker malformation: an incidental finding. Indian J Hum Genet. 2010;16(1):33–35. doi:10.4103/0971-6866.64936
10. Mitchell V, Howard R, Facer E. Down’s syndrome and anaesthesia. Paediatr Anaesth. 1995;5(6):379–384. doi:10.1111/j.1460-9592.1995.tb00331.x
11. Lewanda AF, Matisoff A, Revenis M, et al. Preoperative evaluation and comprehensive risk assessment for children with Down syndrome. Paediatr Anaesth. 2016;26(4):356–362. doi:10.1111/pan.12841
12. Adnet F, Borron S, Racine S, et al. The Intubation Difficulty Scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology. 1997;87(6):1290–1297. doi:10.1097/00000542-199712000-00005
13. Andrade R, Lima BLS, Lopes DKDO, et al. [Difficult laryngoscopy and tracheal intubation: observational study]. Braz J Anesthesiol. 2018;68(2):168–173. Portuguese. doi:10.1016/j.bjan.2017.10.009
14. Sinha R, Muthiah T, Subramaniam R, et al. Prolonged postoperative desaturation in a child with Down syndrome and atrial septal defect. Indian J Anaesth. 2011;55(6):608–610. doi:10.4103/0019-5049.90619
15. Bhattarai B, Kulkarni AH, Rao ST, et al. Anesthetic consideration in downs syndrome–a review. Nepal Med Coll J. 2008;10(3):199–203.
16. Kozanhan B, Basaran B, Aygin F, et al. Anaesthetic management of laparoscopic Morgagni hernia repair in a patient with coexisting down syndrome, patent foramen ovale and pectus carinatum. Turk J Anaesthesiol Reanim. 2016;44(1):44–46. doi:10.5152/TJAR.2016.13007
17. Tait AR, Pandit UA, Voepel-Lewis T, et al. Use of the laryngeal mask airway in children with upper respiratory tract infections: a comparison with endotracheal intubation. Anesth Analg. 1998;86(4):706–711. doi:10.1213/00000539-199804000-00006
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

