Back to Journals » Clinical Ophthalmology » Volume 16
A Novel Biomarker in Primary Glaucoma: Aqueous Humor and Serum Levels of Ischemia Modified Albumin (IMA)
Authors Rusmayani E, Artini W, Sasongko MB , Suhardjo, Viona V
Received 28 September 2022
Accepted for publication 5 December 2022
Published 10 December 2022 Volume 2022:16 Pages 4075—4087
DOI https://doi.org/10.2147/OPTH.S388382
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Emma Rusmayani,1 Widya Artini,1 Muhammad Bayu Sasongko,2 Suhardjo,2 Viona Viona1
1Glaucoma Department, Jakarta Eye Center Hospitals and Clinics, Jakarta, Indonesia; 2Ophthalmology Department, Faculty of Medicine University Gadjah Mada, Yogyakarta, Indonesia
Correspondence: Emma Rusmayani, Glaucoma Department, Jakarta Eye Center Hospitals and Clinics, Terusan Arjuna Utara / 1 Kedoya, West Jakarta, Jakarta, Indonesia, 11520, Email [email protected]
Purpose: To analyze ischemia-modified albumin (IMA) levels in aqueous humor and serum, and their correlation to RNFL thinning in primary glaucoma patients.
Design: Cross-sectional study.
Methods: Patients were divided into the control and glaucoma groups. The control group was patients with senile cataracts. The glaucoma group consisted of patients diagnosed for the first time as primary open-angle glaucoma (POAG) or primary angle closure glaucoma (PACG). Exclusion criteria were secondary glaucoma and patients with systemic disease. A complete cataract examination was done for all patients, and glaucoma examinations for the glaucoma group. In both groups, the IMA aqueous humor was obtained during cataract and glaucoma procedure. Serum levels of IMA, malondialdehyde (MDA), and tumor necrosis factor alpha (TNF-α) were examined during preoperative examinations.
Results: Control group comprised 33 participants, and glaucoma group 41 patients (21 PACG and 20 POAG). Mean IMA aqueous humor (AQH) levels found in cataract group 6.039± 3.16 ng/mL, glaucoma group 14.89± 6.08 ng/mL, PACG group 12.69± 6.25 ng/mL and POAG group 17.33± 4.988 mg/mL. Mean IMA serum levels in cataract group 14.75± 6.53 ng/mL, glaucoma group 13.89± 6.53 ng/mL, PACG group 12.79± 6.46 ng/mL± and POAG group 14.93± 10.74 ng/mL. Glaucoma group had significant higher level of IMA in aqueous humor compared to control group, but opposite findings in serum IMA levels between groups. POAG patients had a higher aqueous IMA level compared to PACG group and correlated significantly with IOP. IMA AQH also negatively correlated to the RNFL thickness in both POAG and PACG group. Cut off 9.5 ng/mL was considered as a normal limit value to differentiate between control and glaucoma group.
Conclusion: Primary glaucoma patients showed a significantly increased level of IMA AQH as a local ischemic biomarker compared to the control group. Systemic oxidative activity is not a representation of local ocular oxidative stress in both cataract and glaucoma group.
Keywords: ischemia-modified albumin, biomarker, primary glaucoma, early detection
Introduction
Glaucoma is a worldwide health-care problem of irreversible blindness. Glaucoma consists of neurodegenerative disorders marked by chronic progressive degeneration and apoptosis of anatomical structure resulting in marked visual field defect.1 Glaucoma prevalence worldwide is approximately 50 million people, with 3.5% diagnosed at 40 to 80 years old.2 Glaucoma patients estimated will increase to 112 million by 2040.3 The increase of intraocular pressure (IOP) is one of the risk factors, which is also the only factor that able to be controlled by medications or surgery. Therefore, the target of glaucoma treatments is to lower the IOP to delay the disease progression. High IOP is the result of aqueous humor (AQH) build-up. Aqueous humor is produced by the ciliary epithelium, which flows to the anterior chamber and then circulates to the trabecular meshwork, Schlemm’s canal, and the venous system. Increased resistance of aqueous outflow results in elevated IOP and leads to an ischemic process in the optic nerve head.4,5
Pathogenesis of glaucoma also associated with oxidative stress process. Moreover, vasoconstriction of vessels as the result of peroxynitrite (ONOO-) is also causing the reduction optic nerve blood flow, which further resulting in RGC death.6,7 Oxidative stress also leads to increase endothelin-1, responsible to vasoconstriction of vessels and reduction of the optic nerve blood flow, resulting in RGC death. Neuronal transport in the optic nerve head is also disrupted by increasing activation of endothelin. Therefore, ischemia, apoptosis of RGC and further damage in glaucoma.8
Early diagnosis, prompt treatment, and progression monitoring in glaucoma have been challenging. Patient evaluation needs to be thorough with the complete clinical examination, IOP measurements, structural, and functional imaging modalities. Screening examination based only on IOP measurements is no longer considered precise, especially in early stage patients with normal IOP range. In addition, observation through cup-to-disc ratio at some point considered not sensitive and specific enough for predicting glaucoma.9 In addition, it is not uncommon that patient with glaucoma diagnosed with 35–40% loss of RGC.10
Therefore, it is imperative to establish a novel diagnostic testing for early diagnosis of patients with glaucoma or risk for developing glaucoma. A novel parameter for early diagnosis, monitoring treatment response, and disease progression may contribute to improve disease prognosis in glaucoma. Molecular biomarkers are now thought to be able to diagnose glaucoma in its early stages or patients with high-risk developing glaucoma, also in glaucoma treatments.
Oxidation induces albumin structure modifications. The binding of the oxidative stress to one of the albumin’s chains causes the formation of IMA, which is considered a novel biomarker of ischemia-related events and oxidative stress.11–13 IMA levels were higher in serum and aqueous humor in diabetic retinopathy (DR).14,15 The changes in glaucoma progression have been considered able to depict by systemic antioxidant levels, and oxidative stress biomarkers. The definite pathways in glaucoma regulated by reactive oxygen species (ROS) are still debatable. The correlation between IMA levels and systemic oxidative stress state is not yet determined, which ROS is one of the risk factors for glaucoma pathogenesis.16 Oxidative stress biomarkers in glaucoma pathogenesis have been previously studied, but no study has analyzed the role of IMA levels in human aqueous humor.17
This study aims to analyze IMA levels in the serum and aqueous humor as an early diagnostic parameter and their correlation to RNFL thinning in primary glaucoma.
Participants and Methods
This cross-sectional study participants were patients who came to the Jakarta Eye Center Ophthalmology Clinic Cibubur from January 2021 to June 2021. Ethical clearance was issued by the Ethics Committee Faculty of Medicine Gadjah Mada University. Patients were given complete and thorough information regarding the procedures of the study, the indications, risks, and benefits of the surgery, then provided with written consent. All procedures and protocols were under the Declaration of Helsinki. Subjects divided to control and glaucoma group. The POAG and PACG (study) group comprised patients with primary glaucoma, and cataract (control) group comprised patients with senile cataract, age and sex matched. Exclusions criteria of this study were participants with history of systemic diseases such as hypertension, diabetes mellitus, hyperuricemia, cardiac, thyroid diseases (hyper or hypothyroid), lung inflammation (TBC), autoimmune diseases, smokers, and alcoholics. Patients with secondary glaucoma due to diabetes, trauma, and steroids induced, pseudoexfoliation were also excluded. Exclusion criteria included patients with a history of regular eyedrop usage in the past month, a history of uveitis, and history of intraocular surgeries.
A thorough and related medical history and ophthalmologic examinations (visual acuity, applanation, slit lamp and fundus examinations) were done. Glaucoma examinations were done to assess the structural (OCT) and functional defects (HFA). Glaucoma severity was classified as early, moderate and advance based on mean deviation value. IOP lowering medications were given to all glaucoma groups as preoperative preparation. IOP was evaluated within 7–10 days and then aqueous humor sample was taken intraoperatively.
Blood samples were collected in both groups as part of the preoperative examination. Aqueous humor samples (0.1–0.3 cc) by paracentesis were collected in both groups before the cataract surgery or trabeculectomy. Both serum and aqueous humor samples were centrifuged at 2500 rpm and 10,000 rpm before being stored at 8°C. Then, they were analyzed for IMA (both aqueous and serum), MDA, and TNF-α (serum only). IMA was analyzed using an IMA ELISA kit with an autoanalyzer (LS Bio Human Ischemia Modified Albumin Elisa Kit LS-F27035, Seattle, USA). TNF-α was analyzed using a human TNF-α assay (Quantikine® HSTA00E, R&D system, Minneapolis, USA). Malondialdehyde (MDA) was analyzed using MDA ELISA kit (abx257171, R&D system, Minneapolis, USA).
Statistical Analysis
Statistical analysis was done with SPSS 23.0 (IBM Corp, NY, USA) and Microsoft Office Excel 2021 (Microsoft, Washington, USA). Normality test was performed using Kolmogorov-Smirnov, parameters were analyzed using t-test or Mann–Whitney depends on the distribution, and linear regression.
Results
The study subjects were 74 people, 33 people were in the control group and 41 people were glaucoma patients. The mean age and sex of the study subjects did not show any statistically significant differences between groups (Table 1). The clinical characteristics of the study subjects consisted of baseline intraocular pressure (IOP), preoperative IOP, retinal nerve fiber layer (RNFL), and mean deviation (MD) visual field.
 |
Table 1 Baseline Characteristics of Study Participants |
The measurement results of IMA AQH levels were quantified through aqueous humor samples between glaucoma and cataract patients. Serum IMA levels were also analyzed as a noninvasive systemic comparison. IMA AQH levels were statistically higher in glaucoma groups compared to control group (p < 0.005) (Table 2). The highest IMA AQH level was found in the POAG group with an average of 17.33 ± 4.988 ng/mL. There was no statistically significant difference between the PACG and POAG groups. In contrast to IMA AQH levels, IMA serum levels showed no statistically significant difference between groups. The highest mean serum IMA level was found in the POAG group, but not statistically significantly different compared to the PACG and control groups. This result was similar to the IMA AQH levels in the POAG group which were the highest among groups. The correlation found between IMA AQH levels and lowered IOP in POAG describes a state of chronic oxidative stress (Figure 1).
 |
Table 2 IMA Levels of Study Participants |
This study evaluated IMA levels as a biological marker of early diagnostic parameter in comparison to RNFL thinning that occurs early in the course of glaucoma (Table 3). IMA AQH levels were not correlated with RNFL thickness in the control group (Figure 2). RNFL thickness in the control group was still within normal limits (>80 μm), with a wide range of IMA AQH levels (2.10 ng/mL–15.20 ng/mL). This may be due to the variety lens sclerosis and types of cataracts.
 |
Table 3 Univariate Analysis of IMA AQH Levels and RNFL Thinning |
The relationship between IMA AQH levels and RNFL thinning was assumed that local ischemic events could describe glaucoma progression. IMA AQH levels were found to be correlated to RNFL thinning in all glaucoma groups. POAG subjects in this study demonstrated mostly moderate to advanced glaucoma, in contrast with PACG groups with more various stages (Figure 3). RNFL thickness at 90 microns was considered as a y-axis cutoff point for early diagnosis of glaucoma (Figure 4). Cut-off of IMA AQH levels (x-axis) to differentiate glaucoma and non-glaucoma groups was found at 9.8 ng/mL (Table 4). Based on Figure 4, with y-axis s and x-axis cutoff points, only PACG and POAG patients were placed in the area. IMA AQH levels of both glaucoma groups were found to have an important role in RNFL thinning (Table 5). On the contrary, IOP was found to be significant in RNFL thinning only in POAG group.
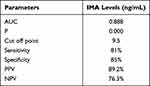 |
Table 4 AUC Cutoff Point of IMA AQH Levels |
 |
Table 5 Univariate and Multivariate Analysis of IOP and IMA AQH Levels to RNFL in PACG and POAG Groups |
IMA serum was analyzed as biomarker in comparison to aqueous humor samples (Table 6). Serum TNF-α and MDA levels were also evaluated as systemic comparative biomarker of glaucoma pathogenesis. There was no significant correlation between all systemic biomarkers (IMA, TNF-α and MDA) to RNFL thinning in glaucoma.
 |
Table 6 Univariate and Multivariate Analysis of IMA, TNF-α and MDA Serum Levels to RNFL in Glaucoma, PACG and POAG Groups |
Discussion
This study aims to analyze IMA levels as a biomarker and parameter for early detection of glaucoma. The correlation between IMA AQH, IMA, TNF-α, MDA serum levels, and RNFL thinning was analyzed in primary glaucoma patients compared to the control group.
The mean age in the control group was 64 years and the glaucoma group was 65 years. Lens opacity caused by protein changes in the lens begins at the age of 40 years. The process of aging results in the accumulation of epithelial cells and changes in the structure of the lens nucleus protein to be modified and cross-linked. In addition to the altered structure, the lens’ defense against oxidative stress also diminishes, which causes the accumulation of free radicals.12 The accumulation of free radicals can be illustrated by the increase in levels of IMA AQH in the control group of this study. These findings support the previous research that shows IMA AQH levels were increased in cataract patients.13
Glaucoma is a neurodegenerative disease of the optic nerve that results in retinal ganglion cell death and blindness. Population studies of Southeast Asian population found that the prevalence of POAG and PACG increased at age above 40 years old.14 The pathogenesis of many degenerative diseases as well as glaucoma are associated with mitochondrial dysfunction. This process occurs related to the aging process which causes the accumulation of oxidative stress and leads to apoptosis. Glaucoma has similar characteristics to neurodegenerative diseases such as an increasing prevalence in the elderly and a mechanism of selective neuronal cell death according to target organs. Optic nerve head (ONH) has abundant mitochondria and acts as a target site for neuronal cell damage.15 The aging process also causes an increased susceptibility of ONH in glaucoma. Mitochondrial dysfunction also occurs in the anterior chamber of the eye, mainly the trabecular meshwork.16 Our study found the mean age of the glaucoma group was above 40 years old with no significant difference in the POAG and PACG groups consistent to previous studies.17
Female gender has a higher risk of angle-closure glaucoma in Asian populations where women were more at risk for a shallow anterior chamber angle.18,19 Meanwhile, in POAG, gender was not found as a risk factor.20,21 This study demonstrated similar results; more female subjects were found in PACG but no statistical difference between groups. In the POAG group it was equal in both female and male.
The clinical characteristics of the glaucoma subjects described in Table 1 showed the mean of baseline intraocular pressure (IOP) 31.90 ± 6.67 mmHg and the mean of preoperative IOP 20.38 ± 4.71. All patients received IOP lowering medications before undergoing a surgical procedure to prevent intraoperative complications. In this study, 36.1% decrease in IOP from baseline was obtained about 7–10 days from the first visit.
This study analyzed IMA AQH levels between glaucoma patients and controls. Ischemia-modified albumin (IMA) is an albumin structure that modifies to an isoform form as a result of ischemia and oxidative stress. IMA levels are metabolic variations of albumin, which will increase as a result of ischemic event.22 There were significant differences in aqueous humor samples between the glaucoma and control groups. This indicates IMA as a product of albumin modification due to oxidative stress is present in significant amount in the aqueous humor of glaucoma patients. Serum IMA levels were not found to be significant between the control and glaucoma groups. It can be concluded that serum IMA levels cannot represent the intraocular ischemia event due to glaucoma.
The ratio of IMA AQH levels and serum was found to be the highest in the POAG group of 2.87 times compared to the control group. While the PACG group was 2.10 times higher than the control group. The results of this study were similar to previous studies by Comez et al in experimental animals.22 This study found no significant difference in IMA serum levels between groups. This result differs from the previous study by Karakurt et al, Gulpamuk et al, and Comez et al, regarding IMA serum levels in glaucoma. Previous studies had shown a significant difference in IMA serum levels between glaucoma groups, and these results were considered to be able to distinguish the severity of glaucoma.22–24
Based on the results of this study, IMA serum levels should be analyzed cautiously considering the many confounding factors that can interfere the results systemically. The ischemia process itself can occur in any part of the body and contribute to an increase of IMA serum levels. The different method of quantifying serum IMA levels also needs further evaluation. Albumin has four chains, A and B chains, N-terminal chains and Cys 34. The method of quantifying IMA serum levels in the study of Karakurt et al, Gulpamuk et al, and Comez et al were the Albumin Cobalt Binding (ACB).22–24 ACB assay method is based on a comparison of the decreased ability of cobalt binding capacity between normal albumin and albumin with N-terminal deletion so that it is unable to bind cobalt or what is called IMA. This ACB assay is not specific to the N-terminal but has a stronger affinity for the A and B chains. Meanwhile, the specific ELISA method measures the N-terminal of albumin25 This difference in the measurement method of quantifying serum IMA levels might be the cause of different results in IMA serum levels in this study.
The process of chronic ischemia also causes an inflammatory reaction, reduces ATP production from mitochondria, impairs the energy formation and ion pumps and ends in disruption of the ocular blood barrier. Based on previous studies, the CRP/albumin ratio has a role in the severity and type of uveitis as an inflammatory disease that affects systemic conditions. Decreased systemic albumin levels are a strong prognostic indicator of inflammation, so the CRP/albumin ratio (CAR) could be used as a sensitive marker for the acute phase of uveitis.26 This study provided a basis for assessing the ratio of systemic albumin to ocular disease, therefore IMA aqueous humor levels were compared to IMA serum levels. Based on Table 2, the mean ratio between IMA aqueous humor and serum levels in the cataract group was 1:2.44, the primary angle-closure glaucoma group 1:1.01, the primary open-angle glaucoma group 1:0.86, and the glaucoma group 1:0.93. The ratio between IMA aqueous humor and serum levels in the PACG group was 1:1.01, the ratio between PACG and the glaucoma group was not significantly different. The smallest ratio was found in the POAG group, 1:0.86. IMA aqueous humor levels were found to be higher overall in the glaucoma group. In the control group, the ratio of IMA AQH and serum levels was 40.9%. These results are similar to those of Elmazar et al with comparison of IMA AQH levels of about 33%.13 This shows that the process of oxidative stress that causes chronic ischemia also occurs in cataracts, although the levels are not as high as ischemia in the glaucoma group. The presence of the ocular blood barrier prevents large amounts of protein from entering the eye to prevent damage to intraocular structures. Therefore, increase IMA AQH levels represents the production and expression of IMA of the anterior structures and aqueous humor. It is estimated that proteins in aqueous humor can be found in plasma approximately 10% through an outflow pathway.27 The ratio of IMA AQH levels to serum in the control group was 40%. While in the PACG and POAG groups in this research was 99% and 116%, respectively. Although no significant findings were found in the study serum samples, an increasing ratio between IMA AQH and serum levels was identified. The ratio of IMA AQH and serum levels was found to be higher in POAG compared to PACG. This is consistent with the pathogenesis of POAG which is chronically progressive in nature. Oxidative stress in POAG occurs in the trabecular meshwork structure of the anterior chamber and retinal ganglion cells. POAG is chronically asymptomatic with a continuous ischemia process which is proven by increasing IMA AQH levels.
Intraocular pressure in glaucoma is the only known modifiable factor associated with disease progression. Elevated IOP is associated with disturbances in the regulation of the trabecular meshwork leading to decreased outflow of aqueous humor through both conventional and unconventional pathways. The duration of IOP elevation associated with retinal ganglion cell apoptosis. RGC cell death is divided into two phases. The initial phase occurred in the first three weeks by apoptosis of 36% RGC cells. The second phase is a deceleration of apoptosis.28 The populations of this study were patients who were diagnosed with glaucoma for the first time without a history of previous treatment. The POAG group showed a more severe stage than PACG group. This could be due to the possibility that the increase in IOP that occurred in the POAG was slower and chronic. Based on the glaucoma pathogenesis, elevation of IOP is caused by an increase in outflow resistance due to damage of the trabecular meshwork structures. Therefore, the duration of the IOP elevation also affected apoptosis of RGC.
The IMA AQH sample obtained from the anterior chamber of the eye, so it is possible that ischemia resulted from the trabecular meshwork structure. Based on research by Izzotti et al, the structure of the trabecular meshwork in the anterior chamber is the most susceptible to oxidative stress compared to other ocular structures. The trabecular meshwork consists of a structure of collagen beams surrounded by endothelium cells with an extracellular matrix. Structure of trabecular meshwork, which consisted of the porous structure, size and shape of the trabecular meshwork cells, volume changes, and intracellular permeability have a role in the aqueous humor outflow. This outflow process can be damaged if there is an accumulation of protein degradation due to oxidative stress or aging process that causes apoptosis. Disruption to the structure of this trabecular meshwork will trigger oxidative stress, also interfere with the aqueous humor outflow.29 In this study, oxidative stress has a correlation with increasing IOP in POAG group. Oxidative stress changes the structure of the extracellular matrix of the trabecular meshwork so that the outflow of aqueous humor is disrupted and eventually leads to IOP elevation in glaucoma. Dysfunction of the outflow accompanied by lens opacities caused the IMA AQH level of the glaucoma group to be higher than the control group. In this study, IMA AQH levels were found to have a significant correlation with IOP in the POAG group, but no correlation was found in the PACG group.
Based on the IOP elevation that occurs in glaucoma, the researchers assume that the quantification of the damage that occurs in the anterior segment through IMA AQH levels may describe the process that occurs in the posterior segment. The study showed that the trabecular meshwork and lamina cribrosa had the most similar collagen structure and protein expression. This conformity of structure results in the similarity in susceptibility to oxidative stress between the lamina cribrosa and the trabecular meshwork.30 In this study, the measurement of IMA AQH levels were associated with RNFL thinning. This study measured the level of IMA AQH in the condition that the intraocular pressure had been lowered to normal limits, but the level of IMA was still found to be significantly increased in glaucoma patients. This represents that the RNFL apoptotic process occurs not only due to mechanical factor of IOP elevation, but also through oxidative stress mechanisms.31
The current method of early detection of glaucoma is through OCT examination by quantifying RNFL thinning that describes structural glaucoma damage. Based on the previous study, it was found that the majority of glaucoma patients showed RNFL abnormalities at least 3–6 years before the damage reaching 30–50% prior to the visual field defect. Examination of RNFL thinning via OCT has several drawbacks. These tests generally need to be performed serially with sufficient time intervals to assess disease progression. In addition, the OCT value is compared with normal population data to assess the normality of the data. It is difficult to assess patients who are still in the normal range but have experienced significant thinning in RNFL or described as progression in green. Therefore, it is important to do an early detection of glaucoma, especially in patients with risk factors, because of the wide window period between the occurrence of structural damage that precedes functional impairment.4 On this basis, biomarkers have a role in early detection of disease before structural damage occurs.
This study found a significant correlation between IMA AQH levels and RNFL thinning, so the increased level of ischemia that occurs can predict the progression of RNFL thinning before the damage process can be shown by OCT examination. This is based on the IMA AQH levels as a quantification of anterior segment damage in glaucoma, where similar protein expression occurs in the posterior segment. In the glaucoma, PACG and POAG groups, there was a significant correlation between IMA AQH levels and RNFL thinning. These results indicate that the quantification of IMA AQH in addition to describing the levels of anterior segment oxidative stress can also represent processes in the posterior of intraocular especially RGC.
The data in this study found that IMA AQH levels above 9.5 ng/mL with RNFL within normal limits were the cut off for probable glaucoma patients. This value is obtained by determining the cut-off point of the population with the thickness of the RNFL still within normal limits of 90 μm. The cut-off point aims to detect populations with normal RNFL thickness but have experienced thinning progression from 2 or 3 OCT examinations (progression in green). RNFL also physiological thinning with 0.17% per year, so quantification of IMA AQH levels can be considered as an early diagnosis parameter of glaucoma in high risk population. The researchers obtained a balanced sensitivity and specificity value at the IMA level of 9.5 ng/mL with an AUC value (0.88) which is good for differentiating between the glaucoma group and the control group.
Multivariate analysis was done to assess the most contributing factor in RNFL thinning in glaucoma. This study showed that in the POAG group there was a significant correlation in IOP and IMA AQH levels. This suggests that in POAG, chronically elevated IOP and accumulation of oxidative stress contribute to RNFL thinning. However, in the PACG group a significant correlation found with IMA AQH but not in IOP elevation. According to the pathogenesis of PACG, the increase in IOP is generally shorter than POAG. This is due to anatomical factors such as lens thickness, iris apposition, and anterior chamber angle that contribute to the intermittent increase in IOP. While in POAG, the location of the outflow resistance is in the trabecular meshwork causes the increase in IOP is chronic and continuous. IMA AQH levels correlated with both POAG and PACG, indicating that oxidative stress plays a role in the pathogenesis of both glaucoma groups.
This study also analyzed other glaucoma biomarkers as a comparison. MDA as a biological marker of peroxidative cell damage triggered by oxidative stress. Lipid peroxidation is an indicator of oxidative stress at the cellular level. Elevated MDA levels are often associated with diseases caused by oxidative stress. Nucci et al found that the MDA levels in the serum and aqueous humor of glaucoma patients were increased compared to the non-glaucoma group. High serum MDA levels may reflect a similar increase in aqueous humor. This assumption is based on the state of oxidative stress that occurs locally in the ocular as well as systemically.32
We also assessed TNF-α levels as a comparative biomarker. TNF-α is an immunomodulatory cytokine, which is associated with tissue ischemia as well as damaged and remodelling of neurons. In glaucoma, an increase in TNF-α expression was found in glial cells, in addition to TNF-α receptors on retinal ganglion cells. The inflammatory component has a correlation with increased IOP and ischemia with RGC damage in glaucoma. Ischemia causes inflammation, which produces proinflammatory mediators and disrupts the integrity of vascular endothelial cells.33
This study found no correlation between serum MDA and TNF-α levels on RNFL thinning in the glaucoma group. These data were consistent with serum IMA levels that showed no association with RNFL thinning. This may be caused by a disease process that occurs mainly intraocular and systemic conditions cannot describe the course of the disease. In glaucoma, the damage to the ocular blood barrier was relatively unaffected, otherwise the main problem was the reduction of the outflow pathway. Therefore, the levels of oxidative stress in aqueous humor were not reflected by systemic levels. The equilibrium of oxidant and antioxidant levels in serum is also thought to have many confounders. Although exclusion criteria for subjects in this research have excluded systemic diseases such as diabetes, hypertension, gout, and a history of heart problems, the aging process itself is a risk factor for increased levels of systemic oxidative stress. Moreover, the small sample size can cause the discrepancy in the results of serum biological markers in this study compared to previous studies.
Overall, this study supports the role of oxidative stress in the pathogenesis of glaucoma. As far as author’s knowledge, this is the first study that evaluated the IMA AQH levels in all primary glaucoma. Biological markers of ischemia through IMA AQH levels quantification can be an alternative for early detection of glaucoma. This research could be considered to be a reference for further studies regarding the role of oxidative stress in the course of glaucoma. Research on biological markers of IMA can also develop as an alternative to glaucoma treatment through the role of local and systemic antioxidants.
Conclusions
IMA aqueous humor levels represent the state of intraocular local oxidative stress in glaucoma patients. IMA serum levels do not represent the intraocular abnormalities of glaucoma caused by local oxidative stress with an intact ocular blood barrier. Serum TNF-α and MDA levels were not found to be associated with RNFL depletion in glaucoma patients. Therefore, serum biomarkers are unable to illustrate glaucoma pathogenesis and intraocular local damage. The state of systemic oxidative stress does not reflect the local intraocular events in glaucoma. IMA AQH levels were found to increase with RNFL thinning in glaucoma. The value for the IMA aqueous humor level reference is 9.5 ng/mL as probable early diagnosis for glaucoma. This figure can be considered as a reference value for screening testing through the anterior chamber paracentesis method, especially in individuals with risk factors. IMA AQH levels in patients with POAG describe a chronic ischemic process associated with increased IOP for a longer time accompanied by accumulation of oxidative stress. IMA AQH levels reflecting intraocular oxidative stress as a factor affecting RNFL thinning in POAG and PACG groups, but were not correlated by increased IOP in PACG.
Abbreviations
AQH, aqueous humor; AUC, area under curve; DR, diabetic retinopathy; HFA, Humphrey visual field analyzer; IMA, ischemia-modified albumin; IOP, intraocular pressure; MD, mean deviation; MDA, malondialdehyde; OCT, optical coherence tomography; ONOO-, peroxynitrite; ONH, optic nerve head; PACG, primary angle closure glaucoma; POAG, primary open angle glaucoma; RGC, retinal ganglion cell; RNFL, retinal nerve fiber layer; ROC, receiver operating characteristic; rpm, revolutions per minute; ROS, reactive oxygen species; TNF-α, tumor necrosis factor alpha.
Disclosure
The authors have no conflicts of interest to report in this research.
References
1. Jonas JB, Aung T, Bourne RR. Glaucoma. Lancet Lond Engl. 2017;390(10108):2183–2193.
2. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–2090. doi:10.1016/j.ophtha.2014.05.013
3. Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–267. doi:10.1136/bjo.2005.081224
4. Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma. JAMA. 2014;311(18):1901–1911. doi:10.1001/jama.2014.3192
5. Gabelt BT, Kaufman PL. Changes in aqueous humor dynamics with age and glaucoma. Prog Retin Eye Res. 2005;24(5):612–637. doi:10.1016/j.preteyeres.2004.10.003
6. Lipton P. Ischemic cell death in brain neurons. Physiol Rev. 1999;79(4):1431–1568.
7. Kähler J, Ewert A, Weckmüller J, et al. Oxidative stress increases endothelin-1 synthesis in human coronary artery smooth muscle cells. J Cardiovasc Pharmacol. 2001;38(1):49–57. doi:10.1097/00005344-200107000-00006
8. Yorio T, Krishnamoorthy R, Prasanna G. Endothelin: is it a contributor to glaucoma pathophysiology? J Glaucoma. 2002;11(3):259–270. doi:10.1097/00061198-200206000-00016
9. Harper RA, Reeves BC. Glaucoma screening: the importance of combining test data. Optom Vis Sci. 1999;76(8):537–543. doi:10.1097/00006324-199908000-00022
10. Kerrigan–Baumrind LA, Quigley HA, Pease ME, Kerrigan DF, Mitchell RS. Number of ganglion cells in glaucoma eyes compared with threshold visual field tests in the same persons. Invest Ophthalmol Vis Sci. 2000;41(3):741–748.
11. Coleman AL, Kodjebacheva G. Risk factors for glaucoma needing more attention. Open Ophthalmol J. 2009;3:38. doi:10.2174/1874364100903020038
12. Michael R, Bron AJ. The ageing lens and cataract: a model of normal and pathological ageing. Biol Sci. 2011;366(1568):1278–1292. doi:10.1098/rstb.2010.0300
13. Elmazar HM, Elmadbouh I, Mandour SS, Al Ariny GM, Ibrahim AM. Association between cataract progression and ischemia-modified albumin in relation to oxidant–antioxidant profiles in the serum, aqueous humor, and lens. J Cataract Refract Surg. 2018;44(2):134–139. doi:10.1016/j.jcrs.2017.10.051
14. Cho HK, Kee C. Population-based glaucoma prevalence studies in Asians. Surv Ophthalmol. 2014;59(4):434–447. doi:10.1016/j.survophthal.2013.09.003
15. Kong GY, Van Bergen NJ, Trounce IA, Crowston JG. Mitochondrial dysfunction and glaucoma. J Glaucoma. 2009;18(2):93–100. doi:10.1097/IJG.0b013e318181284f
16. Saccà SC, Pulliero A, Izzotti A. The dysfunction of the trabecular meshwork during glaucoma course. J Cell Physiol. 2015;230(3):510–525. doi:10.1002/jcp.24826
17. Alasil T, Wang K, Keane PA, et al. Analysis of normal retinal nerve fiber layer thickness by age, sex, and race using spectral domain optical coherence tomography. J Glaucoma. 2013;22(7):532–541. doi:10.1097/IJG.0b013e318255bb4a
18. Xu L, Cao WF, Wang YX, Chen CX, Jonas JB. Anterior chamber depth and chamber angle and their associations with ocular and general parameters: the Beijing Eye Study. Am J Ophthalmol. 2008;145(5):929–936. doi:10.1016/j.ajo.2008.01.004
19. Liang Y, Friedman DS, Zhou Q, et al. Prevalence and characteristics of primary angle-closure diseases in a rural adult Chinese population: the Handan eye study. Invest Ophthalmol Vis Sci. 2011;52(12):8672–8679. doi:10.1167/iovs.11-7480
20. Dandona L, Dandona R, Mandal P, et al. Angle-closure glaucoma in an urban population in southern India. The Andhra Pradesh eye disease study. Ophthalmology. 2000;107(9):1710–1716. doi:10.1016/S0161-6420(00)00274-8
21. Tehrani S. Gender difference in the pathophysiology and treatment of glaucoma. Curr Eye Res. 2015;40(2):191–200. doi:10.3109/02713683.2014.968935
22. Taskiran Comez A, Cakir DU, Tutunculer FK, Gencer B, Tufan HA. Relationship between raised intraocular pressure and ischemia-modified albumin in serum and humor aqueous: a pilot study in rabbits. Int J Ophthalmol. 2014;7(3):421–425. doi:10.3980/j.issn.2222-3959.2014.03.06
23. Karakurt Y, Mertoglu C, Gok G, et al. Thiol-disulfide homeostasis and serum ischemia modified albumin levels in patients with primary open-angle glaucoma. Curr Eye Res. 2019;44(8):896–900. doi:10.1080/02713683.2019.1594925
24. Gulpamuk B, Elgin U, Sen E, Yilmazbas P, Neselioglu S, Erel O. Evaluation of dynamic thiol-disulfide homeostasis in glaucoma patients and the correlation with retinal nerve fiber layer analysis. Eur J Ophthalmol. 2020;30(4):690–699. doi:10.1177/1120672119839582
25. Oran I, Oran B. Ischemia-modified albumin as a marker of acute coronary syndrome: the case for revising the concept of (N-terminal modification) to (fatty acid occupation) of albumin. Dis Markers. 2017;2017:8. doi:10.1155/2017/5692583
26. Bozkurt E, Muhafiz E, Sengul D, Uçak T, Atum M. Can the CRP/albumin ratio be used as a new indicator of activation in patients with uveitis? Ocul Immunol Inflamm. 2021;29(5):1017–1022. doi:10.1080/09273948.2020.1714061
27. Freddo TF. A contemporary concept of the blood-aqueous barrier. Prog Retin Eye Res. 2013;32:181–195. doi:10.1016/j.preteyeres.2012.10.004
28. Agarwal R, Gupta SK, Agarwal P, Saxena R, Agrawal SS. Current concepts in the pathophysiology of glaucoma. Indian J Ophthalmol. 2009;57(4):257–266. doi:10.4103/0301-4738.53049
29. Izzotti A, Longobardi M, Cartiglia C, Saccà SC. Mitochondrial damage in the trabecular meshwork occurs only in primary open-angle glaucoma and in pseudoexfoliative glaucoma. PLoS One. 2011;6(1):e14567. doi:10.1371/journal.pone.0014567
30. Steely HT, English-Wright SL, Clark AF. The similarity of protein expression in trabecular meshwork and lamina cribrosa: implications for glaucoma. Exp Eye Res. 2000;70(1):17–30. doi:10.1006/exer.1999.0764
31. Pavan J, Lukenda A, Šarlija M, et al. Retinal nerve fibre layer thickness in conditions of severe ischemia in patients without glaucoma. Period Biol. 2010;112(1):121–124.
32. Nucci C, Di Pierro D, Varesi C, et al. Increased malondialdehyde concentration and reduced total antioxidant capacity in aqueous humor and blood samples from patients with glaucoma. Mol Vis. 2013;19:1841–1846.
33. Balaiya S, Edwards J, Tillis T, Khetpal V, Chalam KV. Tumor necrosis factor-alpha (TNF-α) levels in aqueous humor of primary open angle glaucoma. Clin Ophthalmol Auckl NZ. 2011;5:553–556. doi:10.2147/OPTH.S19453
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




