Back to Journals » International Journal of General Medicine » Volume 14
A New Modified Hysteroscopic-Laparoscopic Surgery for Cesarean Scar Pregnancy of Stable Type III
Authors Yang J, Li B, Liu J, Zeng W, Hong L
Received 27 February 2021
Accepted for publication 18 May 2021
Published 3 June 2021 Volume 2021:14 Pages 2289—2295
DOI https://doi.org/10.2147/IJGM.S308768
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Supplementary Video of the Original Research paper “A New Modified Hysteroscopic-laparoscopic Surgery for Cesarean Scar Pregnancy of Stable Type III”.
Views: 620143
Jiang Yang,* Bingshu Li,* Jin Liu, Wanlin Zeng, Li Hong
Department of Gynecology and Obstetrics, Renmin Hospital of Wuhan University, Hubei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Li Hong
Department of Gynecology and Obstetrics, Renmin Hospital of Wuhan University, 238 Jiefang Road, Wuhan, Hubei, 430060, People’s Republic of China
Email [email protected]
Objective: To introduce a modified hysteroscopic-laparoscopic operation for cesarean scar pregnancy (CSP) of stable type III.
Patients and Methods: We retrospectively studied the case notes of 31 patients with stable type III cesarean scar pregnancy who underwent hysteroscopic-laparoscopic surgery in our hospital. Thirteen patients received the modified hysteroscopic-laparoscopic surgery (modified surgery group), and eighteen patients received traditional hysteroscopic-laparoscopic surgery (traditional surgery group).
Results: There was no significant difference in patients’ age, gestational age, number of previous cesarean sections, the serum human chorionic gonadotropin (hCG) level before surgery, gestational sac diameter, myometrium thickness between the two groups. In the modified hysteroscopic-laparoscopic surgery, the mean surgical time was 50.45± 24.45 mins, the mean length of stay in hospital was 4.50± 0.50 days, which was significantly shorter than the traditional surgery group (84.75± 33.28 mins and 5.50± 0.75 days, respectively). And the intraoperative hemorrhage in the modified group was also less than that in the traditional group (40.50± 12.25 mL vs 75.33± 25.45mL). Whereas the time for hCG normalization, postoperative vaginal bleeding and menstrual recovery had no significant difference between the modified surgery group and the traditional surgery group. There was no recurrence of CSP in both groups.
Conclusion: The modified hysteroscopic-laparoscopic surgery had shorter operation time, less blood loss, and sooner recovery time after surgery compared to traditional hysteroscopic-laparoscopic surgery, which could be more beneficial to our patients and should be applied in clinics generally.
Keywords: cesarean scar pregnancy, hysteroscopic-laparoscopic surgery, modified surgery, traditional surgery
Introduction
Cesarean scar pregnancy (CSP) is a relatively novel type of ectopic pregnancy that may occur as a rare and peculiar complication in the subsequent pregnancy following Cesarean delivery (CD), which is characterized by the implantation of the gestational sac (GS) into the previous hysterotomy scar.1 Over the last two decades, with the increasing rate of CD in clinical and the improvement in imaging and diagnostic technology, the morbidity of CSP has been resultantly escalating. It was estimated that 1 in 531 women with the cesarean scar would have the CSP and that nearly 4.2% of ectopic pregnancies are CSP.2 Once the CSP aborts or infiltrates into the muscular tissue, the patients usually suffer from series of dangerous complications, such as massive hemorrhage, uterine placenta implantation, uterine rupture, and they even need to receive a hysterectomy.1,3,4
Diagnostic criteria for CSP include the presence of GS at the site of the previous uterine incision, increased serum β-human chorionic gonadotropin (β-hCG) level (normal range is less than 5 m IU/mL), the presence of an empty uterine cavity, and a discontinuity at the anterior wall of the uterus adjacent to the GS, and the thin myometrium between the sac and the bladder.3,5,6 Importantly, the improvement of ultrasonography permits the earlier and more accurate diagnosis of CSP, allowing more successful preservation of the uterus without maternal complications. Thus, it provides reliable evidence for the diagnosis and the treatment formulation of CSP, which could be conducive to the formulation of treatment plans and post-treatment follow-up.3,7–9
The treatment of CPS should follow the evidence-based principle and we must pay attention to the occurrence of severe complications and focus on the preservation of the patient’s fertility. To date, there is no universal agreement on the best treatment method. For better management of CSP, it is recommended to classify CSP into three types10 (Type I, Type II, and Type III) according to the ultrasonographic imaging characteristics. The classification is based on the growth direction of the GS implantation on the scar and the thickness of the myometrium between the pregnancy sac and the bladder in the anterior uterine wall. So far, a multitude of treatment modalities have been proposed for the management of Type I and Type II CSP, such as uterine artery embolization, drug administration (local or systemic administration of methotrexate or potassium chloride), dilation and curettage (D&C), and surgery (transabdominal, transvaginal, hysteroscopy, hysteroscopy, laparoscopy, and hysteroscopy combined with laparoscopy),1,2,11,12 but in terms of patient’s safety and clinical effectiveness, the best treatment method still requires further evaluation and determination. Particularly, Type III CSP has the highest level of risk among the three types. To be more specific, in Type III CSP the GS in irregular or regular shape entirely penetrates within the myometrium and abundant vascularization can be observed at the incision site on the uterus.10 If it was not terminated as soon as possible, the GS could turn into placenta implantation or placenta previa, which may lead to massive hemorrhage, uterine perforation or even bladder injury. Additionally, during the termination, the rates of enormous intraoperative hemorrhage, incomplete removal of gestational tissue and recurrent CSP in Type III CSP are notably higher than the other two types of CSP. According to China Medical Association (CMA) guidelines, it is recommended that hysteroscopic-laparoscopic operation could be utilized for stable Type III CSP: first, using diagnostic and operative laparoscopy to remove the gestational tissue and repair the scar dehiscence, then utilizing hysteroscopy to confirm no gestational remnants and other intrauterine problems. But there are some limitations of this kind of surgery such as uncontrolled bleeding during the operation and recurrence of incision diverticulum after the operation. Thus, we prefer to introduce a modified hysteroscopic-laparoscopic operation for stable Type III CSP which could repair incision diverticulum without any affection on the integrity of the uterine lining, improve the recovery time of menstruation effectively, eliminate the abnormal bleeding, protect and promote future fertility ability and avoid the recurrence of CSP.
Patients and Methods
Patients
The study was discussed and approved by the Ethics Council of Renmin Hospital of Wuhan University. We retrospectively evaluated the cases of 31 patients with stable Type III CSP who received hysteroscopic-laparoscopic surgery in our hospital from July 2016 to July 2020. Among the 31 cases, 13 patients received the modified hysteroscopic-laparoscopic operation, and 18 cases received traditional hysteroscopic-laparoscopic surgery. The diagnostic criteria13 is as follows: 1. History of previous cesarean birth; 2. Positive pregnancy test; 3. Gestational age <8weeks; 4. Stable vital signs without abdominal pain, abdominal bleeding and hemorrhagic shock. 5. Three-dimensional ultrasound image result including I. Both uterine cavity and cervical canal were empty; II. The pregnancy capsule was implanted in the anterior wall of the uterine isthmus or the cesarean scar defect; III. The continuity of the myometrium of the anterior uterine wall was interrupted, and the myometrium between the pregnancy capsule and the bladder was significantly thinner, which means the thickness of the myometrium ≤3mm. IV. High-speed, low-impedance blood vessels around the trophoblast clearly surround the capsule in Doppler examination. Each patient provided written informed consent before treatment.
Operation Method
Under general endotracheal anesthesia, the patient was placed in the dorsal lithotomy position. The abdominal cavity was insufflated with carbon dioxide and intra-abdominal pressure was maintained at 15 mmHg. A 10-mm trocar was inserted through the supraumbilical port in an attempt to visualize the implantation site within the previous uterine scar. Three more ancillary trocars were placed: one in the left mid quadrant (15-mm trocar); one in the left lower quadrant, 5cm medial to the left anterior superior iliac crest (5-mm trocar); and one at McBurney point (5-mm trocar).
The Modified Hysteroscopic-Laparoscopic Surgery
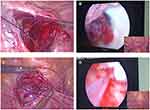
First, peritoneal reflection is dissected and the bladder is pushed down to exposure uterine cesarean scar more clearly. Second, we open the lateral peritoneum, temporarily ligature the bilateral uterine arteries by a surgical suture (Figure 1A). Third, we use hysteroscopy to observe the location of ectopic gestational tissue on the cesarean scar and confirm that the root of villi is not implanted into the myometrium, of particular note is the situation that the root of villi has been implanted into myometrium with abundant blood supply, is not suitable for the modified hysteroscopic-laparoscopic surgery. Then, with the laparoscopic monitoring, we remove the pregnancy tissues by suction curettage and left an intact serosal layer of the cesarean scar (Figure 1B), and then hysteroscopy is utilized once again to check or clear the residual gestational mass. Fourth, a continuous mattress suture is utilized for the seromuscular layer of isthmus uteri with 2–0 spiral PDO to internalize the serosal layer of the cesarean scar for reinforcement (Figure 1C). Last but not least, we release the stitches of bilateral uterine arteries, and hysteroscopy is performed again to confirm the adequate repair of the uterine scar defect (Figure 1D). The whole operation is recorded in Video 1.
Traditional Hysteroscopic-Laparoscopic Surgery
First, we dissect the peritoneum reflection, and the bladder is pushed down to visualize the lower uterine myometrial implantation site more clearly. Second, we occlude the bilateral internal iliac arteries with metal clips. Third, we dissect the gestation from the anterior uterine isthmus with electrocautery, the dark reddish tissue is swiftly removed with laparoscopic spoon forceps. Fourth, we repair the cesarean scar dehiscence with one layer of continuous endoscopic sutures with 2–0 spiral PDO. Then the metal clips are removed. As designed, hysteroscopy is performed to confirm there is no remnant.
Statistical Analysis
All the data were subjected to statistical analysis with the Statistical Product and Service Solutions (SPSS) 22.0 software (SPSS, Inc., USA). The skewness and kurtosis were utilized to evaluate the data distribution. If the normal distribution was met, continuous data were expressed as mean ± standard deviation, and an unpaired two-tailed Student’s t test was used to compare the differences. Otherwise, continuous data were described as median (P25-P75), and Mann–Whitney U-test was performed for comparison. The value of p<0.05 was considered statistically significant.
Results
The General Data of the Patients
The clinical characteristics of the patients are presented in Table 1. There were no significant differences between the two groups in patient age, gestational age, number of previous cesarean sections, the serum human chorionic gonadotropin (hCG) level before surgery, the average diameter of the gestational sac, the myometrium thickness and vaginal bleeding.
 |
Table 1 Clinical Characteristics of the Patients |
Surgical Indicator of the Patients
However, as it is illustrated in Table 2, in the modified hysteroscopic-laparoscopic surgery, the mean surgical time and the length of stay in hospital were 50.45±24.45 mins and 4.50±0.50 days, respectively, which was significantly shorter than the traditional surgery group (84.75±33.28 mins and 5.50±0.75 days, respectively). Besides, the intraoperative hemorrhage in the modified group was less than that in the traditional group (40.50±12.25 mL vs 75.33±25.45mL). Whereas the time for hCG normalization, postoperative vaginal bleeding and menstrual recovery had no significant difference between the modified hysteroscopic-laparoscopic surgery group and traditional hysteroscopic-laparoscopic surgery group. There was no recurrence of CSP in both groups.
 |
Table 2 Comparison of the Parameters of the Two Groups |
Discussion
For type III CSP, although a number of researches have proved that traditional hysteroscopic-laparoscopic surgery was safe and efficient surgical procedures could be adopted as primary treatment modalities, the ideal management should be minimally invasive, with low morbidity and low cost. Reducing surgical time could lower the cost of surgery and the risk of complications. Previous studies found that the operation time of traditional hysteroscopic-laparoscopic surgery group ranged from 56 to 120 minutes with a median of 75 minutes,14 which showed similar results with ours (84.75±33.28 mins). Fortunately, the operation time of 13 patients who underwent the modified surgery in our study was significantly shortened (50.45±24.45 mins). It is noted that the two surgery methods were performed by surgeons with comparative excellent skills in laparoscopy and hysteroscopy, the shorter surgical time in the group with the modified technique was not due to the greater experience of the treating group. Moreover, the modified surgeries have been operated successfully so that no patient have to switch to the traditional surgery. Therefore, the modified hysteroscopic-laparoscopic surgery has significant advantages in operation time. Many studies have proved the mean procedure time was positive correction with the mean total cost and complications,15–18 regrettably, we did not include patient cost in the study. Therefore, we cannot prove that the modified surgery reduces the total cost in our study, but we believe that later studies that include this parameter will illustrate the advantages in patient costs in the modified surgery. Moreover, hospitalization time of patients has been demonstrated significantly decreased in patients who underwent the modified hysteroscopic-laparoscopic surgery compared with the patients with traditional surgery (4.50±0.50 days vs 5.50±0.75 days) in our study, which is considered to be another parameter for patient’s cost.18,19 Therefore, the modified hysteroscopic-laparoscopic surgery may reduce cost and bring more benefits for patients.
Intraoperative bleeding volume is a crucial parameter to evaluate the quality of surgery, and it is significantly related to the recovery of patients after surgery. Our study demonstrated that the intraoperative bleeding volume of the modified hysteroscopic-laparoscopic surgery group was significantly less than that of the traditional surgery group (40.50±12.25 mL vs 75.33±25.45mL), which also indicates that the modified surgery could lead less damage. Indeed, the modified hysteroscopic-laparoscopic surgery we proposed could reduce the harm to the uterus and less blood vessels would be cut off because it just need to be performed a continuous mattress suture for the seromuscular layer of isthmus uteri to internalize the serosal layer of the cesarean scar for reinforcement and does not cut the serosal layer of uterus.
Cesarean scar endometriosis (CSE) is an iatrogenic disease caused by endometrium implantation in the incision during the surgical operation. The main reason is that the whole layer of the uterus is cut and the endometrial tissue is directly inoculated. Cesarean section is the most common cause of CSE.20,21 Therefore, avoiding endometrial tissue being inoculated in the abdominal cavity or surgical incision is an important measure to reduce the incidence of endometriosis. In the modified surgery, we do not need to perform hysterotomy and can retain the integrity of the serosal layer, effectively avoiding the inoculation of endometrial tissue and the risk of occurrence of endometriosis. Laparoscopic hysterectomy permits a higher incidence of infection, with major risk factors of vaginitis and retrograde infection due to pathogenic organisms within 1 month before cervical or uterine surgery.22 Thirteen scar pregnancies are often accompanied by prolonged vaginal bleeding that increases the risk of infection. Traditional hysteroscopic-laparoscopic surgery could lead to exposure of pelvic and abdominal organs and increase the risk of intra-abdominal infection because of the loss of uterine integrity. The modified surgery can effectively avoid the aforementioned situation because of the maintenance of serosal layer integrity and less harm of myometrium. Unfortunately, due to the small number of cases we collected, the abdominal infection did not occur in either group of patients. Therefore, a large sample study is needed.
There were no significant differences in HCG normalization time, menstrual recovery time and CSP recurrence time between the two groups, which supposed that the modified hysteroscopic-laparoscopic surgery had the same safety and effectiveness compared with the traditional hysteroscopic-laparoscopic. What is more, the modified surgery could bring more benefit for patients and should be applied in clinics generally. Although our current results suggest that patients can benefit more from the modified hysteroscopic-laparoscopic surgery, the findings may be biased due to the insufficient sample size. Therefore, multi-center, large-sample clinical studies are needed to explore the effectiveness and safety of the modified surgical. In addition, the parameters not included in this study, such as postoperative administration time of antibiotics, postoperative infection rate, patient total costs, surgical complication, the incidence of scar endometriosis, etc., are supposed to be analyzed in further studies. Moreover, the size of the “niche” from a range of time periods (such as 3 months, 6 months, 1 year and 3 years after operation) and the situation of repregnancy of the patients should be also included, these are, after all, key factors in evaluating the effectiveness of the modified surgery.
Conclusion
The modified hysteroscopic-laparoscopic surgery had shorter operation time, less blood loss, and sooner recovery time after surgery compared to traditional hysteroscopic-laparoscopic surgery, which could benefit more for our patients and should be applied in clinics generally.
Ethical Approval
This study was reviewed and approved by the Ethics Council of Renmin Hospital of Wuhan University and written informed consents were obtained from all participants (No: 2016K-C009). This study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
We are grateful to everyone involved in carrying out the study, analyzing the data and producing the manuscript from the Department of Obstetrics and Gynecology, Renmin Hospital of Wuhan University, for their sincere help and technique support. This study was supported by the Hubei Province’s Outstanding Medical Academic Leader Program.
Author Contributions
Jiang Yang, Bingshu Li, Jin Liu and Li Hong were responsible for designing the research and generating the primary draft and the graphics. Bingshu Li, Li Hong and Wanling Zeng were the operators of the surgeries and contributed to the organization, suggestions on the content and drafting the manuscript. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors have no conflicts of interest to declare.
References
1. Birch Petersen K, Hoffmann E, Rifbjerg Larsen C, Svarre Nielsen H. Cesarean scar pregnancy: a systematic review of treatment studies. Fertil Steril. 2016;105(4):958–967. doi:10.1016/j.fertnstert.2015.12.130
2. Fylstra DL. Ectopic pregnancy within a cesarean scar: a review. Obstet Gynecol Surv. 2002;57(8):537–543.
3. Timor-Tritsch IE, Monteagudo A. Unforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy. A Review. Am J Obstet Gynecol. 2012;207(1):14–29.
4. Gregory KD, Jackson S, Korst L, Fridman M. Cesarean versus vaginal delivery: whose risks? Whose benefits? Am J Perinatol. 2012;29(1):7–18.
5. Naji O, Abdallah Y, Bij De Vaate AJ, et al. Standardized approach for imaging and measuring Cesarean section scars using ultrasonography. Ultrasound Obstet Gynecol. 2012;39(3):252–259.
6. D’Antonio F, Palacios-Jaraquemada J, Lim PS, et al. Counseling in fetal medicine: evidence-based answers to clinical questions on morbidly adherent placenta. Ultrasound Obstet Gynecol. 2016;47(3):290–301.
7. Wang CJ, Yuen LT, Yen CF, Lee CL, Soong YK. Three-dimensional power Doppler ultrasound diagnosis and laparoscopic management of a pregnancy in a previous cesarean scar. J Laparoendosc Adv Surg Tech A. 2004;14(6):399–402.
8. Liu D, Yang M, Wu Q. Application of ultrasonography in the diagnosis and treatment of cesarean scar pregnancy. Clin Chim Acta. 2018;486:291–297.
9. Maheux-Lacroix S, Li F, Bujold E, Nesbitt-Hawes E, Deans R, Abbott J. Cesarean scar pregnancies: a systematic review of treatment options. J Minim Invasive Gynecol. 2017;24(6):915–925.
10. Wu Y, Zhou L, Chen L, Zhou Q, Zeng T. Efficacy of contrast-enhanced ultrasound for diagnosis of cesarean scar pregnancy type. Medicine (Baltimore). 2019;98(44):e17741.
11. Siedhoff MT, Schiff LD, Moulder JK, Toubia T, Ivester T. Robotic-assisted laparoscopic removal of cesarean scar ectopic and hysterotomy revision. Am J Obstet Gynecol. 2015;212(5):681e681–684.
12. Sugawara J, Senoo M, Chisaka H, Yaegashi N, Okamura K. Successful conservative treatment of a cesarean scar pregnancy with uterine artery embolization. Tohoku J Exp Med. 2005;206(3):261–265.
13. Zhang B, Jiang ZB, Huang MS, et al. Uterine artery embolization combined with methotrexate in the treatment of cesarean scar pregnancy: results of a case series and review of the literature. J Vasc Interv Radiol. 2012;23(12):1582–1588.
14. Fu LP. Therapeutic approach for the cesarean scar pregnancy. Medicine (Baltimore). 2018;97(18):e0476.
15. Mazzola F, Smithers F, Cheng K, et al. Time and cost-analysis of virtual surgical planning for head and neck reconstruction: a matched pair analysis. Oral Oncol. 2020;100:104491.
16. Awad MA, Buzalewski J, Anderson C, et al. Robotic inguinal hernia repair outcomes: operative time and cost analysis. JSLS. 2020;24:4.
17. Daley BJ, Cecil W, Clarke PC, Cofer JB, Guillamondegui OD. How slow is too slow? Correlation of operative time to complications: an analysis from the Tennessee surgical quality collaborative. J Am Coll Surg. 2015;220(4):550–558.
18. Chen BP, Clymer JW, Turner AP, Ferko N. Global hospital and operative costs associated with various ventral cavity procedures: a comprehensive literature review and analysis across regions. J Med Econ. 2019;22(11):1210–1220.
19. Noba L, Rodgers S, Chandler C, Balfour A, Hariharan D, Yip VS. Enhanced Recovery After Surgery (ERAS) reduces hospital costs and improve clinical outcomes in liver surgery: a systematic review and meta-analysis. J Gastrointest Surg. 2020;24(4):918–932.
20. Zhang P, Sun Y, Zhang C, et al. Cesarean scar endometriosis: presentation of 198 cases and literature review. BMC Womens Health. 2019;19(1):14.
21. Zhu X, Chen L, Deng X, Xiao S, Ye M, Xue M. A comparison between high-intensity focused ultrasound and surgical treatment for the management of abdominal wall endometriosis. Bjog-Int J Obstet Gy. 2017;124:53–58.
22. Weijia Y, Wanwan X, Rui W, Xiaofeng Z. Risk factors for perioperative infection after laparoscopic hysterectomy. Chinese J Med. 2020;55(8):864–867.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.