Back to Journals » OncoTargets and Therapy » Volume 9
A randomized Phase II trial of the tumor vascular disrupting agent CA4P (fosbretabulin tromethamine) with carboplatin, paclitaxel, and bevacizumab in advanced nonsquamous non-small-cell lung cancer
Authors Garon EB, Neidhart JD, Gabrail NY, de Oliveira MR, Balkissoon J, Kabbinavar F
Received 25 March 2016
Accepted for publication 2 July 2016
Published 30 November 2016 Volume 2016:9 Pages 7275—7283
DOI https://doi.org/10.2147/OTT.S109186
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr William C. Cho
Edward B Garon,1,2 Jeffrey D Neidhart,3 Nashat Y Gabrail,4 Moacyr R de Oliveira,5 Jai Balkissoon,6 Fairooz Kabbinavar1,2
1Department of Medicine, 2Department of Hematology and Oncology, David Geffen School of Medicine at University of California Los Angeles, Los Angeles, CA, 3San Juan Oncology Associates, Farmington, NM, 4Gabrail Cancer Center, Canton, OH, 5Northwest Medical Specialties, Tacoma, WA, 6Global Product Development and Immuno-Oncology, PPD, Wilmington, NC, USA
Introduction: Combretastatin A4-phosphate, fosbretabulin tromethamine (CA4P) is a vascular disrupting agent that targets tumor vasculature. This study evaluated the safety of CA4P when combined with carboplatin, paclitaxel, and bevacizumab in chemotherapy-naïve subjects with advanced nonsquamous, non-small-cell lung cancer.
Methods: Adult subjects with confirmed American Joint Committee on Cancer six stage IIIB/IV non-small-cell lung cancer and an Eastern Cooperative Oncology Group performance score of 0 or 1 were randomized to receive six cycles (treatment phase) of paclitaxel (200 mg/m2), carboplatin (area under the concentration versus time curve 6), and bevacizumab (15 mg/kg) on day 1 and repeated every 21 days, or this regimen plus CA4P (60 mg/m2) on days 7, 14, and 21 of each cycle. Subjects could then receive additional maintenance treatment (excluding carboplatin and paclitaxel) for up to 1 year.
Results: Sixty-three subjects were randomized, 31 to control and 32 to CA4P, and 19 (61.3%) and 17 (53.1%), respectively, completed the treatment phase. Exposure to study treatment and dose modifications were comparable between the randomized groups. The overall incidence of treatment-emergent adverse events was similar between groups, with increased neutropenia, leukopenia, and hypertension in the CA4P group. Deaths, serious adverse events, and early discontinuations from treatment were comparable between the randomized treatment groups. The overall tumor response rate with CA4P was 50% versus 32% in controls. Overall and progression-free survival rates were comparable between the groups.
Conclusion: CA4P plus carboplatin, paclitaxel, and bevacizumab appears to be a tolerable regimen with an acceptable toxicity profile in subjects with advanced non-small-cell lung cancer.
Keywords: CA4P, bevacizumab, paclitaxel, carboplatin, NSCLC
Introduction
Lung cancer was responsible for more than a quarter (~160,000) of all cancer-related deaths in 2015, and remains the leading cause of cancer-related mortality in the US.1 Non-small-cell lung cancer (NSCLC), which has a 5-year survival rate of 1% in those with metastatic disease, accounted for ~85% of the total.2 While there have recently been important therapeutic advances in the field for patients with relapsed nonsquamous NSCLC – including recent approval of immune checkpoint inhibitors3,4 in previously treated patients – and patients with abnormalities in epidermal growth factor receptor or anaplastic lymphoma kinase receive frontline targeted therapy,5,6 first-line treatment for metastatic disease in the great majority of patients has remained unchanged for years, and new therapies are needed.
Bevacizumab, an antibody directed against vascular endothelial growth factor (VEGF), inhibits new tumor vasculature formation by binding VEGF.7 In the E4599 trial, adding bevacizumab to carboplatin and paclitaxel versus paclitaxel-carboplatin alone significantly improved the response rate (RR; 35% vs 15%; P<0.001); progression-free survival (PFS; 6.2 vs 4.5 months; hazard ratio [HR], 0.66; P<0.001); and overall survival (OS; 12.3 vs 10.3 months; HR, 0.79; P=0.003).8 More recently, subjects with stage IV NSCLC who experienced progression on a platinum-based doublet and received second-line treatment with the VEGF receptor 2-directed antibody, ramucirumab, plus docetaxel had significantly improved RR (23% vs 14%; P<0.0001), PFS (4.5 vs 3.0 months; HR 0.76; P<0.0001), and OS (10.5 vs 9.1 months; HR, 0.86; P=0.023),9 leading to the US Food and Drug Administration approval of the ramucirumab–docetaxel combination for treatment of patients with previously treated NSCLC.10
Because tumors ultimately overcome the inhibition of angiogenesis produced by anti-VEGF antibodies, clinical trials have studied the simultaneous targeting of the VEGF pathway, looking to achieve additive or synergistic outcomes with the combination of bevacizumab with tyrosine kinase inhibitors. The combination produced promising antitumor activity but increased toxicity, most frequently hypertension and cardiac ischemia.11,12
Other promising candidates for use in combination to achieve optimal antivascular effects include vascular disrupting agents (VDAs). These agents rapidly and selectively bind to tubulin, which leads to dramatic effects on the shape of the immature endothelial cells. This compromises the tumor blood vessels, thereby leading to widespread ischemia and necrosis of the cancer cells within the central core of the tumor.13,14 Although one small-molecule VDA, the flavonoid ASA404, has shown activity in Phase II studies,14,15 Phase III trials combining ASA404 with carboplatin and paclitaxel (as first-line), and with docetaxel (as second-line) were terminated at interim analysis for futility.16–18
An interesting feature of the activity of VDAs is that treatment efficacy has been shown to increase as tumors become larger, probably because, as tumors become larger, a smaller proportion of interior tumor cells depend on the normal tissue blood vessels at the rim of the tumor. This increased activity in larger tumors has been characterized in several preclinical studies19,20 and is a trend seen in the clinical data from subgroups in the Fosbretabulin in Anaplastic Cancer of the Thyroid (FACT) and Gynecologic Oncology Group-0186I trials.21,22
Combretastatin A4-phosphate, fosbretabulin tromethamine (CA4P) is a tubulin-binding VDA that was originally isolated from the African Bush Willow (Combretum caffrum). It acts as a potent and reversible tubulin depolymerizing agent and is a water-soluble prodrug of cis-combretastatin A4.23 Preclinical models, which show that CA4P results in massive acute vascular disruption as early as 2 hours after administration with recovery as soon as 24 hours post-dose, provide strong theoretical rationale for a CA4P–bevacizumab combination.11 In a Phase I study of the combination of CA4P plus bevacizumab, the dose-limiting toxicity was hypertension, with a maximum tolerated dose of 63 mg/m2 for CA4P. Profound vascular changes associated with CA4P administration were sustained following bevacizumab, as revealed in dynamic contrast-enhanced and diffusion-weighted magnetic resonance imaging.12 In three Phase I studies of CA4P in subjects with refractory solid tumors (N=96), tumor responses were seen in two patients, including a complete response in a patient with anaplastic thyroid cancer.24–26 Phase IB trials showed good tolerability of CA4P when given with bevacizumab or with carboplatin and paclitaxel.27,28 A Phase II/III study was conducted in patients with anaplastic thyroid cancer comparing CA4P, carboplatin and paclitaxel to carboplatin and paclitaxel. Enrollment was stopped at 80 patients due to limited accrual, but a trend toward improved survival was seen with the combination of CA4P and chemotherapy.21
Based on the positive efficacy trends and relative safety seen in previous studies, we conducted a randomized, open-label, multicenter, parallel-group Phase II study to evaluate the safety of a combination of carboplatin, paclitaxel, bevacizumab, and CA4P in subjects with chemotherapy-naïve stage IIIB/IV NSCLC. The rationale for adding a VDA to this regimen was based on preclinical and initial clinical data27,29,30 supporting the therapeutic potential of combining a VDA with an antiangiogenic, as they have complementary mechanisms of action; VDAs disrupt tumor blood flow within the tumor, whereas antiangiogenic agents inhibit regrowth. We compared this group with a control arm that received the same combination without CA4P to isolate toxicities related to the addition of CA4P. Efficacy endpoints were also assessed.
Materials and methods
Subject eligibility
Eligible subjects were adults (≥18 years) with histologically or cytologically confirmed stage IIIB (with malignant pleural effusion) or IV nonsquamous NSCLC (according to American Joint Committee on Cancer classification, 6th edition) and an Eastern Cooperative Oncology Group Performance Status (ECOG PS) of 0 or 1. Subjects were required to be chemotherapy naïve and have measurable and/or nonmeasurable disease by the Response Evaluation Criteria in Solid Tumors (RECIST) criteria31 and no evidence of active brain metastasis. Subjects were required to have adequate bone marrow function, adequate hepatic function, partial thromboplastin time within normal limits, and adequate renal function.
Subjects were excluded if they had hemoptysis within 3 months (≥½ teaspoon bright red blood per event); therapeutic anticoagulation; uncontrolled hypertension (>150/100 mmHg) despite medication; ≥ grade 1 peripheral neuropathy; history of torsade de pointes, ventricular tachycardia or fibrillation, pathologic sinus bradycardia, greater than first-degree heart block, congenital long QT syndrome or new ST segment elevation or depression or new Q wave on electrocardiogram (ECG); corrected QT (QTc) >450 ms for male subjects, QTc >470 ms for female subjects; potassium or magnesium below the midpoint of the interval between lower limit of normal and upper limit of normal (ULN), calcium less than lower limit of normal, recent surgery, hypersensitivity to any of the study agents, or serious nonhealing wound, ulcer, or bone fracture. Subjects were also excluded if within the last 6 months they had a thrombotic or hemorrhagic disorder, cerebrovascular event, angina pectoris, myocardial infarction, or New York Heart Association Class ≥III congestive heart failure. Institutional review board approval was obtained from Copernicus Group IRB (Research Triangle Park, NC, USA) or institutional review boards at each study site (UCLA, Boca Raton Regional Hospital, Lahey Hospital & Medical Center, West Virginia University). Subjects provided written informed consent prior to enrollment.
Treatment
Subjects in the chemotherapy control group received intravenous (IV) therapy with paclitaxel (200 mg/m2) over 180 minutes, carboplatin (area under the concentration-time curve [AUC] 6) over 30 minutes, plus bevacizumab (15 mg/kg) over 90 minutes for Cycle 1, 60 minutes for Cycle 2, and 30 minutes for all subsequent cycles, if well tolerated, on day 1 of a 21-day cycle for six cycles (treatment phase). Subjects in the CA4P experimental group received IV chemotherapy and bevacizumab as mentioned earlier, plus IV CA4P (60 mg/m2 [Mateon Therapeutics, South San Francisco, CA, USA]) infused over 10 minutes on days 7, 14, and 21 of each 21-day cycle for six cycles. All subjects in the CA4P group received oral or IV dexamethasone 8 mg and oral acetaminophen 1 hour prior to CA4P administration. After the first dose of CA4P, subjects who required treatment for transient hypertension received oral amlodipine (5–10 mg) or diltiazem (30–60 mg) 1 hour prior to subsequent doses. After completing the treatment phase, subjects who did not have disease progression were eligible to enter a maintenance phase. In the maintenance phase, subjects in the control arm received bevacizumab 15 mg/kg on day 1 of each 21-day cycle while subjects in the CA4P arm received bevacizumab on day 1 and CA4P 60 mg/m2 on days 7, 14, and 21 of each 21-day cycle. For convenience, CA4P on day 21 could be given on day 1 of the following cycle during the maintenance phase. Maintenance therapy continued until disease progression, 12 months of follow-up since randomization, unacceptable toxicity, withdrawal of consent, or death.
Dose delays
Toxicity assessments were graded according to National Cancer Institute Common Terminology Criteria for Adverse Events version 3.0. A new treatment cycle was started only if ECOG PS was ≤1; absolute neutrophil count ≥1,500 cells/μL, platelet count ≥100,000/μL; adverse events (AEs) considered at least possibly related to treatment had recovered to baseline or ≤grade 1; blood pressure ≤150/100; urine protein/creatinine ratio ≤2.0; and serum potassium and magnesium levels ≤0.2 meq/L below midpoint of the normal range. Subjects were discontinued from the trial if a cycle was delayed for more than 14 days.
Dose adjustments
After a dose reduction of any study drug, all subsequent doses of that agent were given at the reduced dose level. A maximum of two dose reductions was allowed.
CA4P was decreased by 10 mg/m2 for subjects with QTc >480 ms; grade ≥2 hypertension during the 4 hours post-CA4P infusion despite premedication; grade ≥2 hypotension during the 4 hours post-CA4P; grade ≥3 diarrhea, central neurological symptoms, motor or sensory neuropathy, or hematological symptoms (during maintenance phase); or grade ≥4 hematological symptoms during the treatment phase (growth factors could be given rather than dose reduction for myelosuppression at the investigator’s discretion). If a subject experienced grade ≥2 myocardial ischemia, the dose was reduced by 20 mg/m2.
Bevacizumab was reduced (first reduction to 7.5 mg/kg, second reduction to 5 mg/kg) for subjects with chronic grade 3 hypertension; protein/creatinine ratio >1.5, grade ≥2 hemorrhage (gastrointestinal, genitourinary, or upper respiratory); or a severe thromboembolic event. Bevacizumab was discontinued for grade 4 hypertension, hypertensive crisis, hypertensive encephalopathy, nephrotic syndrome, serious hemorrhage, gastrointestinal perforation, fistula formation, or reversible posterior leukoencephalopathy syndrome.
For the following toxicities, carboplatin was decreased by an AUC of 1, and paclitaxel was reduced by 25% for subjects with: grade 4 neutropenia or grade 3 or 4 febrile neutropenia; platelets ≤25,000/μL or ≤50,000/μL with clinically significant bleeding; grade ≥3 nausea or vomiting despite maximal treatment; grade ≥3 mucositis; or grade ≥3 peripheral neuropathy (after resolution to ≤ grade 1). For liver dysfunction, total bilirubin 1.26–2.0× ULN and aspartate aminotransferase (AST) <10× ULN led to reduction of paclitaxel to 175 mg/m2, total bilirubin 2.01–5× ULN and AST <10× ULN led to reduction of paclitaxel to 135 mg/m2, and bilirubin >5× ULN or AST >10× ULN resulted in holding the dose or discontinuing treatment.
Study evaluations
Safety
Assessments before each administration of study drug included AEs (graded according to National Cancer Institute Common Terminology Criteria for Adverse Events version 3.0); vital signs; concomitant medications; laboratory tests; and ECOG PS. Before and at 2 and 4 hours after CA4P dosing, ECGs were obtained.
Antitumor activity and survival
Tumor response and progression were evaluated according to RECIST criteria (version 1.0) within 28 days of enrollment and once every 8 weeks (±7 days) during the treatment phase and every 12 weeks (±7 days) during the maintenance phase. Tumor response was based on investigator assessment of imaging. Responses were confirmed by subsequent imaging ≥4 weeks after the initial indication of response. After the last clinic visit, subjects were followed monthly for survival until either death, termination of the study by sponsor, or withdrawal of informed consent by the subject.
Statistical design and analysis
This was a randomized, controlled, open-label, Phase II study conducted at 18 centers in the US. Subjects were randomized in a 1:1 ratio to receive carboplatin, paclitaxel, and bevacizumab or this combination plus CA4P. Randomization was stratified based on ECOG PS (0 vs 1) and whether the subject had received prior treatment (surgery or radiation). The primary objective was to determine the safety and tolerability of CA4P when combined with carboplatin, paclitaxel, and bevacizumab compared with carboplatin, paclitaxel, and bevacizumab alone. Additional objectives were to assess RR, PFS, and OS in both arms. The study was designed to assess the potential treatment effect size and was not powered to be a superiority study. The sample size was planned using a confidence interval (CI) approach, based on the assumption that the 6-month PFS rate would be ~50% for the control group and for the CA4P arm would be within the 95% CIs of 50%±17.9%. All subjects randomized constituted the intent-to-treat (ITT) population.
The safety population included all subjects who were randomized and received at least one dose of study medication. The assessment of safety was based on AEs, clinical laboratory evaluations, physical examination findings, ECG results, and vital signs. AEs were coded according to the Medical Dictionary for Regulatory Activities, version 10.1, and were summarized by system organ class and preferred term for each treatment group.
Efficacy endpoints were assessed for the ITT population, and analyzed to determine if further study of this quadruplet combination was warranted. Tumor response and PFS were evaluated using RECIST 1.0 criteria. Kaplan–Meier estimates were used to analyze PFS and OS. In order to further study the impact of baseline ECOG PS or prior treatment on the efficacy endpoints, stratified analyses for survival and RRs were also performed using a Cox regression model.
Results
Subject characteristics
Between March 2008 and July 2011, 63 subjects were randomized to study drug treatment (ITT population; CA4P arm, n=32; control arm, n=31). Sixty subjects received at least one dose of study treatment (safety population), including 31 in the CA4P group and 29 in the control group. Fifteen subjects in the CA4P group and 17 subjects in the control group continued into the maintenance phase (Figure 1). Baseline demographic and clinical characteristics were similar between the treatment arms (Table 1).
  | Figure 1 Trial profile. |
Exposure and safety
The cumulative doses received of carboplatin, paclitaxel, bevacizumab, and CA4P are shown in Table 2. All subjects in the safety population in both randomized treatment groups experienced at least one treatment-emergent AE (TEAE). TEAEs reported in ≥10% of subjects in the CA4P group that occurred at a higher frequency than in the control group are shown in Table 3. Twenty-seven of 31 safety subjects (87.1%) in the CA4P group experienced TEAEs considered at least possibly related to CA4P.
Altogether, 26/60 subjects (43.3%) experienced TEAEs that required dose adjustments of any study medication: 16/31 (51.6%) in the CA4P group and 10/29 (34.5%) in the control group. Overall, 39/60 subjects (65.0%) experienced TEAEs, resulting in study drug treatment delays: 20/31 (64.5%) in the CA4P group and 19/29 (65.5%) in the control group. Overall, there was a similar distribution in the frequencies of most severe TEAEs for grades 1 to 5 between the CA4P and control groups. Grade 3/4 TEAEs were reported in 26/31 (83.8%) in the CA4P group and 27/29 (93.1%) in the control group. Neutropenia was more frequent in the CA4P group, with 3/31 (9.7%) of subjects developing febrile neutropenia compared with no subjects in the control group. Equal numbers of patients in the active and control groups received growth factors, 48.4% and 48.3%, respectively.
A total of 38/63 ITT subjects (60.3%) died while enrolled in this study, 20/32 (62.5%) in the CA4P group and 18/31 (58.1%) in the control group. The primary causes of death were disease-related. Treatment-emergent serious AEs were recorded in 32/60 subjects (53.3%) in the safety population overall: 16/31 (51.6%) in the CA4P group and 16/29 (55.2%) in the control group. Two subjects who received CA4P experienced three episodes of myocardial ischemia. Both subjects discontinued treatment due to the episodes. Hypertension was reported in 17/31 (54.8%) subjects in the CA4P arm compared with 13/29 (44.8%) subjects in the control arm. Among subjects who experienced hypertension on CA4P, increases in systolic and diastolic blood pressures were seen from 30 minutes post-dose through 2 hours post-dose and returned to baseline by 4 hours post-dose.
Survival and response
There were no statistically significant differences between the randomized treatment groups in RR, PFS, or OS. The overall best confirmed objective RR was 50% in the CA4P group compared with 32% in the control group (Table 4). Median PFS in the CA4P group was 8.6 months versus 9.3 months for the control group (HR 1.04; 95% CI, 0.56–1.91) (Figure 2A), and median OS in the CA4P group was 13.6 months versus 16.2 months in the control group (HR 1.06; 95% CI, 0.55–2.03) (Figure 2B).
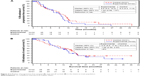  | Figure 2 K-M plots of progression-free survival (A) and overall survival (B) in the intent-to-treat population. |
Multiple post hoc analyses were performed. Trends were seen toward longer survival in subjects treated with CA4P when the baseline tumors measured more than 10 cm (14.2 vs 11.0 months, HR, 0.67; 95% CI, 0.26, 1.70) and when subjects were anemic at baseline (12.0 vs 6.3 months, HR, 0.54; 95% CI, 0.18, 1.65).
Discussion
This is the first clinical trial evaluating the safety and efficacy of a VDA in combination with bevacizumab, carboplatin, and paclitaxel in adult subjects with chemotherapy-naïve stage IIIB/IV nonsquamous NSCLC. Based on evidence that CA4P is well tolerated in combination with paclitaxel and carboplatin, and that CA4P and bevacizumab may have synergistic effects on tumor vasculature, this randomized, multicenter, controlled, open-label, Phase II clinical trial explored the safety and potential benefit of adding CA4P to triple-combination therapy in subjects with advanced NSCLC.
Dose reductions and/or delays were infrequent in the CA4P and control groups. Dose adjustments of bevacizumab, paclitaxel, and carboplatin due to neutropenia or leukopenia occurred more frequently in the control group compared with the CA4P group. CA4P dose modifications due to neutropenia or leukopenia were reported in approximately one-third of subjects.
The most common TEAEs were neutropenia, leukopenia, and hypertension, all of which had an increased incidence with CA4P versus controls. CA4P postinfusion blood pressure increase has been shown to be controllable in animal models with nitrates or calcium channel blockers.32,33 One study in a hypertensive rat model examined the potential for cardiotoxicity with CA4P using serum troponin I levels 24 hours postadministration. Pretreatment with an antihypertensive effectively blocked both the CA4P-induced blood pressure increase and cardiac damage.
Both subjects who experienced the three episodes of myocardial ischemia, events that were not associated with any evidence of infarction, had a history of hypertension. Of interest, one occurrence coincided with an episode of CA4P postinfusion blood pressure increase, which was not pretreated with an antihypertensive agent, while another occurred during the bevacizumab infusion, 24 hours post-CA4P infusion. The incidence of treatment-related serious AEs was similar between the treatment groups.
The numerical difference between the treatment groups in overall tumor response should be interpreted cautiously because of a relatively small sample size. Interpretation of PFS data is further confounded by the high number of subjects who discontinued prior to disease progression. This study was not adequately powered to assess efficacy, and the 95% CI for the HR for the primary efficacy endpoint of PFS includes the possibility that either arm is nearly twice as effective as its comparator. Larger studies are necessary to provide enough power to analyze this regimen for efficacy. It should also be noted that, as testing for many of the currently known markers were not standard at the time the study was conducted, there was no attempt to correlate clinical outcome with tumor tissue; as a result, these outcomes should be considered in light of the absence of correlative data. In light of recent advances in the management of advanced NSCLC, development of chemotherapy plus an antiangiogenic agent and a VDA should be considered in other settings in which antiangiogenic therapy is currently indicated and initial evidence of efficacy of the combination has been seen, such as recurrent ovarian cancer,22 prior to further evaluation in advanced NSCLC.
In conclusion, data from the current study showed that CA4P combined with carboplatin, paclitaxel, and bevacizumab had an acceptable toxicity profile in subjects with NSCLC. The difference in RR also suggested evidence of activity in NSCLC. It is hoped that these results might serve as a guide for the development of protocols for future studies in other cancer types where combination vascular targeted therapy with an antiangiogenic and VDA might enhance patient outcomes.
Acknowledgments
The authors thank the participating patients and their families; James A. Neidhart, MD from San Juan Oncology Associates; the investigators; Kim Perkins from the FALCON team at Mateon Therapeutics (formerly OXiGENE, Inc); and former FALCON team members Pallavi Rao, Freya Zsombory, Frances McNamara, and Shiao-Ping Lu for their invaluable contributions to the study and the creation of this manuscript. Medical writing services were provided by Christopher Caiazza. This study was sponsored by Mateon Therapeutics (formerly OXiGENE, Inc.). Preliminary results of this study were presented as a poster at the 2010 Annual Meeting of the American Society of Clinical Oncology. See Garon EB et al. J Clin Oncol. 2010;28:15s (suppl; abstr 7587).
Disclosure
JB was employed by OXiGENE, Inc at the time of conducting the study. The authors report no other conflicts of interest in this work.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29. | ||
American Cancer Society. What is non-small cell lung cancer? Available from: http://www.cancer.org/cancer/lungcancer-non-smallcell/detailedguide/non-small-cell-lung-cancer-what-is-non-small-cell-lung-cancer. Accessed January 4, 2016. | ||
Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373(2):123–135. | ||
Garon EB, Rizvi NA, Hui R, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med. 2015;372(21):2018–2028. | ||
Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–957. | ||
Solomon BJ, Mok T, Kim DW, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371(23):2167–2177. | ||
Folkman J, Merler E, Abernathy C, Williams G. Isolation of a tumor factor responsible for angiogenesis. J Exp Med. 1971;133(2):275–288. | ||
Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355(24):2542–2550. | ||
Garon EB, Ciuleanu TE, Arrieta O, et al. Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): a multicentre, double-blind, randomised phase 3 trial. Lancet. 2014;384(9944):665–673. | ||
Mok TS, Loong HH. A REVELation in non-small-cell lung cancer treatment? Lancet. 2014;384(9944):640–642. | ||
Prise VE, Honess DJ, Stratford MR, Wilson J, Tozer GM. The vascular response of tumor and normal tissues in the rat to the vascular targeting agent, combretastatin A-4-phosphate, at clinically relevant doses. Int J Oncol. 2002;21(4):717–726. | ||
Rini BI, Garcia JA, Cooney MM, et al. A phase I study of sunitinib plus bevacizumab in advanced solid tumors. Clin Cancer Res. 2009;15(19):6277–6283. | ||
Das M, Wakelee H. Vascular disrupting agents. J Thorac Oncol. 2010;5(12 Suppl 6):S482–S483. | ||
Gridelli C, Rossi A, Maione P, et al. Vascular disrupting agents: a novel mechanism of action in the battle against non-small cell lung cancer. Oncologist. 2009;14(6):612–620. | ||
McKeage MJ, Von Pawel J, Reck M, et al. Randomised phase II study of ASA404 combined with carboplatin and paclitaxel in previously untreated advanced non-small cell lung cancer. Br J Cancer. 2008;99(12):2006–2012. | ||
Lara PN Jr, Douillard JY, Nakagawa K, et al. Randomized phase III placebo-controlled trial of carboplatin and paclitaxel with or without the vascular disrupting agent vadimezan (ASA404) in advanced non-small-cell lung cancer. J Clin Oncol. 2011;29(22):2965–2971. | ||
Mazzone P, Mekhail T. Current and emerging medical treatments for non-small cell lung cancer: a primer for pulmonologists. Respir Med. 2012;106(4):473–492. | ||
National Institutes of Health. A study of ASA404 or placebo in combination with docetaxel in second-line treatment for (stage IIIb/IV) non-small cell lung cancer (ATTRACT-2). Available from: https://clinicaltrials.gov/ct2/show/study/NCT00738387?term=ASA404&rank=11. Accessed January 4, 2016. | ||
Landuyt W, Verdoes O, Darius DO, et al. Vascular targeting of solid tumours: a major ‘inverse’ volume-response relationship following combretastatin A-4 phosphate treatment of rat rhabdomyosarcomas. Eur J Cancer. 2000;36(14):1833–1843. | ||
Siemann DW, Rojiani AM. The vascular disrupting agent ZD6126 shows increased antitumor efficacy and enhanced radiation response in large, advanced tumors. Int J Radiat Oncol Biol Phys. 2005;62(3):846–853. | ||
Sosa JA, Elisei R, Jarzab B, et al. Randomized safety and efficacy study of fosbretabulin with paclitaxel/carboplatin against anaplastic thyroid carcinoma. Thyroid. 2014;24(2):232–240. | ||
Monk BJ, Sill MW, Walker JL, et al. Randomized phase II evaluation of bevacizumab versus bevacizumab plus fosbretabulin in recurrent ovarian, tubal, or peritoneal carcinoma: an NRG oncology/gynecologic oncology group study. J Clin Oncol. 2016;34(19):2279–2286. | ||
Pettit GR, Singh SB, Niven ML, Hamel E, Schmidt JM. Isolation, structure, and synthesis of combretastatins A-1 and B-1, potent new inhibitors of microtubule assembly, derived from Combretum caffrum. J Nat Prod. 1987;50(1):119–131. | ||
Dowlati A, Robertson K, Cooney M, et al. A phase I pharmacokinetic and translational study of the novel vascular targeting agent combretastatin A-4 phosphate on a single-dose intravenous schedule in patients with advanced cancer. Cancer Res. 2002;62(12):3408–3416. | ||
Rustin GJS, Galbraith SM, Anderson H, et al. Phase I clinical trial of weekly combretastatin A4 phosphate: clinical and pharmacokinetic results. J Clin Oncol. 2003;21(15):2815–2822. | ||
Stevenson JP, Rosen M, Sun W, et al. Phase I trial of the antivascular agent combretastatin A4 phosphate on a 5-day schedule to patients with cancer: magnetic resonance imaging evidence for altered tumor blood flow. J Clin Oncol. 2003;21(23):4428–4438. | ||
Nathan P, Zweifel M, Padhani AR, et al. Phase I trial of combretastatin A4 phosphate (CA4P) in combination with bevacizumab in patients with advanced cancer. Clin Cancer Res. 2012;18(12):3428–3439. | ||
Rustin GJ, Shreeves G, Nathan PD, et al. A Phase Ib trial of CA4P (combretastatin A-4 phosphate), carboplatin, and paclitaxel in patients with advanced cancer. Br J Cancer. 2010;102(9):1355–1360. | ||
Siemann DW, Shi W. Dual targeting of tumor vasculature: combining avastin and vascular disrupting agents (CA4P or OXi4503). Anticancer Res. 2008;28(4B):2027–2031. | ||
Shaked Y, Ciarrocchi A, Franco M, et al. Therapy-induced acute recruitment of circulating endothelial progenitor cells to tumors. Science. 2006;313(5794):1785–1787. | ||
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–247. | ||
Ke Q, Bodyak N, Rigor DL, Hurst NW, Chaplin DJ, Kang PM. Pharmacological inhibition of the hypertensive response to combretastatin A-4 phosphate in rats. Vascul Pharmacol. 2009;51(5–6):337–343. | ||
Ke Q, Samad MA, Bae S, Chaplin DJ, Kang PM. Exaggerated hypertensive response to combretastatin A-4 phosphate in hypertensive rats: effective pharmacological inhibition by diltiazem. Vascul Pharmacol. 2015;74:73–79. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




