Back to Journals » Clinical Ophthalmology » Volume 10
A randomized, double-masked, parallel-group, comparative study to evaluate the clinical efficacy and safety of 1% azithromycin–0.1% dexamethasone combination compared to 1% azithromycin alone, dexamethasone 0.1% alone, and vehicle in the treatment of subjects with blepharitis
Authors Hosseini K, Lindstrom R, Foulks G, Nichols K
Received 17 April 2016
Accepted for publication 6 June 2016
Published 10 August 2016 Volume 2016:10 Pages 1495—1503
DOI https://doi.org/10.2147/OPTH.S110739
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Kamran Hosseini,1 Richard L Lindstrom,2,3 Gary Foulks,4 Kelly K Nichols5
1InSite Vision, Alameda, CA, 2Minnesota Eye Consultants, 3Department of Ophthalmology and Visual Neurosciences, University of Minnesota Medical School, Minneapolis, MN, 4Department of Ophthalmology and Vision Science, School of Medicine, University of Louisville, Louisville, KY, 5School of Optometry, University of Alabama at Birmingham, Birmingham, AL, USA
Purpose: To evaluate the clinical efficacy and safety of a 1% azithromycin–0.1% dexamethasone combination in DuraSite (“combination”) compared to 0.1% dexamethasone in DuraSite, 1% azithromycin in DuraSite, and vehicle in the treatment of subjects with blepharitis.
Materials and methods: This was a Phase III, double-masked, vehicle-controlled, four-arm study in which 907 subjects with blepharitis were randomized to combination (n=305), 0.1% dexamethasone (n=298), 1% azithromycin (n=155), or vehicle (n=149). Ten study visits were scheduled: screening visit, days 1 and 4 (dosing phase) and 15, and months 1–6 (follow-up phase). On day 1, subjects applied one drop of the study drug to the eyelid of the inflamed eye(s) twice daily, and continued with twice-daily dosing for 14 days. After completing 14 days of dosing, subjects were followed for 6 months for efficacy and safety.
Results: A total of 57 subjects (6.3%) had complete clinical resolution at day 15: 25 (8.2%), 17 (5.7%), 8 (5.2%), and 7 (4.7%) subjects in the combination-, 0.1% dexamethasone-, 1% azithromycin-, and vehicle-treatment groups, respectively. The combination was superior to 1% azithromycin and vehicle alone, but not to 0.1% dexamethasone alone. Mean composite (total) clinical sign and symptom scores improved in all four treatment groups during the posttreatment evaluation phase for the intent-to-treat population, but outcomes were superior when a drop containing 0.1% dexamethasone was utilized. Clinical response was noted as early as day 4, and persisted as long as 6 months. Most adverse events were considered mild in severity and not related to the study drug.
Conclusion: A higher percentage of subjects in the combination group achieved complete clinical resolution of the signs and symptoms of blepharitis at day 15 than with 1% azithromycin and vehicle, but outcomes were similar to treatment with 0.1% dexamethasone alone. The combination was well tolerated.
Keywords: blepharitis, dexamethasone, azithromycin, eyelid inflammation
Introduction
Chronic blepharitis is a common multifactorial ocular disease commonly associated with eyelid inflammation and secondary ocular irritation.1,2 The disease is chronic, difficult to manage, supposedly recurs often, and its chronicity can lead to scarring of the eyelid and loss of proper eyelid and tear-film function. There are no therapeutic guidelines, and the standard treatment involves local lid hygiene and eyelid scrubs with warm-compress lid therapy. Topical and systemic antibiotics, topical corticosteroids, and tear-replacement therapy are common adjunctive therapies. Antibiotics are used to decrease the bacterial load, while corticosteroids are used to relieve inflammation. Clinical trials have shown antibiotics and corticosteroids can produce “significant” improvement in signs and symptoms.3
Topical azithromycin is a second-generation macrolide under investigation for the treatment of blepharitis. This broad-spectrum antibiotic has antimicrobial and anti-inflammatory activities, as well as lipid-inducing effects, and has been observed in open-label studies to provide significant clinical benefits.4–10
Currently available ocular antibiotic–steroid fixed-dose combination products are typically dosed every 4–6 hours. ISV-502 (hereafter referred to as “combination”) is an ophthalmic formulation of the antibiotic azithromycin and the corticosteroid dexamethasone formulated in DuraSite (InSite Vision, Alameda, CA, USA). This drug-delivery system has been designed as a long-acting topical eyedrop that can be dosed twice daily for 14 days, which should improve treatment compliance. Safety and efficacy of systemic azithromycin have been documented during the 25+ years it has been marketed in the US. An ophthalmic solution (AzaSite; InSite Vision) was approved for marketing in 2007 for the treatment of bacterial conjunctivitis.11 Similarly, dexamethasone has been used since the mid-1960s to treat numerous inflammatory conditions, including allergy, skin conditions, and ulcerative colitis. In ophthalmic indications, dexamethasone is approved to treat conjunctivitis, keratitis, and diabetic macular edema.12
This study (C-10-502-004; NCT01408082) was designed to evaluate the efficacy and safety of the combination compared with 0.1% dexamethasone alone, 1% azithromycin in DuraSite, and vehicle applied twice daily for 14 days to subjects with blepharitis. Clinical efficacy was defined as complete resolution of signs and symptoms at day 15.
Materials and methods
Study design
This Phase III, randomized, double-masked, vehicle-controlled, four-arm study evaluated the efficacy and safety of the combination compared to 0.1% dexamethasone, to 1% azithromycin, and to vehicle in 907 subjects with blepharitis. Follow-up was 6 months (including the 14-day dosing period) to evaluate recurrence rates and long-term safety of the combination.
The study was conducted in compliance with all applicable governmental rules, ethical principles, Good Clinical Practice regulations, International Conference on Harmonisation guidelines, and in accordance with the Declaration of Helsinki. The study protocol for all sites was reviewed and approved by Copernicus IRB (Durham, NC, USA). The trial was registered at ClinicalTrials.gov under the registry number NCT01408082.
Written informed consent was obtained from all subjects. At each study site, subjects were randomized sequentially by assigning the number corresponding to the lowest-numbered drug kit available at the site. All investigators were masked to the randomization code. All study medications were administered from identical multidose containers, so that neither the participant nor the investigator knew which medication the subject was receiving. All medications were identical in color (colorless) and viscosity, so the appearance of the drug was the same to all the subjects.
Study population
Following eligibility screening, a total of 907 subjects were enrolled and assigned to one of four groups: combination 1% azithromycin and 0.1% dexamethasone in DuraSite (InSite Vision), 0.1% dexamethasone in DuraSite, 1% azithromycin in DuraSite, or vehicle alone in a 2:2:1:1 ratio, respectively, according to a randomization schedule generated by the trial’s sponsor. All enrolled subjects had used lid-scrub therapy prior to study enrollment and were at least 18 years of age; sex and race were not considered in the inclusion criteria. All subjects had best-corrected visual acuity of 20/100 or better in each eye, intraocular pressure (IOP) of ≤22 mmHg in either eye, had used lid scrubs for at least 1 week prior to the day 1 study visit, and had a clinical diagnosis of blepharitis, defined as a minimum combined score of 5 for the signs and/or symptoms in at least one eye. Each sign or symptom – eyelid redness, eyelid swelling, eyelid debris, and eyelid irritation – could be scored at four different values: 0 (absent), 1 (mild), 2 (moderate), and 3 (severe). The enrolled study eye must have had a minimum score of 1 for eyelid redness and a minimum score of 1 for eyelid irritation. For subjects who had both eyes qualify, the eye with the highest total clinical sign and symptom score on day 1 was designated as the study eye. If the total score was the same for both eyes, the right eye was designated as the study eye for efficacy analyses.
Among the study-exclusion criteria were previous eyelid surgery within 12 months before study entry or during the study that would interfere with study parameters, as determined by the investigator of record; acute ocular infection (bacterial, viral, or fungal) or active ocular inflammation other than blepharitis in the study eye; used topical corticosteroid or topical ophthalmic medications within 14 days before study enrollment; used any nondiagnostic topical ophthalmic solution in the study eye within 2 hours before study enrollment; used eye makeup during the dosing period; had any clinically significant lash or lid abnormality other than blepharitis in the study eye; or had moderate-to-severe dry eye in the study eye.
Planned treatment protocol
Subjects in each treatment arm were directed to apply the study medication to inflamed study eyelids twice daily (at approximately 12-hour intervals) for 14 days. After placing the single drop on the subject’s eyelid, subjects were instructed to rub the drop in gently with the tip of a precleaned finger. The first dose of medication was administered under an investigator’s supervision. Study participants subsequently were responsible for the remaining instillations.
Instructions for administering all other doses at home were provided, and patients were asked to complete a dosing diary. Subjects were instructed to bring the bottles of study medication and the subject diary at each planned study visit and return for all subsequent visits.
Examination procedures
Visual acuity, biomicroscopy, IOP, and ophthalmoscopy examinations were conducted in the treated eye(s) at specified intervals during the study. At screening and day 1 visits, standardized photographs were taken of both eyes. Photos of only the study eye were taken at day 15, with all subsequent visits to be used as a visual reference of the severity of subject’s blepharitis.
Identification of study medications
All study medications were formulated with the polymeric drug-delivery system DuraSite (polycarbophil, sodium chloride, ethylenediaminetetraacetic acid disodium, and sterile water for injection; InSite Vision), which prolongs the drug’s residence time on the ocular surface and allows for distribution of the drug into the conjunctiva, cornea, and eyelids for ocular conditions. DuraSite also maintains the dexamethasone suspension and increases viscosity upon instillation, allowing for use as both an eyedrop or as an alternative to an ointment.
The vehicle consisted of a formulation with the same viscosity and appearance as the study medications. It contained sodium hydroxide, mannitol, poloxamer 407, citric acid anhydrous, sodium citrate, and DuraSite. All formulations were preserved with benzalkonium chloride 0.003%.
Per protocol clinical visits
At the screening visit (visit 1), the investigator performed an initial eye examination, including assessment of best-corrected visual acuity, signs and symptoms of blepharitis in both eyes, biomicroscopy, and IOP measurement. Subjects not meeting the appropriate inclusion criteria were disqualified. Subjects meeting the enrollment criteria were asked to use lid scrubs in the inflamed eyes for at least 1 week prior to the enrollment visit.
At the enrollment visit (visit 2/day 1), the investigator repeated an eye examination to confirm the total blepharitis score remained above 5; if subjects were below that score, they were not enrolled. Enrolled subjects then were instructed to self-administer their first dose to the inflamed eyelid(s), to self-administer their second dose at home at bedtime, and then twice daily in the morning and evening for a total of 14 days. A dosing diary was used to record the medication-application times. Patients were instructed to bring their bottles of medication and dosing diaries with them to their next two visits.
The following two visits (3 and 4) were designated as a “safety visit” and an “end of dosing visit,” respectively. At the end of the dosing visit, eye examinations and the patients’ response were used to gauge any improvement (or worsening) of the blepharitis. From this point, patients who remained in the study were assigned to a monthly follow-up period up to 6 months after the end of dosing to ascertain the lasting effect of their improvement (and/or signs and symptoms relapse) and to monitor their overall ocular health.
Blepharitis quality-of-life questionnaire
A blepharitis quality-of-life (QoL) questionnaire was drafted in collaboration with experts from the University of California, Los Angeles and reviewed by the US Food and Drug Administration. Subjects completed the questionnaire at screening, day 1, day 15, and month 6 visits. Subjects who exited the study before the month 6 follow-up completed the questionnaire at their last study visit.
Investigator global efficacy rating
Investigators provided a global efficacy rating for each subject at day 4, day 15, and monthly during the posttreatment phase using the following scoring system based on the clinical signs and symptoms of blepharitis (eyelid redness, eyelid swelling, eyelid debris, eyelid irritation):
- 0= cured: all signs and/or symptoms of blepharitis clear
- 1= improved: signs and/or symptoms still present but of less severity than at pretreatment
- 2= no change: signs and/or symptoms unchanged from pretreatment
- 3= worsened: signs and/or symptoms worse than at pretreatment.
Outcome measurements
End points were based on the total composite score (0–12) of the ratings (0–3 for each item) for each of the following clinical signs: eyelid redness, eyelid swelling, and eyelid debris, and the clinical symptom of eyelid irritation.
The primary efficacy end point was the proportion of subjects with complete clinical resolution (total summed score of 0) of signs and symptoms at day 15 when comparing combination and 1% azithromycin. For the comparison between combination and 0.1% dexamethasone, the primary efficacy end point was the proportion of subjects with recurrence of clinical signs and symptoms by visit 10 (6-month follow-up). Recurrence was defined as a change in total composite sign and symptom score of ≥4 at month 6 from day 15 in the study eye, and had to include a score of 1 for eyelid redness and a score of 1 for eyelid irritation. Recurrence was only evaluated for those who reached clinical resolution at day 15.
Secondary efficacy end points included individual clinical sign and symptom ratings of eyelid redness, eyelid swelling, eyelid debris, and eyelid irritation; the composite clinical sign and symptom score; time to recurrence (score ≥4 with score of at least 1 for both eyelid redness and eyelid irritation) or exacerbation (score increase from day 15) within the evaluation phase; and severity of recurrence or exacerbation, as determined by the composite clinical sign and symptom score. Additionally, the investigator’s global efficacy rating and the QoL questionnaire were used as subjective end points, and are not reported here.
Results
Disposition and demographics
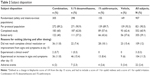
Of the 907 subjects randomized in the study, 552 (60.9%) completed the study through month 6. The average age of subjects was 60 (range 18–92) years, with 44.3% being ≥65 years old. The majority of subjects were white (86.1%) and female (56.8%). See Table 1 for subject demographics.
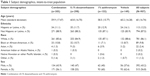  | Table 1 Subject demographics, intent-to-treat population |
All enrolled subjects received at least one dose of the study drug and were included in the both the intent-to-treat (ITT) and safety populations. Three subjects were lost to follow-up immediately following enrollment, and four other subjects discontinued the study without any postdose clinical assessments, leaving 900 enrolled subjects with a postdose clinical assessment.
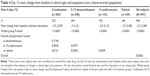
There were 355 of 907 subjects (39.1%) who exited the study before the month 6 visit. Of 907 subjects, 900 completed the dosing period through day 15. These subjects had some degree of improvement in one or more sign(s) or symptom(s). The most frequent reason for exiting the study early was either inability to reach complete clinical resolution (score of 0 for all signs and symptoms) or an increase in signs and symptoms after day 15. Table 2 summarizes patient disposition, in particular the percentage of subjects per study arm that did not achieve a score of 0 in all signs and symptoms and/or achieved additional improvement after completion of the dosing period (day 15). Further, qualified subjects were required to use lid scrubs for at least 1 week prior to study enrollment (day 1); at day 1, subjects were rescreened to ensure lid-scrub use did not affect study entry criteria. If lid-scrub use effectively reduced total blepharitis score, subjects were discontinued from the study.
Efficacy
Primary end points
Of the subjects who completed the study, 57 (6.3%) had complete clinical resolution (total score 0) at day 15. Specifically, 25 (8.2%), 17 (5.7%), 8 (5.2%), and 7 (4.7%) of subjects in the combination-, 0.1% dexamethasone-, 1% azithromycin-, and vehicle-treatment groups, respectively, achieved the primary end point of complete clinical resolution at day 15. There were no statistically significant differences noted among any of the treatment groups. The 57 subjects with complete clinical resolution were assessed for the coprimary end point: proportion of subjects with recurrence of clinical signs and symptoms by 6 months. However, the low number of subjects did not allow for meaningful comparisons among the four groups.
Secondary end points
Individual clinical signs and symptoms
Eyelid redness. The mean decrease in eyelid-redness score was similar between the combination- and 0.1% dexamethasone-treatment groups throughout the study. Statistically significantly greater improvement at day 4 and day 15 occurred in the combination-treatment group compared to 1% azithromycin (P=0.0059 and P=0.0025, respectively) and compared to vehicle (P=0.0188 and P=0.0240, respectively). Table 3 summarizes the changes in eyelid redness at day 15.
Eyelid swelling. Eyelid swelling was most improved at visit 4 (day 15) for all treatment groups and continued to improve in all four treatment groups during the posttreatment evaluation phase for the ITT population.
Eyelid debris. The maximum decrease in mean eyelid-debris score occurred at visit 4 (day 15) for all treatment groups. The combination-treatment group showed statistically significantly greater improvement in eyelid-debris mean score than the 1% azithromycin-treatment group (P=0.0108) at visit 4 (day 15).
Eyelid irritation. Improvements in mean scores for eyelid irritation were seen in all four treatment groups during the posttreatment evaluation phase for the ITT population, with the biggest change from the preceding visit occurring at visit 4 (day 15). The combination treatment showed statistically significantly greater improvement in the mean eyelid-irritation score than 1% azithromycin (P≤0.0286) at visit 5 (1 month), visit 7 (3 months), and visit 8 (4 months). The combination treatment also showed statistically significantly greater improvement in eyelid-irritation mean score than 0.1% dexamethasone (P=0.0403) at visit 6 (2 months).
Composite clinical sign and symptom score
Mean composite (total) clinical sign and symptom scores improved in all four treatment groups during the posttreatment evaluation phase for the ITT population, with the largest decrease from a preceding visit occurring at visit 4 (day 15) in all four treatment groups (Table 4). Table 5 confirmed the improvement in total clinical scores observed at day 15 was maintained through month 6 (visit 10).
Safety
The majority of adverse events (AEs) were considered mild in severity across all treatment groups. A total of 19 subjects experienced a serious AE during the study (all nonocular), and none was judged by the investigator to be related to the study drug. Of the ocular AEs leading to study withdrawal, most were mild, occurred during the dosing period, and resolved; those occurring after the dosing period were mostly systemic, unrelated events. Increased IOP/ocular hypertension occurred in more subjects treated with combination than with 0.1% dexamethasone, 1% azithromycin, or vehicle (9, 3, 2, and 0 subjects, respectively). AEs are reported in Table 6.
Discussion
Blepharitis continues to challenge clinicians: there are numerous treatment options to manage the disease, but none are ideal. While lid scrubs and warm compresses used in combination with antibiotics and/or anti-inflammatory agents are the most frequently used management strategy, recurrence remains high. With 907 subjects randomized and evaluated, this clinical trial is the largest controlled study on a topical medical treatment ever conducted in subjects diagnosed with blepharitis.
Overall, our results showed the azithromycin–dexamethasone combination used for 14 days twice daily was safe and well tolerated. While this study failed to reach its primary efficacy end point of complete clinical resolution (score of 0 for all signs and symptoms) of both clinical signs and symptoms of blepharitis, the combination drop achieved complete clinical resolution in a greater percentage of patients (8.2%) than 1% azithromycin (5.2%), 0.1% dexamethasone (5.7%), or vehicle (4.7%). In most of the secondary efficacy analyses, the combination azithromycin–dexamethasone drop was statistically superior to 1% azithromycin, but similar to 0.1% dexamethasone. Both drops containing 0.1% dexamethasone improved the clinical signs of blepharitis more than 1% azithromycin or vehicle alone, and this treatment effect was maintained through the month 6 visit. This suggests that topical 0.1% dexamethasone is a more powerful agent than 1% azithromycin alone in treating blepharitis. Much has been written on the positive treatment effect of azithromycin on blepharitis,1,4–6,13–15 but this is the first large-scale clinical trial evaluating its safety and efficacy.
The same 1% azithromycin–0.1% dexamethasone combination in DuraSite has been previously studied as a treatment for blepharoconjunctivitis, where it proved to be superior to both azithromycin alone and dexamethasone alone in achieving a clinical cure and reducing bacterial colony-count scores.16 In this study, the combined 1% azithromycin–0.1% dexamethasone was superior to 1% azithromycin and vehicle alone, but not to 0.1% dexamethasone alone. Blepharitis and blepharoconjunctivitis represent a diverse spectrum of disease, and the difference in study outcomes may be a reflection of the multimodality of the disease state, rather than the investigated treatments. Luchs summarized several studies evaluating 1% azithromycin for blepharitis where efficacy was reported, but most of the studies were small in nature and open-label in design.6 In our study, both drops containing 0.1% dexamethasone were found to be superior to 1% azithromycin or vehicle alone in resolving the clinical signs of eyelid redness and eyelid debris. In this study, no evaluation of bacterial eradication was performed, and many clinicians believe the addition of an antibiotic is important to manage microbial overgrowth.
There are several strengths to this study. The first is the large number of patients enrolled. In addition, this is the first study to evaluate the safety and efficacy of a treatment for blepharitis for 6 months postdosing. In most other studies, patients were only followed until day 15 or at most 1 month.1,6 The longer follow-up was selected to detect a possible recurrence rate and evaluate the long-term efficacy and safety of 1% azithromycin and 0.1% dexamethasone alone and in combination. Our study, while large and enrolling more than 900 subjects, also retained the majority of subjects through the 6-month follow-up. This suggests that longer treatment regimens may be necessary in some patients, in order to achieve and maintain complete clinical resolution.
There are some limitations to this study, however. There were a small number of patients who reached full resolution by study exit (a primary end point). This could be reflective of overall poor end-point choice, but discussions with the US Food and Drug Administration dictated these chosen end points. Unfortunately, the small numbers also mean we are unable to generalize our findings to a wider potential patient base. Finally, our QoL questionnaire had not been validated in time to generate more than subjective impressions.
Further study of the 1% azithromycin–0.1% dexamethasone combination is indicated, considering the positive outcomes of this study and the prior trial on blepharoconjunctivitis. Eyelid redness appears to be a preferred sign to evaluate in blepharitis management, along with the symptoms of ocular irritation. The role of bacterial overgrowth in the pathophysiology of blepharitis and blepharoconjunctivitis also deserves more study.
Acknowledgments
William B Krebs and Jiali Tang provided biostatistical support, funded by InSite. Michelle Dalton, ELS provided editorial assistance in the preparation of this manuscript, funded by InSite.
Author contributions
Study design was undertaken by KH, patient evaluations and disease management by KH, RLL, GF, and KKN, and manuscript development by KH, RLL, GF, and KKN.
Disclosure
KH is an employee (chief medical officer and vice president, clinical and regulatory affairs) of InSite Vision. RLL, GF, and KKN are consultants to InSite Vision and members of the InSite scientific advisory board. InSite Vision is now a subsidiary of Sun Pharmaceutical Industries. All aspects of this study were undertaken by InSite Vision prior to its acquisition. RLL consults for Alcon, Allergan, Bausch + Lomb, and Sun Pharmaceuticals. GF consults for Kala Inc., Lexitas Pharma, Inc., and Parion, Inc. KKN or her spouse consult for Allergan, Kala, Science Based Health, Parion, Santen, and Shire and receive research grants from Allergan, Eleven Biotherapeutics, Kala, Shire, Tear Science, and Vistakon. The authors report no other conflicts of interest in this work.
References
Fadlallah A, Rami HE, Fahd D, et al. Azithromycin 1.5% ophthalmic solution: efficacy and treatment modalities in chronic blepharitis. Arq Bras Oftalmol. 2012;75(3):178–182. | ||
Auw-Haedrich C, Reinhard T. [Chronic blepharitis: pathogenesis, clinical features, and therapy]. Ophthalmologe. 2007;104(9):817–826; quiz 27–28. German. | ||
Pflugfelder SC, Karpecki PM, Perez VL. Treatment of blepharitis: recent clinical trials. Ocul Surf. 2014;12(4):273–284. | ||
John T, Shah AA. Use of azithromycin ophthalmic solution in the treatment of chronic mixed anterior blepharitis. Ann Ophthalmol (Skokie). 2008;40(2):68–74. | ||
Luchs J. Efficacy of topical azithromycin ophthalmic solution 1% in the treatment of posterior blepharitis. Adv Ther. 2008;25(9):858–870. | ||
Luchs J. Azithromycin in DuraSite for the treatment of blepharitis. Clin Ophthalmol. 2010;4:681–688. | ||
Amar T, Caillaud T, Elena PP. Ocular pharmacokinetic study following single and multiple azithromycin administrations in pigmented rabbits. Curr Eye Res. 2008;33(2):149–158. | ||
Chiambaretta F, Garraffo R, Elena PP, et al. Tear concentrations of azithromycin following topical administration of a single dose of azithromycin 0.5%, 1.0%, and 1.5% eyedrops (T1225) in healthy volunteers. Eur J Ophthalmol. 2008;18(1):13–20. | ||
Retsema J, Fu W. Macrolides: structures and microbial targets. Int J Antimicrob Agents. 2001;18 Suppl 1:S3–S10. | ||
Liu Y, Kam WR, Ding J, Sullivan DA. Effect of azithromycin on lipid accumulation in immortalized human meibomian gland epithelial cells. JAMA Ophthalmol. 2014;132(2):226–228. | ||
AzaSite [package insert]. Whitehouse Station, NJ: Inspire Pharmaceuticals; 2007. | ||
Maxidex [package insert]. Fort Worth, TX: Alcon Laboratories Inc; 2003. | ||
Akpek EK, Vittitow J, Verhoeven RS, et al. Ocular surface distribution and pharmacokinetics of a novel ophthalmic 1% azithromycin formulation. J Ocul Pharmacol Ther. 2009;25(5):433–439. | ||
Opitz DL, Harthan JS. Review of azithromycin ophthalmic 1% solution (AzaSite®) for the treatment of ocular infections. Ophthalmol Eye Dis. 2012;4:1–14. | ||
Opitz DL, Tyler KF. Efficacy of azithromycin 1% ophthalmic solution for treatment of ocular surface disease from posterior blepharitis. Clin Exp Optom. 2011;94(2):200–206. | ||
Hosseini K, Hutcheson J, Lindstrom RL. A phase III clinical study to evaluate the efficacy of combined azithromycin and dexamethasone in the treatment of blepharoconjunctivitis. Clin Ophthalmol. 2013;7:2225–2234. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.