Back to Journals » International Medical Case Reports Journal » Volume 14
A Life Saving Emergent Temporary External Carotid Artery Controlled in Extensive Craniofacial Injury
Authors Tanmit P , Angkasith P , Teeratakulpisarn P , Thanapaisal C, Surakunprapha P, Kitkuandee A, Limwattananon P
Received 13 January 2021
Accepted for publication 6 March 2021
Published 30 March 2021 Volume 2021:14 Pages 199—204
DOI https://doi.org/10.2147/IMCRJ.S300774
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Parichat Tanmit, Phati Angkasith, Panu Teeratakulpisarn, Chaiyut Thanapaisal, Palakorn Surakunprapha, Amnat Kitkuandee, Phumtham Limwattananon
Department of Surgery, Faculty of Medicine, Khonkaen University, Khon Kaen, Thailand
Correspondence: Parichat Tanmit
Department of Surgery, Khonkaen University, 123 Moo16 Mittraphap Road, Nai-Muang, Muang District, Khon Kaen, 40002, Thailand
Tel +66850001714
Email [email protected]
Introduction: Craniofacial trauma may potentially have significant blood loss which may lead to death in some trauma patients.
Case Report: We report a case of a 43-year-old male who had a lethal noncompressible arterial hemorrhage from a penetrating wound on his left frontotemporal and preauricular region. Extensive bleeding was successfully temporarily controlled by external carotid artery (ECA) occlusion. The definitive operation was completed in a staged fashion following a computed tomography angiography assessment extension of the injury.
Conclusion: Temporarily controlling the bleeding from the carotid artery should be considered as a life saving procedure in a lethal craniofacial injury.
Keywords: craniofacial injury, external carotid artery ligation, temporary external carotid artery control, maxillary artery bleeding
Introduction
An uncontrolled extensive arterial bleed from a craniofacial injury is the leading cause of death in trauma patients. The emergency external carotid artery (ECA) ligation for exsanguinating hemorrhage is a useful life saving procedure.
Case Report
A 43-year-old male sustained an extensive penetrating injury to his left frontotemporal and preauricular region—from a broken grass-cutting blade—with an incompressible pulsating lesion (Figure 1). He was immediately transferred to a trauma center. His vital signs showed systolic blood pressure of 60–70 millimeters of mercury and his pulse rate was 140 beats per minute and oxygen saturation was 80%. The physical examination suggested an active arterial bleed from the maxillary artery, anterior to the mandibular neck. A few minutes after the patient arrived, his consciousness was deteriorating to E1V1M5 and an endotracheal tube was inserted. An immediate transfusion of group O red blood cell was initiated.
 |
Figure 1 Penetrating wound on left frontotemporal and preauricular region. |
The trauma plus protocol (The protocol trauma team activation for severe trauma patient of institute) was activated and the patient was immediately transferred to the operating room. A longitudinal skin incision along the anterior margin of the left sternocleidomastoid muscle was performed. The posterior belly of the digastric muscle was cut to reveal the carotid bifurcation clearly. The left common facial vein was divided. The left common carotid artery, external and internal carotid arteries were exposed and encircled by vascular slings. Transient left ECA occlusion by application of a Rumel tourniquet was performed (Figure 2). A massive artery bleedwas controlled. The duration between the activation of the trauma protocol and the occlusion of the ECA was 8 minutes. The penetrating tract at the preauricular region was tamponaded by balloon (Figure 3). Subsequently, the patient was transferred to computed tomographic angiography (CTA) of the brain and neck to evaluate the adjacent structure and intracranial vascular injury. The study revealed a metallic foreign body with multiple left side skull fractures with multiple comminuted fractures involving the zygomatic process of the left temporal bone, lateral wall of left orbit, left orbit apex, left superior orbital fissure and left optic canal, squamous part of left temporal bone, wall of sphenoid and ethmoid sinuses, and the greater and lesser wing of the sphenoid bone (Figure 4). There was acute subarachnoid hemorrhage along the left Sylvian fissure and an acute subdural hemorrhage along the frontotemporal convexity with brain swelling (Figure 5). There was no evidence of intracranial arterial injury (Figure 6). The patient was returned to the operating room and the foreign body was carefully removed. A completed transection of the maxillary artery was identified and ligated, then the ECA was released and revealed no active bleeding site. The total duration of the transient ECA occlusion was 100 minutes. The foreign body fragments were removed. The dura was repaired and a subgaleal drain was placed. The patient had received 6 units of packed red cells, 6 units of fresh frozen plasma and 4 units of single donor platelets. Ongoing resuscitation continued in the trauma intensive care unit (ICU). The preauricular area was re-explored over the next 2 days. The left mandible condyle fixation with plate and screw was performed and the complete transection of the facial nerve was re-anastomosed to the great auricular nerve. The duration of stay was 10 days. The patient had good levels of conscious with a GCS of E4V5M6 and motor power grade V. The patient was paralyzed on the left side of the face from the facial nerve injury and suffered permanent visual loss in the left eye due to extensive optic nerve damage.
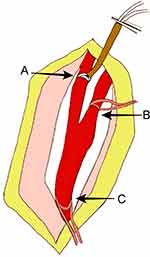 |
Figure 2 The transient left external carotid artery occlusion. (A) External carotid artery; (B) internal carotid artery; (C) common carotid artery. |
 |
Figure 3 Technique of bleeding control. (A) External carotid artery occlusion; (B) internal carotid artery; (C) balloon tamponade; (D) common carotid artery. |
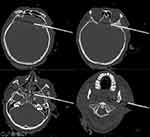 |
Figure 4 Computed tomography of a metallic foreign body with multiple left side skull and facial bone fracture. |
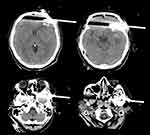 |
Figure 5 Computed tomography scan showing the presence of subarachnoid hemorrhage along left Sylvian fissure and acute subdural hemorrhage along frontotemporal convexity with brain swelling. |
 |
Figure 6 Computed tomography angiography shows no visible intracranial vascular injury. |
Discussion
Arterial bleeding from a craniofacial injury is a life-threatening condition. The immediate management consists of assessing a patient’s condition rapidly and accurately, then resuscitating and stabilizing the patient according to priority, including airway with cervical spine protection, breathing, circulation, disability, and exposure/environmental control.1
The craniofacial area consists of several structures, including branches of the internal and external carotid artery, vertebral artery, veins, cranial nerve, bony structure, brain, and other intracranial structures. The amount of tissue damage depends on the amount of energy transferred to that tissue.
Vascular complications in a penetrating brain injury have been reported to range from 5 to 40% in both high and low velocity penetrating injury.2–4 The active pulsatile arterial bleeding can cause hemorrhagic shock. The physical examination is helpful to determine the possible injury. An extensive external bleedmust be quickly assessed and controlled. Superficial vessel compression may minimize blood loss. The traumatic facial hemorrhage usually results from the lacerated periosteum, mucosa or major vessels. The most commonly injured vessels include branches of the ECA, the maxillary artery, and its intraosseous branches.5 However, bleeding from deep vessels is difficult to localize and treat.
The direct application to the common carotid artery can reduce bleeding, but the prolonged compression will result in cerebral ischemia. The selective occlusion of the ECA with local pressure by balloon tamponade can effectively reduce blood loss.6
Neuroimaging is vital for surgical purposes,7 especially for determining type of surgery, size and location of the approach, and route of extraction of the foreign body. The literature shows many advantages from CT-scans with respect to skull radiography, including increased capacity to identify missile and bone fragments, characterization of the projectile trajectory, evaluation of the extent of brain injury, and detection of intracranial hematomas.
Multidisciplinary management was represented in this case. The patient was immediately transferred from the emergency room to the operating theater through the trauma plus protocol of our center. After the active hemorrhage was controlled and vital signs were stable, the patient underwent a brain computed tomography scan. The neurosurgeon evaluated the scan and the foreign body fragments were removed and then the patient continued to be resuscitated in the ICU. The remaining facial nerve injury was re-evaluated and reconstructed after a few days.
Conclusion
The active craniofacial bleeding is threatening hemorrhage. If the bleeding cannot be controlled and the patient becomes unstable, immediate surgical selective temporary external carotid artery controlled should be considered.
Ethics Approval and Consent to Participate
Center for Ethics in Human Research of Khon Kaen University (KKUEC) approved this case report and the committee’s reference number is HE631669.
Consent for Publication
The patient informed consent for publish the case details and images.
Acknowledgments
The authors gratefully acknowledge the Srinagarind hospital surgeons team and the nursing team for their contributions to the work presented in this paper.
Disclosure
The authors declare that there is no conflicts of interest in this work.
References
1. Committee American College of Surgeon. Advance Trauma Life Support.
2. Gutiérrez-González R, Boto GR, Rivero-Garvía M, et al. Penetrating brain injury by drill bit. Clin Neurol Neurosurg. 2008;110(2):207–210. doi:10.1016/j.clineuro.2007.09.014
3. Nathoo N, Boodhoo H, Nadvi SS, et al. Transcranial brainstem stab injuries: a Retrospective Analysis of 17 Patients. Neurosurgery. 2000;47(5):1117–1122. doi:10.1097/00006123-200011000-00018
4. Levy ML, Rezai A, Masri LS, et al. The significance of subarachnoid hemorrhage after penetrating craniocerebral injury, correlations with angiography and outcome in a civilian population. Neurosurgery. 1993;32(4):532–540. doi:10.1097/00006123-199304000-00007
5. Smith TP. Embolization in the external carotid artery. J Vasc Interv Radiol. 2006;17(12):1897–1913. doi:10.1097/01.RVI.0000247301.64269.27
6. Lee TS, Ducic Y, Gordin E, et al. Management of carotid artery trauma. Craniomaxillofac Trauma Reconstr. 2014;7(3):175–189. doi:10.1055/s-0034-1372521
7. Alvis-Miranda HR, Rubiano AM, Agrawal A, et al. Craniocerebral gunshot injuries, a review of the current literature. Bull Emerg Trauma. 2016;4(2):65–74.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
