Back to Journals » Infection and Drug Resistance » Volume 15
A High Level of Antimicrobial Resistance in Gram-Positive Cocci Isolates from Different Clinical Samples Among Patients Referred to Arsho Advanced Medical Laboratory, Addis Ababa, Ethiopia
Authors Gebremariam NM, Bitew A, Tsige E , Woldesenbet D, Tola MA
Received 12 May 2022
Accepted for publication 27 July 2022
Published 3 August 2022 Volume 2022:15 Pages 4203—4212
DOI https://doi.org/10.2147/IDR.S372930
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Nuhamin Melaku Gebremariam,1 Adane Bitew,2 Estifanos Tsige,3 Daniel Woldesenbet,4 Mekdes Alemu Tola5
1Ethiopian National Accreditation Office, Addis Ababa, Ethiopia; 2Department of Medical Laboratory Sciences, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 3Department of Clinical Bacteriology and Mycology National Reference Laboratory, Ethiopian Public Health Institute, Addis Ababa, Ethiopia; 4Mailman School of Public Health, Columbia University ICAP in Ethiopia, Addis Ababa, Ethiopia; 5Armauer Hansen Research Institute, Addis Ababa, Ethiopia
Correspondence: Mekdes Alemu Tola, Email [email protected]
Background: Gram-positive cocci are clinically important pathogens that cause infections and their development of antibiotic resistance continues to pose a severe threat to public health. Therefore, this study aims to investigate the level of antimicrobial resistance among Gram-positive cocci isolated from different clinical samples among patients referred to Arsho Advanced Medical Laboratory, Addis Ababa, Ethiopia.
Methods: From January to April 2018, a cross-sectional study was conducted at Arsho Advanced Medical Laboratory. Seven hundred ninety-two (792) different clinical samples were obtained from 792 individuals and inoculated into blood culture bottles and Blood Agar base. Bacterial identification was done using the number, type, and morphology of colonies, as well as Gram staining, catalase testing, and coagulase test after isolation of pure growth on culture media using the standard operating procedure. VITEK 2 compact system was used for bacterial identification and drug susceptibility testing. The information entry and analysis were performed by using SPSS version 20.
Results: Out of 792 clinical samples cultured, the prevalence of Gram-positive cocci was 12.6% (n=100/792). The most frequent one is S. aureus 54% (n=54/100) followed by coagulase-negative Staphylococcus species 42% (n=42/100), S. agalactiae 1% (n=1/100) and E. faecalis 3% (n=3/100). Penicillin showed the highest resistance rate 85% (n=85/100), followed by sulfamethoxazole/trimethoprim (47%), and oxacillin (38%); however, highest sensitivity was seen towards linezolid 97% (n=97/100) and vancomycin 94% (n=94/100). The total multi-drug resistance (MDR) Gram-positive cocci were 44% (n=44/100).
Conclusion: This study demonstrated high antimicrobial resistance and multi-drug resistance. This suggests that the importance of continuous monitoring of antimicrobial resistance patterns is crucial for selecting the suitable drug for treatment and infection prevention.
Keywords: antimicrobial resistance, Gram-positive cocci, multi-drug resistance
Introduction
Antimicrobial resistance poses a serious threat to the public’s Health and places a heavy financial and health burden on people and the healthcare system. If preventive measures are not taken to address antimicrobial resistance, it is predicted that by 2050, global costs reach $ 3 trillion yearly and an additional 10 million people may die annually; total expenditures may also exceed $ 100 trillion.1 Due to their quick potential to develop resistance to the currently prescribed medicines, gram-positive bacteria are the main cause of healthcare-associated and community-acquired infections.2 For both hospital and community-associated infections, Gram-positive bacteria, especially Gram-positive cocci (GPC) such staphylococci, streptococci, and enterococci, are among the most frequent pathogens.3–6
Staphylococcus aureus (causes wound infections) and coagulase-negative staphylococci (CoNS) (causes nosocomial bloodstream infections), and Enterococci are the most commonly isolated Gram-positive cocci from nosocomial infections. Among community-acquired infections, pneumococci is a common cause of upper (sinusitis, otitis media) and lower (pneumonia) respiratory tract infections, meningitis, bacteremia, and other suppurative infections and Streptococcus pyogenes is the most common bacteria which causes pharyngitis.3
Prolonged usage of the available effective antibiotics against GPC coupled with their decreasing susceptibility rates have led to the emergence and spread of multidrug-resistant pathogens.2 Gram-positive cocci bacteria have shown the ability to acquire and express numerous antimicrobial resistance mechanisms which lead to a multidrug-resistant (MDR) phenotype that further complicates treatment efforts in addition to the innate virulence exhibited by bacteria like S. aureus and S. pneumoniae.6
Infections caused by MDR pathogens are an increasing problem and remain one of the main challenges in the treatment of infectious diseases. Multidrug-resistant GPC such as methicillin-resistant Staphylococcus aureus (MRSA) and enterococci with vancomycin (VAN) and linezolid (LNZ) resistance or decreased susceptibility to daptomycin (DAP) and multidrug-resistant coagulase-negative staphylococci (CoNS) had been alerted. In addition, new mechanisms of resistance have been recently found in Europe such as beta-lactamase production in Enterococcus faecium.7
The ongoing increase of antimicrobial resistance among GPC infections continues to be a big threat to public health, which complicates antimicrobial therapy leading to treatment failures and imposing additional costs on health systems and patients. In addition, the emergence of antibiotic resistance in GPC has had a significant impact on patterns of prescribing and has created a clinical demand for effective novel therapeutic agents.8–13
The global increase of antimicrobial-resistant bacteria infection in both community and hospital settings is endangering the ability to effectively treat patients. Hence, recent data is needed for more appropriate antimicrobial prescribing, and careful infection control. Therefore, this study aims to investigate the prevalence and antimicrobial resistance profile of Gram‑positive cocci isolates from different clinical samples among patients referred to Arsho Advanced Medical Laboratory, Addis Ababa, Ethiopia.
Materials and Methods
Study Setting
A laboratory-based cross-sectional study was conducted from January to April 2018 at Arsho Advanced Medical Laboratory (AAML), Addis Ababa, Ethiopia. A total of 792 different clinical samples were collected from 792 patients who were referred to AAML for culture and drug sensitivity tests during the study period. Informed written consent was taken from all study participants. Study participants who were not willing to participate and who took antibiotics within the last week (7 days) were excluded from the study. The information concerning socio-demographic characteristics was obtained from the laboratory request form which was requested by physicians.
Specimen Collection and Processing
Different clinical samples (wound, blood, urine, ear swab, nasal swab, body fluid, eye swab, CSF, semen, and urogenital) were collected from study subjects following standard microbiological procedures. All samples were transported to the microbiology laboratory of AAML aseptically for culture and drug sensitivity tests. All samples were inoculated on blood culture bottles and Blood Agar base (Oxoid, Basingstoke, and Hampshire, UK) with 10% sheep blood. The blood culture bottles were incubated at 37°C in a 5% CO2 incubator for five to seven days, where similarly all plates were incubated accordingly based on their specimen type and the organism expected. Bacterial isolates were characterized by colony morphology, hemolysis, and Gram stain, catalase test, slide coagulase test, and tube coagulase test were performed according to the standard methods.14
Bacterial Identification and Antimicrobial Susceptibility Testing
VITEK 2 compact system (bioMérieux, France) was used for bacterial identification and antimicrobial susceptibility testing as per the instruction of the manufacturer. The bacterial suspension for the inoculation of ID-GP (Gram-positive identification) cards which was used for the automated identification of 115 taxa of the most significant non-spore-forming Gram-positive bacteria (primarily cocci) was prepared by transferring a sufficient number of colonies of pure culture using a sterile swab or applicator stick into 3 mL of sterile saline (aqueous 0.45% to 0.50% NaCl, pH 4.5 to 7.0) in a 12 × 75 mm clear plastic (polystyrene) test tube and the turbidity of the suspension was adjusted accordingly and measured using a turbidity meter called the DensiChek. Then, suspension for inoculation of AST GP 71 card which was used for drug susceptibility test was done by transferring 280μL of culture suspension from the first suspension into another 3mL of sterile saline solution (0.45% to 0.50% NaCl, pH 6.8–7.2) to obtain the final turbidity of 8 × 106 CFU/mL. AST-GP71 card which was used for drug susceptibility tests of Gram-positive bacteria contains; penicillin (0.125, 0.25, 1, 2, 8, 64), ciprofloxacin (1, 2, 4), clindamycin (0.5, 1, 2), daptomycin (0.5, 1, 2, 4, 16), erythromycin (0.25, 0.5, 2), gentamicin (8, 16, 64), levofloxacin (0.25, 2, 8), linezolid (0.5, 2, 8), minocycline (0.12, 0.5, 2), moxifloxacin (0.25, 2, 8), nitrofurantoin (16, 32, 64), oxacillin (0.5, 1, 2), quinupristin/dalfopristin (0.25, 0.5, 2), rifampicin (0.25, 0.5, 2), tetracycline (0.5, 1, 2), tigecycline (0.25, 0.5, 1), trimethoprim/sulfamethoxazole (2/38, 8/152, 16/304), and vancomycin (1, 2, 4, 8, 16). The concentration values are expressed in µg/mL, which were obtained from the package insert information provided in the kit of AST-GP71 card. The result interpretation was performed according to the Clinical and Laboratory Standards Institute (CLSI) guidelines.15,16
Quality Control
Standard reference strains S. aureus (ATCC 25923), S. agalactiae (ATCC 12386), and S. pyogens (ATCC 19645) were used as control reference strains for identifications and drug susceptibility testing.
Statistical Analysis
Data entry and analysis were done using Statistical Package for Social Science (SPSS) version 20 (IBM-SPSS Inc., Chicago, IL, USA).
Results
Socio-Demographic Characteristics
Out of 792 study participants, 63% (499/792) were females and 37% (293/792) were males. Concerning the age groups of the study participants, 44.4% (n=352/792) were 25–44 and 15.5% (n=123/792) were 1–14 years of age. Among the total clinical samples, growth for gram-positive cocci was observed only in 12.6% (n=100/792) samples. Females had a 51% (n=51/100) isolation rate of gram-positive cocci while male had 49% (n=49/100) as shown in Table 1. The age classification is based on the World Health Organization (WHO) age classification for health.17
 |
Table 1 Frequency of Gram-Positive Cocci Isolates with Sex and Age Group |
Prevalence of Gram-Positive Cocci from Different Clinical Samples
Among the gram-positive cocci isolates 12.6% (n=100/792), the most frequent one is S. aureus 54% (n=54/100) followed by CoNs 42% (n=42/100), E. faecalis 3% (n=3/100) and S. agalactiae 1% (n=1/100). Most of the isolates were from wound 48% (n=48/100) followed by blood 18% (n=18/100), and urine 17% (n=17/100) (Table 2).
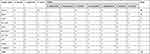 |
Table 2 Frequency of Gram-Positive Cocci Isolated from Different Clinical Specimens |
Antimicrobial Susceptibility Pattern of Gram-Positive Cocci Isolates
A total of eighteen antimicrobial drugs were used for the drug susceptibility profile of GPC isolates and the results are summarized in Table 3 and Figure 1. A high resistance rate was detected in penicillin (85%), followed by sulfamethoxazole/trimethoprim (47%), and oxacillin (38%). The highest sensitivity towards linezolid (97%), vancomycin (94%), minocycline (95%), daptomycin (95%), quinupristin/dalfopristin (95%), gentamicin (92%), and tigecycline (95%) were observed among GPC isolates.
 |
Table 3 Antimicrobial Susceptibility Pattern of Gram-Positive Cocci Isolates from Different Clinical Specimens |
S. aureus which is the most frequently isolated bacteria that showed high resistance rates for penicillin (81.5%), followed by trimethoprim/sulfamethoxazole (51.8%), tetracycline (22.2%), and oxacillin (18.5%) which is MRSA. The least resistance was seen for vancomycin, daptomycin, and rifampicin (1.9%), respectively, whereas gentamycin, quinupristin/dalfopristin, linezolid minocycline, nitrofurantoin, and tigecycline showed no resistance. The second commonly isolated GPC CoNS exhibited high resistance for penicillin (90.4%), oxacillin (64.2%), and tetracycline (47.6%). The least resistance was observed in quinupristin/dalfopristin, linezolid, minocycline, and nitrofurantoin (4.7%) each followed by vancomycin and daptomycin (7.1%), respectively.
E. faecalis showed 100% resistance to penicillin, minocycline, tetracycline, clindamycin, and quinupristin/dalfopristin and 33.3% resistance for oxacillin, gentamycin, linezolid, daptomycin, vancomycin, tigecycline, nitrofurantoin, rifampicin, and trimethoprim/sulfamethoxazole. One isolate of E. faecalis was found to be vancomycin-resistant. S. agalactiae, which is the least isolated GPC organism, was susceptible to most of the drugs but it showed 100% resistance to ciprofloxacin, levofloxacin, moxifloxacin, and nitrofurantoin.
Multidrug Resistance Patterns of Gram-Positive Cocci Isolates
A total of 44% of GPC showed multi-drug resistance. Among the isolated GPC, S. aureus showed 24.1% (n=13/54), CoNS 66.7% (n=28/42) and E. faecalis 100% (n=3/3) were MDR (Table 4). Multi-drug resistance is defined as non-susceptibility to at least one agent in three or more antimicrobial categories.18
 |
Table 4 Multidrug Resistance Pattern of Gram-Positive Cocci Isolates |
Discussion
In the present study, the gram-positive cocci isolate rate was 12.6% (n=100/792), which is lower compared to the previous studies from Ethiopia; in Addis Ababa, Gram-positive isolates constitute 45.2% (n=76/168),19 in Jimma, 47% (68/145) were Gram-positive,20 and in Bahir Dar, 52.6% (123/234) of the isolates were Gram-positive.21 The difference may be due to the difference in the study settings, study place, sample type, and sample size/number. S. aureus (54%) was the most common isolated bacteria, which is consistent with the previous reports conducted in Jimma 28.4% and Mekelle 37.5% from Ethiopia, Cameron 20.9%, India 47.7%, and Nepal 65%.22–26 The overall drug susceptibility profile of GPC, penicillin showed the highest resistance rate (85%), followed by sulfamethoxazole/trimethoprim (47%), and oxacillin (38%) which was consistent with the study in Jimma and Gondar.20,27 The most effective drugs for gram-positive cocci isolates in our study were linezolid (97%), vancomycin (96%), minocycline (95%), quinupristin/dalfopristin (95%), daptomycin (95%), which are similar to the finding of a study from Ethiopia.28
In this study, the most frequently isolated S. aureus showed high resistance rates for penicillin (81.5%), followed by trimethoprim/sulfamethoxazole (51.8%), tetracycline (22.2%), and oxacillin (18.5%) which is MRSA. The penicillin resistance rate (81.5%) of S. aureus was lower than the report from Jimma (91.5%) and Debre Markos (93.8%).20,29 Oxacillin (18.5%) resistance rate of S. aureus is comparable with the report in Bahir Dar (18.5%) and Addis Ababa (17.5%) from Ethiopia,21,30 and Nigeria (16%)31 but lower than the report of study in Gondar, Ethiopia (34.6%),27 Uganda (25%),32 and Italy (54.4%).33 In addition, S. aureus isolated in this study showed 1.9% resistance to vancomycin which is higher than the previous studies in Nigeria,31 and Namibia34 which showed no vancomycin resistance however lower than 5.1% resistance reported in Ethiopia30 and 6% resistance in a study done in Rwanda,35 whereas gentamycin, quinupristin/dalfopristin, linezolid minocycline, nitrofurantoin, and tigecycline showed no resistance.
In this study, CoNs showed high resistance to penicillin (90.4%) and oxacillin (64.2%), which is similar to the report in Iran.36 On the other hand, it showed 7.1% resistance for vancomycin, which is higher than the study done in Gondar, Ethiopia, which is 4.5%27 and 4.4% in Iran36 but lower than the finding in Addis Ababa, Ethiopia, which is 13.4%.37
A total of 44% multidrug resistance levels of gram-positive cocci isolates were observed in this study. This finding was lower compared to the report from Bahir Dar, North-west Ethiopia, where the MDR level was 54.3%,21 Dessie, North-east Ethiopia, where 65.2% of MDR was reported,38 and Jimma, South-west Ethiopia, which reported 85.2% of MDR.20 S. aureus which was the most frequently isolated GPC showed a 24.1% of MDR level in our study is lower compared to the report from Jimma University Specialized Hospital, Ethiopia, which reported 86.2%.39 However, our report is comparable to the study from Bahir Dar, North-west Ethiopia, which reported 48%.21 The second commonly isolated gram-positive cocci, CoNs, showed a 66.7% of MDR level in our study, which is consistent with the study at Tikur Anbessa Specialized Hospital, which was 66.7% from septicemia and urinary tract infections.40 On the other hand, our study result was lower than the study done on postoperative wound infections at Tikur Anbessa Specialized Hospital which was 84.2%.19 In this study, resistance was observed to the commonly prescribed drugs in the country, in Ethiopia like other developing countries prescribing drugs without knowing their antibiotic sensitivity profile due to lack of infrastructure for drug susceptibility testing, irrational or inappropriate usage of drugs, and purchasing drugs without prescription could be the possible reason for raising of antimicrobial resistance in the country.
Limitations
The lack of patient clinical information in their request paper could have been a good variable for this study due to the study being laboratory-based. In addition, there is a lack of representativeness because this study was conducted only using a single laboratory.
Conclusions
High antimicrobial and multi-drug resistance were demonstrated. Penicillin was the most resistant followed by trimethoprim/sulfamethoxazole and oxacillin, while linezolid and vancomycin were exhibited as the most susceptible drug. This suggests that the importance of continuous monitoring of antimicrobial resistance patterns is crucial for selecting the suitable drug for treatment and infection prevention.
Data Sharing Statement
The data used during the current study are included in the article.
Ethics Approval and Consent to Participate
This study was approved by the Department Research and Ethical Review Committee (DRERC) of the Department of Medical Laboratory Sciences, College of Health Science, Addis Ababa University (Ref. No: DRERC/332/18/MLS). Written informed consent was obtained from the study participants before data collection. An assent/consent form was completed and signed by a family member and/or adult guardian for participants under the age of 18 years. All methods were performed following the relevant guidelines and regulations in compliance with the declaration of Helsinki.
Acknowledgments
The authors would like to acknowledge Arsho Advanced medical Laboratory and all study participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Disclosure
All authors declare that they have no conflicts of interest.
References
1. Alhumaid S, AlMutair A, Alalawi Z, et al. Antimicrobial susceptibility of gram-positive and gram-negative bacteria: a 5-year retrospective analysis at a multi-hospital healthcare system in Saudi Arabia. Ann Clin Microbiol Antimicrob. 2021;20(1):43. doi:10.1186/s12941-021-00450-x
2. Shah S, Rampal R, Thakkar P, Poojary S, Ladi S. The prevalence and antimicrobial susceptibility pattern of gram-positive pathogens: three-year study at a private tertiary care hospital in Mumbai, India. J Lab Physicians. 2021. doi:10.1055/s-0041-1731136
3. Jeljaszewicz J, Mlynarczyk G, Mlynarczyk A. Antibiotic resistance in Gram-positive cocci. Int J Antimicrob Agents. 2000;16:473–478. doi:10.1016/S0924-8579(00)00289-2
4. Gales AC, Sader HS, Ribeiro J, Zoccoli C, Barth A, Pignatari AC. Antimicrobial susceptibility of gram-positive bacteria isolated in Brazilian hospitals participating in the SENTRY program (2005–2008). Braz J Infect Dis. 2009;13:90–98. doi:10.1590/S1413-86702009000200004
5. Eades C, Hughes S, Heard K, Moore LSP. Antimicrobial therapies for gram-positive infections. Off j R Pharm Soc. 2017;9(9):41.
6. Pfaller MA, Mendes RE, Duncan LR, Flamm RK, Sader HS. Activity of dalbavancin and comparator agents against gram-positive cocci from clinical infections in the USA and Europe 2015–2016. J Antimicrob Chemother. 2018;73(10):2748–2756. doi:10.1093/jac/dky235
7. Coronado-Alvarez NM, Parra D, Parra-Ruiz J. Clinical efficacy of fosfomycin combinations against a variety of gram-positive cocci. Enferm Infecc Microbiol Clin. 2019;37(1):4–10. doi:10.1016/j.eimc.2018.05.009
8. Woodford N, Livermore DM. Infections caused by gram-positive bacteria: a review of the global challenge. J Infect. 2009;59(S1):S4 S16. doi:10.1016/S0163-4453(09)60003-7
9. Tian Y, Li T, Zhu Y, Wang B, Zou X, Li M. Mechanisms of linezolid resistance in staphylococci and enterococci isolated from two teaching hospitals in Shanghai, China. BMC Microbiol. 2014;14:292. doi:10.1186/s12866-014-0292-5
10. Zhao C, Sun H, Wang H, et al. Antimicrobial resistance trends among 5608 clinical gram-positive isolates in China: results from the gram-positive cocci resistance surveillance program (2005–2010). Diagn Microbiol Infect Dis. 2012;73:174–181. doi:10.1016/j.diagmicrobio.2012.03.003
11. Beigverdi R, Sattari-Maraji A, Jabalameli F, Emaneini M. Prevalence of genes encoding aminoglycoside-modifying enzymes in clinical isolates of gram-positive cocci in Iran: a systematic review and meta-analysis. Microb Drug Resist. 2020;26(2):126–135. doi:10.1089/mdr.2019.0139
12. Finch R. Gram-positive infections: lessons learnt and novel solutions. Clin Microbiol Infect. 2006;12:3–8. doi:10.1111/j.1469-0691.2006.01624.x
13. Kulkarni AP, Nagvekar VC, Veeraraghavan B, et al. Current perspectives on treatment of gram-positive infections in India: what is the way forward? Interdiscip Perspect Infect Dis. 2019;2019:7601847. doi:10.1155/2019/7601847
14. Cheesbrough M. District Laboratory Practice in Tropical Countries Part 2.
15. Pincus DH. Microbial Identification Using the bioMe’rieux Vitek 2 System. Hazelwood, MO, USA: BioMérieux, Inc; 2016.
16. CLSI. Performance Standards for Antimicrobial Susceptibility Testing.
17. Series M; World Health Organization. Provisional Guidelines on Standard International Age Classifications: Statistical Papers, WHO, United Nations, New York. Vol. 74. World Health Organization; 1982:4–11.
18. Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pan drug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi:10.1111/j.1469-0691.2011.03570.x
19. Seyoum Asres G, Hailu Legese M, Woldearegay GM. Prevalence of multi-drug resistant bacteria in postoperative wound infections at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Arch Med. 2017;09:04. doi:10.21767/1989-5216.1000233
20. Mama M, Abdissa A, Sewunet T. Antimicrobial susceptibility pattern of bacterial isolates from wound infection and their sensitivity to alternative topical agents at Jimma University Specialized Hospital, South-West Ethiopia. Ann Clin Microbiol Antimicrob. 2014;13:14. doi:10.1186/1476-0711-13-14
21. Hailu D, Derbie A, Mekonnen D, et al. Drug resistance patterns of bacterial isolates from infected wounds at Bahir Dar Regional Health Research Laboratory Center, Northwest Ethiopia. Ethiop J Health Dev. 2016;30(3):112–117.
22. Kumalo A, Kassa T, S/Mariam Z, Daka D, Tadesse AH. Bacterial profile of adult sepsis and their antimicrobial susceptibility pattern at Jimma University Specialized Hospital, South West Ethiopia. Health Sci J. 2016;10(2):3.
23. Wasihun AG, Wlekidan LN, Gebremariam SA, et al. Bacteriological profile and antimicrobial susceptibility patterns of blood culture isolates among febrile patients in Mekelle Hospital, Northern Ethiopia. Springerplus. 2015;4:314. doi:10.1186/s40064-015-1056-x
24. Kamga HLF, Njunda AL, Nde PF. Prevalence of septicaemia and antibiotic sensitivity pattern of bacterial isolates at the University Teaching Hospital, Yaoundé, Cameroon. Afr J Clin Exper Microbiol. 2011;12(1):2–8.
25. Lal Das AK. A prospective study on antibiotic sensitivity pattern in septicaemic patients attending emergency medicine department of a tertiary care teaching hospital. Int J Med Res Prof. 2015;1(3):92–95.
26. Karki S, Rai GK, Manandhar R. Bacteriological analysis and antibiotic sensitivity pattern of blood culture isolates in Kanti Children Hospital. J Nepal Paediatr Soc. 2010;30(2):94–97. doi:10.3126/jnps.v30i2.2482
27. Amare B, Abdurrahman Z, Moges B, Ali J. Postoperative surgical site bacterial infections and drug susceptibility patterns at Gondar University Teaching Hospital, Northwest Ethiopia. J Bacteriol Parasitol. 2011;02(8). doi:10.4172/2155-9597.1000126
28. Bitew A, Admassie M, Getachew T. Spectrum and Drug susceptibility profile of bacteria recovered from patients with wound infection referred to arsho advanced medical laboratory. Clin Med Res. 2018;7(1):8. doi:10.11648/j.cmr.20180701.12
29. Mulu W, Abera B, Yimer M, Hailu T, Ayele H, Abate D. Bacterial agents and antibiotic resistance profiles of infections from different sites that occurred among patients at Debre Markos Referral Hospital, Ethiopia: a cross-sectional study. BMC Res Notes. 2017;10(1):254. doi:10.1186/s13104-017-2584-y
30. Dilnessa T, Bitew A. Prevalence and antimicrobial susceptibility pattern of methicillin-resistant Staphylococcus aureus isolated from clinical samples at Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia. BMC Infect Dis. 2016;16:398. doi:10.1186/s12879-016-1742-5
31. Shittu AO, Okon K, Adesida S, et al. Antibiotic resistance and molecular epidemiology of Staphylococcus aureus in Nigeria. BMC Microbiol. 2011;11:92. doi:10.1186/1471-2180-11-92
32. Anguzu JR, Olila D. Drug sensitivity patterns of bacterial isolates from septic post-operative wounds in a regional referral hospital in Uganda. Afr Health Sci. 2007;7(3):148–154.
33. Giacometti A, Cirioni O, D’errico MM, et al. Epidemiology and microbiology of surgical wound infections. J Clin Microbiol. 2000;38(2):918–922. doi:10.1128/JCM.38.2.918-922.2000
34. Iileka AEK, Mukesi M, Engelbrecht F, Moyo SR. Antimicrobial susceptibility patterns of staphylococcus aureus strains isolated at the Namibia institute of pathology from 2012 to 2014. Open J Med Microbiol. 2016;6:116–124. doi:10.4236/ojmm.2016.63016
35. Ntirenganya C, Muvunyi CM, Manzi O, Ogbuagu O. High prevalence of antimicrobial resistance among common bacterial isolates in a tertiary healthcare facility in Rwanda. Am J Trop Med Hyg. 2015;92(4):865–870. doi:10.4269/ajtmh.14-0607
36. Ghadiri H, Vaez H, Khosravi S, Soleymani E. The antibiotic resistance profiles of bacterial strains isolated from patients with hospital-acquired bloodstream and urinary tract infections. Crit Care Res Pract. 2012;2012:890797. doi:10.1155/2012/890797
37. Ten-hove RJ, Tesfaye M, Ten Hove WF, Nigussie M. Profiling of antibiotic resistance of bacterial species recovered from routine clinical isolates in Ethiopia. Ann Clin Microbiol Antimicrob. 2017;16(1):46. doi:10.1186/s12941-017-0221-1
38. Azene MK, Beyene BA. Bacteriology and antibiogram of pathogens from wound infections at Dessie Laboratory, North-East Ethiopia. Tanzan J Health Res. 2011;13(4). doi:10.4314/thrb.v13i4.64901
39. Godebo G, Kibru G, Tassew H. Multidrug-resistant bacterial isolates in infected wounds at Jimma University Specialized Hospital, Ethiopia. Ann Clin Microbiol Antimicrob. 2013;12:17. doi:10.1186/1476-0711-12-17
40. Hailu M, Mulugeta G, Asrat D. Prevalence-and-antimicrobial-resistance-pattern-of-bacterial-isolates-among-children suspected for septicemia and urinary tract infections at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Int j Sci Eng Res. 2016;7(10):1431–1444.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

