Back to Journals » Clinical Interventions in Aging » Volume 17
A High Postoperative Atropinic Burden is Associated with Postoperative Delirium in Elderly Patients with Hip Fracture: Results of the Prospective, Observational, ATROPAGE Trial
Authors Ferré F, Piel-Julian ML, Tincres F, Ba C, Menut R, Ferrier A, Bosch L, Martin C, Labaste F , Montastruc F, Sommet A, Balardy L, Minville V
Received 11 May 2022
Accepted for publication 6 November 2022
Published 30 December 2022 Volume 2022:17 Pages 1931—1938
DOI https://doi.org/10.2147/CIA.S372400
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Fabrice Ferré,1,* Marie-Léa Piel-Julian,2,* Francis Tincres,1 Cyndie Ba,1 Rémi Menut,1 Anne Ferrier,1 Laetitia Bosch,1 Charlotte Martin,1 François Labaste,1 François Montastruc,3 Agnès Sommet,3 Laurent Balardy,2,* Vincent Minville1,4,*
1Département d’Anesthésie-Réanimation et de Médecine Péri Opératoire, Centre Hospitalo-universitaire (CHU) de Toulouse, Toulouse, France; 2Service d’Oncogériatrie, Centre Hospitalo-universitaire (CHU) de Toulouse, Institut Universitaire du Cancer de Toulouse-Oncopole (IUCT-O), Toulouse, France; 3Laboratoire de Pharmacologie Médicale et Clinique, Centre Midi-Pyrénées de Pharmacovigilance, de Pharmacoépidémiologie et d’Informations sur le Médicament, Pharmacopôle Midi-Pyrénées, INSERM UMR 1027, CIC INSERM 1436, CHU Toulouse, Toulouse, France; 4RESTORE, UMR 1301 Inserm - 5070 CNRS - Université Paul Sabatier, Université de Toulouse, Toulouse, France
*These authors contributed equally to this work
Correspondence: Fabrice Ferré, Hôpital Pierre-Paul Riquet, CHU Purpan, place du Dr Baylac, Toulouse, 31059, France, Tel +33 5 61 77 99 88, Email [email protected]
Background: Postoperative delirium frequently occurs in the elderly after hip fracture surgery and is associated with poor outcomes. Our aim was to identify a correlation between the atropinic burden (AB) due to drugs with clinical antimuscarinic effect and the occurrence of postoperative delirium.
Methods: We carried out a prospective, monocentric, observational study including 67 patients over 65 years of age who underwent hip fracture surgery. The addition of the anticholinergic weight of each drug was calculated at different time points to distinguish the prehospital, intra- and postoperative part of the AB. A multivariate analysis was carried out to identify the explanatory variables associated with postoperative delirium.
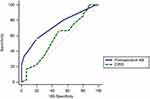
Results: Patients were 78 [71– 86] years old. The time from admission to surgery was 12 [12– 24] hours. The ADL and CIRS scores were 6 [5.5– 6] and 6 [4– 9], respectively. The total (prehospital plus intraoperative plus postoperative) AB was 5 [3– 9]. The incidence of postoperative delirium was 54% (36/67). The demographic characteristics were comparable between delirium and no delirium groups. Univariate analysis showed statistically significant differences between no delirium and delirium groups concerning the number of prehospital atropinic drugs, prehospital AB, the number of postoperative atropinic drugs, postoperative AB, in-hospital AB and the MMSE calculated on postoperative day 5. Using multivariate analysis, postoperative AB, but not pre- and in-hospital ABs, was associated with postoperative delirium with an odds ratio of 1.84 (95% CI: 1.25– 2.72; p = 0.002). A postoperative AB > 2 was associated with a postoperative delirium with an area under ROC curve of 0.73 (95% CI: 0.61– 0.83; p = 0.0001).
Conclusion: Contrary to a prior exposure to atropinic drugs, a postoperative atropinic burden > 2 was associated with postoperative delirium in elderly patients with hip fracture. Postoperative administration of (new) antimuscarinic drugs is a precipitating factor of delirium that could be avoided.
Keywords: post-operative, anesthesia, atropinic burden, hip fracture, delirium
Introduction
Postoperative Delirium
Delirium is defined by the DSM-V as a disorder of attention and consciousness that develops over a short period of time, fluctuates throughout the day and is accompanied by cognitive changes (eg, memory). These disorders are caused as a direct consequence of a medical context. Thus, the diagnosis of delirium identifies the constellation of clinical signs of an acute and polymorphic brain dysfunction with a mandatory component: a disturbance in attention.1 Interestingly, this acute multifactorial and multidimensional impairment of consciousness is an independent predictor of long-term cognitive decline and mortality. Currently, the diagnosis of delirium is based on clinical screening tools like the Confusion Assessment Method (CAM).2,3 In elderly and vulnerable patients, the frequent combination of precipitating (trauma, pain, inflammation, infection, physical restraints, acute urine retention) and predisposing factors (pre-existing cognitive impairment, co-morbidities, sensory disturbances) explains the high incidence of delirium.4 Thus, postoperative delirium is reported to occur in up to 50% of surgical elderly patients over the age of 65.5 The incidence of delirium may be as high as 61% in hip fractured patients.6
Atropinic Burden
Acetylcholine, a neurotransmitter acting on the muscarinic and nicotinic receptors of the central and peripheral nervous system, is involved in various cognitive functions (eg, attention, memory). The atropinic effect of anticholinergic drugs may be desirable for some conditions (eg, Parkinson’s disease) but can also be the result of side effects by acting on the muscarinic receptors (eg, codeine, serotonergic antidepressants, bronchodilators or H1 anti-histaminic drugs).7 The atropinic activity can then cause central (eg, irritability, confusion, hallucination, cognitive impairment) and peripheral (eg, accommodation disorders, constipation, urinary retention) adverse effects.7 It is worth noting that these drugs are frequently prescribed: 50% of patients over 65 years of age take at least one drug with atropinic effect.8 Even if each substance has its own atropinic effect, the effects add up when several of them are combined, making multi-medicated elderly patients particularly at risk. The atropinic burden (AB) is the sum of the atropinic weight of each drug to which the subject is concomitantly exposed.9 Exposure to atropinic drugs is thought to increase the risk of falls and mortality and to reduce cognitive performance in elderly subjects.8,11–13 An association between a high atropine load and the occurrence of delirium has been demonstrated in medical patients hospitalised in a geriatric setting.14 The concepts of “atropine weight” and “atropine burden” are based on two assumptions. The first hypothesis is that the power of the atropine effect varies between different drugs with properties of antimuscarinics. The second is that the combination of several drugs having atropine effects results in a summation of these effects.
Objective of the Study
The aim of this study was to demonstrate an association between AB and occurrence of postoperative delirium in hip fractured patients. We hypothesize that the frequent prescription of drugs with antimuscarinic effects in this context would favor the occurrence of postoperative delirium.
Materials and Method
Study Design
This prospective, observational, single-center study was conducted at the Toulouse University Hospital in the orthopaedic and trauma surgery department between from May 2018 to May 2019. The study was performed in compliance with the Code of Ethics of the World Medical Association (Declaration of Helsinki), approved by the Comité de Protection de la Personne (CPP Ile de France V on 7th November 2017 #2017-A01847-46). According to French Legislation, and given it was an observational study, oral informed consent was obtained from the study participants.
Inclusion and Non-Inclusion Criteria
All patients over 65 years of age who were to undergo urgent surgery of hip fracture were eligible. The patient’s pre-operative cognitive status was to allow for the collection of written consent. Patients who had delirium at baseline or cognitive impairment/dementia were not included in the study. Patients with preoperative delirium (positive CAM), a history of severe or moderate head injury (GCS < 13) in the previous 3 months, or a fracture requiring revision surgery (eg, hip fracture on arthroplasty) were not included in the study.
Atropinic Burden
The atropinic burden (AB) was the addition of the “atropine weight”/anticholinergic weight of each drug to which the subject is concomitantly exposed. The anticholinergic weight was calculated from the Durán et al9 and Laroche et al15 lists (to include drugs marketed in France not present in the list of Durán). As an example, for the post-operative period, if the patients received a single dose of morphine vs several doses, this was considered equivalent that is to say the patient was exposed to the atropinic weight of morphine.
The primary objective of the study was to assess the correlation between the overall AB during hospitalization and the incidence of delirium during the first 7 days postoperatively. The overall AB was defined as the sum of the prehospital (ie, present on admission), intraoperative and postoperative atropinic burdens.
Secondary objectives were to assess the correlation between in-hospital AB (defined as overall AB minus prehospital AB) and the occurrence of delirium. All the components of the overall AB were also analyzed (prehospital, in-hospital, intraoperative and postoperative AB). The occurrence of postoperative cognitive impairment was assessed by Mini Mental State Examination (MMSE) on postoperative day 5.16,17
Sample Size
Given the incidence of postoperative delirium in the literature (26–61% after hip fracture surgery6) and the number of explanatory variables we wished to include in the model (notably overall AB, in-hospital AB and CIRS-G), 60 patients seemed necessary to demonstrate a correlation between overall AB and the occurrence of postoperative delirium with a first-species risk α set at 0.05 and a ß risk at 0.20. In regression analysis, there should be at least 10 observations per variable.
Data Collection
Patient demographics (age, sex, weight, height, education level, ASA score, comorbidities) were collected and aggregated into a geriatric score (Cumulative Illness Rating Scale Geriatric, CIRS-G).18 The cognitive state of the patients was assessed by the MMSE.16 The MMSE was carried out preoperatively and then repeated on postoperative day 5 or at the patient’s discharge. The pre-existing state of autonomy was assessed by collecting ADL (activities of daily living) and IADL (instrumental activities of daily living) scores at inclusion.19,20 Factors predisposing to delirium (deafness, chronic alcohol abuse, uncorrected visual impairment, previous delirium, use of benzodiazepines or related drugs) were systematically investigated. The patients’ usual treatments (including self-medication) and hospital treatments were collected. The occurrence of delirium was detected by the CAM,3 performed at least 3 times daily until postoperative day 7 or until discharge. Additional CAM could be performed by nurses or physician if necessary. CAM was performed by trained assessors. Other factors favoring confusion classically described in the geriatric context (hydroelectrolytic disorders, hyperthermia, anemia, fecal impaction, acute retention of urine) were systematically sought. Medical complications were collected. Length of hospital stay, post-interventional complications, time between surgery and the first rise, and indwelling bladder catheterization were also collected.
Statistical Analysis
Qualitative data were expressed as numbers (%). Quantitative data were expressed as median [25th–75th percentile] or mean (± standard deviation) as appropriate. Categorical variables were compared using Fisher’s exact test or the Chi2 test. Quantitative variables were compared using the non-parametric Mann–Whitney U-test. Multivariate analysis (stepwise logistic regression) was performed to identify explanatory variables for the occurrence of postoperative delirium. ABs with a statistical significance in univariate analysis were included in the multivariate analysis, as well as the CIRS-G frailty score. To test the ability of ABs to predict delirium, areas under the ROC curves [area under the curve (AUC) = 0.5: no better than chance, no prediction possible; AUC = 1.0: best possible prediction] were calculated and compared using the Hanley–McNeil test. Statistical analysis was performed using MedCalc software (version 12.6.1, MedCalc Software Bvba, Ostend, Belgium; 2013). A p-value <0.05 was considered statistically significant.
Results
Sixty-seven patients meeting the eligibility criteria were included. Thirty-six patients (54%) developed postoperative delirium. Delirium occurred 2 [1–4] days after surgery. Nineteen patients were not included in the study because they had exclusion criterion (eg, pre-operative dementia or cognitive impairment…). Clinical, demographic and geriatric characteristics of the patients are available in Table 1. The characteristics of the ABs and their comparison between delirium and no delirium groups are available in Table 2. The characteristics of the patients’ perioperative course are reported in Table 3.
 |
Table 1 Clinical, Demographic and Geriatric Characteristics of Patients |
 |
Table 2 Atropinic Burden |
 |
Table 3 Perioperative Characteristics |
The two drugs’ classes with antimuscarinic effects administered were in order of frequency: i) opioid analgesics and related (morphine, oxycodone), and ii) bronchodilators (tiotropium, ipratropium). Other atropinic drugs were domperidone, metoclopramide, trimebutine, hydroxyzine, amitriptyline, prostigmine/atropine.
Among the postoperative complications, we noted a severe pulmonary embolism that occurred postoperatively and required transfer to the intensive care unit, followed by, in order of frequency, blood transfusion for anaemia, acute urine retention, faecal impaction, hyperthermia and acute functional renal failure.
When using logistic regression, postoperative AB was independently associated with postoperative delirium with an odds ratio [95% CI] of 1.86 [1.25–2.78] (p = 0.002). A postoperative AB > 2 (best-associated criterion) was associated with a postoperative delirium with an area under ROC curve of 0.73 (95% CI: 0.61–0.83; p = 0.0001) (Figure 1). Prehospital AB, in-hospital AB and CIRS-G included in the multivariate analysis were not identified as independent variables associated with postoperative delirium (p = NS).
Discussion
By prospectively analyzing 67 patients admitted for hip fracture, we were able to demonstrate for the first time a correlation between the atropinic burden induced by the postoperative prescription of drugs with antimuscarinic effects and the occurrence of postoperative delirium. This association represents a precipitating factor that could be avoided by limiting their perioperative prescription.
A projection of epidemiological data to 2050 shows that people over 60 years of age will account for 50% of all the anaesthesia performed.1 Elderly subjects are at particularly high risk of developing postoperative delirium.10,21 Its occurrence is a strong predictor of cognitive impairment and mortality.22 In this context, the identification of preventable precipitating factors is of major interest. Several authors estimate that 30 to 40% of postoperative delirium occurring in hip fractured patients would be avoidable.23,24
Our results confirm that the in-hospital atropinic burden related to the postoperative delivery of drugs with antimuscarinic effects contributes to the occurrence of delirium in a population of elderly patients with hip fracture. The high incidence of postoperative delirium observed in our study (54%) is consistent with previously published data.6 It therefore seems essential to adopt a preventive attitude from the preoperative period including rationalization of drugs with an anticholinergic effect. Actually, nearly one-third of patients were given at least 3 drugs with an atropinic effect in the postoperative period, mainly opioids or bronchodilators. Decreasing immediate postoperative pain and morphine consumption, regional analgesia could be considered as a protective factor for the occurrence of postoperative delirium in patients suffering from hip fracture.25 Besides, the French Society of Anaesthesia and Intensive Care strongly recommends regional analgesia in hip fractured patients to spare opioids and their adverse effects.24
The major limitation of our study is the difficulty in estimating the atropinic weight of drugs. Several biological methods are described in the literature like the serum anticholinergic activity which allows us to classify an anticholinergic equivalence level to atropine26 or the in-vitro measurement of the dissociation constant of the drug for muscarinic receptors. Although quantitative, these biomarkers do not predict the occurrence of central atropinic side effects. In this context, pharmacological scales, which are readily available, seem better suited to the assessment of atropinic burden in the elderly. The Durán scale, established and validated from a consensus of 7 atropinic scales, is now widely used.9 However, 3 main limitations to the use of such a scale can be cited. Firstly, the dose of the offending drug is not taken into account. Klamer et al tried to counteract this pitfall with the Muscarinic Acetylcholinergic Receptor ANTagonist Exposure (MARANTE) scale, which considers the atropinic weight of the drug (defined by Durán), as well as the daily dose prescribed.27 By weighting the atropinic weight of a treatment by its dose (0.5 for low doses, 1 for medium doses, 1.5 for high doses and 2 for very high or supra-therapeutic doses), this tool could have been of major interest but presently only 41 drugs are listed. Secondly, the lack of consideration of blood–brain barrier crossing. Indeed, for the biological methods cited above, the passage of the blood–brain barrier is not considered. For example, the high atropinic weight of ipratropium according to the Durán scale does not predict its plasmatic passage and therefore the brain effects related to its central atropinic activity. This theoretical framework could explain why the prehospital atropinic burden was not associated with postoperative delirium in our study. Indeed, we did not distinguish between prehospital treatments with antimuscarinic effects, while some are known to have central rather than peripheral effects. Similarly, we did not take into account individual variability. For example, acute renal failure, a common situation in elderly patients scheduled for hip fracture surgery, could change the pharmacokinetic properties of treatments. Thirdly and lastly, some atropinic drugs frequently used in a perioperative setting are not listed at all (eg, nefopam or sufentanil). None of the methods of calculating atropinic weight cited seem to stand out. Although designed for the elderly, none of the existing pharmacological scales is adapted to the perioperative setting and the specificities of the French pharmacopoeia. Further researches are necessary to develop a scale suitable for our clinical practice in anaesthesia and perioperative medicine. Moreover, the study does not allow to distinguish between the direct and indirect central effects of anticholinergic therapies. Indeed, the causes may be interrelated. An example could be the occurrence of delirium secondary to acute urinary retention induced by the atropinic effect of opioids.
To conclude, we were able to demonstrate a strong correlation between the postoperative atropinic burden of antimuscarinic drugs and the occurrence of delirium following hip fracture surgery. Further studies evaluating the prognostic impact of avoiding drugs with high atropinic weight are needed to definitely integrate this rule in a bundle of care to optimising the perioperative pathway of high-risk patients.
Acknowledgments
We would like to thank all the patients involved in this study and their family.
Funding
Support was provided solely from department sources. This work should be attributed to the Département d’Anesthésie-Réanimation, Centre Hospitalier Universitaire de Toulouse Purpan, Toulouse, France.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Evered L, Silbert B, Knopman DS, et al. Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. Br J Anaesth. 2018;121(5):1005–1012.
2. Laplante J, Cole MG. Detection of delirium using the confusion assessment method. J Gerontol Nurs. 2001;27(9):16–23.
3. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941–948.
4. Oh ST, Park JY. Postoperative delirium. Korean J Anesthesiol. 2019;72(1):4–12.
5. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–922.
6. Contin AM, Perez-Jara J, Alonso-Contin A, Enguix A, Ramos F. Postoperative delirium after elective orthopedic surgery. Int J Geriatr Psychiatry. 2005;20(6):595–597.
7. Montastruc F, Benevent J, Touafchia A, et al. Atropinic (anticholinergic) burden in antipsychotic-treated patients. Fundam Clin Pharmacol. 2018;32(1):114–119.
8. Fox C, Richardson K, Maidment ID, et al. Anticholinergic medication use and cognitive impairment in the older population: the medical research council cognitive function and ageing study. J Am Geriatr Soc. 2011;59(8):1477–1483.
9. Duran CE, Azermai M, Vander Stichele RH. Systematic review of anticholinergic risk scales in older adults. Eur J Clin Pharmacol. 2013;69(7):1485–1496.
10. Moulis F, Moulis G, Balardy L, et al. Exposure to atropinic drugs and frailty status. J Am Med Dir Assoc. 2015;16(3):253–257.
11. Salahudeen MS, Duffull SB, Nishtala PS. Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review. BMC Geriatr. 2015;15:31.
12. Salahudeen MS, Hilmer SN, Nishtala PS. Comparison of anticholinergic risk scales and associations with adverse health outcomes in older people. J Am Geriatr Soc. 2015;63(1):85–90.
13. Wilson NM, Hilmer SN, March LM, et al. Associations between drug burden index and falls in older people in residential aged care. J Am Geriatr Soc. 2011;59(5):875–880.
14. Flacker JM, Cummings V, Mach JR
15. Laroche ML, Charmes JP, Merle L. Potentially inappropriate medications in the elderly: a French consensus panel list. Eur J Clin Pharmacol. 2007;63(8):725–731.
16. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198.
17. Zhuang L, Yang Y, Gao J. Cognitive assessment tools for mild cognitive impairment screening. J Neurol. 2021;268(5):1615–1622.
18. Miller MD, Paradis CF, Houck PR, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the cumulative illness rating scale. Psychiatry Res. 1992;41(3):237–248.
19. Barberger-Gateau P, Commenges D, Gagnon M, Letenneur L, Sauvel C, Dartigues JF. Instrumental activities of daily living as a screening tool for cognitive impairment and dementia in elderly community dwellers. J Am Geriatr Soc. 1992;40(11):1129–1134.
20. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186.
21. Chen CC, Li HC, Liang JT, et al. Effect of a modified hospital elder life program on delirium and length of hospital stay in patients undergoing abdominal surgery: a cluster randomized clinical trial. JAMA Surg. 2017;152(9):827–834.
22. Aldecoa C, Bettelli G, Bilotta F, et al. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol. 2017;34(4):192–214.
23. Aubrun F, Marmion F. The elderly patient and postoperative pain treatment. Best Pract Res Clin Anaesthesiol. 2007;21(1):109–127.
24. Aubrun F, Baillard C, Beuscart J, et al. Recommandation sur l’anesthésie du sujet âgé: l’exemple de fracture de l’extrémité supérieure du fémur. Anesthésie Réanimation. 2019;52:122–138.
25. Mouzopoulos G, Vasiliadis G, Lasanianos N, Nikolaras G, Morakis E, Kaminaris M. Fascia iliaca block prophylaxis for Hip fracture patients at risk for delirium: a randomized placebo-controlled study. J Orthop Traumatol. 2009;10(3):127–133.
26. Carnahan RM, Lund BC, Perry PJ, Pollock BG, Culp KR. The Anticholinergic Drug Scale as a measure of drug-related anticholinergic burden: associations with serum anticholinergic activity. J Clin Pharmacol. 2006;46(12):1481–1486.
27. Klamer TT, Wauters M, Azermai M, et al. A novel scale linking potency and dosage to estimate anticholinergic exposure in older adults: the muscarinic acetylcholinergic receptor antagonist exposure scale. Basic Clin Pharmacol Toxicol. 2017;120(6):582–590.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.