Back to Journals » Local and Regional Anesthesia » Volume 16
A Randomized Controlled Trial to Compare the Efficacy of Single versus Triple Injection Technique for Ultrasound-Guided Infraclavicular Block in Upper Limb Surgeries
Authors Vedavyas R, Saravanan R , Mirunalini G , Gayathri B
Received 19 February 2023
Accepted for publication 10 May 2023
Published 18 May 2023 Volume 2023:16 Pages 51—58
DOI https://doi.org/10.2147/LRA.S409211
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Stefan Wirz
Raksha Vedavyas, Ravi Saravanan, Gunaseelan Mirunalini, Balasubramaniam Gayathri
Department of Anesthesiology, SRM Medical College Hospital and Research Center, SRMIST, Kattankulathur, Tamil Nadu, India
Correspondence: Gunaseelan Mirunalini, Department of Anesthesiology, SRM MCH RC, SRMIST, No. 219, Second Floor, Block B, SRM Nagar, Chengalpattu District, Kattankulathur, Tamil Nadu, 603203, India, Tel +91 9486131643, Email [email protected]
Introduction: The ultrasound-guided infraclavicular brachial plexus block by triple-point injection method was aimed at blocking the three individual cords in the infraclavicular region. Recently, a single-point injection method which does not require visualization of cords to produce nerve block has been introduced. This study compared the block onset time, performance time, patient’s satisfaction, and complications between the ultrasound guided triple-point injection and single-point injection methods.
Patients and Method: This randomized controlled trial was conducted in a tertiary care hospital. Sixty patients were divided into two groups – Group S: 30 patients received single-point injection method of infraclavicular block. Group T: 30 patients received triple-point injection method of infraclavicular block. Drugs used were 0.5% ropivacaine with 8 mg dexamethasone.
Results: The sensory onset time was significantly longer in Group S (11.13 ± 1.83 min) than Group T (6.20 ± 1.19min). No statistically significant difference was found between the two groups regarding mean motor onset time. The composite sensorimotor onset time was similar between the groups. The mean time to perform the block was significantly lesser in Group S (1.35 ± 0.38 min) when compared to group T (3.44 ± 0.61min). The patient satisfaction score, conversion to general anesthesia and complications were not significant among the two groups.
Conclusion: We concluded that single-point injection method had a shorter performance time and similar total onset time with less procedural complications compared with triple point injection method.
Keywords: ultrasonography, interventional, infraclavicular, anesthesia, ropivacaine, dexamethasone, patient satisfaction
Introduction
Infraclavicular brachial plexus block (ICBPB) provides anesthesia for upper limb surgeries below the elbow. After formation in the neck, the brachial plexus travels along the inter-scalene groove and passes between the clavicle and the first rib. In the infraclavicular fossa, it divides into three cords and lies beneath the fascia of the pectoralis minor muscle. The three cords, namely the lateral, medial and posterior cords, are spread around the axillary artery and then continue as terminal nerves to supply the upper arm. The infra-clavicular approach blocks the plexus at the level of the cords.
Because of the anatomical difficulty in accessing the cords, the ultrasound-guided visualization and administration of the block have gained more popularity than the landmark and nerve stimulation methods.1,2 Until the previous decade, the ultrasound-guided infraclavicular approach aimed at identifying the three individual cords around the axillary artery and blocking them individually by administering local anesthetics.
The infraclavicular space is occupied by many small blood vessels. The cords can be identified at three to five centimetres from the skin. Even by ultrasound method, much effort is needed to visualize the fascia of the pectoral muscles and the cords beneath them, which is crucial to obtain a successful block. In order to completely block all three cords separately, the ultrasound probe and the needle must be repositioned several times during the procedure.3 Furthermore, technical expertise is needed to approach the cords around the blood vessels.4
The New York School of Regional Anesthesia has recently stated that the visualization of the cords is not necessary for a successful block.5 Instead, a single-point injection posterior to the axillary artery completely blocks all three cords. A few studies have been conducted to compare the triple versus single-point injection method and have come to varied conclusions regarding the success rates and the time of block onset.6–9 Therefore, this randomized controlled study was planned to compare the single-point injection approach of the infraclavicular block with the conventional triple-point separate cord approach method in terms of onset time, performance time, patient satisfaction and complication rate.
We hypothesized that the ultrasound-guided single-point injection infraclavicular block method would be superior to the conventionally performed triple-point injection method in the onset time and performance time in patients undergoing surgery for upper limb fractures. The study’s primary objective was to compare the composite sensorimotor onset time of the block. The secondary objectives were to compare the time required to perform the block, the patient satisfaction score assessed by the Numeric Rating Scale (NRS), the rate of block failure, and technique-associated complications.
Methods
This study was approved by the SRM Medical College Hospital and Research Centre institutional ethical committee (2386/IEC/2021), registered in the clinical trials registry of India (CTRI/2022/06/04330), and conducted according to the Helsinki Declaration standards for trials on humans in a tertiary care hospital between July 2022 and December 2022. Informed written consent was obtained from all the study participants. The confidentiality of all the participants was maintained throughout the study period. Sixty patients between 18 and 60 years, ASA class 1–3, with BMI ranging from 18 to 30 and who were posted for upper limb orthopedic surgeries below the elbow were included in the study. Patients who were unwilling to participate and those who had coagulopathy, sepsis, hepatic or renal failure, pregnancy, allergy to local anesthetics, pre-existing neuropathy, and prior surgery in infraclavicular fossa were excluded from the study.
A computer-generated random number and sealed envelope technique were used to randomize and allocate the patients to specific groups. Patients and the principal investigator who observed the various timings were not aware of the group allotment. On the day before surgery, a thorough clinical examination was performed, the patients were explained about the anesthetic technique, and written informed consent was obtained. On the day of the procedure, the patients were divided into two groups: Group S received an ultrasound-guided single-point injection method of the infraclavicular block, and Group T received an ultrasound-guided triple-point injection method of the infraclavicular block. All the ultrasound-guided blocks were conducted by an anesthesiologist with more than five years of experience.
After arrival in the premedication area, standard anesthesia monitors were attached, and oxygen was administered. Intravenous midazolam (0.02 mg/kg) was administered to all patients. All the ICBPBs were performed in the anesthesia procedure room approximately one hour before the scheduled surgery. Patients were made to lie supine with heads turned to the other side. The arm was positioned with 90-degree abduction. A soft pad was placed in the interscapular region to make access to the plexus easier. Under strict aseptic conditions and local anesthetic skin infiltration with 2mL of lidocaine 1%, the ICBPB was performed using a GE LOGIQ V2 ultrasound machine with a high-frequency (8–13 MHz) linear transducer probe. The ultrasound probe was placed vertically in the lateral end of the infraclavicular fossa and adjusted to obtain the best image of the axillary artery and 30 mL of 0.5% ropivacaine with 8 mg dexamethasone was administered in both groups.
In group S, using an in-plane approach, the needle was inserted in the craniocaudal direction and positioned beneath the axillary artery corresponding approximately to the 6’o clock position. Then, 30 mL of the drug was administered after negative aspiration for blood. The spread of the drug was visually confirmed by the appearance of U shaped or double bubble-like distribution of local anesthetic surrounding the artery (Figure 1B). In group T, the needle was placed at three different positions around the vessel corresponding to the location of the three cords - 6 o’clock position for the posterior cord, 8 o’clock position for the lateral cord, and 2 o’clock position for the medial cord. Then, 10 mL of the drug was administered at each position to surround all the cords (Figure 1A).
The principal investigator recorded the various times. The anesthesiologist announced the procedure’s start when the probe was placed over the patient and the ending time was announced when the local anesthetic was deposited entirely. This was taken as the total procedural time. The onset time for sensory and motor blocks was done every two minutes from the time of completion of block administration. The musculocutaneous, median, radial, and ulnar nerves were examined for loss of cold sensation. Each nerve was examined individually and was assigned scores as follows. Score 0 = can feel cold; 1 = patient cannot feel cold but can feel touch, 2 = patient cannot feel cold and touch.
Similarly, the motor blockade of the musculocutaneous nerve was tested by elbow flexion; the radial nerve was tested by thumb abduction; the median nerve was assessed by thumb opposition; and the ulnar nerve was assessed by thumb adduction. The motor blockade of the individual nerves was given scores: Score 0 = able to move freely, 1 = able to move but not freely, 2 = unable to move. Overall, the maximal composite sensorimotor score was 16. When the patient attained a score of at least seven in sensory component and a score of 14 out of the total 16 the block was considered adequate for surgical anesthesia. The time was noted from the completion of block administration till the score of 14 was attained. This time was defined as the onset time.
A dedicated anesthesiologist was present with the patient throughout the intraoperative period to monitor the vitals and address any patient discomfort. The block was considered failed if the sensory score was less than seven, the composite score was less than 14 at the end of 30 minutes, or the patient experienced pain during the surgery. The failed blocks were treated at the discretion of the attending anesthesiologist, either by supplemental nerve blocks, opioid analgesics, or conversion to general anesthesia. The principal investigator noted these details. At the end of the surgery, the patient satisfaction score was recorded using a numeric rating scale, with a 0 to 10 score, ten being highly satisfactory and zero being total dissatisfaction.
Complications related to the block, like vascular puncture, residual postoperative paraesthesia, local anesthetic systemic toxicity, and pneumothorax, were noted.
The study’s sample size was calculated using the G*Power software version 3.1.9.4. The effect size was determined using the means and standard deviations of the performance time from the previous similar study done by Lee et al.7 With the power of 85% and alpha error of 0.05, the estimated sample size was 52. Considering the dropouts, we included 60 patients in our study.
The collected study data were analyzed using SPSS software version 21. Before analyzing the data, each variable was checked for missing values, blank values, and typing errors. Continuous variables like age, weight, height, Body Mass Index (BMI), time to perform the block, sensory onset time, motor onset time, total onset time, and mean fentanyl supplementation were expressed as mean and standard deviation. Description of categorical variables like gender, ASA PS status, complications, conversion to GA, rescue blocks, and total analgesics required was expressed as frequency and proportion. Ordinal data like patient satisfaction score was expressed as median with the interquartile range. Shapiro–Wilk test was used to confirm the normal distribution of data, and no skewing was observed. An Independent Student’s t-test was used to compare two groups of means. In addition, the chi-square test was employed to compare the distribution of qualitative variables between the two groups. All tests were two-tailed, with results considered statistically significant if the p-value was less than 0.05.
Results
The flow of study participants through the study is shown in the CONSORT flow chart (Figure 2). The demographic characteristics of the participants (Table 1) were statistically comparable. Table 2 shows the results of the study outcomes. The total composite sensorimotor onset time of the block was comparable between the groups. However, on separate assessments, the sensory onset time was prolonged in group S compared to group T, which was significant (p = 0.001).
 |
Table 1 Comparison of Patients’ Characteristics Between Groups |
 |
Table 2 Comparison of Outcome Variables Between Groups |
 |
Figure 2 Consolidated standards of reporting trials (CONSORT) flow chart depicting the flow of participants through the study. |
On the other hand, the motor onset time showed no statistical significance difference between the groups (p = 0.104). The mean time to perform the block was 1.35 ± 0.38 minutes in group S and 3.44 ± 0.61 minutes in group T. The p-value was 0.001.
The total duration of surgery in group S was 168.33 ± 9.24 minutes, and in group T was 170.47 ± 8.76 minutes, the difference of which was insignificant (p = 0.36). The mean fentanyl supplementation of study participants among the single injection group was 45.00 ± 25.96 mcg, and that of the triple injection group was 26.00 ± 33.69 mcg with a p-value of 0.018. Out of 30 patients in group S, five (16.7%) patients were converted to general anesthesia, and six (20%) needed rescue blocks. Among 30 patients in group T, three (10%) patients were converted to general anesthesia (GA), and four (13.3%) patients needed rescue block. Conversion to GA was slightly higher in the single-point injection group than the triple point injection group, although it was not significant, with a p-value of 0.448. The rate of rescue block was slightly higher in group S compared to group T, with a p-value of 0.488.
There was no incidence of pneumothorax and local anesthetic toxicity in both groups. Group T reported vascular puncture in 3 (10%) patients. In comparison, no incidence of vascular puncture in group S. Paraesthesia was observed in three (6.7%) patients in group S and four (13.3%) patients in group T. Table 3 compares the incidence of complications between the two groups. The median patient satisfaction score in the single-point injection group was 9 (8–9.25), and that of the triple-point injection group was 8 (7–9). There is no significant difference in the patient satisfaction scale between groups (p = 0.104), as shown in Figure 3.
 |
Table 3 Comparison of Complications Between Groups |
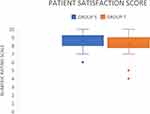 |
Figure 3 Box and whisker plot showing the numeric rating scale of the patient satisfaction scores. |
The total mean duration of analgesia of study participants among group S was 12.70 ± 4.25 hours, and that of group T was 11.67 ± 4.12 hours. The mean duration of analgesia was equally distributed in both groups, with a p-value of 0.343. Regarding the total postoperative analgesia, one patient (3.3%) among the single-point injection group needed 1 g of paracetamol after surgery, and 29 patients (96.7%) needed 2 g of paracetamol. Out of 30 patients in the triple point injection group, three (10%) required one gram of paracetamol, and 27 (90%) required two grams of paracetamol. The total postoperative analgesic requirement between the two groups was similar, with a p-value of 0.306. Table 3 compares the incidence of complications between the two groups.
Discussion
Over the past decade, studies have proven that ultrasound has tremendously reduced the performance times and reduced the complications for various blocks.10 Infraclavicular block, when performed under ultrasound guidance, prevents complications like phrenic nerve palsy and pleural injuries associated with other approaches.11–14 Studies have proven that ultrasound-guided ICBPC produced similar success rates as a supraclavicular block.15 Blockage of the musculocutaneous nerve is more common in the infraclavicular approach than the axillary approach.16
The infraclavicular approach to brachial plexus block was introduced early in the 20th century. Since its introduction, the conventional method for the ultrasound-guided ICBPB has been the triple point injection method. The three cords are visualized before depositing the local anesthetic drugs around each cord to achieve the desired analgesia. Due to the deeper anatomical location and many small vessels in that plane, the successful ICBPB demands specific technical expertise. Even though alternative newer method like the single point injection method has been introduced more recently, there have been some uncertainties regarding the method and the success rate of the block, leading to the less frequent usage of this method.
This study found that the time needed to attain the composite sensorimotor block was similar between the two methods. However, when the onset times were analyzed separately for sensory and motor blocks, the single-point injection method had a significantly faster sensory onset time. The total procedural time was also significantly shorter in the single-point injection method. The incidence of ICBPB-related complications, intraoperative and postoperative additional analgesic requirement, the requirement of supplemental nerve blocks or conversion to GA in failed blocks, and the technique-related patient satisfaction scores were all similar in both methods.
A study performed by Desgagnés et al,6 compared the ultrasound-guided ICBPB by single and triple point injection methods and found that the block onset at 15 minutes was achieved in 84% in the single point injection group and 78% in the triple-point injection group. They concluded that the onset time was similar between the two groups, the same as our study result.
In the same study, Desgagnes et al6 found that the time to perform block was significantly lesser in the single-point injection group (124 ± 62s) than triple-point injection (185 ± 72s). Fredrickson et al9 compared the procedural time between the single and triple point injection methods in the infraclavicular block. They found that the single-point injection (117 s) was faster than the triple-point injection (158 s). These results are similar to our study.
Regarding the success rates of the methods, our result was comparable to the results of the study by Aytuluk et al.17 They stated that both the methods (single point injection = 84.5% vs triple point injection = 94.1%) had similar success rates.
There were three incidences of accidental vascular puncture in the triple point injection group in our study. Lee et al7 studied the complications among the single-point and triple-point injection ICBPB and found no vascular or pleural punctures occurred during the procedures. Rodriguez et al,8 Fredrickson et al,9 and Aytuluk et al17 have concluded that there was no difference in the incidence of complications and conversion rates to general anesthesia between the two methods, which is also similar to the findings of our study. In our study, the most common reason for conversion to general anesthesia was patient anxiety and inadequate response to sedation. There were no incidences of complete block failure or intraoperative surgical site pain in either of the groups. Studies have proven that using a triple monitoring method for block administration using ultrasound, nerve stimulator and opening injection pressure techniques, the blocks’ safety and efficacy can be improved.18
The major strengths of our study are that we used the newer local anesthetic ropivacaine, which has not been exclusively studied in previous research on ICBPB and dexamethasone as an additive for the infraclavicular block has also not been studied previously. There are a few limitations in our study. First, in the ultrasound-guided infraclavicular approach, the needle insertion targeting the cords around the artery is more acute, which might be technically challenging in novice trainees and lead to more block failure and prolonged procedural time. Secondly, we did not use a nerve stimulator to administer block in our study. This could have provided a better inference for a reason for block failure in the single-point injection method. Third, we included only patients with BMI < 30. The USG-guided ICBPB might have been technically challenging in obese patients and could have given longer performance times.
Conclusion
Compared to the triple-point injection method, the single-point injection method had a shorter performance time, similar onset time, similar need for rescue blocks, and conversion to general anesthesia but with fewer procedural complications. Hence, we conclude that the single-point injection method of ultrasound-guided infraclavicular block can be an effective alternative to the classical triple-point injection method in patients requiring anesthesia for upper limb surgeries.
Data Sharing Statement
The data used to support the findings of this study were stored in a computerized database after deidentifying the participants and will be available with the corresponding author. The authors are willing to share the data regarding the outcome measures for research purpose upon request.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Abrahams MS, Aziz MF, Fu RF, Horn J-L. Ultrasound guidance compared with electrical neurostimulation for peripheral nerve block: a systematic review and meta-analysis of randomized controlled trials. Br J Anaesth. 2009;102(3):408–417. doi:10.1093/bja/aen384
2. Tsui B. Ultrasound-guidance and nerve stimulation: implications for the future practice of regional anesthesia. Can J Anaesth. 2007;54(3):165–170. doi:10.1007/BF03022635
3. Dingemans E, Williams SR, Arcand G, et al. Neurostimulation in ultrasound-guided infraclavicular block: a prospective randomized trial. Anesth Analg. 2007;104(5):1275–1280. doi:10.1213/01.ane.0000226101.63736.20
4. Macfarlane A, Anderson K. Infraclavicular brachial plexus blocks, continuing education in anaesthesia. Crit Care Pain. 2009;9(5):139143. doi:10.1093/bjaceaccp/mkp024
5. Atchabahian A, Vandepitte C, Lopez AM. Ultrasound-guided infraclavicular brachial plexus nerve block. New York School of Regional Anesthesia. Available from: https://www.nysora.com/topics/regional-anesthesia-for-specific-surgical-procedures/upper-extremity-regional-anesthesia-for-specific-surgical-procedures/anesthesia-and-analgesia-for-elbow-and-forearm-procedures/ultrasound-guided-infraclavicular-brachial-plexus-block/.
6. Desgagnés MC, Lévesque S, Dion N, et al. A comparison of a single or triple injection technique for ultrasound-guided infraclavicular block: a prospective randomized controlled study. AnesthAnalg. 2009;109(2):668–672.
7. Lee MG, Jung WS, Go DY, et al. Efficacy of a single injection compared with triple injections using a costoclavicular approach for infraclavicular brachial plexus block during forearm and hand surgery: a randomized controlled trial. Medicine. 2020;99(43):e22739. doi:10.1097/MD.0000000000022739
8. Rodríguez J, Bárcena M, Taboada-Muñiz M, et al. A comparison of single versus multiple injections on the extent of anaesthesia with coracoid infraclavicular brachial plexus block. Anesth Analg. 2004;99:1225–1230. doi:10.1213/01.ANE.0000131724.73956.8E
9. Fredrickson MJ, Wolstencroft P, Kejriwal R, et al. Single versus triple injection ultrasound-guided infraclavicular block: confirmation of the effectiveness of the single injection technique. Anesth Analg. 2010;111(5):1325–1327. doi:10.1213/ANE.0b013e3181f1bbb6
10. Cataldo R, Carassiti M, Costa F, et al. Starting with ultrasonography decreases popliteal block performance time in inexperienced hands: a prospective randomized study. BMC Anesthesiol. 2012;12:33. doi:10.1186/1471-2253-12-33
11. Kumar AN, Krishna NVM, Karthik VJ, et al. A randomized comparative study on brachial plexus block using nerve stimulator: infraclavicular - coracoid approach v/s supra-clavicular approach. Indian J Clin Anesth. 2017;4(1):8–12. doi:10.18231/2394-4994.2017.0003
12. Yang CW, Kwon HU, Cho CK, et al. A comparison of infra-clavicular and supraclavicular approaches to the brachial plexus using neurostimulation. Korean J Anesthesiol. 2010;58(3):260–266. doi:10.4097/kjae.2010.58.3.260
13. Satani TR, Shah SS, Rathod KB, et al. A comparison of infraclavicular and supraclavicular approaches to the brachial plexus. Int J Sci Res. 2012;2(12):442–445. doi:10.15373/22778179/DEC2013/136
14. Shah S, Mehta K, Patel K, et al. Comparison of infraclavicular brachial plexus block with supraclavicular brachial plexus block in upper limb surgeries. NHL J Med Sci. 2013;2:43–45. doi:10.4103/ija.IJA_402_16
15. Arcand G, Williams SR, Chouinard P, et al. Ultrasound-guided infraclavicular versus supraclavicular block. Anesth Analg. 2005;101:886–890. doi:10.1213/01.ANE.0000159168.69934.CC
16. Brenner D, Iohom G, Mahon P, et al. Efficacy of axillary versus infraclavicular brachial plexus block in preventing tourniquet pain: a randomized trial. Eur J Anaesthesiol. 2019;36(1):48–54. doi:10.1097/EJA.0000000000000928
17. Aytuluk HG, Colak T. The need for supplemental blocks in single versus triple injections in infraclavicular brachial plexus blocks with a medial approach: a clinical and anatomic study. Rev Bras Anestesiol. 2020;70:28–35.
18. Pascarella G, Strumia A, Costa F, et al. Triple monitoring may avoid intraneural injection during interscalene brachial plexus block for arthroscopic shoulder surgery: a prospective preliminary study. J Clin Med. 2021;10(4):781. doi:10.3390/jcm10040781
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

