Back to Journals » Drug Design, Development and Therapy » Volume 12
A randomized, double-blind clinical trial of canrenone vs hydrochlorothiazide in addition to angiotensin II receptor blockers in hypertensive type 2 diabetic patients
Authors Derosa G, Gaudio G, Pasini G, D'Angelo A , Maffioli P
Received 12 September 2017
Accepted for publication 3 January 2018
Published 24 August 2018 Volume 2018:12 Pages 2611—2616
DOI https://doi.org/10.2147/DDDT.S151449
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sukesh Voruganti
Giuseppe Derosa,1–4 Giovanni Gaudio,5 Gianfranco Pasini,6 Angela D’Angelo,1,4 Pamela Maffioli1
1Department of Internal Medicine and Therapeutics, University of Pavia, Fondazione IRCCS Policlinico S Matteo, Pavia, Italy; 2Center for the Study of Endocrine-Metabolic Pathophysiology and Clinical Research, University of Pavia, Pavia, Italy; 3Center for Prevention, Surveillance, Diagnosis and Treatment of Rare Diseases, Fondazione IRCCS Policlinico S Matteo, Pavia, Italy; 4Laboratory of Molecular Medicine, University of Pavia, Pavia, Italy; 5Internal Medicine Division, Ospedale Angelo Bellini, Somma Lombardo, Varese, Italy; 6Cardiologic Unit, Ospedale di Gavardo, Brescia, Italy
Aim: The aim of this study was to evaluate the effects of canrenone compared to hydrochlorothiazide (HCTZ) added to angiotensin II receptor blockers (ARBs) on glycemia, lipid profile, potassium, aldosterone and renal function in patients with hypertension and type 2 diabetes mellitus.
Patients and methods: The study enrolled 182 Caucasian patients with hypertension and type 2 diabetes mellitus. Patients were already taking ARBs and were randomized to canrenone, 50 mg once a day, or HCTZ, 12.5 mg once a day for 1 month. After the first month, patients not reaching an adequate blood pressure (BP) were up-titrated to canrenone 100 mg or HCTZ 25 mg once a day for 12 months. The following parameters were considered at 6 and 12 months: BP, body weight, body mass index (BMI), fasting plasma glucose (FPG), post-prandial glucose (PPG), fasting plasma insulin (FPI), homeostasis model assessment insulin (HOMA-IR), lipid profile, potassium, plasma aldosterone, urine albumin excretion rate and estimated glomerular filtration rate (eGFR).
Results: We observed a similar decrease in BP with both treatments. Canrenone led to a significant decrease in FPG, PPG and HOMA index compared to baseline, while there was a significant increase in the same parameters with HCTZ. HCTZ also worsened glycated hemoglobin (HbA1c), while canrenone did not change it. No variations in lipid profile were recorded with canrenone, while there was a worsening of total cholesterol (TC) and triglycerides (Tg) with HCTZ. Potassium levels were decreased and uric acid levels were increased by HCTZ, but not by canrenone that had a neutral effect on these parameters. We recorded a slight decrease in eGFR with HCTZ and an improvement with canrenone; creatinine and eGFR were improved by canrenone compared to HCTZ. Plasma aldosterone levels were decreased by canrenone and increased by HCTZ.
Conclusion: Canrenone and HCTZ have a similar effect on BP; however, canrenone seems to improve metabolic parameters, while HCTZ worsens them.
Keywords: canrenone, hydrochlorothiazide, type 2 diabetes mellitus, metabolism
A Letter to the Editor has been received and published for this article.
Introduction
Aldosterone is the primary endogenous agonist ligand for the mineralocorticoid receptors. It induces active reabsorption of sodium and consequent passive reabsorption of water by kidneys; it also plays a role in active potassium secretion in the cortical collecting tubule and in secretion of active protons in the luminal membrane of the intercalated cells of the collecting tubule. For these reasons, aldosterone leads to an increased blood pressure (BP) and blood volume.1 Based on this, it appears clear that mineralocorticoid receptor antagonists can play an important role in BP control. Actually, two generations of mineralocorticoid receptor antagonists have been marketed: spironolactone and canrenone belong to the first generation, while eplerenone belongs to the second generation. Compared to the first-generation agents, eplerenone is more selective, but less effective, with no active metabolites and a shorter half-life.2 Compared to spironolactone, canrenone induces less adverse events such as gynecomastia, because canrenone prevents the genesis of intermediate products with anti-androgenic and progestational effects.3 Aldosterone already proved to have a positive effect in reducing some factors involved in metabolic syndrome and in reducing insulin resistance and inflammatory markers levels observed in patients affected by metabolic syndrome.4,5
We have already conducted a study comparing canrenone or hydrochlorothiazide (HCTZ) added to valsartan/amlodipine combination in type 2 diabetic hypertensives.6 The results showed that canrenone added to valsartan/amlodipine combination had a better effect in reducing urinary albumin excretion compared to HCTZ addition; however, data on glycometabolic parameters were not fully investigated. This double-blind, randomized clinical trial was aimed to investigate if canrenone would be a better choice than HCTZ in not only obtaining a better BP control but also not to worsen glycometabolic effects, the action on electrolytes and renal function in patients affected by type 2 diabetes mellitus and hypertension.
Patients and methods
Study design
This double-blind, multi-center, controlled clinical trial study was conducted at the Department of Internal Medicine and Therapeutics, University of Pavia, Pavia, Italy (coordinating site); Internal Medicine Division, Ospedale Angelo Bellini, Somma Lombardo, Varese, Italy, and Cardiologic Unit, Ospedale di Gavardo, Brescia, Italy.
The study protocol was approved by the ethics committee of Fondazione IRCCS Policlinico San Matteo and was conducted following the Declaration of Helsinki and its amendments and the Good Clinical Practice Guidelines.
Patients
We enrolled 182 Caucasian patients older than 18 years, of either sex (Table 1), overweight and with type 2 diabetes mellitus and hypertension according to the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD) Guidelines criteria.7 To be included, patients needed to take an angiotensin II receptor blocker (ARB), at a stable dose, from at least 3 months. We excluded patients with secondary hypertension or BP levels ≥160/100 mmHg, patients with a genetic condition affecting lipid metabolism (eg, familial hypercholesterolemia, type III hyperlipidemia and LPL deficiency) or patients with total cholesterol (TC) >240 mg/dL and/or with triglycerides (Tg) >400 mg/dL. We also excluded subjects with impaired hepatic and/or renal function or severe anemia (hemoglobin level <8 g/dL). We did not include patients with thyroid diseases, history of alcohol or drug abuse or patients with neoplastic, infectious, inflammatory or autoimmune diseases. Patients with previous cardiovascular or cerebrovascular conditions within 6 months before study start were excluded. Pregnant or breastfeeding women or women not taking adequate contraceptive precautions were not included.
Patients were identified from review of case notes and/or computerized clinic registers and were contacted personally or by telephone. All patients provided written informed consent to participate in the trial.
Treatments
The patients fulfilling the inclusion and exclusion criteria were randomized to add to their current therapy canrenone 50 mg or HCTZ 12.5 mg daily for 1 month; after 1 month, patients not reaching adequate BP (established as BP <140/90 mmHg) were up-titrated to canrenone 100 mg or HCTZ 25 mg daily. Both treatments were maintained for 12 months (Figure 1). Both canrenone and HCTZ were supplied as identical, opaque, white capsules in coded bottles to ensure the blind status of the study. Randomization was done with envelopes containing randomization codes prepared by a statistician. A copy of the code was provided only to the statistician. The code was broken after database lock but could have been broken for individual subjects in cases of an adverse event. All subjects were supplied with two bottles containing a supply of the study medication for at least 100 days; the first dose was taken the day after the visit. Patient compliance was evaluated by counting pills returned by patients at the visit.
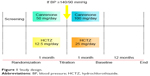  | Figure 1 Study design. |
Diet and exercise
Subjects were encouraged to follow a controlled-energy diet based on the recommendations of the American Heart Association.8 Standard diet advice was given by a dietician and/or a specialist doctor.
Assessments
At study start, patients were interviewed regarding their medical history and underwent an accurate physical examination and a 12-lead electrocardiogram. The following parameters were collected: BP, body weight, body mass index (BMI), fasting plasma glucose (FPG), post-prandial glucose (PPG), glycated hemoglobin (HbA1c), fasting plasma insulin (FPI), homeostasis model assessment (HOMA) index, TC, high-density lipoprotein-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C), Tg, urine albumin excretion rate (UAER), estimated glomerular filtration rate (eGFR), creatinine, potassium, plasma aldosterone and uric acid.
In order to evaluate the tolerability assessments, all adverse events were recorded.
For a description of how various parameters and BP were assessed, please see our previous paper.5
Safety measurements
Physical examination, vital sign, weight, electrocardiogram and laboratory tests were considered for safety monitoring purpose. All adverse events were recorded.
Statistical analysis
Considering an α error of 0.05, a sample of 75 patients per group was required to obtain a 90% power. An intention-to-treat analysis was performed. Continuous variables were evaluated using a two-way repeated measures analysis of variance (ANOVA), while intervention effects were adjusted for the presence of potential confounding variables using analysis of covariance (ANCOVA). Statistical analysis was performed using the Statistical Package for the Social Sciences software version 14.0 (SPSS Inc., Chicago, IL, USA). A p-value of <0.05 was considered significant. Variables normally distributed were presented as mean ± SD, whereas variables with skewed distribution were analyzed after logarithmic transformation.9
Results
Study sample
We enrolled 182 patients (92 were randomized to canrenone and 90 were randomized to HCTZ); 163 patients completed the study. The characteristics of the patients at baseline are shown in Tables 1 and 2. Antidiabetic treatments taken at baseline are listed in Table 3.
  | Table 3 Antidiabetic treatment |
BP
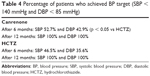
A significant, similar decrease in systolic blood pressure (SBP) and diastolic blood pressure (DBP) was obtained with both canrenone and HCTZ after 6 and 12 months, without differences between groups. At 6 months, 52.7% of patients treated with canrenone and 46.5% of patients treated with HCTZ achieved SBP pressure target (SBP < 140 mmHg). Regarding DBP pressure target (<85 mmHg), the percentage was 42.9% for canrenone and 35.6% for HCTZ (p < 0.05 vs HCTZ). At 12 months, all patients reached BP target, without difference between the two treatments (Table 4).
Metabolic parameters
There was a significant decrease in FPG, PPG and HOMA index with canrenone compared to baseline (p < 0.05), while HCTZ increased the same parameters (p < 0.05 vs baseline and p < 0.05 vs canrenone). HCTZ also worsened HbA1c (p < 0.05 vs baseline and p < 0.05 vs canrenone), while canrenone did not change it.
Lipid profile was not affected by canrenone, while TC (p < 0.05 vs baseline) and Tg (p < 0.01 vs baseline) were increased with HCTZ. Both TC and Tg were higher with HCTZ compared to canrenone (p < 0.05).
Renal parameters
Potassium levels were decreased (p < 0.05 vs baseline) and uric acid levels were increased (p < 0.01 vs baseline) by HCTZ but not by canrenone that had a neutral effect on these parameters.
We recorded a slight decrease in eGFR with HCTZ (p < 0.01 vs baseline) and an improvement with canrenone (p < 0.05); creatinine and eGFR were improved by canrenone compared to HCTZ (p < 0.01). Plasma aldosterone levels were decreased by canrenone (p < 0.01 vs baseline) and increased by HCTZ (p < 0.05 vs baseline and p < 0.01 vs canrenone).
Adverse events
Gynecomastia was reported in 3% of patients taking canrenone and in 2% of patients taking HCTZ. No menstrual abnormalities were reported.
Discussion
Our study showed a similar effect of canrenone and HCTZ in decreasing BP, according to what we have previously reported.6 The effects of canrenone on BP were already previously reported in two previous papers where the authors reported that the systolic and diastolic BP (24 h, daytime and nighttime) and mean arterial and pulse pressures were significantly reduced when canrenone was added to the preexisting therapy.10,11 Moreover, the authors did not observe any significant differences between canrenone 50 and 100 mg: among patients treated with canrenone 50 mg, 67.5% and 74% normalized the 24 h systolic and diastolic BP, respectively, and among patients treated with 100 mg, 61.6% and 68.5% (p not significant for 50 vs 100 mg).10
What really differentiate canrenone from HCTZ are the effects on glycometabolic control. Regarding this, canrenone better improved glycometabolic control compared to HCTZ.
The positive effect of canrenone and the negative effect of HCTZ on metabolism can be explained considering the two different mechanisms of action. Considering all the physiological effects of aldosterone, HCTZ has two opposite actions: a negative effect due to the stimulation of aldosterone synthesis as a consequence of the volume depletion and a positive effect due to its diuretic effect and the reduction of BP it causes. On the other hand, canrenone is able to activate the renin angiotensin aldosterone system and has the advantage that it cannot produce an aldosterone-like effect being an aldosterone receptor blocker. This point is very important since both drugs can further control BP, but while thiazides increase plasma aldosterone activating mineralocorticoid receptors, canrenone increases aldosterone without activating the receptors.12
This is in line with what was previously reported in the literature.13,14 The authors observed that HCTZ worsens the cardiovascular risk due to the stimulation of aldosterone, while canrenone ameliorates this parameter being mineralocorticoid receptor blocker.
It is interesting to understand why, during treatment with canrenone, our data showed a reduction in aldosterone levels; this disagrees with previously published studies conducted with canrenone.15 This may be due to the fact that canrenone was used in combination with ARB therapy, which suppresses aldosterone levels. The lack of increase in aldosterone could also be interpreted as a lack of diuretic action.
Conclusion
Our study showed that canrenone and HCTZ have a similar effect on BP; however, canrenone seems to improve metabolic parameters, while HCTZ worsened them.
Acknowledgments
The abstract of this paper was presented at the ESC Congress 2016 as a poster presentation. The poster’s abstract was published in “Poster Abstracts” in European Heart Journal, 2016, Volume 37, Issue suppl_1, page 66. The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending or royalties. No writing assistance was utilized in the production of this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Stewart P. The adrenal cortex. In: Kronenberg HM, Melmed S, Polonsky KS, Larsen RP, editors. Williams Textbook of Endocrinology. 11 ed. Philadelphia, PA: Saunders Elsevier; 2008:445–504. | ||
Hawkins UA, Gomez-Sanchez EP, Gomez-Sanchez CM, Gomez-Sanchez CE. The ubiquitous mineralocorticoid receptor: clinical implications. Curr Hypertens Rep. 2012;14(6):573–580. | ||
Mantero F, Lucarelli G. Aldosterone antagonists in hypertension and heart failure. Ann Endocrinol (Paris). 2000;61(1):52–60. | ||
Derosa G, Bonaventura A, Bianchi L, et al. Effects of canrenone in patients with metabolic syndrome. Expert Opin Pharmacother. 2013;14(16):2161–2169. | ||
Derosa G, Romano D, Bianchi L, D’Angelo A, Maffioli P. The effects of canrenone on inflammatory markers in patients with metabolic syndrome. Ann Med. 2015;47(1):47–52. | ||
Fogari R, Derosa G, Zoppi A, Lazzari P, D’Angelo A, Mugellini A. Comparative effect of canrenone or hydrochlorothiazide addition to valsartan/amlodipine combination on urinary albumin excretion in well-controlled type 2 diabetic hypertensive patients with microalbuminuria. Expert Opin Pharmacother. 2014;15(4):453–459. | ||
Rydén L, Standl E, Bartnik M, et al; Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC); European Association for the Study of Diabetes (EASD). Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur Heart J. 2007;28(1):88–136. | ||
Lichtenstein AH, Appel LJ, Brands M, et al. Summary of American Heart Association diet and lifestyle recommendations revision 2006. Arterioscler Thromb Vasc Biol. 2006;26(10):2186–2191. | ||
Winer BJ. Statistical Principles in Experimental Design. 2nd ed. New York: McGraw-Hill; 1971. | ||
Derosa G, Maffioli P, D’Avino M, et al; ESCAPE-IT Trial Investigators Group. Efficacy and safety of two dosages of canrenone as add-on therapy in hypertensive patients taking ace-inhibitors or angiotensin II receptor blockers and hydrochlorothiazide at maximum dosage in a randomized clinical trial: the ESCAPE-IT trial. Cardiovasc Ther. 2017;35(1):47–54. | ||
Guasti L, Gaudio G, Lupi A, et al. Ambulatory blood pressure parameters after canrenone addition to existing treatment regimens with maximum tolerated dose of angiotensin-converting enzyme inhibitors/angiotensin II type 1 receptor blockers plus hydrochlorothiazide in uncontrolled hypertensive patients. Drug Des Devel Ther. 2017;11:2293–2300. | ||
Armanini D, Sabbadin C, Donà G, Clari G, Bordin L. Aldosterone receptor blockers spironolactone and canrenone: two multivalent drugs. Expert Opin Pharmacother. 2014;15(7):909–912. | ||
Armanini D, Fiore C. Choice of diuretic therapy and reconsideration for aldosterone receptors blockers. Hypertension. 2010;55(1):e5. | ||
Ma J, Lee KV, Stafford RS. Changes in antihypertensive prescribing during US outpatient visits for uncomplicated hypertension between 1993 and 2004. Hypertension. 2006;48(5):846–852. | ||
de Simone G, Chinali M, Mureddu GF, et al; AREA-in-CHF Investigators. Effect of canrenone on left ventricular mechanics in patients with mild systolic heart failure and metabolic syndrome: the AREA-in-CHF study. Nutr Metab Cardiovasc Dis. 2011;21(10):783–791. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.