Back to Journals » Pragmatic and Observational Research » Volume 10
A multicenter, open-label, noninterventional study to evaluate the impact on clinical effects, user-friendliness and patients’ acceptance of AirFluSal Forspiro in the treatment of asthma under real-life conditions (ASSURE)
Authors Backer V , Bjermer L , Refvem OK, Søderman A, Jones S
Received 9 January 2019
Accepted for publication 12 April 2019
Published 24 May 2019 Volume 2019:10 Pages 29—39
DOI https://doi.org/10.2147/POR.S200654
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor David Price
Vibeke Backer,1 Leif Bjermer,2 Olav Kåre Refvem,3 Andreas Søderman,4 Spencer Jones5
1Department of Respiratory Medicine, Bispebjerg Hospital, Copenhagen University, 48 2400 Copenhagen, Denmark; 2Department of Respiratory Medicine and Allergology, Skåne University Hospital, 221 85 Lund, Sweden; 3Lungepraksis AS, Oslo 0873, Norway; 4Medical Affairs Nordics, Sandoz AS, Copenhagen, DK-2300, Denmark; 5Global Medical Affairs, Sandoz International GmbH, Holzkirchen, D-83607, Germany
Background: The design of inhaler devices may potentially influence adherence/persistence and outcomes in asthma.
Objective: The primary objective was to assess asthma control and any change in the quality of life in patients using an intuitive dry powder inhaler containing fluticasone propionate/salmeterol (AirFluSal®, Forspiro®,) for the treatment of asthma in everyday practice.
Methods: ASSURE was a multicenter, noninterventional, open-label, prospective study in patients with asthma, aged ≥12 years and treated with the Forspiro device in Denmark, Sweden and Norway. Patients’ opinions of their asthma control were assessed by the Asthma Control Test (ACT) questionnaire and asthma-related quality of life by the Mini Asthma Quality of Life Questionnaire (miniAQLQ) at baseline and at two follow-up visits (approximately 4–8-week intervals).
Results: Of 321 patients enrolled in the study, 299 received at least one dose of fluticasone propionate/salmeterol via the Forspiro device and 204 had evaluable data at the baseline visit and at least one later visit. Patients showed improvements in asthma control and quality of life during the study. The mean sum score of ACT increased from 18.0 (SD 4.5) at visit 1 to 19.9 (4.2) at visit 2 and 20.5 (4.3) at visit 3. Overall, 38.2% of patients improved by the minimal clinically important difference (MCID) of ≥3 points (45.6% among those with a baseline score below 23 [ie, not already well controlled]). The mean score on the miniAQLQ increased from 5.16 (SD 1.24) at visit 1 to 5.58 (SD 1.20) at visit 2 and 5.82 (SD 1.04) at visit 3. Overall, 42.6% of patients improved by the MCID of ≥0.5.
Conclusion: This real-life study suggests that treatment with fluticasone propionate/salmeterol via the Forspiro device can improve asthma symptom control and quality of life.
Keywords: asthma, fluticasone propionate, salmeterol, symptom control, quality of life
Introduction
Background and rationale
Bronchial asthma is one of the most frequent chronic diseases in Western industrialized countries. Asthma is the most common chronic disease among children and affects millions of adults. It is a significant public health problem and a high-burden disease for which prevention is partly possible and treatment can be effective.1 According to World Health Organization estimates, the number of people with asthma globally is 300 million, and these numbers are expected to increase to 400 million by 2025.2 Although effective treatments for asthma are available, low adherence and persistence rates result in poor patient outcomes including symptoms, reduced quality of life, exacerbations, hospitalizations and increased mortality, as well as a substantial health care burden and high economic costs.3,4 Globally, approximately 250,000 people die annually because of asthma.5
In patients whose asthma is not controlled by regular inhaled corticosteroid alone, international guidelines recommend treatment with fixed-dose combinations of inhaled corticosteroids and long-acting beta-agonists to reduce symptoms, exacerbations, mortality and health care–associated costs in moderate-to-severe asthma.6,7 The proven combination of fluticasone propionate and the long-acting beta-agonist salmeterol (as xinafoate) is available in an intuitive dry powder inhaler device (AirFluSal® Forspiro®; Sandoz International GmbH, Germany). For successful therapy with inhaled medication, inhalation technique must be correct.8 The design of inhaler devices, in terms of ease-of-use and intuitive features that help to maintain good inhaler technique over time, may potentially influence persistence.9–11 The Forspiro device has been designed to be easy to use and to teach, to encourage consistently good inhaler technique.12 However, clinicians need to provide a clear, initial demonstration even with an apparently easy-to-use device; in addition, inhaler technique is known to deteriorate over time.13 Intuitive device design may aid a consistently good inhaler technique over the long-term, potentially promoting persistence.
Real-world data provide valuable information on the effectiveness of treatment in a much wider patient population than would be evaluated in a Phase III clinical trial program. Persistence to treatment with fluticasone propionate/salmeterol via the Forspiro device relative to another dry powder inhaler (Seretide® Diskus®; GlaxoSmithKline, Brentford, UK) has already been assessed in a large retrospective analysis of a pharmacy database, which showed greater persistence with the Forspiro device in patients with asthma and chronic obstructive pulmonary disease (COPD).14 The noninterventional study ASSURE was designed primarily to assess patients’ asthma control and quality of life while using the Forspiro inhaler device in everyday practice, for the treatment of bronchial asthma in line with its licensed indication. In addition, the study aimed to obtain information on patient acceptance and the user-friendliness of the device in real-world use.
Objectives
The primary objectives of the study were to assess change in asthma control using the self-assessed Asthma Control Test (ACT) and to assess any change in patients’ quality of life. Secondary objectives were to assess patients’ acceptance of the Forspiro inhaler and to obtain information about manipulation and user-friendliness of the device.
Material and methods
ASSURE (multicenter, open-label, noninterventional study to evaluate the impact on clinical effects, user-friendliness and patients’ acceptance of AirFluSal Forspiro in the treatment of asthma under real-life conditions) was a noninterventional, open-label, prospective study in patients enrolled by 64 centers in Denmark, Sweden and Norway. Each center could include a maximum of 20 patients. The decision to include a patient in the study was made by the treating physician. The decision to treat a patient with fluticasone propionate/salmeterol via the Forspiro device was made irrespective of the decision to include the patient in the study. The study was approved by the Swedish Ethical Review Authority, Lund University, Sweden, and the National Committee for Medical and Health Research Ethics, Norway. Ethics approval for a noninterventional study was not needed in Denmark.
Inclusion and exclusion criteria
Investigators included consecutive male or female patients aged 12 years or over (no upper age limit) if they had a confirmed diagnosis of asthma and had been prescribed fluticasone propionate/salmeterol via the Forspiro device as per the approved indication, and written informed consent was provided by the patient or their legal representative. Patients were excluded if they were being treated in another study, suffered from a respiratory disease other than asthma, had already taken part in the study, had contraindications to the use of fluticasone propionate/salmeterol or were pregnant or breastfeeding.
Study schedule
Eligibility criteria were checked and, after patients provided informed consent, the baseline examination (visit 1) was documented. Two more examinations (visits 2 and 3) were planned to be documented at intervals of approximately 4 weeks (between visits 1 and 2) and approximately 8 weeks (between visits 2 and 3). Patients could end their participation in the study at any time at their own request. At visit 3, or if the study was discontinued prematurely, additional data were collected for ending the study. The maximum observation period per patient in this study was three successive visits at intervals of approximately 4–8 weeks or approximately 3 months overall.
Data collection
Data were collected using an electronic case report form (eCRF). Data gathered from patient records included demographics (sex, age, height, weight, smoking status); medical history (comorbidities, allergies); diagnosed disease (diagnosis, date diagnosed, diagnostic procedure); ongoing or newly prescribed concomitant medication (number and names of drugs); other therapeutic measures; visits (date of visit); prescription of fluticasone propionate/salmeterol via the Forspiro device (dose strength, frequency of use); asthma symptoms, exacerbations and lung function tests (interval to use of bronchodilators, measurements, if available); patient training (using demonstration inhaler) and adverse events (AEs). Adherence to treatment (previous treatment, study treatment) was assessed by the investigator using predefined categories (<50%, 50–80%, 80–120%, >120%). AEs (whether serious or not) and unexpected events ascribable to treatment with fluticasone propionate/salmeterol via the Forspiro device were recorded.
Questionnaires
Other data were captured using patient questionnaires, which were handed out by the investigator/center and completed by the patient. The patient’s opinion on their asthma control was assessed at each visit by the validated ACT questionnaire.15 This self-administered questionnaire includes five questions on asthma control, each with five possible answers rated on a Likert scale. Each answer was assigned a specific score, and the sum of all scores, which reflected the level of patient-specific asthma control, was noted by the investigator/study center in the eCRF. A difference in the total score of 3 points or more is considered to be clinically important.15
Asthma-related quality of life was assessed at each visit by means of the validated, self-administered Mini Asthma Quality of Life Questionnaire (miniAQLQ).16 This questionnaire consists of 15 questions each with seven possible answers rated on a Likert scale. The scores were noted by the investigator/study center in the eCRF and reflected the extent to which the patient’s quality of life was restricted due to their asthma. A difference in the mean score of 0.5 points or more is considered to be clinically important.16
Patients’ acceptance of and ability to operate the Forspiro inhaler device was assessed using a product-specific patient satisfaction questionnaire (see Appendix 1). The questionnaire evaluates satisfaction with the device and the estimated effect on the symptoms of the patient’s asthma and assesses various aspects of the inhaler (eg, manipulation, size, shape of the mouthpiece) using (5-point) Likert scales and comparison with previous treatment (a 3-point Likert scale).
Final assessment
At the final visit, investigators handed out the patient satisfaction questionnaire for the assessment of patients’ satisfaction with the Forspiro device and its effect on their asthma symptoms. Both patients and investigators evaluated the technical characteristics of the inhaler (ease of use, weight, size, design and shape/ergonomics of mouthpiece). Any handling problems reported by patients were recorded.
Statistical analysis
The planned number of approximately 300 patients was adequate for identifying a change of 1.0 in the ACT total score between baseline and final visit, using assumptions of power =0.9 and alpha error =0.01.
All statistical evaluations were descriptive in nature. Demographic data, baseline characteristics, and tolerability and effectiveness data were described with summary statistics such as number, mean and standard deviation, and median and range for continuous variables. Categorical variables were described by category counts and frequencies (percentages) and could include 95% confidence intervals if applicable. The incidence of AEs and adverse drug reactions (ADRs) was calculated for events overall and by event type.
The full analysis set (FAS) comprised all patients who gave written consent to their data being recorded. The safety analysis set (SAS) included all patients who did not violate any inclusion or exclusion criteria of the study and who received at least one dose of fluticasone propionate/salmeterol via the Forspiro device. The modified FAS (mFAS) was a fraction of the FAS and included all the patients who had evaluable data at the start date (baseline visit) and at least one later visit.
Missing values were not replaced. Where information about the relationship of an AE to study drug (suspected/not suspected) was “missing”, the AE analysis was performed twice: a worst-case (ie, missing was set as “related”) and a best-case scenario approach (ie, missing was set as “not related”). Only the results of the worst-case scenario approach are reported here.
Results
Patient disposition and visits
Overall, 321 patients gave written consent to their data being recorded and thus comprised the FAS. Of these, 22 patients violated the inclusion or exclusion criteria, leaving 299 patients in the SAS. Of these, 63 patients were lost to follow-up and 46 did not have confirmed/signed documentation (with some overlap) and so the mFAS included 204 patients. The reasons for loss to follow-up are not known, but some patients were probably lost to follow-up during a prolonged period of database shutdown, and some sites were also lost during this period.
Physicians documented the initial visit (visit 1) and two follow-up visits per patient. For the 204 patients in the mFAS, data were recorded for all patients from visit 1, for 142 (69.6%) patients from visit 2 and for 178 (87.3%) patients from visit 3. The median duration between visits 1 and 2 was 33.0 (range 1–367) days, corresponding to about 1 month, and the median duration between visits 1 and 3 was 93.5 (range 55–450) days, corresponding to about 3 months.
Most patients (181; 88.7%) completed the study as planned. Twenty-three (11.3%) patients terminated the study prematurely, most frequently due to “therapy discontinuation” (n=8), “patient request” (n=5) and “lost to follow-up” (n=5). Three patients discontinued due to “lack of efficacy”, one due to “adverse events” and one due to “long-term hospitalization”.
Patient characteristics
Table 1 summarizes the demographic and baseline characteristics of the patients in the mFAS. Most patients (63.7%) were female, and the median age was 50 years. All 204 patients were diagnosed with bronchial asthma, and over half (53.4%) had allergies. Comorbidities were present in 31.4% of patients, the most common being hypertension (10.8%). Physicians assessed patient adherence to previous asthma treatment to be 80–120% in most cases (71.1%), with lower adherence (<80%) in relatively few cases (n=18). The 18 patients with “moderately reliable” or “unreliable” use of their asthma medication were asked about reasons for this. These were “lack of understanding of the therapy” (n=5), “fear of inhaled steroids” (n=5), “problems with the inhaler” (n=1) and “other” reasons (n=10; most frequently “forgotten”). Twelve (5.9%) patients were reported to have used other therapeutic measures in the 6 months before the start of the study, including “breathing physiotherapy” (n=4) and “physical training” (n=3).
 | Table 1 Demographics and baseline characteristics of patients in the modified full analysis set (n=204) |
Study treatment
At the initial visit, 130 (63.7%) patients were prescribed treatment with fluticasone propionate/salmeterol via the Forspiro device at a dose of 250 µg/50 µg and 74 (36.3%) at the higher dose of 500 µg/50 µg. These proportions remained largely the same at the two follow-up visits. The clear majority of patients (196 [96.1%] at the initial visit) used the inhaler twice daily throughout the study.
About one-third of patients (69; 33.8%) had not received any concomitant medication (ongoing and/or newly prescribed) during the previous 6 months or during the study. Forty-six (22.5%) patients received one concomitant medication, 33 (16.2%) received two, 21 (10.3%) received three, and 35 (17.2%) received four or more concomitant drugs. The median number of concomitant medications was 1.0 (range 0.0–14.0).
Asthma symptoms, lung function and exacerbations
The frequency of daytime symptoms decreased during the study, with the proportion of patients experiencing daytime symptoms more than twice per week decreasing from 38.7% at visit 1 to 20.8% at visit 3. Likewise, the proportion of patients who felt restricted in their day-to-day activities decreased from 52.5% to 28.7%. The proportion of patients reporting night-time symptoms also decreased (from 41.2% to 21.9%), as did those requiring relief/rescue medication more than twice per week (from 38.7% to 25.3%).
Over half of the patients (51.5%) presented with normal lung function (peak expiratory flow or forced expiratory volume in 1 s) at the initial visit, which hardly changed at the two follow-up visits (51.4% and 52.2%). Low lung function (<80% predicted) was found in 28.9% of patients at visit 1, 16.2% at visit 2 and 18.5% at visit 3. Lung function examinations were not performed in 40 (19.6%) patients at visit 1, 46 (32.4%) at visit 2 and 52 (29.2%) at visit 3.
Exacerbations in the previous 12 months were reported at the initial visit in 22.1% of patients. The proportion of patients with exacerbations since the previous visit decreased from 8.5% at visit 2 to 5.6% at visit 3. The median number of exacerbations was 1.0 at each visit, with a maximum of 6.0 at visit 1, 5.0 at visit 2 and 3.0 at visit 3).
Patient questionnaires
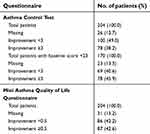
Patients completed the ACT at each visit to evaluate the impact of their asthma medication on symptoms over the previous 4 weeks. Patients showed an improvement of asthma control during the study, as the mean sum score of ACT increased from 18.0 (SD 4.5) at visit 1 to 19.9 (SD 4.2) at visit 2 and 20.5 (SD 4.3) at visit 3 (Figure 1). Overall, 38.2% of patients improved by the minimal clinically important difference (MCID) of ≥3 points (Table 2). However, among patients with a baseline score below 23 (that is, those whose asthma was not already well controlled), the proportion with a ≥3-point improvement was 45.6%.
 | Table 2 Improvement in patient questionnaires in relation to minimal clinically important difference |
 | Figure 1 Changes in scores on patient questionnaires over the course of the study. |
Patients completed the miniAQLQ at each visit to evaluate their health-related quality of life. Patients showed an improvement in the quality of life during the study, as the mean score on the miniAQLQ increased from 5.16 (SD 1.24) at visit 1 to 5.58 (1.20) at visit 2 and 5.82 (1.04) at visit 3 (Figure 1). Overall, 42.6% of patients improved by the MCID of ≥0.5 (Table 2).
Correct inhaler use and adherence
At the initial visit, the investigator showed the patient how to use the Forspiro device correctly using a demonstration inhaler. The investigator then asked the patient to use the inhaler and documented whether the patient could reproduce the correct inhaler technique (yes/no). If the patient did not show the correct inhaler technique at the follow-up visits, the demonstration was repeated and the patient’s next attempt documented. At each visit, more than 98% of patients demonstrated the correct inhalation technique. About a third (n=62; 30.4%) of patients received additional training materials at the initial visit, with 7% (10/142) and 10.1% (18/178) receiving such materials at visits 2 and 3, respectively. These materials included brochures, a booklet on inhalation technique and written guidance.
Investigators evaluated treatment adherence during the study to be 80–120% in most patients (148; 72.5%) and >120% in 35 (17.2%). Adherence was judged to be better with the study device than with previous therapy in 64 (31.4%) patients, the same in 91 (44.6%) and worse in 6 (2.9%).
Continuation/evaluation of treatment
Most (163; 79.9%) patients continued therapy with the study device at the final assessment; 36 (17.6%) did not continue treatment, and treatment continuation was unknown for 5 patients (2.5%). The most frequently given reason for not continuing treatment was “patient request” (16; 44.4%). Over half of the patients (111; 54.4%) evaluated their degree of asthma control as “improved”, 37.3% (n=76) patients said that it was unchanged and 5.9% (n=12) reported that it had “worsened”. Most patients (~80%) evaluated the efficacy and tolerability of fluticasone propionate/salmeterol via the Forspiro device as “good” to “very good”, with fewer patients assessing treatment efficacy/tolerability as “moderate” or “poor” (Table 3). Only 11 (5.4%) patients reported persistent handling problems with the device.
 | Table 3 Patients’ evaluation of efficacy and tolerance of fluticasone propionate/salmeterol therapy via the Forpiro inhaler (n=204) |
Final patient and physician assessment
Almost three-quarters (152; 74.5%) of patients were satisfied with the Forspiro device and 14.7% (n=30) were not satisfied. About half (95; 46.6%) of patients assessed their symptoms as “improved” and 76 (37.3%) as “not changed” due to the study treatment. A minority of patients (11; 5.4%) assessed their symptoms as “worsened”. Patient satisfaction questionnaire data were missing for 22 (10.8%) patients.
The technical aspects of the device (ease of use, weight, size, design and shape/ergonomics of mouthpiece) were evaluated as “good” to “very good” by more than 60% of patients and more than 65% of investigators. Ninety (44.1%) of patients assessed the ease of use as “very good”, with a further 73 (35.8%) assessing it as “good”. Only 4 (2.0%) and 3 (1.5%) patients assessed ease of use as “poor” or “very poor”, respectively.
Over two-thirds of patients (140; 68.6%) found that the Forspiro device helped them to adhere to the prescribed treatment, while 16.2% (n=33) found that it did not help to increase their adherence. Almost all (48/49; 98%) of the investigators indicated that they would continue to prescribe fluticasone propionate/salmeterol via the Forspiro device for suitable patients.
Adverse events
Fifty-five (18.4%) patients experienced 73 nonserious AEs, which were not related to the study medication during the observational period (Table 4). Patients recovered completely from 71.2% (n=52) of the nonserious AEs and recovered with sequelae in 8.2% of the events (n=6). None of the nonserious AEs worsened.
 | Table 4 Adverse events and adverse drug reactions |
Two (0.7%) patients experienced four serious AEs, which were not thought to be related to the study drug. One of these patients recovered completely, and in one patient, the SAE was ongoing. These four non-related serious AEs were epilepsy in one patient, and paresthesia and two events of oral hypoesthesia in the other patient.
Discussion
This multicenter, open-label, noninterventional, prospective study suggests that treatment with fluticasone propionate/salmeterol via the Forspiro device improved asthma symptom control and quality of life in a real-world setting. Of 204 patients in the mFAS population, most (54.4%) reported improvements in asthma control, with 37.3% reporting no change in control. Among patients whose asthma was not already well controlled at baseline, 46% achieved a clinically important improvement on the ACT questionnaire. In addition, the quality of life as assessed with the miniAQLQ improved by at least the minimally importance difference in 43% of patients. Patients were very likely to persist with the treatment, with 79.9% still using the device at the end of the study. Adherence to treatment was also high, with 89.7% of patients having adherence levels of at least 80%. Patient satisfaction with treatment was high (74.5% satisfied), with many patients (68.6%) indicating that the Forspiro inhaler device helped them adhere to treatment.
Treatment was efficacious in this heterogeneous asthmatic population, as indicated by a sustained decrease in symptoms. Most patients (78.4%) evaluated the efficacy of treatment as good or very good.
Device design, in terms of ease-of-use and intuitive features that help to maintain good inhaler technique over time, can potentially influence treatment adherence and persistence, which in turn could support better asthma outcomes in terms of disease and symptom control and quality of life.8,9,11 Real-world data provide valuable information for practicing physicians in a broad patient population. The results reported support the real-world acceptability of the Forspiro device, in that most patients (60%) and physicians (65%) evaluated the technical aspects of the device as either good or very good.
Fluticasone propionate/salmeterol via the Forspiro device was well tolerated in a heterogeneous patient population, with 82.8% of patients evaluating tolerability as good or very good. This is reflected by the low incidence of adverse events and ADRs.
Limitations
This was an open-label, noninterventional study design with no control group. Noninterventional studies may suggest correlations between clinical effect and therapy; however, they cannot establish cause and effect. No tests of statistical significance were performed.
The findings of this study are representative of a heterogeneous asthmatic patient population comprising a wide age range and various comorbidities and allergies. More than half of the patients were receiving concomitant medication for their asthma, which could confound the results. In addition, patients received training in the use of the Forspiro inhaler device, which may have contributed to the improvements in symptom control and quality of life seen.
Comparison with other studies
Two observational studies in Poland and Germany looked at the characteristics of reliever inhalers. One study in 263 adult/adolescent patients with asthma and 115 with COPD, as well as 164 children with asthma, examined usage and usability of a particular dry-powder inhaler (Easyhaler®; Orion Pharma, Finland) compared with other inhalers.17 Inhaler usage, patient satisfaction, compliance and patients’ assessments of usability were better with the Easyhaler than with the other inhalers. As in the current study, physicians considered inhaler technique to be poor in very few patients (5/378 adults/adolescents), with inhaler handling being mostly rated good or very good, and most patients (63.8%) receiving only one demonstration of inhaler technique. The other study looked at asthma control (according to Global Initiative for Asthma criteria for controlled, partly controlled and uncontrolled asthma) in 16,844 patients treated with a beclomethasone and formoterol combination pressurized metered-dose inhaler.18 After 6 months of therapy, asthma control improved in 74.2% of patients, which is a larger proportion than seen in the current study (38.2% improved by the MCID of ≥3 points on the ACT; 45.6% among those with a baseline score below 23). The authors noted that training of patients in the correct inhaler technique was an important factor in improving treatment outcomes.
Conclusion
Effective treatments for asthma are available, but poor inhaler technique, lack of adherence and low persistence may result in poor patient outcomes including asthma symptoms, reduced quality of life, exacerbations, hospitalizations and increased mortality, as well as burden on health care systems and high economic costs. This real-world study suggests that treatment with fluticasone propionate/salmeterol via the Forspiro inhaler device may improve asthma symptom control and quality of life, as well as positively contributing to good adherence and persistence to treatment. Patient satisfaction with treatment, correct inhaler technique and motivation to continue using an inhaler device are likely to be interrelated factors that influence the success of asthma treatment in everyday practice. Accepting the limitations of this type of study, these new data provide evidence that treatment with fluticasone propionate/salmeterol via the Forspiro inhaler device may play a valuable role in improving asthma outcomes in a real-life setting.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Swedish Ethical Review Authority, Lund University, Sweden, and the National Committee for Medical and Health Research Ethics (NEM), Norway. Ethics approval for a non-interventional study was not needed in Denmark.
Informed consent
Written informed consent was obtained from all individual participants included in the study or their legal representative.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
Medical writing assistance was provided by Synergy Medical Communications. Project management, data management, and statistical analysis was performed by Institut Dr. Schauerte, Munich, Germany. A full list of participating investigators is available on request from the corresponding author. The study was funded by Sandoz International GmbH. The funder was involved in study design; in the analysis and interpretation of data; in the writing of the report and in the decision to submit the article for publication. Medical writing assistance was also funded by Sandoz International GmbH.
Author contributions
Vibeke Backer, Leif Bjermer and Olav Kåre Refvem were coordinating investigators for Denmark, Sweden and Norway, respectively. All authors made substantial contributions to the conception or design of the work; or the acquisition, analysis or interpretation of data for the work. All authors were involved in drafting the work or revising it critically for important intellectual content, and all gave final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
Andreas Søderman is an employee of Sandoz AS. Spencer Jones is an employee of Sandoz International GmbH and holds stock in Novartis. Leif Bjermer reports honoraria from ALK, Airsonette, AstraZeneca, Boehringer, Chiesi, GlaxoSmithKline, Novartis, Teva, outside the submitted work. Olav Kåre Refvem reports personal fees from Boehringer-Ingelheim, outside the submitted work, and is the owner of Lungepraksis AS. The authors report no other conflicts of interest in this work.
References
1.
2. Pawankar R. Allergic diseases and asthma: a global public health concern and a call to action. World Allergy Organ J. 2014;7(1):12. doi:10.1186/1939-4551-7-12
3. Thomas M. Why aren‘t we doing better in asthma: time for personalised medicine? NPJ Prim Care Respir Med. 2015;25:15004. doi:10.1038/npjpcrm.2015.4
4. Mäkelä MJ, Backer V, Hedegaard M, Larsson K. Adherence to inhaled therapies, health outcomes and costs in patients with asthma and COPD. Respir Med. 2013;107(10):1481–39. doi:10.1016/j.rmed.2013.04.005
5.
6. Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343–373. doi:10.1183/09031936.00175113
7.
8.
9. Virchow JC, Crompton GK, Dal Negro R, et al. Importance of inhaler devices in the management of airway disease. Respir Med. 2008;102(1):10–19. doi:10.1016/j.rmed.2008.04.008
10. Lavorini F, Braido F, Baiardini I, Blasi F, Canonica GW;
11. Chogtu B, Holla S, Magazine R, Kamath A. Evaluation of relationship of inhaler technique with asthma control and quality of life. Indian J Pharmacol. 2017;49(1):110–115.
12. Jones S, Weuthen T, Harmer QJ, Virchow JC. Assessing the intuitive ease of use of a novel dry powder inhaler, the Forspiro™ device, for asthma and COPD [abstract]. Thorax. 2012;67(Suppl 2):A66–A67. doi:10.1136/thoraxjnl-2012-201768
13. Lavorini F. Inhaled drug delivery in the hands of the patient. J Aerosol Med Pulm Drug Deliv. 2014;27(6):414–418. doi:10.1089/jamp.2014.1132
14. Bender BG, Hernandez Vecino RA, McGrath K, Jones S. Comparative analysis of persistence to treatment among patients with asthma or COPD receiving AirFluSal Forspiro or Seretide Diskus salmeterol/fluticasone propionate combination therapy. J Allergy Clin Immunol Pract. 2016;4(5):884–889. doi:10.1016/j.jaip.2016.07.006
15. Schatz M, Kosinski M, Yarlas AS, Hanlon J, Watson ME, Jhingran P. The minimally important difference of the Asthma Control Test. J Allergy Clin Immunol. 2009;124(4):719–723. doi:10.1016/j.jaci.2009.06.053
16. Juniper EF, Guyatt GH, Cox FM, Ferrie PJ, King DR. Development and validation of the Mini Asthma quality of life questionnaire. Eur Respir J. 1999;14(1):32–38.
17. Hantulik P, Wittig K, Henschel Y, Ochse J, Vahteristo M, Rytila P. Usage and usability of one dry powder inhaler compared to other inhalers at therapy start: an open, non-interventional observational study in Poland and Germany. Pneumonol Alergol Pol. 2015;83:365–377. doi:10.5603/PiAP.2015.0059
18. Kuna P, Kupryś-Lipińska I, Dębowski T. Control of asthma in adults treated with beclomethasone and formoterol in extrafine particle formulation in a real-life setting in Poland: the CASPER noninterventional, observational trial. Pol Arch Med Wewn. 2015;125:731–740.
Supplementary materialAppendix 1: ASSURE patient satisfaction questionnaire
 |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
