Back to Journals » Clinical Interventions in Aging » Volume 18
A Higher Postoperative Barthel Index at Discharge is Associated with a Lower One-Year Mortality After Hip Fracture Surgery for Geriatric Patients: A Retrospective Case‒Control Study
Authors Pan L, Wang H, Cao X, Ning T, Li X, Cao Y
Received 5 March 2023
Accepted for publication 19 May 2023
Published 23 May 2023 Volume 2023:18 Pages 835—843
DOI https://doi.org/10.2147/CIA.S409282
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Maddalena Illario
Liping Pan,1,* Hao Wang,1,* Xiangyu Cao,2 Taiguo Ning,1 Xueying Li,3 Yongping Cao1
1Department of Orthopedics, Peking University First Hospital, Beijing, 100034, People’s Republic of China; 2Department of Orthopedics, Peking University Third Hospital, Beijing, 100191, People’s Republic of China; 3Department of Medical Statistics, Peking University First Hospital, Beijing, 100034, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yongping Cao, Department of Orthopedics, Peking University First Hospital, No. 8 Xishiku Street, XiCheng District, Beijing, 100034, People’s Republic of China, Email [email protected]
Purpose: To evaluate the relationship between the postoperative Barthel index assessing activities of daily living at discharge and the one-year mortality after hip fracture surgery.
Methods: Patients with hip fracture admitted to Peking University First Hospital from January 2015 to January 2020 were enrolled retrospectively according to the inclusion and exclusion criteria. The Barthel index and other related confounding variables were collected. Logistic regression and Kaplan‒Meier survival curves were constructed to explore the relationship between the postoperative Barthel index at discharge and the one-year mortality of geriatric patients after hip fracture surgery.
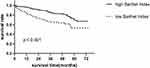
Results: A total of 444 patients with a mean age of 81.61± 6.14 years were included. A significant difference was not observed in the preoperative Barthel index at admission between the deceased group and the surviving group (38.90± 15.83 vs 36.96± 10.74, p=0.446). However, the difference in the postoperative Barthel index at discharge between these two groups was statistically significant (43.08± 14.40 vs 53.18± 13.43, P< 0.001). The multivariable logistic regression analysis revealed that the postoperative Barthel index at discharge was an independent risk factor for one-year mortality after adjustment for confounding variables (adjusted OR 0.73, 95% CI 0.55– 0.98, p˂0.05). The Kaplan‒Meier survival curve showed that patients who had a high Barthel index (≥ 50) at discharge had a significantly lower mortality in the long term than patients with a low Barthel index (< 50) at discharge (P< 0.001).
Conclusion: The postoperative Barthel index at discharge was independently associated with the one-year mortality of geriatric patients after hip fracture surgery. A higher postoperative Barthel index at discharge indicated a lower mortality after hip fracture surgery. The Barthel index at discharge has the potential to provide essential prognostic information for early risk stratification and directing future care.
Keywords: Hip fracture, Barthel index, one-year mortality, geriatrics, at discharge
Introduction
Hip fracture is a devastating public health problem with a high epidemiology worldwide in geriatrics.1,2 High disability rates, mortality and social cost after hip fracture impose substantial pressure on patients and their care providers. The mortality one year after hip fracture is estimated to range from 2.4% to 34.8%.2–4 Many risk factors and models are proposed to stratify the mortality risk after hip fracture surgery. Demographic characteristics, including age, sex and BMI (body mass index), comorbidities, complications and special laboratory test results, such as serum albumin and haemoglobin levels, were identified as risk factors.2,5 The delay of surgery and other factors associated with surgery have been shown in other study.5 Several predictive models were constructed based on these risk factors.6,7 However, the accuracy of the models stratifying the mortality risk after hip fracture surgery was not satisfactory,6,7 and the levels of activities of daily living after surgery were rarely explored as potential risk factors.
Hip fracture impairs activity levels, even after surgery. Approximately 30% to 80% of patients lose functional independence after hip fracture.1,8 The Barthel index is one of the most widely used tools assessing functional independence and activity of daily living. Several studies confirmed that the Barthel index affected mortality in geriatric patients,9,10 or patients with heart diseases11–13 or pneumonia.14 Other studies found that the Barthel index seemed useful for the assessment of activities of daily living and functional recovery in patients with hip fracture.15–17 However, few studies have explored the relationship between the Barthel index and one-year mortality after hip fracture surgery in geriatric patients.
This study aimed to explore whether the postoperative Barthel index at discharge was independently associated with the one-year mortality after hip fracture surgery in geriatric patients.
Methods and Patients
Study Population
This study was approved by the Peking University First Hospital Ethics Committee. The patients with hip fracture who were admitted to Peking University First Hospital from January 2015 to January 2020 were enrolled retrospectively. The inclusion criteria were as follows: 1) patients were diagnosed with a femoral neck fracture or intertrochanteric fracture; 2) the age at admission was no less than 70 years; and 3) patients were treated with surgery, including internal fixation (such as SHS or DHS, cephalo-medullary nail, multiple screw and so on) or hip arthroplasty. The exclusion criteria were as follows: 1) hip fracture identified as a pathological fracture; 2) death before discharge due to extremely severe complications and thus the Barthel index could not be acquired at discharge; and 3) loss to follow-up.
Variables and Study Endpoints
Variables extracted were divided into several groups, including demographic characteristics, comorbidities, preoperative laboratory test results and parameters related to surgery. Demographic characteristics were age, sex and BMI. Comorbidities included heart disease, neurovascular disease, hypertension, diabetes mellitus and others. Health status was evaluated by calculating the age-adjusted Charlson Comorbidities Index (aCCI) and American Society of Anaesthesiologists (ASA) score.18 The aCCI was calculated using the original Charlson Comorbidities Index with an additional 4 points added for patients older than 70 years.19,20 Preoperative laboratory test results included the serum albumin, sodium and haemoglobin levels at admission. Parameters related to surgery included the fracture type, days the operation was delayed, anaesthesia type, transfusion, surgery type, postoperative complications and the total length of stay (LOS) in the hospital. Postoperative complications included atrial fibrillation, heart failure, delirium, myelosuppression, gastrointestinal haemorrhage, acute cerebral vascular disease, pulmonary infection, hypotension, urinary tract infection, acute kidney failure, acute respiratory failure, acute cardiovascular diseases, deep vein thrombosis, pulmonary embolism, and shock, among others.
The patients were followed by telephone for at least one year after surgery. The primary endpoint was one-year mortality. The secondary endpoint was the long-term survival rate for up to 6 years.
Barthel Index
The activities of daily living (ADL) were evaluated with the Barthel index, which is one of the most widely used tools assessing functional independence.21 The Barthel index comprises 10 items: feeding, bathing, grooming, dressing, bowel control, bladder control, toilet use, transfers (bed to chair and back), mobility on level surfaces, and stairs. Four response categories are assigned to each item, and the total score ranges from 0 to 100 points with a fixed interval of 5 points. The higher the score, the greater the activities of daily living. The Barthel index was acquired by nurses when the patients were admitted to the hospital and discharged from the hospital. Thus, two Barthel index scores, namely, the preoperative Barthel index at admission and the postoperative Barthel index at discharge, were acquired for each patient.
Statistical Analysis
Categorical variables are presented as the numbers of patients (n, %) and were analysed using Pearson’s chi-square test. Continuous variables are presented as the means ± standard deviation or medians with 95% confidence intervals (CIs) when needed and were analysed using one-way ANOVA (analysis of variance) or the Kruskal‒Wallis test.
The association between the early postoperative Barthel index at discharge and one-year mortality after surgery was analysed using univariable and multivariable logistic regression models. Univariable logistic regression was conducted to identify potential risk factors for one-year mortality after surgery based on a threshold p value below 0.05. Multivariable logistic regression was conducted to identify independent risk factors for one-year mortality after surgery, based on a threshold p value below 0.05. The Barthel index was divided by 10 for its fixed interval of 5 before being analysed using a logistic regression models. Models were adjusted for the following potential confounding variables: age, sex, BMI, aCCI, ASA score, albumin level, sodium level, haemoglobin level, surgery types and complications. The odds ratio (OR) was acquired and is presented with 95% CIs and p values. The Kaplan‒Meier survival curve was constructed according to the level of the postoperative Barthel index at discharge and analysed using the Log rank test.
All data were analysed with SPSS Statistics version 25 (SPSS, Inc., Chicago, IL, USA), and a p value less than 0.05 was considered a significant difference.
Results
In total, 444 patients with a mean age of 81.61±6.14 years were included in this study, and 322 (72.52%) were females. A screening diagram of the enrolled patients is shown in Figure 1. A total of 266 (59.90%) patients were diagnosed with a femoral neck fracture. A total of 238 (53.60%) patients were treated with total or hemi-hip arthroplasty, and the remainder were treated with internal fixation with screws, plates or intramedullary nails. Forty-one (8.45%) patients were lost to follow-up. The mean follow-up time after discharge was 35.56±19.80 months, and the overall mortality one year after hip fracture surgery was 9.7%. According to the survival status one year after surgery, the patients were divided into the deceased group and the surviving group. Their characteristics, including demographic characteristics, comorbidities, preoperative laboratory test results and parameters related to surgery, are listed in Table 1.
 |
Table 1 Demographic and Clinic Characteristics of the Patients Included in This Study |
 |
Figure 1 Flow chart of patient inclusion. |
A significant difference was not observed in the preoperative Barthel index at admission between the deceased group and the surviving group (38.90±15.83 vs 36.96±10.74, p = 0.446). However, the difference in the postoperative Barthel index at discharge between these two groups was significant (43.08±14.40 vs 53.18±13.43, P< 0.001), as shown in Figure 2. The mean duration from surgery to discharge was 10.09±8.29 days. No significant difference in the duration from surgery to discharge was observed between these two groups (11.27±6.44 vs 9.96±8.46, p = 0.328).
The multivariable logistic regression analysis revealed that the postoperative Barthel index at discharge was an independent risk factor for one-year mortality after adjustment for confounding variables (adjusted OR 0.73, 95% CI 0.55–0.98, p<0.05), as shown in Table 2. A 10-point increase in the postoperative Barthel index at discharge was associated with a decrease in the one-year mortality by a factor of 0.73.
 |
Table 2 Univariate and Multivariate Logistic Regression of Variables for One-Year Mortality After Hip Fracture Surgery in Geriatrics |
Based on the midpoint of the postoperative Barthel index at discharge, the patients were divided into a high Barthel index group (Barthel index ≥50) and a low Barthel index group (Barthel index ˂50). The Kaplan‒Meier survival curve showed that patients with a high Barthel index at discharge had a significantly lower mortality risk after assessing long-term survival for durations of up to 6 years than patients with a low Barthel index at discharge (P< 0.001), as shown in Figure 3. Median survival rates of the high Barthel index group is 0.962 ± 0.011; Median survival rates of the low Barthel index group is 0.835 ± 0.032.
Discussion
Disability and mortality after hip fracture remain high in geriatric patients. After adjusting for available confounding variables, the postoperative Barthel index at discharge was an independent risk factor for one-year mortality after hip fracture surgery. An increase in the postoperative Barthel index at discharge indicated a decrease in the one-year mortality. Furthermore, patients with a high postoperative Barthel index (≥50) at discharge had a significantly lower mortality in an assessment of their long-term survival for up to 6 years. Thus, the postoperative Barthel index at discharge was a significant factor stratifying the mortality after hip fracture surgery in geriatric patients.
The Barthel index, which can be easily determined by nurses and interpreted in clinical practice, is a simple and highly reliable tool to evaluate activities of daily living.22,23 The Barthel index is a tool to evaluate activities of daily living after hip fracture surgery. With common knowledge of drop in mobility post surgery, someone would expect drop in postoperative Barthels index compared to preoperative Barthels index. But the main purpose of surgery is to maximize the recovery of function, so compared with the preoperative, the patient must have a higher Barthel index at discharge. This is how the Barthel index changes before and after surgery compared to other operations, such as surgical treatment of tumors. Some studies have explored the validity and responsiveness of the Barthel index to assess functional recovery in hip fracture patients. Unnanuntana et al24 confirmed that the Barthel index had good validity in assessing functional recovery in patients who underwent hemiarthroplasty after femoral neck fracture due to its mild to moderate association with the EuroQol visual analogue scale (EQ-VAS) and moderate to strong association with the Morton Mobility Index (DEMMI) and performance-based tests. Inui et al25 found that the early postoperative Barthel index after trochanteric fractures was associated with long-term walking ability. Other studies also used the Barthel index to evaluate functional recovery after hip fracture surgery.16,17 Thus, the use of the Barthel index to evaluate functional recovery after hip fracture surgery in this study was reliable and reasonable. However, the relationship between the Barthel index and mortality of geriatric patients after hip fracture surgery has rarely been investigated.
The association between the Barthel index and mortality has also been explored in patients with other diseases. According to Li et al, the Barthel index at admission is useful for early risk stratification, and the Barthel index is an independent risk factor for all-cause mortality over a median follow-up duration of 10.63 months.11 In a Danish nationwide study,9 Ryg et al found that the Barthel index at admission was independently and strongly associated with mortality within a long follow-up time of 11 years for patients aged ≥65 years. Bahrmann et al reported that both the CCI and Barthel index independently predict mortality in unselected geriatric patients.26 Other studies also documented similar results for patients with other diseases, and a higher Barthel index indicated a lower mortality.10,12–14 These results were consistent with our finding that a higher Barthel index at discharge indicated a lower mortality after hip fracture surgery in geriatric patients. A higher Barthel index indicates higher functional independence and a better health status. Thus, patients with a higher Barthel index are able to move easily and have a better quality of life with fewer complications, and their survival duration may be prolonged.
The postoperative Barthel index in our study was acquired at discharge within a mean time point of 10.09 days after surgery, although some other studies acquired the Barthel index at admission9,11,12 or at discharge.16,17 The Barthel index recorded at admission in our study was not significantly different between patients who survived or died at one year postoperatively. Actually, disability in geriatric patients is mainly affected by pre-existing illnesses and injuries leading to hospitalization.27 As shown by Covinsky et al28 most patients recover to their original functional status before discharge. Different diseases, especially injuries, greatly affect activities of daily living. Hip fracture is a severe injury to geriatric patients and exerts a tremendous effect on their activities of daily living. Thus, the Barthel index at admission must decrease substantially after hip fracture, and the difference between groups was unable to be discovered. After hip fracture surgery, the patients recovered from the acute injury but were still affected by the hip fracture and surgery to some extent. The Barthel index at discharge might accurately reflect the effects of their pre-existing illnesses, new hip fracture, and corresponding surgery. Thus, the postoperative Barthel index at discharge might provide a better prediction of mortality after hip fracture surgery.
The postoperative Barthel index at discharge was divided into two groups based on the cut-off value of 50, and a high Barthel index at discharge was related to a low mortality after hip fracture surgery. This cut-off value for the Barthel index has been used in previously published studies.10,29 In these studies, a Barthel index less than 50 was categorized as severe dependence, and severely dependent patients had a worse prognosis, consistent with our findings.
Several limitations existed in this study. First, this study employed a retrospective design with a limited number of patients. Although much effort was made, selection and information bias could not be avoided. Although our sample size is small, our study is very meaningful. We found a relationship between Barthel index and 1-year mortality after hip fracture, which would raise clinicians’ attention to Barthel index and encourage them to develop effective postoperative treatment plans to improve discharge Barthel index. In our center, the one-year mortality after hip fracture was low, we will further increase the sample size and conduct multi-center joint research in future. Second, the postoperative Barthel index was acquired at discharge, but the time of discharge after surgery differed for every patient. Researchers have not explored whether the duration from surgery to discharge would change the Barthel index. In the present study, the duration from surgery to discharge was limited to 10.09±8.29 days, and no significant difference was observed between those two groups. Third, the postoperative Barthel index at discharge was divided by the cut-off value of 50. However, different cut-off values of the Barthel index were used in different studies and for patients with different diseases. Although we have already shown that the Barthel index, a consecutive variable, was significantly associated with the one-year mortality after hip fracture surgery, the best cut-off value of the Barthel index after hip fracture surgery in geriatric patients should be explored in future studies.
Conclusions
Our study showed that the Barthel index at discharge was independently associated with one-year mortality after hip fracture in geriatric patients and that the higher the Barthel index at discharge, the lower the mortality after hip fracture surgery. The Barthel index at discharge has the potential to provide essential prognostic information for early risk stratification and directing future care.
Abbreviations
BMI, body mass index; aCCI, age-adjusted Charlson Comorbidities Index; ASA, American Society of Anaesthesiologists; LOS, length of stay; ADL, activity of daily living; SD, standard deviation; CI, confidence interval; ANOVA, analysis of variance; OR, odds ratio; EQ-VAS, EuroQol visual analogue scale; DEMMI, de Morton Mobility Index.
Ethical Approval and Consent for Publication
This study was approved by the Institutional Ethics Committee of Peking University First Hospital (No. 2021-432), and complied with the Declaration of Helsinki. The informed consent was waived because it was a retrospective study. All the data collected was confidential.
Acknowledgments
We acknowledge our colleagues from the Department of Orthopaedics, Peking University First Hospital for their help and advice in the process of data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was received to conduct this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49(8):1458–1460. doi:10.1016/j.injury.2018.04.015
2. Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. 2017;377(21):2053–2062. doi:10.1056/NEJMcp1611090
3. Downey C, Kelly M, Quinlan JF. Changing trends in the mortality rate at 1-year post hip fracture - a systematic review. World J Orthop. 2019;10(3):166–175. doi:10.5312/wjo.v10.i3.166
4. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87(3):483–489. doi:10.2106/jbjs.D.01796
5. Sheehan KJ, Sobolev B, Guy P. Mortality by timing of hip fracture surgery: factors and relationships at play. J Bone Joint Surg Am. 2017;99(20):e106. doi:10.2106/jbjs.17.00069
6. Karres J, Heesakkers NA, Ultee JM, Vrouenraets BC. Predicting 30-day mortality following hip fracture surgery: evaluation of six risk prediction models. Injury. 2015;46(2):371–377. doi:10.1016/j.injury.2014.11.004
7. Pallardo Rodil B, Gómez Pavón J, Menéndez Martínez P. Mortalidad tras fractura de cadera: modelos predictivos. Hip fracture mortality: predictive models. Med Clin (Barc). 2020;154(6):221–231. doi:10.1016/j.medcli.2019.09.020
8. Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51(3):364–370. doi:10.1046/j.1532-5415.2003.51110.x
9. Ryg J, Engberg H, Mariadas P, et al. Barthel Index at hospital admission is associated with mortality in geriatric patients: a Danish nationwide population-based cohort study. Clin Epidemiol. 2018;10:1789–1800. doi:10.2147/clep.S176035
10. Ocagli H, Cella N, Stivanello L, Degan M, Canova C. The Barthel index as an indicator of hospital outcomes: a retrospective cross-sectional study with healthcare data from older people. J Adv Nurs. 2021;77(4):1751–1761. doi:10.1111/jan.14708
11. Li F, Li D, Yu J, et al. Barthel index as a predictor of mortality in patients with acute coronary syndrome: better activities of daily living, better prognosis. Clin Interv Aging. 2020;15:1951–1961. doi:10.2147/cia.S270101
12. Higuchi S, Kabeya Y, Matsushita K, et al. Barthel index as a predictor of 1-year mortality in very elderly patients who underwent percutaneous coronary intervention for acute coronary syndrome: better activities of daily living, longer life. Clin Cardiol. 2016;39(2):83–89. doi:10.1002/clc.22497
13. Katano S, Yano T, Ohori K, et al. Barthel index score predicts mortality in elderly heart failure- a goal of comprehensive cardiac rehabilitation. Circulation J. 2021;86:70–78. doi:10.1253/circj.CJ-21-0584
14. Murcia J, Llorens P, Sánchez-Payá J, et al. Functional status determined by Barthel index predicts community acquired pneumonia mortality in general population. J Infect. 2010;61(6):458–464. doi:10.1016/j.jinf.2010.08.006
15. Hulsbæk S, Larsen RF, Rosthøj S, Kristensen MT. The Barthel index and the cumulated ambulation score are superior to the de Morton mobility index for the early assessment of outcome in patients with a hip fracture admitted to an acute geriatric ward. Disabil Rehabil. 2019;41(11):1351–1359. doi:10.1080/09638288.2018.1424951
16. Knauf T, Buecking B, Hack J, et al. Development of the Barthel index 5 years after hip fracture: results of a prospective study. Geriatr Gerontol Int. 2019;19(8):809–814. doi:10.1111/ggi.13723
17. Mayoral AP, Ibarz E, Gracia L, Mateo J, Herrera A. The use of Barthel index for the assessment of the functional recovery after osteoporotic Hip fracture: one year follow-up. PLoS One. 2019;14(2):e0212000. doi:10.1371/journal.pone.0212000
18. Quach LH, Jayamaha S, Whitehouse SL, Crawford R, Pulle CR, Bell JJ. Comparison of the Charlson Comorbidity Index with the ASA score for predicting 12-month mortality in acute Hip fracture. Injury. 2020;51(4):1004–1010. doi:10.1016/j.injury.2020.02.074
19. Bannay A, Chaignot C, Blotière PO, et al. The best use of the Charlson comorbidity index with electronic health care database to predict mortality. Med Care. 2016;54(2):188–194. doi:10.1097/mlr.0000000000000471
20. Minol JP, Dimitrova V, Petrov G, et al. The age-adjusted Charlson comorbidity index in minimally invasive mitral valve surgery. Eur J Cardio Thorac Surg. 2019;56(6):1124–1130. doi:10.1093/ejcts/ezz240
21. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65.
22. White DK, Wilson JC, Keysor JJ. Measures of adult general functional status: SF-36 Physical Functioning Subscale (PF-10), Health Assessment Questionnaire (HAQ), Modified Health Assessment Questionnaire (MHAQ), Katz Index of Independence in activities of daily living, Functional Independence Measure (FIM), and Osteoarthritis-Function-Computer Adaptive Test (OA-Function-CAT). Arthritis Care Res. 2011;63(Suppl 11):S297–307. doi:10.1002/acr.20638
23. Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel index for stroke rehabilitation. J Clin Epidemiol. 1989;42(8):703–709. doi:10.1016/0895-4356(89)90065-6
24. Unnanuntana A, Jarusriwanna A, Nepal S. Validity and responsiveness of Barthel index for measuring functional recovery after hemiarthroplasty for femoral neck fracture. Arch Orthop Trauma Surg. 2018;138(12):1671–1677. doi:10.1007/s00402-018-3020-z
25. Inui T, Watanabe Y, Kurata Y, et al. Early postoperative Barthel index score and long-term walking ability in patients with trochanteric fractures walking independently before injury: a retrospective cohort study. Arch Orthop Trauma Surg. 2021;141(8):1283–1290. doi:10.1007/s00402-020-03548-7
26. Bahrmann A, Benner L, Christ M, et al. The Charlson Comorbidity and Barthel Index predict length of hospital stay, mortality, cardiovascular mortality and rehospitalization in unselected older patients admitted to the emergency department. Aging Clin Exp Res. 2019;31(9):1233–1242. doi:10.1007/s40520-018-1067-x
27. Gill TM, Allore HG, Gahbauer EA, Murphy TE. Change in disability after hospitalization or restricted activity in older persons. JAMA. 2010;304(17):1919–1928. doi:10.1001/jama.2010.1568
28. Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51(4):451–458. doi:10.1046/j.1532-5415.2003.51152.x
29. Saxena SK, Ng TP, Yong D, Fong NP, Gerald K. Total direct cost, length of hospital stay, institutional discharges and their determinants from rehabilitation settings in stroke patients. Acta Neurol Scand. 2006;114(5):307–314. doi:10.1111/j.1600-0404.2006.00701.x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.