Back to Journals » Clinical Ophthalmology » Volume 17
A Novel Procedure for Keratoconus/Corneal Ectasia Treating Epithelial Compensation of Higher-Order Aberrations, Topographic Guided Ablation, and Corneal Cross Linking – The CREATE+CXL Protocol
Authors Motwani M
Received 7 March 2023
Accepted for publication 22 June 2023
Published 13 July 2023 Volume 2023:17 Pages 1981—1992
DOI https://doi.org/10.2147/OPTH.S411472
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Manoj Motwani
Cornea Revolution/Motwani LASIK Institute, San Diego, CA, 92121, USA
Correspondence: Manoj Motwani, Cornea Revolution/Motwani LASIK Institute, 8710 Scranton Road, Ste 170, San Diego, CA, 92121, USA, Tel +1 858 554-0008, Email [email protected]
Purpose: To present the outcomes of a retrospective study in keratoconus/corneal ectasia patients of treating the higher order aberrations compensated for the corneal epithelium in addition to topographic guided ablation followed by corneal cross linking.
Methods: Twenty-seven eyes of 14 patients were treated for keratoconus/corneal ectasia utilizing trans-epithelial topographic guided ablation photorefractive keratectomy (PRK) for treatment of corneal higher order aberrations and lower order astigmatism followed immediately by 15-minute cross linking were examined retrospectively. Six-month results were analyzed via measurement of vision, refraction, residual higher-order aberrations (HOAs), residual lower-order and higher-order aberrations, as well as for loss or gains of lines of best corrected visual acuity.
Results: All eyes save one had reduction in K1, K2, K Max, and K Mean. All eyes had reduction in manifest astigmatism, Contoura measured astigmatism, 57% reduction of higher-order aberrations (HOA), and 53% reduction of higher-order aberrations grouped with lower-order aberrations (Grouped). Nearly all (96.3%) eyes achieved 20/40 vision or better, 20 eyes had 1– 7 lines gained of vision, and no eyes had any loss of lines of vision.
Conclusion: Use of the CREATE+CXL protocol combined with 15-minute corneal cross linking results in a significant increase in HOA reduction, as well as a significant improvement in corrected distance visual acuity over past procedures.
Keywords: astigmatism, corneal cross linking, higher-order aberrations, keratoconus, lower-order aberrations, photorefractive keratectomy, corneal ectasia
Introduction
Corneal ectasia is a degenerative condition that causes progressive corneal protrusion, irregular astigmatism, and thinning. Keratoconus is a type of corneal ectasia, and the most common one.1 Historically in the United States treatment has utilized contact lenses (soft/rigid gas permeable (RGP)/scleral), spectacles, Intacs corneal implants to attempt to modify the shape, and in severe cases corneal transplant.2 Corneal cross linking has been available in the United States since 2016 to prevent progression of the ectasia, but does little to improve vision. Contact lenses do not modify disease progression, and become more difficult to fit in severe disease. Intacs have been shown to be useful, but are a gross attempt to modify the corneal shape rather than a specific normalization of the cornea. Corneal transplants have their own issues from newly induced irregular astigmatism, to rejection, and corneal failure over time.3,4
The goal has been to find a permanent solution that would allow the highest degree of normalization of the original cornea while preventing further progression. For well over a decade, the Athens Protocol has been utilized to decrease corneal irregularity via topographic guided ablation (WaveLight Contoura, WaveLight Laser Technologie AG, Erlangen, Germany) and then perform corneal cross linking to stiffen the cornea and “freeze” it into place.5
In a prior publication, the author described the United States experience with this procedure, with modifications from new scientific understanding from the LYRA Protocol/San Diego Protocol to attempt to achieve a better visual outcome.6–9 One of the fundamental problems with normalizing the cornea is that the topography system cannot measure corneal stromal irregularity that has been compensated for by changes in corneal epithelial thickness. This compensation has been described as significant (20–30 µm) in publications by Reinstein et al, Kanellopoulos et al, as well this author.10–15
Over the past several years commercial technology such as anterior segment optical coherence tomography has been available to map this epithelial compensation, but there is no existing technology that combines the topographic analysis with the epithelial compensation to create a map of the full irregularity.
As such a device is unavailable, the authors used PTK (Phototherapeutic Keratectomy) to the depth of epithelial compensation provided by an Visionix/Optovue epithelial thickness mapping (ETM) device. This would ablate corneal stromal tissue compensated for by the corneal epithelium as corneal stroma and epithelium ablate similarly for each excimer laser pulse. This trans-epithelial PRK utilizing topographic guided ablation (WaveLight Contoura) was termed the CREATE Protocol, Corneal Repair Epithelium and Topography Enhanced, and when used in conjunction with corneal cross linking for corneal ectasia is termed the CREATE+CXL Protocol.
Another major change from our prior publication has been the use of mitomycin-C. In Feb 2021, a publication demonstrated deep scarring and haze from the use of mitomycin-C with corneal cross linking.16 Since that time, we have eliminated the usage of mitomycin-C with CREATE+CXL procedures, and all patients in this manuscript’s series have not had mitomycin-c exposure.
As stated in our prior publication,9 the goals of the procedure, in order of importance, are:
- Stop progression of keratoconus and strengthen the cornea to avoid cornea transplant.
- Normalize the cornea by decreasing the irregularity of the anterior cornea improving the optics of the cornea, as well as increasing the ability of further refractive correction via spectacles, soft contact lenses, and RGP/scleral lenses.
- In cases where sufficient tissue is available, also correct the sphere and cylinder to get as close to plano correction as possible.
Materials and Methods
We retrospectively examined patients who had keratoconus/corneal ectasia treatment the CREATE+CXL Protocol, and also had at least 6 months of follow-up results. As many of our patients come from out of town, we do not have full long-term results on many of our treatments, therefore we included all eyes in this study where at least 6-month results were obtained at our clinic. We were able to analyze data from 27 eyes of 14 patients.
Results were tabulated for pre- and post-operative vision, average K and Kmax, and manifest cylinder. Pre-op Contoura (topography utilizing the Topolyzer Vario (WaveLight, Erlangen, Germany)) measured astigmatism was also averaged. Pre- and post-operative corrected distance visual acuity (CDVA) was tabulated, as were lines of vision gained or lost.
Measurements up to 6th order Zernike polynomials to measure higher order aberrations (HOA) were tabulated, as were what we defined as Grouped. These are HOA plus lower order sphere and astigmatism, excluding piston and tilt. The first number was measured to demonstrate corneal irregularity reduction, the second to include lower order aberration reduction.
Epithelial compensation was measured utilizing the Visionix/Optovue (Visionix/Optovue, Fremont, CA) epithelial mapping system on their OCT devices (Solix and Avanti), by measuring epithelial thickness of the thinnest and thickest areas in the central 5 mm of the cornea. The difference between these two numbers was the epithelial compensation for the corneal irregularity.
Epithelium removal was performed utilizing either the PTK mode the Nidek EC-5000, or the WaveLight WFO myopic treatment to the depth of corneal epithelium removal determined by Optovue OCT mapping. This is due to the fact that there is no PTK mode available on WaveLight lasers in the United States. Residual epithelial removal was accomplished to a width of 9 mm via manual removal by cellulose sponge or corneal epithelial scraper. WaveLight Contoura was then used to treat the corneal higher-order aberrations and irregular astigmatism measurable by topography of the anterior cornea.13 Surgical planning utilized the measured astigmatism up to the maximum 3 diopters (D) allowed in the Contoura FDA approval. Most patients had no sphere treated due to tissue constraints. In milder keratoconus cases where the cone was not in the central visual axis spherical treatment was performed to a maximum of 70% of the manifest sphere after any adjustment for the spherical equivalent of astigmatism difference between manifest and measured astigmatism. Treatment parameters were designed to leave a corneal bed of 350 µm to maintain safety parameters for corneal cross linking. If the residual corneal bed after laser ablation was less than 350 µm (in this study between 320–350 µm) hypotonic saline was used to increase the thickness of the cornea to over 400 µm before cross-linking was performed. Measured astigmatism axis was always used for the topography guided ablation.
It is notable that in many patients the highest amount of corneal tissue removal during topographic guided ablation was often not centrally, but in the superior periphery to normalize the superior flat area. It was essential during surgical planning to only use the central tissue removal depth, and not the overall ablation depth during calculations to leave a corneal bed of 350 µm to ensure safe corneal cross linking. We calculated this utilizing pachymetry from scheimpflug imaging, OCT pachymetry, OCT epithelial thickness maps, as well as the optical pachymetry on the WaveLight EX500.
The amount of treatment was limited only by available tissue and the limit of 3 diopters of astigmatism treatment with WaveLight Contoura. No other excimer treatment was performed except for epithelial removal and the sole topographic guided ablation treatment.
Corneal saturation with riboflavin was performed immediately after laser treatment for 2 minutes. As corneal cross linking (CXL) treatment was performed on the right eye first as a rule, the left eye would be re-saturated for another minute before UV treatment.
An “off-label” 15-minute cross-linking procedure using a 10-mm spot size, homogenous UV light beam, with 6 mW/cm2 (ie a total UV light dose of 5.4 J/cm2), was performed. The riboflavin formulation used was 0.1% riboflavin w/Carboxymethyl Cellulose pH Balance (no dextran).
All LASIK procedures were performed on the WaveLight EX500 excimer laser. All procedures were performed by one surgeon (MM) at one center in San Diego, California. All topographies were obtained utilizing the Topolyzer Vario (Alcon Surgical, Fort Worth, TX, USA). All epithelial thickness maps (ETM) were obtained with the Optovue Avanti or Solix devices (9-mm ETM) (Optovue, Fremont, CA, USA).
Post-operative care consisted of fluorometholone 0.1% bid for 6 weeks, ofloxacin 0.3% qid x 1 week, and Prolensa qd as needed for pain during epithelial healing. Bandage contact lenses were removed with healing of the corneal abrasion which was between 4–5 days on average. As mentioned in the discussion, no Mitomycin-C was applied to any patients in this study.
All patients signed written informed consent forms allowing their data to be used in this study and published including sample cases 1–4. This study falls under the exemption of the Health and Human Services (HHS) Policy for the Protection of Human Research Subjects 45 CFR 46.104 (d) for retrospective studies and 46.104 for exempt research, and thus, no Institutional Review Board approval was required. This study also conforms to the Declaration of Helsinki guidelines. There were no safety-related incidents that occurred or were reported to Alcon Inc. or WaveLight concerning patients involved in this study.
Results
Twenty seven (27) eyes of 14 patients are included in this study, 7 men and 7 women. The average patient age was 31.85 years, range 18–50 years. 25 eyes had keratoconus, and 2 post-LASIK ectasia. All results come from eyes that had at least 6 months of post-operative follow-up.
Table 1 shows pre-op and post-op values for average K and Kmax, pre-op measured and manifest cylinder, and post-op manifest cylinder. Average post-op average K and Kmax all decreased, as did the post-operative manifest refraction. Pre-op average Contoura measured astigmatism was higher than the pre-op average manifest astigmatism.
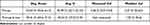 |
Table 1 Pre-Op and Post-Op Values for Average K and Kmax, Pre-Op Measured and Manifest Cylinder, and Post-Op Manifest Cylinder |
Table 2 presents the best corrected visual acuities pre-op and post-op by Snellen chart measurements, as well as the percentages of eyes in that category. It is notable that 96.3% of eyes were able to see 20/40 or better postoperatively, while only 70.35% could achieve 20/40 pre-op.
 |
Table 2 Best Corrected Visual Acuities Pre-Op and Post-Op by Snellen Chart Measurements |
Table 3 shows the lines of BCVA gained. 74% of eyes gained between 1–7 lines of vision, while the remaining 26% neither gained nor lost lines of vision. Notably no eyes lost any lines of BCVA.
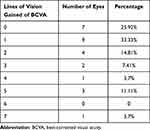 |
Table 3 Gains in Best Corrected Visual Acuity |
In Table 4 Zernike polynomials are presented for 6th order higher-order aberrations (HOA), and for Grouped polynomials which includes HOA and lower-order sphere and astigmatism (does not include tilt or constant height/piston). The average HOA were reduced by 57.3% and the Grouped values were reduced by 52.8%. This compares favorably with our prior corneal ectasia treatment study that did not treat epithelial compensation which had an average reduction of 31.8% for HOA and 25.5% for the Grouped values. Statistical testing with two tailed t-test for pre-and post-op HOA and Grouped values were statistically significant with P < 0.05, as was the difference in reduction values between our prior study and this study.
 |
Table 4 Zernike Polynomials for 6th Order Higher-Order Aberrations and for Grouped Polynomials |
Table 5 shows the average amount of epithelial compensation of the stroma. This was determined for the entire cohort to be 18.9 µm, or 24% of the overall aberration treatment depth of 78 µm. The average number was calculated utilizing the depth of ablation treatment determined by WaveLight Contoura utilizing the 6mm treatment zone. This was limited by the maximum 3 diopters of astigmatism correction, as 15 out of the 27 eyes had measured astigmatism greater than 3 diopters. As treating lower-order aberrations (LOA) in combination with HOA creates a unique topography guided ablation pattern (in many cases treating the astigmatism does not increase the overall HOA reduction tissue removal as much as performing the astigmatism correction separately), it was not possible in these eyes to determine the total amount of aberration that topography system was measuring. In 12 eyes the measured astigmatism was below 3 diopters, and in these eyes the average epithelial compensation was 19.6 µm, or 28% of the total aberration of 69.2 µm. When statistical testing with two tailed t-test was performed comparing the two, it was not statistically significant with a P > 0.05.
 |
Table 5 Average Amount of Epithelial Compensation of the Stroma |
All eyes had minimal haze, trace to 1+, that was easily controlled and reduced with steroid treatment via either fluorometholone 0.1% or combined with a short burst of prednisolone 0.1%. It was noted through the entire patient group that haze was significantly less of a factor than when mitomycin-C was used.
Two tailed t-tests were performed to look for statistical significance. Comparisons of pre-op to post op HOA values and HOA values were statistically significant, with P less than 0.05. This test was also performed comparing pre-op HOA and grouped values to the three different sub groups.
Sample Cases
Case 1: 49 year old male (Figure 1A–E).
CASE 2: 32 year old male (Figure 2A–E).
CASE 3: 20 year old female (Figure 3A–E).
Discussion
The amount of irregularity removed during corneal laser normalization increased significantly with use of the CREATE+CXL protocol in comparison to our prior publication results, from 31.87% for HOA and 25.5% for the Grouped values, to 57.3% HOA and 52.8% Grouped. This increase in the reduction of corneal irregularity was reflected in the increase in quantity of vision as well as significant improvements in the topographic shape of the corneas. Corresponding with that reduction in irregularity, 96.3% of eyes had post-operative vision of 20/40 or better (all but 2 eyes), and 74% eyes gained 1–7 lines of best corrected visual acuity (BCVA). The other 26% of eyes did not lose or gain lines of BCVA. No eyes lost lines of BCVA.
It is important to note here that epithelial compensation of stromal irregularity can be seen with epithelial mapping devices such as the Optovue OCT machines, but cannot be measured by the Vario Topolyzer/WaveLight Contoura platforms, or for that matter any topography or wavefront measurement system. In other words, Contoura measures the topographic shape after epithelial compensation, and once that irregularity is removed the epithelium re-compensates to the smaller but not completely removed irregularity exposing residual irregularity. The only commercial epithelial thickness mapping device to measure epithelial compensation available in the United States are the Optovue OCT epithelial mapping devices, and as of yet no device exists to combine epithelial compensated HOA with topographic measured HOA. Disclaimer, such a device is described in United States patent no. 10857033 granted to the author in December 2020 but as of this writing has not yet been built. Furthermore, the author knows of no current device, software algorithm such as the Phorcides Analytic Engine, or any upcoming device that measures and includes epithelial compensation of stroma in its topographic guided laser ablation algorithm.
The significantly increased reduction in HOA, combined with visual results and visual reduction of topographic abnormality as displayed in the case examples, make a strong case for including epithelial compensation as part of any algorithm to decrease corneal irregularity. It is notable that in a prior publication in 2019, the authors found that epithelial compensation negatively affected the accuracy of outcomes even in primary LASIK corrections utilizing topographic guided ablation and the LYRA Protocol.15
The outcomes in this study confirm that omitting Mitomycin-C in topographic guided ablation and cross-linking procedures actually produces significantly less haze. Haze has ceased to be an issue in our patients, with at most some +1 superficial corneal haze noticed on some patients that was easily treatable with steroid treatment. Notably, this lack of deep haze was part of the reason no eyes lost BCVA, along with the increased HOA reduction. The decrease in haze also allowed for a decrease in strength and frequency in the post-operative steroid regimen, which decreased post-operative epithelial healing time and aberrant healing issues.
This increased reduction of HOA also seemed to lead to a faster visual rehabilitation time for patients. Many patients were achieving good, functional vision within 7–10 days post-operatively allowing for more rapid return to work and driving.
Corneal cross linking was always performed after laser correction, and thus was always “epithelial off”. This has a deeper corneal penetration and depth of corneal stiffening than “epithelial on”. Past studies have shown that the depth of epithelial off cross linking is approximately double that of epithelial on,17,18 and it is our practice never to do epithelial on cross-linking on any patient due to the limited depth of structural strengthening.
Reduction of average K, Kmax, and manifest astigmatism were all useful measures, but reduction of K is skewed by the large differences of K due to corneal irregularity, and reduction of manifest astigmatism is skewed by the limitation of WaveLight Contoura to treating astigmatism only up to 3 diopters as well as by the amount of tissue available for laser ablation. We believe that the most important measurements are the reduction of HOA and increase in BCVA, and secondarily the vision outcomes.
It is reasonable to question why the amount of HOA reduction was not even greater in some patients, and we believe at this time the limitation is due to the maximum of 3 diopters of astigmatism treatable with Contoura. As we have shown in the original LYRA Protocol publications, the WaveLight Contoura laser ablation pattern for HOA and astigmatism correction corresponded closely with the anterior elevation irregularity as measured on scheimpflug devices. If the full amount of the measured astigmatism is not treated, the full amount of anterior elevation is not corrected, thereby leaving residual higher order aberration. In keratoconus patients, the main limiting factor is the tissue availability to ensure a 350 µm bed for corneal cross-linking, but in some eyes the limiting factor was the 3 diopter astigmatism treatment limit.
Another limiting factor in treatment was the arbitrary limitation of Contoura treatment to 6.0 mm and 6.5 mm treatment zones as utilizing a 5.0 mm treatment zone would allow for greater irregularity reduction. It has long been confusing to us why treatment zones not included in the FDA approval, nor why they are not available to the surgeon with a precaution as is allowed for Wavefront Optimized corrections.
Case 1 shows the treatment of a 49 y.o. male with keratoconus, more severe on the right eye which was chosen for this example (Figure 1A–E). Such a patient typically has keratoconus progress in their teens and 20’s, but stabilizes as they age. This patient had significant issues with scleral lens fit and complained of compromised vision even though the patient could achieve 20/30 BCVA. This patient had a 48.7% reduction in HOA, with a resultant 1 line improvement in BCVA to 20/25 (Figure 1E). Treatment included no spherical correction, but normalization of the cornea resulted in significant reduction in sphere by flattening the cone in the visual axis area. The resulting small amount of manifest astigmatism correlates with the small amount of cylinder left untreated due to the limits of Contoura of 3 diopters of cylinder treatment. The patient anecdotally reported increased vision and dramatically increased quality of vision which he described as the best since he was a teenager.
Case 2 is a 32 year old male that had bilateral LASIK performed in 2012 (Figure 2A–E). After being diagnosed with lasik induced corneal ectasia in the right eye, he traveled to a surgeon experienced with Intacs for Keratoconus, and underwent Intacs placement with epithelial-on crosslinking in 2019 of his right eye. This procedure had a suboptimal visual outcome, so the patient had the Intacs removed several months later. He then had a surgeon perform refractive wavefront PRK with a VISX laser removing approximately 70 µm of tissue. Incidentally, since epithelial on cross-linking only strengthens the approximately 125 µm of the anterior cornea, a large portion of the strengthened tissue was removed by this procedure. The patient noted progressive worsening of his vision after this procedure, and presented to us with the LASIK induced ectasia in Figure 2 with multiple scars from the prior procedures. This patient had one of the largest amounts of epithelial compensation at 40 µm, but treatment demonstrates a cornea with a significant reduction of the irregularity on topography which correlates with the 64% reduction in HOA. The patient was limited in his post-operative BCVA by severe dry eye that was likely caused by the multiple procedures he had undergone. This was in the process of relatively successful treatment as of their last visit.
The topographic outcome demonstrates a cornea that has had the majority of the cone normalized, which corresponds to the 65% reduction of HOA. The patient had epithelial off cross-linking performed subsequent to the transepithelial topography guided ablation, which would allow for the maximum depth of cross-linking. No progression has been noted since this procedure, and the patient anecdotally reports the best vision he has had since the ectasia was diagnosed.
Case 3 is the classic young person with progressive keratoconus, a 20 year old female with bilateral disease and the case example is of the more severely affected of the two eyes (Figure 3A–E). Of interest is her younger brother also had progressive severe keratoconus, highlighting the genetic nature of this disease. This patient had a significant reduction of her cone on topography while having only a 37% reduction of HOA, a low number for this study, but yet had a dramatic improvement of her BCVA from 20/70 to 20/25 (Figure 3E). This correlates with what we observed in our earlier study, that HOA reduction does not correlate directly with BCVA improvement.9 It may well be that the cornea in the central visual axis greater improvement than the overall HOA reduction number, thus the significant improvement in vision. The right eye (OU) vision result was 20/20, allowing this young lady to have the vision to resume her education.
No patient required or desired scleral lens fitting post-op. Some did wear glasses to correct post-operative refraction, but most chose to wear these glasses occasionally rather than regularly. This corresponds with the HOA reduction, as patient’s quality of vision would improve to where the LOA was the more prominent issue, so spectacles could correct the patient satisfactorily.
Some patients did have slow epithelial healing issues. As haze became significantly less of an issue by terminating use of the mitomycin-C, steroid was used in lesser strengths and lower dosing which helped improved epithelial healing response. Slow healing epithelium responded well to temporary halting of the steroid, lubrication, and bandage lens replacement. Haze was not a significant problem in these patients even the steroid use was suspended. The enrollment of patients in this retrospective study was limited by the number of out-of-town patients, as comprehensive follow-up to obtain the requisite data was not available for many patients. Only limited visual and anecdotal data as reported by patients and their local ophthalmologists was available, and seemed to match the data measured in our center. We currently have no evidence or report of negative outcomes such as BCVA loss, significant haze, or other serious issues related to these procedures save one patient that ended up with a severe corneal ulcer during travel back home after the epithelial abrasion had already closed and bandage lens removed. Since we did not have the follow up information for this patient, we did not include them in this study.
Keratoconus/corneal ectasia affects a small, but significant percentage of the population, but the potential visual debilitation can have a massive impact on the patient’s life, their career, and even their social interactions. Many patients report the inability to maintain a job, go to school, or drive. The goal for these patients is a permanent treatment that allows them to keep their own cornea but with significant visual rehabilitation, and the prevention of progression of the disease. The long desired ultimate goal for these patients is also to rehabilitate their vision to the point where they can lead “normal” lives with good vision that does not interfere with their lives or chosen careers. The results of the CREATE+CXL Protocol indicate that we are close to achieving this long desired goal. We realize this is a relatively small sample, but the overall results have been consistently good even with patients we do not have a full complement of data to include in this manuscript. We plan to continue to accumulate data and analyze a larger group of patients in a future manuscript.
Abbreviations
BCVA, best-corrected visual acuity; CXL, Corneal cross linking; D, diopters; ETM, epithelial thickness maps; FDA, Food and Drug Administration; HHS, Health and Human Services; HOAs, higher-order aberrations; MMC, mitomycin C; OD, right eye; OS, left eye; PRK, photorefractive keratectomy; qd, daily; qid, four times daily; RGP, rigid gas permeable; UCVA, uncorrected visual acuity; US, United States.
Acknowledgments
The author would like to thank Julie Crider, PhD for editing contributions, and Gerardo Lozano and Charlene Lloyd for data collection and editing contributions.
Disclosure
The author has been granted United States patent no. 10857032 concerning the creating of a more uniform cornea utilizing the topography measured astigmatism, and United States patent no. 10857033 for the treatment of epithelial compensation of corneal irregularity in conjunction with the use of topography guided ablation system. The author reports no other conflicts of interest in this work.
References
1. Sorkin N, Varssano D. Corneal collagen crosslinking: a systematic review. Ophthalmologica. 2014;232(1):10–27. doi:10.1159/000357979
2. Boyd K. Keratoconus diagnosis and treatment. American Academy of Ophthalmology; 2020. Available from: https://www.aao.org/eye-health/diseases/keratoconus-diagnosis.
3. Gomez-Benlloch A, Montesel A, Pareja-Arico L, et al. Causes of corneal transplant failure: a multicentric study. Acta Ophthalmol. 2021;99(6):e922–e928. doi:10.1111/aos.14708
4. Lains I, Rosa AM, Guerra M, et al. Irregular astigmatism after corneal transplantation--efficacy and safety of topography-guided treatment. Cornea. 2016;35(1):30–36. doi:10.1097/ICO.0000000000000647
5. Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the Athens protocol. J Refract Surg. 2011;27(5):323–331. doi:10.3928/1081597X-20101105-01
6. Motwani M. The use of WaveLight® Contoura to create a uniform cornea: the LYRA Protocol. Part 3: the results of 50 treated eyes. Clin Ophthalmol. 2017;11:915–921. doi:10.2147/OPTH.S133841
7. Motwani M. The use of WaveLight® Contoura to create a uniform cornea: the LYRA Protocol. Part 2: the consequences of treating astigmatism on an incorrect axis via excimer laser. Clin Ophthalmol. 2017;11:907–913. doi:10.2147/OPTH.S133840
8. Motwani M. The use of WaveLight® Contoura to create a uniform cornea: the LYRA Protocol. Part 1: the effect of higher-order corneal aberrations on refractive astigmatism. Clin Ophthalmol. 2017;11:897–905. doi:10.2147/OPTH.S133839
9. Motwani M. Treatment of keratoconus with WaveLight Contoura and corneal cross-linking combined. Clin Ophthalmol. 2021;15:2455–2472. doi:10.2147/OPTH.S303559
10. Reinstein DZ, Archer TJ, Gobbe M. Refractive and topographic errors in topography-guided ablation produced by epithelial compensation predicted by 3D Artemis VHF digital ultrasound stromal and epithelial thickness mapping. J Refract Surg. 2012;28(9):657–663. doi:10.3928/1081597X-20120815-02
11. Kanellopoulos AJ, Asimellis G. Novel Placido-derived topography-guided excimer corneal Normalization With cyclorotation adjustment: enhanced Athens protocol for keratoconus. J Refract Surg. 2015;31(11):768–773. doi:10.3928/1081597X-20151021-06
12. Reinstein DZ, Archer TJ, Vida RS. Epithelial thickness mapping for corneal refractive surgery. Curr Opin Ophthalmol. 2022;33(4):258–268. doi:10.1097/ICU.0000000000000867
13. Motwani M. A protocol for topographic-guided corneal repair utilizing the US Food and Drug Administration-approved Wavelight Contoura. Clin Ophthalmol. 2017;11:573–581. doi:10.2147/OPTH.S127855
14. Motwani M. Epithelial Compensation of Corneal Higher-Order Aberrations and Its Effect on Topographic Guided LASIK Outcomes as Demonstrated by OCT Epithelial Thickness Mapping. ASCRS; 2020.
15. Motwani M. Analysis and causation of all inaccurate outcomes after WaveLight Contoura LASIK with LYRA protocol. Clin Ophthalmol. 2020;14:3841–3854. doi:10.2147/OPTH.S267091
16. Awwad ST, Chacra LM, Helwe C, et al. Mitomycin C application after corneal cross-linking for keratoconus increases stromal haze. J Refract Surg. 2021;37(2):83–90. doi:10.3928/1081597X-20201124-01
17. Yuksel E, Cubuk MO, Yalcin NG. Accelerated epithelium-on or accelerated epithelium-off corneal collagen cross-linking: contralateral comparison study. Taiwan J Ophthalmol. 2020;10(1):37–44. doi:10.4103/tjo.tjo_11_19
18. Mazzotta C, Ramovecchi V. Customized epithelial debridement for thin ectatic corneas undergoing corneal cross-linking: epithelial island cross-linking technique. Clin Ophthalmol. 2014;8:1337–1343. doi:10.2147/OPTH.S66372
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



