Back to Journals » Neuropsychiatric Disease and Treatment » Volume 10
A positive correlation between serum amyloid β levels and depressive symptoms among community-dwelling elderly individuals in Japan
Authors Tsuruga K , Sugawara N , Yasui-Furukori N, Takahashi I, Tsuchimine S, Kaneda A, Nakaji S, Nakamura K
Received 4 May 2014
Accepted for publication 26 June 2014
Published 30 August 2014 Volume 2014:10 Pages 1621—1627
DOI https://doi.org/10.2147/NDT.S67205
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Koji Tsuruga,1 Norio Sugawara,1 Norio Yasui-Furukori,1 Ippei Takahashi,2 Shoko Tsuchimine,1 Ayako Kaneda,1 Shigeyuki Nakaji,2 Kazuhiko Nakamura1
1Department of Neuropsychiatry, 2Department of Social Medicine, Hirosaki University School of Medicine, Hirosaki, Japan
Background: Amyloid beta (Aβ) levels have been associated with an increased risk of Alzheimer’s disease (AD). As depression is common before the onset of AD, serum Aß levels could be associated with depressive symptoms. The aim of this study was to investigate whether serum Aβ levels are associated with depressive symptoms and/or cognitive function in community-dwelling elderly individuals.
Methods: We examined the association between serum Aβ levels and depression among 419 Japanese community-dwelling elderly individuals aged 60 years and over. Subjects were divided into two subgroups: younger elderly between 60 and 69 years old and older elderly over 69 years old. The Mini-Mental State Examination (MMSE) was used to assess cognitive function, and symptoms of depression were assessed using the Center for Epidemiologic Studies Depression Scale (CES-D). The ability to perform activities of daily living was evaluated using the Tokyo Metropolitan Institute of Gerontology Index of Competence. Serum Aβ levels were measured with a human amyloid beta enzyme-linked immunosorbent assay kit.
Results: After controlling for potential confounding variables, a multiple linear regression analysis showed that increased levels of serum Aβ40 and Aβ42 were associated with higher CES-D scores in the older elderly subgroup. Under the same condition, multiple regression showed that serum Aβ levels were not associated with MMSE scores among the total subjects, younger elderly, or older elderly.
Conclusion: Serum Aβ levels were associated with depressive symptoms in community-dwelling elderly individuals. The present study indicates the possibility that serum Aβ may be involved in the development of late-onset depression.
Keywords: Alzheimer’s disease, depression, dementia, Japanese
Introduction
Depression is a serious affective illness with heterogeneous etiologies and underlying pathologies.1–3 The unsatisfactory results of antidepressant medication and the high prevalence of somatic symptoms and physical illness in patients with depression imply that the serotonin hypothesis cannot fully explain the etiology of depression.4 In particular, late-onset depression is heterogeneous and requires various interventions,5 and different pathogenic processes are thought to occur between younger elderly and older elderly individuals with depression.6,7
Recently, an association between depression and cognitive impairment or dementia has been recognized.8,9 Although the mechanisms are not fully understood, a meta-analysis of studies concerning the association between depression and dementia showed that a history of depression significantly increased the risk of Alzheimer’s disease (AD) by twofold.10 AD is characterized by the presence of extracellular neuritic plaques and intracellular neurofibrillary tangles in the brain. Two major components of neuritic plaques, amyloid β1-40 (Aβ40) and amyloid β1-42 (Aβ42), have been associated with an increased risk of AD.11–13 Several studies have indicated that changes in Aβ40 and Aβ42 or the ratio of Aβ42 to Aβ40 levels in the blood may be associated with depression, but these results have been inconclusive.14–17
The objective of this study was to investigate whether serum Aβ levels are associated with depressive symptoms and/or cognitive function in Japanese community-dwelling elderly individuals. We hypothesized that depression among older elderly individuals would be more significantly associated with Aβ than that among younger elderly individuals.
Materials and methods
Participants
The subjects included 419 volunteers 60 years of age and over (150 males and 269 females) who participated in the Iwaki Health Promotion Project in 2012. The data collection for this study was approved by the ethics committee at the Hirosaki University School of Medicine, and all subjects provided written informed consent before participating in the project. Demographic information (age, sex, and level of education) was obtained from self-administered questionnaires and interviews.
Procedure
Blood samples were drawn and centrifuged immediately, and serum samples were stored at −80°C until use. A sandwich Aβ enzyme-linked immunosorbent assay kit (Wako, Osaka, Japan) was employed. The Aβ40 kit uses the BAN50 monoclonal antibody, which specifically detects the N-terminal portion of human Aβ (residues 1–16), and the BA27 monoclonal antibody, which detects the C-terminal portion of Aβ40. The Aβ42 kit uses BAN50 and the BC05 monoclonal antibody, which detects the C-terminal portion of Aβ42. The sensitivity has been reported as 0.019 pmol/L (dynamic range, 1.0–100 pmol/L) for Aβ40 and 0.06 pmol/L (dynamic range, 0.1–20 pmol/L) for Aβ42.18
The Mini-Mental State Examination (MMSE) was administered to all participants to measure their global cognitive status. This test assesses orientation to place and time, short-term memory, episodic long-term memory, subtraction ability, ability to construct a sentence, and oral language ability. The maximum score is 30, and scores less than 25 indicate poor cognitive function.19
The Japanese version of the Center for Epidemiologic Studies Depression Scale (CES-D) was administered to all of the participants to measure their depression symptoms.20,21 The CES-D is a 20-item self-report measure that focuses on depression symptoms during the week prior to administering the questionnaire. The maximum score on this scale is 60, and depression is considered present for subjects with CES-D scores of 16 or more.
The ability to perform activities of daily living was evaluated using the Tokyo Metropolitan Institute of Gerontology Index of Competence (TMIG-IC), a multidimensional 13-item scale.22 The TMIG-IC was developed to measure the functional capacity of an independently living elderly subject and is composed of three competencies: instrumental self-maintenance, intellectual activity, and social role. The TMIG-IC has been used in previous studies to examine the functional capacity of community-dwelling Japanese elderly.23,24
Statistical analysis
Data are presented as the mean ± standard deviation (SD). P-values of less than 0.05 were considered to be statistically significant. Because prevalence of dementia has increased from the 1970s,25 we divided the subjects into age subgroups of younger elderly between 60 and 69 years old and older elderly over 69 years old. Student’s unpaired t-test was used to analyze continuous variables, and a chi-square test was performed to analyze categorical variables between age subgroups. Pearson product moment correlation was used to explore the relationships among depression, cognitive function, and the serum Aβ (Aβ40, Aβ42, and Aβ40/Aβ42) levels among the total subjects, younger elderly, and older elderly. Multiple linear regression was employed for the MMSE and CES-D scores to analyze the associations among Aβ40, Aβ42, and Aβ40/Aβ42 levels. Regression analyses were adjusted for confounding factors (age, sex, level of education, and TMIG-IC score).
The data were analyzed using the PASW Statistics software for Windows, Version 18.0.0 (SPSS Inc., Chicago, IL, USA), and Amos software for Windows, Version 17.0 (SPSS Inc.).
Results
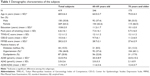
The demographic characteristics of the subjects are listed in Table 1. Compared with the younger elderly subgroup, the older elderly subgroup showed a significantly higher age, CES-D score, prevalence of hypertension, and level of Aβ40 and Aβ40/Aβ42, but the older elderly subgroup had a lower education level and MMSE score.
In the Pearson product moment correlation analysis, serum Aβ levels were not correlated with MMSE scores among the total subjects, younger elderly, or older elderly. After controlling for age, sex, level of education, and TMIG-IC score, the multiple regression showed that serum Aβ levels were not associated with MMSE scores among the total subjects, younger elderly, or older elderly (Table 2).
In the Pearson product moment correlation analysis, both serum Aβ40 and Aβ42 levels were positively correlated with CES-D scores in the older elderly subgroup. After controlling for age, sex, level of education, and TMIG-IC score, the multiple linear regression showed that both serum Aβ40 and Aβ42 levels were positively associated with CES-D scores only in the older elderly subgroup (Table 3).
Discussion
This cross-sectional study investigated the relationships among depressive symptoms, cognitive function, and serum Aβ levels among community-dwelling elderly individuals in Japan. We found that serum Aβ40 and Aβ42 levels were positively associated with depressive symptoms in the older elderly subgroup but not in the younger elderly subgroup.
Previous studies with a cross-sectional design exploring the relationships between depressive symptoms and plasma Aβ levels have shown inconsistent results. The first study in the US showed that 47 patients with late-life major depression had higher plasma Aβ42 levels than 30 younger controls.14 In another study in Korea among 123 community-dwelling elderly subjects, Moon and colleagues used the Short Geriatric Depression Scale-Korean version (SGDS-K) and found a positive association between plasma Aβ42 levels and depressive symptoms.26 In a population-based cohort of 980 elderly individuals from Rotterdam, Direk and colleagues showed that subjects with higher plasma Aβ40 levels had more depressive symptoms on the Center for Epidemiologic Studies Depression Scale (CES-D).17 The authors found that this cross-sectional association could be explained by subjects with depressive symptoms who developed dementia within the 11-year follow-up period. In contrast, several cross-sectional studies performed in the Nutrition, Aging, and Memory in the Elderly (NAME) study found the opposite association: depressed subjects had lower plasma levels of Aβ42 than the controls.15,27–29
Three longitudinal studies have analyzed the association between plasma Aβ levels and depression. A report from the Vienna Transdanube Aging (VITA) study showed that higher plasma Aβ42 levels at baseline predicted the conversion to depression among 331 subjects who fulfilled the criteria of having no previous history of depression and no dementia or depression at baseline.16 Among 988 community-dwelling elderly subjects in the US Health Aging and Body Composition (ABC) study, lower Aβ42/Aβ40 levels at baseline were associated with an increased risk of developing depression over a 9-year follow-up period, but only in ApoE4 carriers.30 In another study in the Netherlands that assessed 980 community-dwelling elderly subjects with the CES-D, Direk and colleagues also found that low levels of Aβ40 and Aβ42 without dementia were associated with an increased risk of depressive symptoms during the follow-up period.17 Until now, studies have not fully supported the view that subclinical depressive symptoms or clinical depression represents a risk factor for developing AD through a mechanism involving an increase or decrease in Aβ in the blood. However, we cannot completely rule out the possibility of an amyloid-related mechanism, as different disease stages of dementia occur throughout older age; therefore, the criteria used for depression (early onset vs late onset or acute vs chronic) and the apolipoprotein E4 allele could lead to changes of Aβ in the blood.
In the present study, we found that increased levels of serum Aβ40 and Aβ42 levels were associated with higher CES-D scores in the older elderly subgroup but not in the younger elderly subgroup. A previous study that stratified by age subgroup showed that serum Aβ42 levels were lower in subjects younger than 40 years old and in subjects older than 64 years old than in healthy controls, and differences in the severity of illness could have affected this difference.31 The participants in the study were inpatients who were clinically diagnosed with DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, 4th ed) major depressive disorder.
Several mechanisms may explain the positive correlation relation between serum Aβ levels and depressive symptoms. Higher serum Aβ levels might develop the depositions in the neurons and in cerebral vessels which may play a role in the etiology of depression.32,33 In addition, Aβ aggregations in small cerebral vessels can decrease cerebral blood flow and glucose utilization.
We found no relationship between cognitive function, as measured by the MMSE, and serum Aβ levels. However, the MMSE alone may not be sensitive to the subtle cognitive impairment that is present in depression, which may be associated with elevated serum Aβ42 levels. Furthermore, there is evidence linking executive dysfunction to structural and functional brain abnormalities, including white matter pathology, in depressed elderly subjects.34 Therefore, we cannot completely rule out the relationship between cognitive function and the level of Aβ.
The current study has several limitations. First, the cross-sectional nature of the study did not allow for causal assumptions between serum Aβ levels and depressive symptoms; future studies with longitudinal designs are needed to investigate these associations. Second, the assessment of depression was established by the CES-D rather than by a clinician-administered structured diagnostic interview. As a result, we collected no information about the onset or course of the disease. Third, several potential confounding factors, such as marital status, physical illness, and characterization of apolipoprotein E4 allele, were not assessed in our study. Furthermore, Aβ and depressive symptoms may share common genetic or environmental risk factors, such as diabetes and dyslipidemia, in the causal pathway. Although multiple regression analysis was performed, this explanation still cannot be excluded. Fourth, as all of the participants were volunteers who were interested in their health, they may have been healthier than the general population. Thus, the members of the community who were not involved in this study may have presented different depressive symptoms; this selection bias must be considered in future studies of community populations.
Conclusion
This study showed that serum Aβ levels were positively associated with depressive symptoms among community-dwelling elderly individuals. The present results support the possibility that Aβ in the blood may be involved in the development of late-onset depression, although further studies with longitudinal observations are warranted.
Acknowledgments
The authors are grateful to all volunteers who participated in this study. This study was funded by a grant from the Hirosaki Research Institute for Neuroscience. The funders had no role in the study design, data collection/analysis, decision to publish, or preparation of the manuscript.
Disclosure
Norio Yasui-Furukori has received grant/research support or honoraria from and spoken for Asteras, Dainippon, Eli Lilly, GlaxoSmithKline, Janssen-Pharma, Meiji, Mochida, Merck Sharp & Dohme, Otsuka, Pfizer, Takada, and Yoshitomi. The remaining authors declare that they have no other conflicts of interest in this work.
References
Van den Berg MD, Oldehinkel AJ, Bouhuys AL, Brilman EI, Beekman AT, Ormel J. Depression in later life: three etiologically different subgroups. J Affect Disord. 2001;65:19–26. | ||
Byers AL, Yaffe K. Depression and risk of developing dementia. Nat Rev Neurol. 2011;7:323–331. | ||
Kupfer DJ, Frank E, Phillips ML. Major depressive disorder: new clinical, neurobiological, and treatment perspectives. Lancet. 2012;379: 1045–1055. | ||
Su KP. Biological mechanism of antidepressant effect of omega-3 fatty acids: how does fish oil act as a ‘mind-body interface’? Neurosignals. 2009;17:144–152. | ||
Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58:249–265. | ||
Mehta M, Whyte E, Lenze E, et al. Depressive symptoms in late life: associations with apathy, resilience and disability vary between young–old and old–old. Int J Geriatr Psychiatry. 2008;23:238–243. | ||
Yoshimura K, Yamada M, Kajiwara Y, Nishiguchi S, Aoyama T. Relationship between depression and risk of malnutrition among community-dwelling young–old and old–old elderly people. Aging Ment Health. 2013;17:456–460. | ||
Butters MA, Young JB, Lopez O, et al. Pathways linking late-life depression to persistent cognitive impairment and dementia. Dialogues Clin Neurosci. 2008;10:345–357. | ||
Steffens DC, Otey E, Alexopoulos GS, et al. Perspectives on depression, mild cognitive impairment, and cognitive decline. Arch Gen Psychiatry. 2006;63:130–138. | ||
Ownby RL, Crocco E, Acevedo A, John V, Loewenstein D. Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Arch Gen Psychiatry. 2006;63:530–538. | ||
Schupf N, Tang MX, Fukuyama H, et al. Peripheral Abeta subspecies as risk biomarkers of Alzheimer’s disease. Proc Natl Acad Sci U S A. 2008;105:14052–14057. | ||
van Oijen M, Hofman A, Soares HD, Koudstaal PJ, Breteler MM. Plasma Abeta (1–40) and Abeta (1–42) and the risk of dementia: a prospective case-cohort study. Lancet Neurol. 2006;5:655–660. | ||
Koyama A, Okereke OI, Yang T, Blacker D, Selkoe DJ, Grodstein F. Plasma amyloid-β as a predictor of dementia and cognitive decline: a systematic review and meta-analysis. Arch Neurol. 2012;69:824–831. | ||
Pomara N, Doraiswamy PM, Willoughby LM, et al. Elevation in plasma Abeta42 in geriatric depression: a pilot study. Neurochem Res. 2006; 31:341–349. | ||
Qiu WQ, Sun X, Selkoe DJ, et al. Depression is associated with low plasma Abeta42 independently of cardiovascular disease in the homebound elderly. Int J Geriatr Psychiatry. 2007;22:536–542. | ||
Blasko I, Kemmler G, Jungwirth S, et al. Plasma amyloid beta-42 independently predicts both late-onset depression and Alzheimer disease. Am J Geriatr Psychiatry. 2010;18:973–982. | ||
Direk N, Schrijvers EM, de Bruijn RF, et al. 2013. Plasma amyloid β, depression, and dementia in community-dwelling elderly. J Psychiatr Res. 2013;47:479–485. | ||
Kita Y, Baba H, Maeshima H, Nakano Y, Suzuki T, Arai H. Serum amyloid beta protein in young and elderly depression: a pilot study. Psychogeriatrics. 2009;9:180–185. | ||
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. | ||
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. | ||
Shima S, Shikano T, Kitamura T. [New self-rating scales for depression.] Clin Psychiatry. 1985;27:717–723. Japanese. | ||
Koyano W, Shibata H, Nakazato K, Haga H, Suyama Y. Measurement of competence: reliability and validity of the TMIG-index of competence. Arch Gerontol Geriatr. 1991;13:103–116. | ||
Ishizaki T, Watanabe S, Suzuki T, Shibata H, Haga H. Predictors for functional decline among nondisabled older Japanese living in a community during a 3-year follow-up. J Am Geriatr Soc. 2000;48:1424–1429. | ||
Saito Y, Sugawara N, Yasui-Furukori N, Takahashi I, Nakaji S, Kimura H. Cognitive function and number of teeth in a community-dwelling population in Japan. Ann Gen Psychiatry. 2013;12:20. | ||
Ikejima C, Hisanaga A, Meguro K, et al. Multicentre population-based dementia prevalence survey in Japan: a preliminary report. Psychogeriatrics. 2012;12:120–123. | ||
Moon YS, Kang SH, No HJ, et al. The correlation of plasma Aβ42 levels, depressive symptoms, and cognitive function in the Korean elderly. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1603–1606. | ||
Sun X, Mwamburi DM, Bungay K, et al. Depression, antidepressants, and plasma amyloid beta (Beta) peptides in those elderly who do not have cardiovascular disease. Biol Psychiatry. 2007;62:1413–1417. | ||
Sun X, Steffens DC, Au R, et al. Amyloid-associated depression: a prodromal depression of Alzheimer disease? Arch Gen Psychiatry. 2008;65:542–550. | ||
Sun X, Chiu CC, Liebson E, et al. Depression and plasma amyloid beta peptides in the elderly with and without the apolipoprotein E4 allele. Alzheimer Dis Assoc Disord. 2009;23:238–244. | ||
Metti AL, Cauley JA, Newman AB, et al. Plasma beta amyloid level and depression in older adults. J Gerontol A Biol Sci Med Sci. 2013; 68:74–79. | ||
Baba H, Nakano Y, Maeshima H, et al. Metabolism of amyloid-β protein may be affected in depression. J Clin Psychiatry. 2012;73:115–120. | ||
Iadecola C. Cerebrovascular effects of amyloid-beta peptides: mechanisms and implications for Alzheimer’s dementia. Cell Mol Neurobiol. 2003;23:681–689. | ||
Roy S, Rauk A. Alzheimer’s disease and the ‘ABSENT’ hypothesis: mechanism for amyloid beta endothelial and neuronal toxicity. Med Hypotheses. 2005;65:123–137. | ||
Alexopoulos GS. Role of executive function in late-life depression. J Clin Psychiatry. 2003;64:18–23. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.