Back to Journals » International Journal of General Medicine » Volume 14
A New Accurate, Simple and Less Radiation Exposure Device for Distal Locking of Femoral Intramedullary Nails
Authors Gao H , Liu Z, Wang G , Wang B
Received 20 May 2021
Accepted for publication 27 July 2021
Published 4 August 2021 Volume 2021:14 Pages 4145—4153
DOI https://doi.org/10.2147/IJGM.S321005
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hua Gao, Zhenyu Liu, Gang Wang,* Baojun Wang*
Department of Orthopaedics, Beijing Friendship Hospital, Capital Medical University, Beijing, 100050, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Gang Wang; Baojun Wang
Department of Orthopaedics, Beijing Friendship Hospital, Capital Medical University, 95 Yong’an Road, Xicheng, Beijing, 100050, People’s Republic of China
Tel +86-10-63138753
Fax +86-10-63138353
Email [email protected]; [email protected]
Background: Due to the metal elasticity of intramedullary nails (IMs) and irregularities of the long bone marrow cavity and other reasons, one of the greatest challenges for surgeons is to position the distal locking screw. Therefore, a novel laser guiding navigation device was designed for the distal locking of femoral IMs. The purpose of this study was to compare the effectiveness of the novel device and freehand technique for distal locking of IMs in the femoral model.
Methods: The laser guiding navigation device (laser group) and freehand technique (freehand group) were used in the distal locking of the IMs in the femoral model. All operations were performed by surgeons of the same level. The differences between the two groups were compared in terms of operative time, radiation exposure time, first success rate, deviation angle between ideal trajectory and actual trajectory, and learning curve.
Results: The distal locking of the IMs in the femoral model was performed 40 times in each group. The results showed that the laser group was better than the freehand group in terms of operative time (345± 165 VS 212± 105 seconds, t=4.27, P< 0.001), radiation exposure time (164± 57 VS 41± 15 seconds, t=13.15, P< 0.001) and first successrate (χ2=21.36, P< 0.001). Compared with the freehand group, the actual trajectory of the laser group was closer to the ideal trajectory in coronal and horizontal planes. Furthermore, the learning curve time of the laser group was shorter.
Conclusion: Compared with traditional freehand technique, the novel laser guiding navigation device can shorten the operative time and reduce radiation exposure invitro. In addition, it is easy to master with more accuracy and a higher first success rate in vitro.
Keywords: femur, intramedullary nails, laser guiding navigation device, freehand technique
Introduction
Minimally invasive treatment is the development trend of trauma and orthopedics1. Intramedullary nail is one of the key “weapons” for minimally invasive treatment. However, due to the metal elasticity of IMs and irregularities of the long bone marrow cavity2, positioning the distal locking screw is one of the greatest challenges for surgeons3, which results in a long operation and radiation exposure time.
In response to this problem, many novel technologies to localize distal locking holes, have been invented, such as electromagnetic navigation technology4, computer-aided navigation technology5, orthopedic robots6 and so on. However, these technologies (including traditional freehand technique7) still have some limitations, such as inaccurate positioning, low first success rate, high demand for expensive equipment, long learning curve of surgeons.6–13
Based on the above problems, our team designed a laser guiding navigation device based on G-arm and a matching positioning technique by taking advantage of the characteristics of the accuracy and stability of laser. The device has the advantages of easy installation, accurate positioning, no radiation exposure during operation, and is easy to master. This study focused on the application of the new device in the distal locking of IMs in the femoral model, and compared the effectiveness with the traditional freehand technique14.
Materials and Methods
The femoral model (SAWBONES, Left Femur, Foam Cortical, 16 mm Canal, 47cm length) was firmly fixed in the blind box, and it was ensured that the blind box and the femoral model could not be moved during the operation. The distal locking of the IMs (WASTON, Professional X Series, diameter 9.5mm, length 380 mm) in the femoral model was performed 40 times in each group. 40 operations of each group were performed in 4 sequences and one sequence (10 operations) was performed per day. Each time we first used the laser guiding navigation device in 10 operations, then freehand technique in 10 operations. All operations were performed by two senior residents who finished three years of specialized training. They received the same amount of time training for freehand technique, and their skill levels were very close.
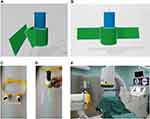
Description of the Novel Device
The laser guiding navigation device consisted of 4 major components: a horizontal green-light laser pointer (in-line, energy 100mW, wavelength 520nm, Senwei Electronic Commerce Co., Ltd), a coronal red-light laser pointer (in-line, energy 100mW, wavelength 635nm, Senwei Electronic Commerce Co., Ltd), two laser pointer pedestals, a round strap attached to the G-arm’s image intensifier (Figure 1). Before operation, the device was adjusted repeatedly to ensure that the intersection of the two laser lines, X-ray fluoroscopy center and display screen center were completely overlapped (Figure 2). When the device was first installed on the G-arm’s image intensifier, it needed to be installed and adjusted. It took no more than 10 minutes. Each G-arm machine needed to be installed and adjusted for the first time and it only needed to be calibrated in the following use. The calibration time was not more than 1 minute every time. This should be done before the operation.
Surgical Procedure
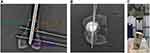
In the group undergoing the freehand technique15, it was crucial to confirm that the distal nail holes appeared as a perfect circle in the lateral image of the G-arm fluoroscope. Then we kept the direction of the Kirschner wire (Φ=2mm) and gradually drilled and stayed on the same axis under fluoroscopic visualization. After fluoroscopy confirmed that the Kirschner wire passed through the nail hole, we used a drill bit to enlarge the screw channel, measured the length of the channel, and inserted the distal screw.
In the laser group, the same as the freehand technique15, when the distal nail hole in the lateral image of the G-arm fluoroscope was a perfect circle, adjusted the position of G-arm to ensure that the center of the nail hole was overlapped with the center of the display screen. It meant that the center of the nail hole was overlapped with the intersection of the two laser lines. Ensured that the Kirschner wire (Φ=2mm) was drilled along the red and green laser lines and confirmed that the Kirschner wire passed through the nail hole through fluoroscopy (Figure 3). Then we used a drill bit to enlarge the screw channel, measured the length of the channel, and inserted the distal screw.
Observation Indicators
1. Main indicators: ① Operative time, starting from the positioning of the distal nail hole, including the total time (seconds) of positioning and insertion of the distal screw; ② Radiation exposure time, including the total fluoroscopy time (seconds) of positioning and insertion of the distal screw.
2. Other indicators: ① Imaging indicators, the Picture Archiving and Communication System (PACS)16 was used to measure the deviation angle (coronal plane, horizontal plane) between the actual trajectory and the ideal trajectory (Figure 4). The coronal deviation angle was measured according to the long axis of IMs17. The ideal vertical line through the center of the nail hole was regarded as the ideal trajectory18, and the Kirschner wire passing through the nail hole was regarded as the actual trajectory19, and the angle between the two lines was regarded as the track angle of the coronal plane (TAC). The femoral vertical fluoroscopy image was used to measure the horizontal deviation angle17. The line parallel to the tangent line of the posterior condyle of the femur was regarded as the ideal trajectory, and the Kirschner wire was regarded as the actual trajectory. The angle between the two lines was regarded as the track angle of horizontal plane(TAH); ② The success rate of the first positioning; ③ The change of the operator’s learning curve.
Sample Size Estimation and Statistical Methods
According to the data obtained in the preliminary test (trauma orthopedics series operation simulator, Melerit Medical TraumaVision20,21), we set the first-class error to 0.025 and the power to be 0.9 through calculation of PASS software based on the 2 main research indicators. The minimum sample size for the study of operative time (seconds) was 14 and 4 for the exposure time (seconds). Considering the actual situation of this study, the sample size of each group was finally determined to be 40. Continuous variables were presented as mean±standard deviation (SD), and the independent sample t-test was used to evaluate differences of quantitative values between two methods, including the operative time, radiation exposure time, TAC and TAH. Categorical variables were presented as frequency and percentage, and the paired chi-square test was used to evaluate differences between two methods, including the first success rate. All statistical analyses were performed using the SPSS Statistics version 22 (IBM Corp., Armonk, NY). Statistical significance was defined as P<0.05.
Results
The average operative time of the freehand group was 345±165 seconds, whereas the time was 212±105 seconds in the laser group. The average radiation exposure time of the freehand group and the laser group was 164± 57 seconds and 41±15 seconds respectively. The average operative time of the laser group was statistically significantly shorter compared to the freehand group (t=4.27, P<0.001), and the exposure time was significantly reduced in the laser group compared to the freehand group (t=13.15, P<0.001). (Figure 5).
 |
Figure 5 The box plot showed the operative and radiation exposure time of the laser group was statistically significantly shorter compared to the freehand group. |
The TAC of the freehand group and the laser group were 6.7±1.1° and 2.9±0.8° respectively, and the difference was statistically significant (t=9.12, P<0.001); In terms of the TAH, the freehand group and the laser group were respectively 8.2±0.5° and 2.8±0.5°, and the difference was statistically significant (t=22.83, P<0.001). (Figure 6)
 |
Figure 6 The box plot showed the ideal and actual trajectory deviation angle of the laser group was statistically significantly less compared to the freehand group. |
In the freehand group, there were 7 first positioning errors, while, there were 2 first positioning errors in the laser group. By comparing the failure rates of the two groups were 17.5% (7/40, the freehand) and 5.0% (2/40, the laser group), the difference was statistically significant (χ2=21.36, P<0.001), and the first success rate of the laser group was higher.
With the improvement of proficiency, the operative time was gradually shortened. Through the changing trend of learning time, it could be seen that the two groups have a gradual downward trend, but in general, the learning time of the laser group was shorter and more stable (Figure 7).
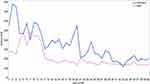 |
Figure 7 The time required for the laser group to master was shorter and more stable compared to the freehand group. |
Discussion
Although there were many solutions to the distal locking of the long bone IMs, including mechanical positioning devices22, electromagnetic navigation devices, surgical robots, Intra-medullary endo-transilluminating (iMET)23 and so on, there were still problems such as inaccurate positioning, low first success rate and long learning curve.7,24 As the freehand technique was the final solution after all the other methods failed, this study compared the effectiveness and safety of the laser device with freehand technique.7,25
According to literature, the freehand positioning of the distal locking screw takes about 7–15 minutes10. It takes more operative and radiation exposure time for novice surgeons. Repeated positioning can lead to lateral cortical defect, reduce the stability of interlocking nail and cortex, which will result in nail withdrawal and affect the surgical effect of internal fixation26. Compared with the freehand method, the laser guiding navigation device could shorten the operative time, increase the first success rate and improve the efficiency of the operation.
The criterion for the successful insertion of the distal screw was judged by the smooth passage of the screw through the nail hole. At the same time, the ideal trajectory27 was through the center of the nail hole and perpendicular to the long axis of the intramedullary nail. Due to the necessary redundancy between the screw and the nail hole, there was a certain angle deviation between the ideal trajectory and the actual trajectory, which could reflect the accuracy of positioning. The deviation angle between the ideal and the actual trajectory of the coronal plane (femoral front position) and horizontal position (femoral vertical position) was measured by the PACS system28. The deviation angle of the laser group on the coronal and the horizontal plane was smaller and the accuracy was higher.
All kinds of positioning methods need X-ray fluoroscopy to localize distal locking holes. It takes about 20–40 seconds for a surgeon skilled in freehand method to complete the distal locking of the intramedullary nail under radiation exposure. The average radiation dose to the surgeon was 1.27 mSv during the procedures of intramedullary nailing of femoral and tibial fracture29. It will take more radiation exposure time for a novice surgeon. Considering the safety of operators and patients, radiation exposure should be minimized. In this study, the radiation exposure time of the laser group was about 1/4 of the freehand group, and fluoroscopy was not necessary in the process of inserting the locking screws, which could significantly reduce radiation exposure (especially for the surgeon).
The operators in this study were all senior residents, with limited freehand experience and needed the guidance of superiors. It was difficult to master the freehand technique and a large amount of radiation exposure was unavoidable to gain experience30. The main challenge was to maintain a stable direction when the guide pin was inserted31. The learning curve chart of this study showed it took the laser group less time to be close to a stable level. In other words, this method was easier to master.
There are problems of long radiation exposure time and cortical defects in freehand techniques. After the guide pin was positioned successfully, the direction deviation may still occur during screw insertion. With the help of the laser guiding navigation device, the surgeon only needs to change the guide needle, drill and the distal screw along the laser direction, which can avoid more radiation exposure and insertion direction deviation. Other laser positioning devices previously reported could only perform body surface positioning but could not perform navigation, and were inconvenient to install and disassemble,32,33 and have poor compatibility. Other electromagnetic navigation technologies and surgical robot navigation systems were either expensive or complicated to operate, which made it difficult to popularize5. The distal locking should be as fast, accurate and low radiation exposure as possible, which can be satisfied by this device.
Strengths and Limitations
According to the results, the advantage of this device was more accurate and effective and was easy to master. But there were some limitations. First of all, this was a study invitro, which may be different from the real clinical setting. Secondly, each G-arm needed to be calibrated and adjusted in advance when it was first used. Thirdly, although the two senior residents have similar experience, there are still slight differences in surgical techniques, which may have a certain impact on the final results. Finally, the secondary damage of the laser to the surgeon’s eyes34 should be protected by wearing special protective glasses.
Conclusions
Compared with the freehand method, this device was more accurate and effective in the distal locking of the IMs. In addition, it could reduce the operative and radiation exposure time, and was easy to master. Therefore, the device has the value of popularity.
Abbreviations
TAC, track angle of coronal plane; TAH, track angle of horizontal plane; IM, intramedullary nail.
Data Sharing Statement
Please contact the author for data requests.
Ethics Approval and Consent to Participate
The study was approved by the ethics committee of Beijing Friendship Hospital. This article does not contain any studies with human participants or animals performed by any of the authors. A New Accurate, Simple and Less Radiation Exposure Device for Distal Locking of Femoral Intramedullary Nails
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This paper was supported by Beijing Municipal Administration of Hospitals Incubating Program Fundings, Code:PX2021004.
Disclosure
The authors declare that they have no competing interests.
References
1. Zhang YZ. [Current status and prospect of traumatic orthopedics treatment]. Zhonghua Wai Ke Za Zhi. 2019;57(1):19–22. Chinese.
2. Krettek C, Mannss J, Miclau T, et al. Deformation of femoral nails with intramedullary insertion. J Orthop Res. 1998;16(5):572–575. doi:10.1002/jor.1100160508
3. Chan DS, Burris RB, Erdogan M, et al. The insertion of intramedullary nail locking screws without fluoroscopy: a faster and safer technique. J Orthop Trauma. 2013;27(7):363–366. doi:10.1097/BOT.0b013e3182828e10
4. Han B, Shi Z, Fu Y, et al. Comparison of free-hand fluoroscopic guidance and electromagnetic navigation in distal locking of femoral intramedullary nails. Medicine (Baltimore). 2017;96(29):e7450. doi:10.1097/MD.0000000000007450
5. Cartiaux O, Paul L, Docquier PL, et al. Computer-assisted and robot-assisted technologies to improve bone-cutting accuracy when integrated with a freehand process using an oscillating saw. J Bone Joint Surg Am. 2010;92(11):2076–2082. doi:10.2106/JBJS.I.00457
6. Hill D, Williamson T, Lai CY, et al. Robots and tools for remodeling bone. IEEE Rev Biomed Eng. 2020;13:184–198. doi:10.1109/RBME.2019.2949749
7. Whatling GM, Nokes LD. Literature review of current techniques for the insertion of distal screws into intramedullary locking nails. Injury. 2006;37(2):109–119. doi:10.1016/j.injury.2005.09.009
8. Trotschel H. [CT-guided interventions on the spine--new laser navigation system]. Rofo. 2014;186(1):9. German.
9. Lilly RJ, Koueiter DM, Graner KC, et al. Computer-assisted navigation for intramedullary nail fixation of intertrochanteric femur fractures: a randomized, controlled trial. Injury. 2018;49(2):345–350. doi:10.1016/j.injury.2017.12.006
10. Wang Y, Han B, Shi Z, et al. Comparison of free-hand fluoroscopic guidance and electromagnetic navigation in distal locking of tibia intramedullary nails. Medicine (Baltimore). 2018;97(27):e11305. doi:10.1097/MD.0000000000011305
11. Zuo K, Qin W, Guo Q, et al. [Electromagnetic navigation interlocking intramedullary nail technology for treatment of femoral shaft fractures]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014;28(10):1204–1207. Chinese.
12. Persiani P, Gurzi M, Moreschini O, et al. Fluoroscopic freehand and electromagnetic-guided targeting system for distal locking screws of humeral intramedullary nail. Musculoskelet Surg. 2017;101(1):19–23. doi:10.1007/s12306-016-0436-x
13. Leloup T, El KW, Schuind F, et al. A novel technique for distal locking of intramedullary nail based on two non-constrained fluoroscopic images and navigation. IEEE Trans Med Imaging. 2008;27(9):1202–1212. doi:10.1109/TMI.2008.920602
14. Wattanakitkrileart S, Tangtrakulwanich B, Yuenyongviwat V. Comparing results between new aiming device and freehand technique for distal locking of intramedullary implants. J Med Assoc Thai. 2016;99(11):1180–1184.
15. Krettek C, Konemann B, Farouk O, et al. Experimental study of distal interlocking of a solid tibial nail: radiation-independent distal aiming device (DAD) versus freehand technique (FHT). J Orthop Trauma. 1998;12(6):373–378. doi:10.1097/00005131-199808000-00001
16. Marx RG, Grimm P, Lillemoe KA, et al. Reliability of lower extremity alignment measurement using radiographs and PACS. Knee Surg Sports Traumatol Arthrosc. 2011;19(10):1693–1698. doi:10.1007/s00167-011-1467-3
17. Zhu Y, Phillips R, Griffiths JG, et al. Recovery of distal hole axis in intramedullary nail trajectory planning. Proc Inst Mech Eng H. 2002;216(5):323–332. doi:10.1243/09544110260216595
18. Gao H, Zhang R, Jia C, et al. Novel placement of cortical bone trajectory screws in the lumbar spine: a radiographic and cadaveric study. Clin Spine Surg. 2018;31(6):E329–E336. doi:10.1097/BSD.0000000000000651
19. Jeong ST, Park YS, Jung GH. Computational simulation of sacral-alar-iliac (S2AI) screw fixation of pelvis and implications for fluoroscopic procedure: a cadaver study. J Orthop Surg (Hong Kong). 2019;27(1):615496534. doi:10.1177/2309499019836246
20. Anderson BD, Nordquist P, Skarman E, et al. Integrated lower extremity trauma simulator. Stud Health Technol Inform. 2007;125:19–24.
21. Vaughan N, Dubey VN, Wainwright TW, et al. A review of virtual reality based training simulators for orthopaedic surgery. Med Eng Phys. 2016;38(2):59–71. doi:10.1016/j.medengphy.2015.11.021
22. Krettek C, Konemann B, Miclau T, et al. A mechanical distal aiming device for distal locking in femoral nails. Clin Orthop Relat Res. 1999;364:267–275. doi:10.1097/00003086-199907000-00033
23. Chu W, Wang J, Young ST, et al. Reducing radiation exposure in intra-medullary nailing procedures: intra-medullary endo-transilluminating (iMET). Injury. 2009;40(10):1084–1087. doi:10.1016/j.injury.2009.04.008
24. Goulet JA, Londy F, Saltzman CL, et al. Interlocking intramedullary nails. An improved method of screw placement combining image intensification and laser light. Clin Orthop Relat Res. 1992;281:199–203.
25. Karachalios T, Babis G, Tsarouchas J, et al. The clinical performance of a small diameter tibial nailing system with a mechanical distal aiming device. Injury. 2000;31(6):451–459. doi:10.1016/S0020-1383(00)00024-3
26. Zhao X, Fan Y, Chen J. A comparison of free-hand method and electromagnetic navigation technique for the distal locking during intramedullary nailing procedures: a meta-analysis. Arch Orthop Trauma Surg. 2021;141(1):45–53. doi:10.1007/s00402-020-03456-w
27. Kaito T, Matsukawa K, Abe Y, et al. Cortical pedicle screw placement in lumbar spinal surgery with a patient-matched targeting guide: a cadaveric study. J Orthop Sci. 2018;23(6):865–869. doi:10.1016/j.jos.2018.06.005
28. Sorin G, Pasquier G, Drumez E, et al. Reproducibility of digital measurements of lower-limb deformity on plain radiographs and agreement with CT measurements. Orthop Traumatol Surg Res. 2016;102(4):423–428. doi:10.1016/j.otsr.2016.02.009
29. Muller LP, Suffner J, Wenda K, et al. Radiation exposure to the hands and the thyroid of the surgeon during intramedullary nailing. Injury. 1998;29(6):461–468. doi:10.1016/S0020-1383(98)00088-6
30. Park SM, Shen F, Kim HJ, et al. How many screws are necessary to be considered an experienced surgeon for freehand placement of thoracolumbar pedicle screws? Analysis using the cumulative summation test for learning curve. World Neurosurg. 2018;118:e550–e556. doi:10.1016/j.wneu.2018.06.236
31. Pardiwala D, Prabhu V, Dudhniwala G, et al. The AO distal locking aiming device: an evaluation of efficacy and learning curve. Injury. 2001;32(9):713–718. doi:10.1016/S0020-1383(01)00100-0
32. Choi J, Kim J, Hwang JY, et al. A novel smart navigation system for intramedullary nailing in orthopedic surgery. PLoS One. 2017;12(4):e174407.
33. Goodall JD. An image intensifier laser guidance system for the distal locking of an intramedullary nail. Injury. 1991;22(4):339. doi:10.1016/0020-1383(91)90026-B
34. Smalley PJ. Laser safety: risks, hazards, and control measures. Laser Ther. 2011;20(2):95–106. doi:10.5978/islsm.20.95
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.