Back to Journals » Advances in Medical Education and Practice » Volume 13
A Mixed Methods Assessment of the Management Role of Physicians
Authors Rechtien L, Gradel M, Fischer MR, Graupe T, Dimitriadis K
Received 24 April 2022
Accepted for publication 4 August 2022
Published 8 September 2022 Volume 2022:13 Pages 1003—1017
DOI https://doi.org/10.2147/AMEP.S370245
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Laura Rechtien,1,2 Maximilian Gradel,1 Martin R Fischer,1 Tanja Graupe,1 Konstantinos Dimitriadis1,3
1Institute of Medical Education University Hospital, Ludwig Maximilian University of Munich, Munich, Germany; 2Department of Dermatology, Friedrich-Alexander-University of Erlangen-Nuremberg, Erlangen, Germany; 3Department of Neurology, Ludwig Maximilian University of Munich, Munich, Germany
Correspondence: Konstantinos Dimitriadis, Email [email protected]
Introduction: Physicians are increasingly confronted with new requirements in their daily job, which go beyond the mere treatment of patients. The aim of this Mixed-Method-Study is to better understand management as it relates to physicians’ daily work, to clarify the physicians’ perception of their management role and to examine physician’s self-assessed competence in these functions.
Methods: We used three different instruments: Semi-structured interviews, a self-assessment survey and direct observations to evaluate managerial activities performed by residents. Both latter were based on instruments established for management research.
Results: Interviewed residents were familiar with the term “Management” but had difficulties in defining it. Concerning managerial functions in context of their daily work, we identified three main categories: Self-management, Patient-management and Management of the ward. In this context, physicians named numerous examples of management tasks and for which they felt ill prepared. Eighty-eight residents participated in the self-assessment survey and rated the majority of the management tasks as necessary for the residents’ work. Although physicians estimated the proportion of managerial work to comprise only 40.6%, a much higher number of mere management tasks could be identified through direct observations (n = 12). Activities related to management were more often observed than genuine physician tasks.
Discussion: This study illustrates the prominent role of management activities in context of the residents’ work, while at the same time showing that residents do not feel sufficiently educated, prepared nor competent in management tasks.
Keywords: medical curriculum, medical education, physician’s leadership, physician’s managerial skills, physician’s manager role
Introduction
Technological progress, demographic development and expensive new treatments pose major challenges for most western health-care systems. Higher efficiency is necessary in order to sustain those health-care systems and improve quality of care. Physicians play a central role in optimizing a health-care systems’ performance by influencing the quality and quantity of care provided.1–3 Within the German health-care system, the gatekeeper’s role is attributed to physicians. This way they control patient’s access to health services4,5 and thus their management skills exert a direct influence on the costs of the health-care system. In addition, defining more efficient processes during hospitalization of patients can influence quality of care. For example, by reducing time to initiate targeted diagnostics, appropriate therapy might be started sooner, influencing health outcomes.1 Therefore, administrative and managerial tasks greatly influence physicians’ efficiency and thus quality of care.2,3 In order to achieve these goals, physicians perform, next to genuine medical activities, organizational and economic tasks. For example, organization of adequate accommodation for patients during their stay, coordination of the sequence of various diagnostic measures and efficient use of scarce resources are part of the everyday professional life of physicians.6
The long-standing consensus within management theory highlights that management is a universal feature of every undertaking, as described by Malik:
The organ of leadership in every institution of society – in enterprises as well as in universities, in hospitals or in every other organisation. [Malik 2013, p. 6]
Additionally, management has an institutional and a functional component. The institutional component focuses on the structural-personal level in industries, while the functional component concentrates on operations which influence the task management of organisations.7 Henri Fayol, the initiator of the first general theory of management, focused on the functional aspect of management, and defined the primary functions of management as: forecasting, planning, organizing, commanding, coordinating and controlling.8 Henry Mintzberg, a leading management thinker and co-creator of the study program “International Masters of Health Leadership” mainly represents the institutional view of management and defined ten managerial functions: Figurehead, Leader, Liaison, Monitor, Disseminator, Spokesperson, Entrepreneur, Disturbance handler, Resource allocator and Negotiator.9
While business economists are particularly prepared for management activities as part of their training, there are no management trainings in medical curricula for undergraduate studies and only a few residency programs, which offer comparable teachings.10–15 So far, the German medical curriculum has focused on imparting knowledge in patient care, ethics and health economics.16 Since administrative and management tasks have a major influence on the efficiency and quality of medical care for patients, physicians should be prepared accordingly for these tasks and functions.
There is less consensus, however, about what exactly management is and entails in a medical setting. A relevant perspective for medical educators used globally is represented by the “Canadian Medical Education Directives for Specialists (CanMEDS) Physician Competency Framework” from the Royal College of Physicians and Surgeons of Canada.17 In 2005, they defined the “manager role” among six key competencies:
As managers, physicians are integral participants in healthcare organizations, organizing sustainable practices, making decisions about allocating resources, and contributing to the effectiveness of the healthcare system. [Frank 2005, p. 17]
In 2015, the framework was updated and the term “manager” was replaced with “leader”.18 This change was made to better emphasize the leading role that physicians hold in addition to their managerial functions.18 The definition of this leader role from the 2015 framework, however, still includes aspects related to their managerial role, including administration, leading of personnel, organising, structuring, budgeting, financing, priority-setting, supervising others and time management.19 The CanMEDS Framework 2005 was evaluated in several studies20,21 and often used for the development of new educational programs promoting physicians’ learning and applying managerial skills.22–24 Apart from the CanMEDS Framework, there are other frameworks aiming to develop competencies among physicians for dealing with contemporary challenges associated with their managerial role such as the “Nationaler Kompetenz-basierter Lernzielkatalog Medizin (NKLM)”25 in Germany, the ACGME Competency-Based Residency Education in the US26 or the AoMRC and the NHS Institute for Innovation and Improvement Medical Leadership Competency Framework in the UK.27 There are hardly noticeable differences in the definition and learning objectives of the mentioned competencies-frameworks concerning the management role of physicians.
Nevertheless, a study evaluating the CanMEDS Framework showed that medical students least identify with the manager role and valued managerial competency lower than the other roles of the framework.28
There is a recognizable discrepancy between the manager role defined by physicians’ competency frameworks and leading management definitions. While the manager role of the here mentioned frameworks only focusses on the allocation of resources and the effectiveness of health care, leading management definitions concentrate on general managerial functions like planning, organizing, controlling or representing the role of a leader, a spokesperson or a disturbance handler. We hypothesized that physicians, even in their early career, carry out a number of managerial tasks as defined by Fayol and thus this discrepancy might explain why students mostly do not feel prepared to take on the role.29–33
The aims of this study were: 1. to characterize management functions in physicians’ daily work, 2. to contrast these with management functions as defined by business and management literature (based on Fayol and Mintzberg) in order to identify overlapping aspects and 3. to examine physician’s self-assessed competence in these functions.
Materials and Methods
To examine in how far residents are confronted with managerial work in their clinical everyday work, a Mixed-Method-Study was undertaken from November 2016 to March 2018. The Mixed-Method-Study was characterized by an equal-status (qualitative and quantitative methods have equal value), dependent and therefore sequential mixed design. For this purpose semi-structured interviews, self-assessment surveys and direct observations were carried out (Figure 1).
 |
Figure 1 Study design. |
As a first inductive step, we performed semi-structured interviews with residents in order to identify and characterize management tasks in physicians’ daily work and explored their perception for management. Using the results of this qualitative part, we adapted the questionnaires and observations’ sheets for the next two parts. In a next deductive part, a self-assessment survey was undertaken to quantify the subjective notion. In a final deductive step, direct observations were applied to objectively collect qualitative data regarding managerial activities performed by residents as part of their daily work (Figure 1).
Semi-Structured Interviews
Semi-structured interviews were conducted to collect qualitative data regarding the physicians’ notion of managerial tasks as part of their profession. In preparation for the interviews, a guideline of 23 open questions was prepared concerning residents’ daily management activities on the ward. The first questions were designed to be broad and explore the physician’s perception of management in their daily work setting. The second part included more narrow questions based on business management literature functions. At the beginning of the interview, the residents were invited to define management and to depict their notion of management as part of their daily work. Therefore, they were asked to give examples (if applicable) out of their daily work reflecting the management functions of Fayol and Mintzberg. Additionally, next to demographic data, residents were asked about their perceived management competence, their opinion on what extent this competence affects patient care, and whether further education on the topic would be appropriate. The questions were developed and reviewed by the two researchers PD Dr. Konstantinos Dimitriadis (Neurologist) and Laura Rechtien (medical student). Then they were proofed of perspicuity by a resident and a medical student before interviews were done. All 628 residents of the University Hospital of the LMU received an email containing the study content and the invitation to participate in interviews through an email distributor of the human resource management of the LMU Munich. Of these, 18 residents (male: 66.7%; female: 33.3%; mean age: 30.1 years; 6 different specialties) declared their willingness to take part in the study by providing an email consent. After nine interviews had been carried out, no new categories were identified, so that further interviewees were not recruited due to saturation of data.
The interviews were carried out by Laura Rechtien at the residents’ workplace and took 25–45 minutes depending on the detail of the residents’ answer and in how far the resident was able to give examples to the questioned management functions. The interviews were fully recorded, transcribed and anonymized. The data evaluation was carried out through the deductive application of categories according to Grounded theory.34 Grounded theory is a method of qualitative content analysis and represents a text-analytical measure that enables the systematic structuring of a text. Data is analyzed using key terms and thus systematized and interpreted with regard to certain content of meaning.35 The taxonomies according to Fayol8 and Mintzberg,36 which were already part of the questionnaire, acted as pre-existing categories. In addition, two researchers (Maximilian Gradel and PD Dr. Konstantinos Dimitriadis) independently formed categories, discussed them and jointly made the selection for the categories used in the evaluation. “MAXQDA”, software for computer-aided text analysis, was used to support this process by allowing a better organization of text and more transparent coding.37
Self-Assessment Survey
The self-assessment survey was applied as a quantitative instrument to collect subjective data from the residents concerning relevance and perceived competency of managerial activities.
A modified version of a validated self-assessment instrument from Yukl and Nameroff, the “Managerial Behavior System-Instruments”, was used.38 The questionnaire has mainly been used to give feedback to managers but has also been applied for self-assessment, and is validated in both contexts.39,40 In order to use it as a self-assessment instrument for residents, the instrument was adapted and translated into German. This modified version was not validated but was already used in a previous study.41 In addition, we extended the instrument by adding a second part based on the taxonomies of Fayol and Mintzberg. Specifically, apart from the included managerial tasks defined by Yukl and Nameroff, other functions defined by Fayol and Mintzberg were added. We chose to use both taxonomies since the first one represents more the functional aspects and the second one more the institutional part of management. Preliminary work showed that physicians have difficulties defining “Management” or “Managing”.41 We therefore hypothesized that physicians would underestimate the amount of management tasks they perform in daily work. In order to look into that, we asked them to estimate the “management amount of their daily work” before continuing with questions on the different taxonomies. We then repeated the same question at the end of the questionnaire in order to see if awareness on management issues changed the initial estimation. In order to assess whether the questions regarding different management taxonomies changed their awareness, we conducted a two-sided t-test, comparing the values from each time point.42 All functions were rated with regard to the importance within the resident’s daily work on the ward. A five-point Likert-scale was used as the rating scale, in which the steps were defined as: 1 = “irrelevant” 2 = “less important” 3 = “important” 4 = “very important” 5 = “absolutely essential”. Additionally, the managerial activities defined by Fayol and Mintzberg were assessed regarding the residents’ own competency. For this, a five-point Likert-scale was used with the following definitions: 1 = “incompetent” 2 = “rather incompetent” 3 = “rather competent” 4 = “competent” 5 = “very competent”. To check that survey respondents would understand the instrument, an informal “Think Aloud”43 exercise was performed in order to check for clarity of the translation and new elements of the questionnaire. Slight changes were implemented after the first “Think Aloud” exercise of a resident with a medical research student of our team. No further changes emerged through further exercises. The 628 residents of the LMU Munich received an email including the link to the online self-assessment survey through an email distributor of the human resource management. Of the 88 participating residents a total of 54 completely filled out the questionnaire, so that only these were taken into account in the analysis. The online self-assessment survey was created by the use of LimeSurvey and neither name, email or other personal information were asked or saved nor did the IP-address. In conclusion, all data were collected anonymously. For each category, the values of mean (M) and standard deviation (SD) were calculated. For the statistical analysis Excel 2010 was utilised.
Direct Observation
The method of direct observation is used for the more precise investigation of processes, properties and behavior.44 The advantage of observations is that with this survey method, the data on the work processes are collected in reality and the information recorded is not based solely on the subjective assessment of study participants.44 Thus, the direct observations were used as a mixed qualitative and quantitative instrument to verify or falsify the results from the two previous instruments. Due to the fact that there is no pre-existing measurement tool for the observation of physicians from a managerial point of view we needed to take a documentation form used in business field.45 We chose the “Leadership-Observation-System” (LOS) by Luthans and Lockwood46 because firstly it has been validated and secondly it already obtained reliable results in a master thesis which used LOS for the documentation of performed management functions by residents.41,45 The LOS was developed based on a 440 hours observation of business managers during their daily work. It consists of twelve main-categories with four to ten sub-categories comprising the different management activities.47 Since most of the core management functions described by Fayol and Mintzberg were evaluated as essential for physicians’ daily work, and since LOS uses a similar taxonomy for management activities we considered LOS an appropriate measurement for identifying and quantifying management tasks among physicians. The instrument already obtained reliable results in a past study.41 LOS was developed for managers; thus, every activity of daily work could be allocated to one of its categories. In contrast, physicians perform “genuine physicians tasks” in addition to management tasks.48,49 For a complete representation of the residents’ various activities and a gapless documentation of the residents’ working day the LOS was modified in regard to the addition of the genuine physician tasks.48,49 According to the “Federal Master Treaty of Medical Practitioners” (Bundesmantelvertrag-Ärzte) the genuine physician tasks include: history taking, defining indication, patients’ examination including invasive diagnostic services, diagnose, patients’ education, decision of therapy, surgical intervention, drug application and wound care as well as dressing.48 Moreover, the “German Medical Association” (Bundesärztekammer) suggests wound control and the taking of blood samples as two more genuine physician activities.49 In conformity with the defined genuine activities, the university medical program focuses on the education of medical treatment through training in medical knowledge, patient consultation, therapeutic approaches and techniques of examination.16
Residents in their first years were followed by trained observers during their whole working day for a whole working week (Monday to Friday). Observers used a prefabricated adaptation of the LOS documentation-sheet including all mentioned categories to document their observations. They were advised to put down how often a mentioned activity occurred within the last hour. Originally, documentation was performed every 10 minutes. However, preliminary work testing different time frames showed that hourly documentations were sufficient.41
We chose to use the final year medical students assigned to each of the observed wards as observers. The reasons for this were: 1. Their participation in daily routine of the ward, 2. Their proximity to the observed physician, 3. Their sufficient medical training status in order to be able to recognize genuine medical tasks, and 4. Avoidance of confidentiality issues concerning sensitive patients’ information, that any other observer would not be allowed to overhear. All future sub-interns (for the defined time period) of the LMU received an email including a brief introduction of the study and the offer to participate as an observer. The final year students (sub-interns) who had declared their willingness to participate (n = 12) took part in the study as observers. One week before the observations started, the participating sub-interns had to attend a training course in which the study hypothesis and the method of direct observation were presented. After a short introduction, most of the training comprised practical exercises with the help of short films showing residents working on a ward.50 During these short films, students documented the observed activities using the documentation-sheet. Exercises were followed by a feedback session with sufficient discussion to clarify occurred difficulties. Training was considered as completed when students achieved a sufficient overlap of their observations with the model solution.
During the observation week, observers had the opportunity to call for advice on the documentation at any time.
In addition, they received a corresponding list of examples for each category next to the prefabricated documentation-sheet. Table 1 pictures an excerpt of the list of examples. The main category “Exchanging routine information” (with the subcategories a-e) is one out of twelve main categories of the modified version of the LOS and is shown as an example. For instance, the managerial sub-category “a) answering routine procedural questions” could be represented in the residents’ working day through ward consultations.
 |
Table 1 Excerpt of the List of Examples |
Before the observation started observers informed the residents about the planned observation and the study content.
Twelve residents of different specialties, including internal medicine, surgery and neurology, were observed for five days from Monday through Friday throughout their entire workday. At the end of every working-hour the student wrote down the observed activities of the past hour. The survey was performed as a one-to-one observation, meaning that every final year student observed one resident. Once the observation was completed, the final year students returned the paper-based documentation forms personally to the authors of this study.
After a one-week observation with hourly documentation, the number of observed activities was summed up separately for each main-category and expressed in a percentage to illustrate a relative frequency among the main-categories with the use of Excel. The results of the main-categories were subsumed in four management fields in line with the description of Luthans.45 For these, the absolute as well as the relative frequency was calculated and compared to the number of genuine physician tasks.
Ethical Considerations
The Institutional Ethics Committee of the Faculty of Medicine of the LMU Munich waived approval for this study. The reason for that was a complete anonymized collection of data. Interview audio data and any personal information were irreversibly deleted in the transcription process. The participants informed consent included publication of anonymised responses. No personal information was documented within the online survey. Sub-interns (already part of the team) did the observation without documenting personal data of the observed physicians. It was therefore not possible to trace back to the participating physicians in the data analysis. The participation of the residents and the medical students was voluntary. In course of the Direct Observations, the students obtained a reward of 25€. None of the participating residents did. All participating residents and students received a full explanation of the study goals and procedures.
Results
Semi-Structured Interviews
In total 9 residents (male: 66.7%; female: 33.3%) of different specialties including Internal medicine, Surgery, Pediatrics, Psychiatry, Neurology and Anesthetics participated. The mean age of the participants was 30.1 years (27–35 years). The average year of residency was 3.6. None of them had a management qualification or a university degree in management, but four of them had participated in SiGma,51 a managerial skills training for physicians at the LMU, during their studies.
In the beginning, the interviewees were asked to define “Management”. Although all participants were familiar with the term, they had difficulties in defining it. Only with some support by the interviewer the participants did attempt to define management. Their proposed definitions comprised only two aspects: “Coordination” and “Organisation” (“To coordinate the ward and the people working on it” (participant (p) 1, female (f), 30 years (y)), “coordination of patients and procedures” (p2, f, 27y) and “coordination of processes on an administrative level” (p3, male (m), 33y), “organisation of tasks and people who should accomplish these” (p4, m, 30y)).
In evaluating their responses to questions about managerial functions in context of their daily work, we identified three main categories.
1. Self-management: “During the first half of my workday I’m busy with planning and during the other half I put the plan into action.” (p1, f, 30y), “You need to monitor yourself by using checklists”. (p4, m, 30y), “I try to handle different working procedures until a certain time, so I have an adequate amount of time for the next processes”. (p5, m, 29y)
2. Patient-management: “You have to arrange that everything is managed for the discharge. If a patient’s discharge is planned I check that all still needed diagnostic procedures are done scheduled in time”. (p6, f, 28), “Planning the sequence of diagnostic and therapeutic procedures”. (p3, m, 33y).
3. Management of the ward: ” […] “planning of bed vacancies” nonstop, the whole day.” (p7, m, 28y), “As a resident you do not have officially the power to command but actually you instruct nurses, students, patients and other residents”. (p4, m, 30y), “I have to monitor the nurses. Of course I have to check if all of my instructions have been followed”. (p6, f, 28y)
Concerning the predefined questions on management functions, physicians named numerous examples of functional management aspects defined by Fayol8 (Table 2). In contrast, with regard to the more institutional management aspects defined by Mintzberg,36 residents had difficulties finding examples for most of the functions (Table 3). Residents were able to come up with examples for only three roles (“Disseminator”, “Disturbance handler” and “Negotiator”). When asked for other roles defined by Mintzberg residents either replied: “No, this is not part of my job” (p4, m, 30y), or gave examples that were not related to the role (for the role “Liaison”): “As a resident I need to coordinate all procedures of a new incoming patient, therefore I’m well connected with the team of the other wards”. (p2, f, 27y)).
 |
Table 2 Fayol’s Managerial Functions |
 |
Table 3 Mintzberg’s Managerial Roles |
No interviewed resident felt adequately educated for managerial activities: “Competency? I am still practicing. Adequately educated? No way!” (p6, f, 28y), “Today I did a lot of things like organising, planning. Actually things I didn’t learn during my studies, but which are part of my daily work on the ward”. (p6, f, 28y)”, The organisation failure on the wards is consistently immense and it is caused by a huge helplessness of all actors”. (p3, m, 33y).
The interviewees assume that they would benefit from management trainings:
I think you would benefit from an additional training for sure. I think ‘Organisation’ would be the most important because ‘Organisation’ and ‘Planning’ on the ward are exactly the activities the residents have to be able to do from the very first day. [p2, f, 27y]
The residents emphasized the importance of their management-competency regarding the quality of patient care. Some representative statements were:
I think that the competency of every resident affects the quality of patient care because all these qualities lead to better patient treatment and ensure that the patient receives examination and therapy earlier. [p4, m, 30y]
I assume that it’s a large share of the quality of patient care, because the more organised you are or a ward is the more precise processes run and controlled, which leads to increased patient safety. [p8, m, 31y].
Self-Assessment Survey
Among the 88 participants, 14.8% had advanced training in management through a university degree, internships or specific advanced training. The average year of residency was 3.7 years (1–10 years). The gender distribution was as follows: 23 were male (42.6%) and 31 were female (57.4%). The response rate was 14.0%.
In the beginning of the questionnaire before individual management functions were explained to them the mean of their estimation was 32.5%, in the end it accounted for 40.6%, which means a highly significant difference (p-value of 0.0005, paired t-test). This might illustrate, that residents carry out managerial activities during their working day without initially identifying them as managerial tasks unless the residents were previously sensitized.
Except for “Monitor” with a mean of 2.94 (SD = 1.04) all of the defined management functions by Yukl and Nameroff39 were rated as important to absolutely essential (Figure 2). “Inform” was rated as the most important function with a mean of 4.28 (SD = 0.72).
 |
Figure 2 Managerial behavior system-instruments by Yukl and Nameroff (n=88). Notes: Scale: 1 = irrelevant 2 = less important 3 = important 4 = very important 5 = absolutely essential. |
Regarding the modified part of the instrument, all aspects of functional management (by Fayol) were rated as important or very important, whereas scores for more institutional functions (Mintzberg) were lower for many functions.
The activities with the lowest grading were all defined by Mintzberg: “Negotiator” (M = 2.34, SD = 1.1), “Figurehead” (M = 2.68, SD = 0.99), “Spokesperson” (M = 2.79, SD = 1.03), “Resource allocator” (M = 2.90, SD = 1.16) and “Innovator” (M = 2.95, SD = 1.03) (Figure 3). The activities: “Organising” (M = 3.95, SD = 0.89), “Coordinating” (M = 3.84, SD = 0.85), and “Commanding” (M = 3.81, SD = 0.83), defined by Fayol (Figure 4), as well as the role “Disseminator” (M = 3.94, SD = 0.88), defined by Mintzberg (Figure 3), were rated with the most relevance for the residents’ work.
Direct Observation
The number of observed activities of the twelve residents within a timeframe of one week is shown in Table 4. The results of the main-categories (Table 4) were summed up in four management fields in conformity with the description of Luthans45 besides the “Genuine physician tasks” (Table 5).
 |
Table 4 Leadership Observation System by Luthans - Frequency of Observed Activities |
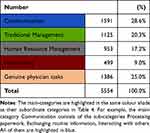 |
Table 5 Subsumption of Table 4, Overview of the Daily Tasks of a Resident |
Activities related to the management field “Communication” were the most often observed in terms of the daily clinical work of residents on the ward. The genuine physician tasks were only the second often observed activities followed by tasks of “Traditional Management” and “Human Resource Management”. The rarest documented activities were those related to the Management field “Networking”.
Discussion
This study illustrates medical residents’ lack of awareness regarding their managerial function in course of their daily work. This point is underlined by the fact that all participants had difficulties in defining “Management” although they were all familiar with the term. Even though physicians could not define management, they estimated 40.6% of their daily work to be managerial activities. We observed that residents undertake managerial tasks without recognising them, which is in line with the results of another study.41 This also explains why there is a big discrepancy between the above estimation and the results of the direct observations, which detected 75.1% of observed activities as managerial.
It is remarkable that “Communication”, more specifically the activity “Exchanging routine information”, was the most often observed activity in residents’ daily clinical work on the ward. This result could be limited by a possible misinterpretation (by the observers) of communication in regards of exchange of medical information as routine management information. However, this observation is in line with results of the self-assessment survey, in which the activity “Inform” was rated as the most important management function. This result was also confirmed by a number of statements of residents during the interviews. Tallying with this, Ilse highlighted “Communication” as a management tool of major importance for the residents’ work.52 This result is important since the above-mentioned competency frameworks for medical education increasingly place emphasis on the role of “communicator”.25,53 Nevertheless, this role only includes interaction between physicians and their patients. Moreover, the related role of “collaborator”, which includes aspects of physicians’ communication with other professional groups also does not include specific management aspects.
“Organising” and “Coordinating” illustrate two further management activities which were emphasised through the self-assessment survey and the semi-structured interviews to be fairly important for the residents’ day-to-day work. Similarly, a large number of observed tasks could fall under the category organization. The way physicians approach their patients is similar to the very popular management method PDCA (plan–do–check–act).54 But the application of this method (that includes basic elements of Fayol’s management-functions) in pure management tasks seems to pose a major difficulty for physicians. This was illustrated by different responses during the interviews, for example:
I am new in this job, so, of course I just have to ask a lot about how the procedures are usually done. Unfortunately this is true for a lot of questions concerning the organization of my working day since university courses are often not application-related. [p2, f, 27y]
This result supports similar observation in Santrić Milicevic’s study, which highlighted shortcomings in physician’s planning and priority setting skills.51
Interestingly, genuine physician tasks were only the second most often observed activities and only comprised 24.9% of all activities. This percentage provides no information about the time spent in each activity, since only the number of tasks (irrespective of their duration) was counted.
Although management activities are an essential part of the residents’ work, they are still not included in medical curricula.13–15 For this reason, it is unsurprising that a study of primary health-care teams detected deficiencies in managerial skills such as communication, planning, priority setting and leading.14 These deficiencies were illustrated through the results of the semi-structured interviews in this study as well. None of the participants felt adequately competent in the managerial activities residents are faced with in context of their daily work. A possible explanation for that could be the lack of perception for the Manager role and its various tasks. This could be explained by the discrepancy between the defined management-role in competency-catalogues and management functions needed for physicians’ everyday work.
Comparing the results of this study with the description of the CanMEDS’ manager role, differences are obvious: The CanMEDS’ Framework defines “Organizing”, “Resource allocation” and “Effectiveness” as central managerial skills, while the residents perceived “Inform” and “Support” to be the most important managerial functions for their daily work. Furthermore, residents considered “Resource allocation” as one of the less important managerial functions of their job. Although residents regarded “Organising” as an important function of their work they considered functions like “Consult”, “Manage”, “Problem solving” and “Recognise” as similarly relevant.
After the development of the CanMEDS Framework in 2005,55 universities and hospitals have increasingly offered managerial training or incorporated managerial skills into their study programs. Even though different programs varied in content, duration and point of time, they were all evaluated positively by the participants.29–33 However, there is no adequate outcome-oriented evaluation associated with these training and education opportunities.56 Thus, it is unclear whether managerial training based on the CanMEDS Framework imparts the necessary knowledge and skills that physicians need. In line with this, the interviewees were convinced that they would benefit from managerial skills training. Brouns found similar results in a study that looked into residents perceptions for the need of management education.20 A recent review of literature also concluded, that there is a need of including management training in medical curricula.57
Residents’ competency in managerial activities such as organising, coordinating or communicating directly affects the course of the patients’ stay in hospital as emphasized by the interviewees. Therefore, managerial skills are not only important for improving economic efficiency, but also but also influence the quality of patient care. The first part has been shown in previous studies, which have observed that physician leadership skills positively influenced the hospitals’ economic outcome as well as patients’ and staff’ satisfaction.58–60 In contrary, data regarding the influence of resident management skills on the quality of patient care is still missing. Nevertheless, the Patient Protection and Affordable Care Act (PPACA) presupposes competencies in managerial activities to conduct residents’ daily work.58
Limitations
There were a number of limitations in the conduct of this study. Firstly the willingness to participate in the interviews was quite low. This could be explained by the fact that we estimated the duration of 60 minutes for an interview, which might have deterred some residents. Secondly, the response rate of the self-assessment survey was low (14.0%). This could be explained by the following facts: 1. As shown by this study, the awareness for the extend of the physicians own management tasks was very low. Many residents might have thought that this survey focused on physicians in institutional management positions. 2. The expected duration of completion was estimated to be 30 Minutes, which might have discouraged some residents. Nevertheless, it still corresponds to the average response rate for written surveys, which is between 5% and 40%.61 It is possible, that a selection bias exists, and those who agreed to participate are more focused on management than those who did not participate, which may have affected the generalizability of the study. Demographics show that only a very small part of the participants were educated in management. In addition, the results point out that participants had very little awareness and knowledge of the issue. Both arguments indicate that selection bias was not very pronounced. Moreover, given that residents of all specialties participated, the results are most likely representative for the whole cohort. Thirdly, the instruments used in the study were not validated for a use in German language. As the instruments were validated in English and applied in German in previous studies, no bias of results was expected.41 A further limitation is given by the direct observation, because only the total number of managerial tasks is considered and not the time these tasks take. A percentage distribution cannot be given. Finally, a possible limitation is related to the use of the five-point Likert-scale of the “Managerial Behavior System-Instruments” of Yukl and Nameroff. The third step is defined as “important” instead of representing a neutral position, resulting in a skewed scale. However, the instrument was selected because it was the only instrument found in literature for that purpose that had been applied in previous studies. A large majority of participants chose the steps 4 = very important (38.28%) or 5 = absolutely essential (22.58%), which suggests that the perceived relevance of the activities was independent of the skewed scale.
Conclusion
This study illustrates the prominent role of management activities in context of medical residents’ clinical work, while at the same time shows that residents do not feel sufficiently competent in this area. Moreover, there is a discrepancy between the definition of management in medical education competency frameworks (concentrating more on institutional aspects) and the more functional aspect of management found as necessary in this study. Although adequate competencies in managerial skills are essential for residents to carry out their daily work on the ward, the education of these skills is still not implemented in study or residency programs. An evaluation of the influence of residents’ managerial competency on quality of patient care is still missing. In view of the results of this study, it is recommended to implement management trainings in medical curricula as a mandatory part, and to evaluate these with regard to the quality of patient care.
Future research should aim to evaluate residents’ managerial competencies in view of the quality of patient care. Due to the fact that quality of patient care is directly linked to the patient-safety, managerial education of residents cannot longer primarily be viewed as an optional improvement related to economic efficiency.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors declare that they have no conflicts of interest.
References
1. Rechkemmer K, Brenzel G, De la Chaux D, Eppinger U, Fischer R. Management Innerer Qualität: Krankenhäuser, Rehakliniken, Soziale Einrichtungen: Krankenhauser, Rehakliniken, Soziale Einrichtungen [Management of Internal Quality. Hospitals, rehabilitation clinics, social institutions]. Stuttgart: W. Kohlhammer GmbH; 2015. German.
2. Fuchs C. Demografischer Wandel und Notwendigkeit der Priorisierung im Gesundheitswesen [Demographic change and the need for prioritization in health care]. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz. 2010;53(5):435–440. German. doi:10.1007/s00103-010-1045-8
3. Bork U, Welsch T, Weitz J. MBA – der Arzt von morgen? [MBA - the doctor of tomorrow?] Augenheilkunde up2date. 2015;5(04):305–315. German. doi:10.1055/s-0041-106520
4. Schubert H. Netzwerkmanagement in Kommune und Sozialwirtschaft: Eine Einführung [Network Management in Municipalities and the Social Economy: An Introduction]. Wiesbaden: Springer VS; 2018. German.
5. Obermann K, Müller P. Der niedergelassene Arzt [The resident physician]. In: Thielscher C, editor. Medizinökonomie 2: Unternehmerische Praxis und Methodik [Medical Economics 2: Entrepreneurial Practice and Methodology]. Wiesbaden: Springer Fachmedien Wiesbaden; 2017:7–46. German.
6. von Eiff W. Der Arzt als Manager: controlling, Personalführung und Organisation als Bestandteile des zukünftigen Mediziner-Profils [The physician as manager: controlling, personnel management and organization as components of the future physician's profile]. In: Ansorg M, Heberer J, Tsekos E, von Eiff W, editors. OP-Management. Vol 2. Berlin: Medizinisch Wissenschaftliche Verlagsgesellschaft; 2009:23–36. German.
7. Steinmann H, Schreyögg G. Management. Wiesbaden: Gabler; 2005.
8. Fayol H. General and Industrial Management. Ravenio Books; 2016.
9. Mintzberg H. The Nature of Managerial Work. Prentice Hall; 1980:59 p.
10. Busch H-P. Arzt und Gesundheitsmanager. Aus dem klinischen Alltag ein Handbuch für Krankenhausärzte [Physician and Health Care Manager. From the clinical everyday life a handbook for hospital physicians]. Kulmbach: Mediengruppe Oberfranken-Fachverlage GmbH & Co. KG; 2017. German.
11. Chan M-K, de Camps Meschino D, Dath D. Collaborating internationally on physician leadership development: why now? Leadersh Health Serv. 2016;29(3):231–239. doi:10.1108/LHS-12-2015-0050
12. von Eiff W. Der Medizin-Manager – die neue Rolle des Arztes [The medical manager - the new role of the physician]. HNO. 2001;49(6):479–481. German. doi:10.1007/s001060170101
13. Abbas MR, Quince TA, Wood DF, Benson JA. Attitudes of medical students to medical leadership and management: a systematic review to inform curriculum development. BMC Med Educ. 2011;11(1):93. doi:10.1186/1472-6920-11-93
14. Santrić Milicevic MM, Bjegovic-Mikanovic VM, Terzic-Supić ZJ, Vasic V. Competencies gap of management teams in primary health care. Eur J Public Health. 2010;21(2):247–253.
15. Bronson D, Ellison E. Crafting successful training programs for physician leaders. Healthcare. 2015;1–5. doi:10.1016/j.hjdsi.2015.01.002
16. Bundesministerium der Justiz. Verbraucherschutz B. Approbationsordnung für Ärzte [Consumer protection B. Licensing regulations for physicians]; 2002. Available from: https://www.gesetze-im-internet.de/_appro_2002/BJNR240500002.html.
17. Frank JR. The CanMEDS 2005 physician competency framework; 2005.
18. Dath D, Chan M-K, Abbott C. CanMEDS 2015: from Manager to Leader. The Royal College of Physicians and Surgeons of Canada; 2015.
19. Canada TRCoPaSo. CanMEDS Role: leader 2015 [24.09.2019]. Available from: http://www.royalcollege.ca/rcsite/canmeds/framework/canmeds-role-leader-e.
20. Brouns J, Berkenbosch L, Ploemen-Suijker FD, Heyligers I, Busari JO. Medical residents perceptions of the need for management education in the postgraduate curriculum: a preliminary study. Int J Med Edu. 2010;1:76–82. doi:10.5116/ijme.4cd8.43f1
21. Fluit C, Bolhuis S, Grol R. Evaluation and feedback for effective clinical teaching in postgraduate medical education: validation of an assessment instrument incorporating the CanMEDS roles. Med Teach. 2012;34(11):893–901. doi:10.3109/0142159X.2012.699114
22. Hall P, Byszewski A, Sutherland S, Stodel E. Developing a sustainable electronic portfolio (ePortfolio) program that fosters reflective practice and incorporates CanMEDS competencies into the undergraduate medical curriculum. Acad Med. 2012;87(6):744–751. doi:10.1097/ACM.0b013e318253dacd
23. Berkenbosch L, Muijtjens A, Zimmermann L, Heyligers I, Scherpbier A, Busari J. A pilot study of a practice management training module for medical residents. BMC Med Educ. 2014;14(1):107. doi:10.1186/1472-6920-14-107
24. Mea G. Simulating the physician as healthcare manager: an innovative course to train for the manager role. GMS J Med Edu. 2016;33(3):e43.
25. Nationaler Kompetenzbasierter Lernzielkatalog Medizin (NKLM) [National Competence Based Learning Objectives Catalogue Medicine (NKLM)]. MFT Medizinischer Fakultätentag der Bundesrepublik Deutschland e. V; 2015. https://www.gmds.de/fileadmin/user_upload/Publikationen/Empfehlungen_Veroeffentlichungen/150604_Lernzielkatalog_Medizin.pdf. Accessed August 31, 2022. German.
26. Batalden P, Leach D, Swing S, Dreyfus H, Dreyfus S. General competencies and accreditation in graduate medical education. Health Affairs. 2002;21(5):103–111. doi:10.1377/hlthaff.21.5.103
27. Colleges A. Medical Leadership Competency Framework - Enhancing Engagement in Medical Leadership. Vol. 3. Coventry: NHS Institute for Innovation and Improvement; 2010.
28. Mea M, Forster J, Biller S, Fabry G. Development of a questionnaire to assess medical competencies: reliability and validity of the Questionnaire. GMS Zeitschrift für medizinische Ausbildung. 2011;28(2):Doc31. doi:10.3205/zma000743
29. Babitch LA. Teaching practice management skills to pediatric residents. Clin Pediatr (Phila). 2006;45(9):846–849. doi:10.1177/0009922806294216
30. Hemmer PR, Karon BS, Hernandez JS, Cuthbert C, Fidler ME, Tazelaar HD. Leadership and management training for residents and fellows: a curriculum for future medical directors. Arch Pathol Lab Med. 2007;131(4):610–614. doi:10.5858/2007-131-610-LAMTFR
31. Kaur N, Singh T. Introducing medical students to health care management. Med Edu. 2009;43(11):1090–1091. doi:10.1111/j.1365-2923.2009.03489.x
32. Stergiopoulos V, Maggi J, Sockalingam S. Teaching the physician-manager role to psychiatric residents: development and implementation of a pilot curriculum. Acad Psychiatry. 2009;33(2):125–130. doi:10.1176/appi.ap.33.2.125
33. Dimitriadis K, Moder S, Pinilla S, von der Borch P. Medical students as managers of their university hospital. Med Edu. 2013;47(11):1125–1126. doi:10.1111/medu.12340
34. Strübing J. Was ist Grounded Theory? Grounded Theory: Zur sozialtheoretischen und epistemologischen Fundierung des Verfahrens der empirisch begründeten Theoriebildung [What is Grounded Theory? Grounded Theory: On the social-theoretical and epistemological foundation of the method of empirically grounded theory building]. Wiesbaden: VS Verlag für Sozialwissenschaften; 2008:13–36. German.
35. Bücker N. Kodieren - aber wie? Varianten der Grounded-Theory-Methodologie und der qualitativen Inhaltsanalyse im Vergleich [Coding - but how? Variants of grounded theory methodology and qualitative content analysis in comparison]. Forum Qual Soc Res. 2020;21(1):43. German.
36. Mintzberg H. The Nature of Managerial Work. Prentice Hall; 1973.
37. MAXQDA. Was ist MAXQDA? 2018. Available from: https://www.maxqda.de/was-ist-maxqda.
38. Yukl G. Leadership in Organizations. Boston, Amsterdam, Cape Town: Pearson; 2013.
39. Yukl G, Lepsinger R. Preliminary report on validation of the managerial practices survey. In: Clark KECMB, editor. Measures of Leadership. West Orange, NJ, US: Leadership Library of America; 1990:223–237.
40. Yukl G. An evaluative essay on current conceptions of effective leadership. Eur J Work Organ Psychol. 1999;8:33–48. doi:10.1080/135943299398429
41. Dimitriadis K. Der Assistenzarzt als Manager; 2015.
42. Müllner M. Erfolgreich wissenschaftlich arbeiten in der Klinik [Successful scientific work in the clinic]. Springer-Verlag Wien GmbH; 2002. German.
43. Häder M. Pretests. Empirische Sozialforschung [Empirical Social Research]. Wiesbaden: VS Verlag für Sozialwissenschaften; 2010:393–394. German.
44. Merchel J. Evaluation in der Sozialen Arbeit [Evaluation in social work]. München: Ernst Reinhardt Verlag; 2015. German.
45. Luthans F, Lockwood DL. Toward an observation system for measuring leader behavior in natural settings. In: Hunt JG, Hosking D-M, Schriesheim CA, Stewart R, editors. Leaders and Managers. Pergamon; 1984:117–141.
46. Hunt JG, Hosking DM, Schriesheim CA. Leaders and Managers: InternationalPerspectives on Managerial Behavior and Leadership. Vol. 2. New York: Pergamon Press; 1985.
47. Luthans F, Rosenkrantz SA, Hennessey HW. What do successful managers really do? An observation study of managerial activities. J Appl Behav Sci. 1985;21(3):255–270. doi:10.1177/002188638502100303
48. Anlage 24 zum Bundesmantelvertrag-Ärzte [Annex 24 to the Federal Manual Agreement - Physicians], § 2; 2015. German.
49. Persönliche Leistungserbringung-Möglichkeiten und Grenzen der Delegation ärztlicher Tätigkeiten [Personal service provision-possibilities and limits of delegation of medical activities]. Dtsch Arztebl 2008; 105(41): A-2173 / B-1865 / C-1817. Available from: https://www.bundesaerztekammer.de/fileadmin/user_upload/_old-files/downloads/Empfehlungen_Persoenliche_ Leistungserbringung.pdf. Accessed September 04, 2022. German.
50. zdf_neo. Junior docs; 2013.
51. MeCuM-SiGma. MeCuM-SiGma goals; 2018. Available from: https://mecum-sigma.de/ziele.html.
52. Ilse RG. Physician Perceptions of Leadership Effectiveness of Front-Line Managers in Hospital [Dissertation]; 2015.
53. Canada TRCoPaSo. CanMEDS role: communicator; 2015. Available from: https://www.royalcollege.ca/rcsite/canmeds/framework/canmeds-role-communicator-e.
54. Tague NR. The Quality Toolbox. Milwaukee, Wis: ASQ Quality Press; 2005.
55. Canada TRCoPaSo. CanMEDS framework 2018; 2019. Available from: http://www.royalcollege.ca/rcsite/canmeds/canmeds-framework-e.
56. Busari JO, Stammen LA, Gennissen LM, Moonen RM. Evaluating medical residents as managers of care: a critical appraisal of assessment methods. Adv Med Educ Pract. 2014;5:27. doi:10.2147/AMEP.S58476
57. Busari JO, Berkenbosch L, Brouns JW. Physicians as managers of health care delivery and the implications for postgraduate medical training: a literature review. Teach Learn Med. 2011;23(2):186–196. doi:10.1080/10401334.2011.561760
58. Blumenthal DM, Bernard K, Bohnen J, Bohmer R. Addressing the leadership gap in medicine: residents’ need for systematic leadership development training. Acad Med. 2012;87(4):513–522. doi:10.1097/ACM.0b013e31824a0c47
59. Peter Angood M, Birk S. The value of physician leadership. Physician Exec. 2014;40(3):6.
60. Tasi MC, Keswani A, Bozic KJ. Does physician leadership affect hospital quality, operational efficiency, and financial performance? Health Care Manage Rev. 2019;44(3):256–262. doi:10.1097/HMR.0000000000000173
61. Döring N, Bortz J. Datenerhebung. Forschungsmethoden und Evaluation in den Sozial- und Humanwissenschaften [Data Collection. Research methods and evaluation in the social and human sciences]. Vol. 5. Heidelberg: Springer-Verlag; 2016. German.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


