Back to Journals » Patient Preference and Adherence » Volume 17
A Health State Utility Study to Elicit Societal Values Associated with Pulmonary Hypertension
Authors Nafees B, de Freitas HM , Beaudet A , Todd E, Gin-Sing W
Received 3 December 2022
Accepted for publication 22 July 2023
Published 25 August 2023 Volume 2023:17 Pages 2119—2130
DOI https://doi.org/10.2147/PPA.S400061
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Beenish Nafees,1 Hayley M de Freitas,1 Amélie Beaudet,2 Eunju Todd,3 Wendy Gin-Sing4
1Patient-Reported Outcomes, Nafees Consulting Limited, London, UK; 2Global Market Access and Pricing, Actelion Pharmaceuticals Ltd, Allschwil, Switzerland; 3Janssen Global Commercial Strategy Organization, High Wycombe, UK; 4Pulmonary Hypertension Service, Hammersmith Hospital, London, UK
Correspondence: Beenish Nafees, Patient-Reported Outcomes, Nafees Consulting Limited, 62 Marlborough Mansions, Cannon Hill, London, NW6 1JS, UK, Tel +447957634170, Email [email protected]
Aim: Pulmonary hypertension (PH) is a rare, severe, and progressive pulmonary vascular disease, which includes five subgroups with similar presentation. Symptoms include dyspnea, and fatigue, and can significantly impact one’s health-related quality of life (HRQL). Although treatments are mainly medical, PH group 4, chronic thromboembolic pulmonary hypertension (CTEPH), can be managed with procedures, ie pulmonary endarterectomy (PEA) and balloon pulmonary angioplasty (BPA). Currently, drugs in Europe are only approved for pulmonary arterial hypertension (PAH), and CTEPH therefore the aim of this study was to elicit novel societal health state utilities in the UK for PAH and CTEPH based on disease severity, functional class (FC), clinical events, and treatment procedures specifically for CTEPH.
Material and Methods: Six health states were defined: World Health Organization (WHO)-FC II, WHO-FC III, and WHO-FC IV [defined by the New York Heart Association (NYHA)]; PH-related hospitalization; and “BPA procedure and recovery” and “PEA surgery and recovery”. Health states were based on a targeted literature review and two rounds of interviews with clinical experts (N = 4) and patients (N = 6). Draft health states were validated in cognitive debriefing interviews with clinical experts (N = 3). Health states were valued by the UK general public (n = 200), using a visual analogue scale (VAS) and time trade-off (TTO) assessment with the lead time method.
Results: The mean TTO values/utilities were 0.81 (FC II), 0.80 (BPA), 0.78 (PEA), 0.59 (FC III), 0.28 (FC IV), and 0.25 (PH-related hospitalization). Each progression in FC was associated with worse TTO scores.
Conclusion: This study reports societal utility values for PAH and CTEPH in the UK. It provides first utility estimates for states such as BPA procedure and recovery, PEA surgery and recovery and PH-related hospitalization for this population. The results show important distinctions between FC, treatment procedures, and hospitalization, and the significant burden of disease on HRQL.
Keywords: time trade-off, vignette, health-related quality of life, CTEPH, hospitalization, PAH
Introduction
Pulmonary hypertension (PH) is a rare, severe, and progressive pulmonary vascular disease characterized by elevated resting mean pulmonary arterial pressure of ≥25 mmHg, as measured by right heart catheterization.1 Symptoms of PH relate to progressive right ventricular dysfunction and typically include dyspnea, fatigue, weakness, chest pain, and syncope.1,2 Initial symptoms are induced by exertion, while symptoms at rest occur at more advanced disease stages.1 As symptoms are non-specific, there is often a delay between symptom onset and diagnosis.3 PH comprises five subgroups, categorized according to similar clinical presentation and pathology;1 pulmonary arterial hypertension (PAH) (Group 1), PH due to left heart disease (Group 2), PH due to lung disease (Group 3), chronic thromboembolic pulmonary hypertension (CTEPH) (Group 4), and PH due to unclear or multifactorial mechanisms (Group 5). The prevalence of PAH is estimated between 47.6 and 54.7 per million, and between 25.8 and 38.4 per million for CTEPH.4 The focus of this study was specifically on PAH and CTEPH because current treatments for PH are only approved in Europe for these two subgroups.5
The goal of treatment in PAH is to achieve a low-risk status, which relates to good quality of life, exercise capacity, right ventricular function, and a low risk of mortality.1 Risk status is calculated using different variables such as FC defined by The New York Heart Association (NYHA) and World Health Organization (WHO), Natriuretic peptide tests measure levels of BNP (NT-pro-BNP), the six-minute walk distance (6MWD) and hemodynamic variables.1 WHO-FC (from now on will be reported as FC) is used to classify severity of symptoms of PH; FC I representing patients with no limitation of physical activity through to FC IV in which patients have symptoms at rest and severe symptoms with an activity.1 Current PAH treatment guidelines recommend a combination of clinical and functional variables to evaluate a patient’s risk of clinical worsening and death.5 Initial treatment should include supportive measures (such as, exercise, rehabilitation, and psychosocial support).6 Patients diagnosed at low or intermediate one-year mortality risk should be initiated with combination endothelin receptor antagonist (ERA) and phosphodiesterase inhibitor (PDE5i) therapies, and those at high risk are recommended combination therapy including continuous intravenous treatment with prostacyclin.6
For patients with CTEPH with surgically accessible disease, pulmonary endarterectomy (PEA) is the gold standard treatment of choice, allowing patients to have a near normal quality of life,1,7 with most patients experiencing considerable symptom relief and significantly improving long-term survival.1,8,9 Patients’ eligibility for PEA is assessed by a specialist multi-disciplinary CTEPH team, including an experienced surgeon.1,7 During PEA, scar tissue and organized thrombus are removed through a median sternotomy incision giving direct access to both main pulmonary arteries. Patients are attached to a heart-lung bypass machine and the body temperature is gradually cooled to 20◦C to enable hypothermia and safe arrest of the circulation.7,10 Post-PEA complications include lung oedema (reperfusion injury) and neurological complications such as stroke. Experienced centers report mortality rates to be <5%10 and freedom from disease-specific death at 10 years post-PEA can be >80%.11 One study aimed to define residual PH post PEA and describe poor long-term outcomes post procedure. Patients who underwent surgery were followed up to five years after PEA. In one center, only six out of 356 experienced recurrent pulmonary emboli.12 It is estimated that 50% of patients are not eligible for PEA, either due to the peripheral location of thrombi or an unfavorable benefit–risk ratio.
Balloon pulmonary angioplasty (BPA) is an emerging therapeutic option for CTEPH, which can be indicated for patients who are not eligible for surgery or have recurrent symptoms following PEA.13 The aim of BPA is to open obstructed vessels or widen stenotic lesions using a catheter-based technique rather than invasive surgery. Small balloons are inflated in the pulmonary arteries to push the blockages aside and reduce the narrowing.14 Long sheaths are used to guide the catheters, which access the right or left main pulmonary artery through the jugular or femoral vein. Patients are given anticoagulants and supplemental oxygen throughout. BPA can be combined with medical therapy and, on average, requires four to five separate procedures to be carried out.15 The risks associated with BPA include pulmonary oedema, vessel injury, and haemorrhage. Between 2019 and 2020, 31 BPA procedures were undertaken in the UK, with its use expected to increase during the next years.14
In addition to the physical burden, PH has a considerable impact on patients’ psychological and emotional wellbeing and health-related quality of life (HRQL).16–18 A survey of 563 patients found that most patients considered PH to have an impact on their overall HRQL, with 90% reporting mental and emotional impact and 80% reporting an impact on their family life.19 Other questionnaire studies also reported impaired HRQL in PH patients, with increased pain and discomfort,20 impact on emotional reactions, sleep disturbances, social isolation and low energy levels.21,22
Currently, there are scarce published utility data describing the impact of PH and its treatment on HRQL. Utility data are required to assess the impact of new treatments and interventions on quality of life and are a key component of economic evaluations. Utilities range from 0 to 1, where 0 equals death and 1 equals full health. While some health technology assessment (HTAs) agencies, such as National Institute of Clinical Excellence (NICE), prefer the use of generic preference-based measures (GPBMs), such as the EuroQol 5 Dimension 5 Level (EQ-5D-5L), to estimate utilities, they acknowledge that this may not be appropriate or possible in all cases due to accessibility of the patient population or specific characteristics of clinical events.23 Alternatively, a vignette-based utility method may be used, whereby a “health state” for a specific condition, clinical event, or procedure, and its impact on HRQL is described and subsequently valued in a preference elicitation task using the time-trade off (TTO) method with the general public. In this manuscript, “utilities” and “TTO values” will be used synonymously to describe the obtained data.
The aim of this study was to elicit societal health state utilities in PH, in the UK, specifically for FC, clinical events for patients, and treatment procedures unique to CTEPH.
Materials and Methods
Study Design
Health State Development
The study was divided into two parts; 1) Development of health state vignettes, through a targeted literature review and qualitative interviews with patients and healthcare professionals (HCPs); and 2) The valuation of the health state vignettes using the TTO exercise, as recommended by NICE.23 Figure 1 shows a flow diagram of the different steps undertaken in parts one and two of the study.
 |
Figure 1 Flow diagram of methodological steps taken in part 1 and 2 of the study. Abbreviations: HRQL, health-related quality of life; HCP, healthcare professional; TTO, time trade-off. |
The study protocol was submitted for review by an Institutional Review Board in the United States (US), WCG-IRB Connexus, and approved by a US ethical board on 14th October 2020 (WCG-IRB 1294140). This study also complies with the Declaration of Helsinki.
Part 1: Health State Vignette Development
Literature Review
A targeted literature review was conducted in September 2019 to identify articles describing the symptoms and HRQL burden of PH, with a focus on PAH and CTEPH. The concepts of interest were symptoms of PAH and CTEPH, risk categories, definitions of FC, clinical markers such as 6MWD, and impact on HRQL. Searches were conducted in PubMed using search terms such as Pulmonary Hypertension, Pulmonary Arterial Hypertension, Chronic thromboembolic pulmonary hypertension, Adult [MeSH Terms], “Health-related quality of life”. The sponsor also provided key articles1,24–29 including two utility study reports conducted in PAH and CTEPH30,31 In total, 9 full articles1,3,6,7,24–27,29 and two utility study reports30,31 were reviewed. The findings were used to inform the content of the health state vignettes.
Health State Definitions
Six health state vignettes were developed for valuation based on information from the literature review and qualitative interviews with HCPs and patients. Health states were defined by WHO/NYHA FC (Figure 2), which directly relates to how PH patients feel and function and is routinely used by physicians to determine treatment decisions.1 A health state describing FC I was not included in the vignettes as patients are usually asymptomatic and rarely diagnosed at this stage. FC II is related to patients experiencing “no symptoms at rest, but normal activities such as climbing the stairs, grocery shopping or making the bed can cause some discomfort and shortness of breath”. FC III is related to patients feeling that “resting may be symptom-free, but normal chores around the house are greatly limited due to shortness of breath or feeling tired”. FC IV is related to patients experiencing “symptoms at rest and severe symptoms with an activity”.
 |
Figure 2 Description of health states developed to describe patients’ experiences of PH. |
A health state describing hospitalization was included as this is a marker of disease progression and represents a severe state that requires additional treatment and impacts patients’ HRQL. This was defined as Hospital admission >1 day for a PH related event. Health states describing the period of recovery after PEA and BPA procedures were also developed as these are treatment options for CTEPH which have an impact on HRQL and there is limited utility evidence available for these treatments. These health states described patients’ recovery period from three months following procedure and six months following surgery. BPA procedure and recovery reflected the time from having the procedure and up to three months recovery following the procedure. PEA surgery and recovery state reflected the time from receiving the surgery up to six months after the procedure.
Qualitative Interviews with Healthcare Professionals
HCPs were identified through the sponsor’s network of clinicians and included a total of four specialists in PH; two were respiratory nurses and two were respiratory consultants. The HCPs were selected if they currently specialized in PH; and were based in UK, Ireland or Switzerland. All clinical experts fulfilled the criteria and had between 12 and 20 years’ experience of treating patients with PAH and CTEPH. All experts provided written informed consent prior to taking part in the interviews.
Two rounds of interviews were conducted. The first was conducted between November to December 2019 and aimed to identify concepts relevant for the health state descriptions. A semi-structured interview guide was used to explore symptoms of PAH and CTEPH at each FC, the impact on HRQL, and experiences during and after hospitalization, PEA surgery, and BPA. Interviews were conducted by trained interviewers over the telephone and lasted approximately 60 minutes. The HCPs were reimbursed for their time in line with fair market value rates for their professional roles and experience.
The second round of review interviews was conducted from January to March 2021 with three HCPs who took part in the first round. These interviews aimed to review the content of the draft health states to, which were then revised and finalised for inclusion in the valuation exercise (Appendix 1).
Healthcare Professional Interview Findings
The HCPs reported considerable variability in disease symptoms between patients. The HCPs all reported that one of the main symptoms of PAH and CTEPH is breathlessness, but only on moderate exertion, with fatigue being a significant problem. The HCPs agreed that patients experience a significant detrimental emotional impact due to the prospect of a very reduced life expectancy. All HCPs reported that symptoms worsen at each FC level and FC IV has the greatest impact on HRQL whereby patients are breathless at rest or while during minimal activity, and experience severe fatigue. The experts said that following successful PEA surgery and BPA procedures, patients can experience a significant improvement in their symptoms and can often go back to their daily activities and their normal lives.
Qualitative Interviews with Patients
Patients were recruited through a specialist recruitment agency and were required to have a confirmed diagnosis of PAH or CTEPH, be at least 18 years old, and resident in the UK. Due to the rarity of the disease, recruitment aimed to include at least one patient who represented each functional class 2–4, and who had undergone one of the two treatment procedures, PEA or BPA. The aim was to recruit at least six participants with PH, in line with previous studies.32,33 Interviews were conducted by two trained interviewers between November and December 2020. All interviews were conducted by video call or telephone and did not last longer than 60 minutes. A semi-structured interview guide was used to understand patients’ experience of living with PH, and the impact of their condition and treatment on HRQL. All patients provided written informed consent prior to taking part in the interviews.
At screening, patients’ FC was identified by the interviewers using the WHO FC classification. The patients then completed a sociodemographic and clinical information form and were asked to describe the symptoms and impact related to the FC they were currently in, as well as any treatments, procedures or hospitalization events they had experienced since receiving their diagnosis. The qualitative data from the interviews enabled the study team to develop health states that accurately reflect patients’ lived experience of the disease, in line with NICE’s recommendations.23
Patient Interview Findings
A total of six patients took part in the interviews in the UK; their mean age was 37 (age range between 22 years and 55 years), two patients had a diagnosis of PAH and four had a diagnosis of CTEPH. Two patients were classed as FC II and FC III and one patient each was classed as FC I and FC IV at the time of the interview. One patient had undergone PEA and two patients had undergone BPA. Full sociodemographic and clinical characteristics are reported in Appendix 2.
The patients described experiencing symptoms such as breathlessness, fatigue, palpitations, and light-headedness, with symptoms getting worse as FC progressed. The patients expressed frustration as symptoms impacted everything they did, including their ability to climb stairs, carry shopping, and get dressed. Patients reported a significant emotional impact of being diagnosed with a life-long condition at a young age. Two patients reported multiple hospitalizations with the length of stay varying between one night and three weeks. One patient reported that hospitalization had a physical and an emotional impact on their daily life. The patients who had undergone PEA reported an improved change in breathing and limited ability to perform daily activities immediately after the procedure, although this became better for most patients once fully recovered. The patient who had undergone BPA reported feeling an instant and significant improvement in breathing following the first procedure, with improvements following the subsequent procedures being less noticeable.
Part 2: Health State Evaluation
Members of the UK general public were recruited to be closely representative of the UK population as possible in terms of age and gender, according to the last census data.34 Participants were required to be aged 18 or over, resident in the UK and provide informed consent to participate. Interviews were conducted online, via video call, by trained interviewers between March – May 2021. Participants evaluated all six health states on a visual analog scale (VAS, 0–100) and using the TTO method and completed the EQ-5D-5L.
A formal sample analysis was not conducted, but in line with previous studies, TTO studies usually aim to achieve a sample of 100–200 participants.32,33,35,36 The current study aimed to include 200 participants to ensure we had a robust sample.
In the TTO task participants imagined that they were currently experiencing each health state (described in the vignette) and were asked to choose whether they preferred:1 to live in the health state for a period of 10 years followed by death;2 to live for X number of years in full health; or3 to indicate that the two previous options were equally desirable. Time in the state of full health (X) was systematically reduced from 10 years downwards until the respondent was indifferent between the two choices. Participants evaluated all states using the standard TTO method.37 However, the lead time method was used for a health state when participants believed that the state was worse than 0 years in full health. Therefore, the utilities elicited could range from −1 to +1.37
Statistical Analysis
Descriptive statistics were used to present socio-demographic data, with means and standard deviations (SD) for continuous data and percentages for categorical data in SAS. The EQ-5D-5L was analysed using developer guidelines. The utilities such as TTO and VAS scores were analysed and calculated as means and SD with 95% confidence intervals (CI). All analyses were performed using Excel or SAS.
Results
A total of 200 participants were recruited to evaluate the health state vignettes. Demographic characteristics (Table 1) and mean EQ-5D-5L scores (Table 2) for the sample were compared to UK population data.34 Overall, the sample largely reflected the UK general population according to the 2011 census. The current sample had a mean VAS score of 87.0, on the EQ-5D-5L which suggested overall they were in good health.
 |
Table 1 Socio-Demographic Profile of the TTO Participants |
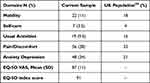 |
Table 2 Participant Self-Reported EQ-5D-5L Score (N = 200) Compared to Normative UK Data |
Table 3 shows the mean calculated utilities for each of the health states, determined using the TTO method, while the equivalent data collected using the VAS method is summarized in Table 4. The mean TTO values ranged from 0.81 (FC II) and 0.25 (PH-related hospitalization). All the states were rated as better than dead. The largest incremental drop in utility value was between FC III and FC IV. The health utility values followed the same order using the VAS method, showing consistent results between the two methods.
 |
Table 3 Mean TTO Scores for All Health States (Best to Worst) |
 |
Table 4 Mean VAS Scores for All Health States (Best to Worst) |
Discussion
The current study aimed to estimate societal utility values associated with PH in the UK general public. The health states described the progressive deterioration of patients with each FC, as well as PH-related events and procedures with a focus on PAH and CTEPH. To our knowledge, this was the first known study to elicit utility values for health states such as PEA and BPA procedures and associated recovery. These values may be applied to other sub-groups of PH (PH due to left heart disease, PH due to lung disease, and PH due to unclear or multifactorial mechanisms) in economic modelling and highlight the benefit of treatment to alleviate the HRQL burden associated with PH.
The mean utility values associated with FC II, BPA procedure and recovery, and PEA surgery and recovery, were higher compared to FC III, FC IV and PH-related hospitalization. The higher values of BPA and PEA could be partly due to the health states describing both the procedure and the recovery period, which included descriptions of the improvements in the patients’ ability to perform daily activities and physical activity. Compared to recent literature, the values for post-BPA and post-PEA are quite similar.39 Boon et al39 reported a model which estimated the economic impact of early diagnosis of CTEPH. They reported EQ-5D values of 0.743 for post PEA and 0.705 for post BPA, which were converted from previously collected 36-Item Short Form Survey (SF-36) in other studies.26,40 In the previous studies, patients were evaluated one year after PEA surgery and after up to three BPA sessions, using the SF-36.
The symptoms of PH severely affect patients’ ability to perform daily activities such as housework and food shopping, and mobility.41 The current study supports these findings where FC IV was rated lower than FC II and FC III, and the largest incremental decrease in utility was observed between FC III and FC IV. In addition, the high mean utility associated with FC II was supported by HCPs who reported that patients have significant or marked decline in physical functioning and HRQL from FCIII onwards, independently from the physicians who assessed the FCIII status. The utility decreased as the burden of symptoms and HRQL worsened as shown by previous literature.42,43 Beaudet et al42 found that as FC progressed, utility values decreased in three trials.44–46 Similarly, Keogh et al43 found that as FC worsened, there was a decrease in utility values measured by the SF-36.
A negative impact of disease progression on the utility values has been observed in other chronic and life-long conditions. Kirsch et al47 reported the following utility values for each FC in heart disease; 0.93 (FCI), 0.765 (FCII), 0.509 (FC III) and 0.284 (FC IV). These values are very similar to the current values in PH, which could be expected as symptoms are similar. Taichman et al48 evaluated the HRQL of patients with PAH and found severe and significant impairments in both physical and psychological dimensions of SF-36 (p < 0.001), which affected patient’s ability to do daily activities and their relationships with family and friends.
PH-related hospitalization was valued as the worst state in this study with a TTO score of 0.245. In the absence of established utility values for hospitalization in PH specifically, current hospitalization values may be compared to other conditions. Swinburn et al49 captured proxy HRQL data for hospitalization in acute heart failure (AHF), using proxy EQ-5D assessments made by informal caregivers and HCPs. In their study, the utility estimates varied by the duration of hospitalization and ranged from 0.199 (Day 1) to 0.817 (Day 7) based on data from HCPs. Hong et al50 conducted a TTO study in heart failure in Korea and also reported low utility values for hospitalization, with a utility of 0.360.
Utility data derived from GPBMs (eg EQ-5D) may not be appropriate when it is difficult to access patients with the condition (eg patients with rare diseases), or to estimate utilities for temporary events (eg hospitalization or adverse events) and for treatment-specific attributes (eg mode of administration). The current study adopted the TTO approach because PAH and CTEPH are rare diseases and patients are difficult to recruit for qualitative studies. In addition, it would not be appropriate to obtain data directly from patients who are experiencing the severe health states included in this study. This study provides novel utility data for patients in FC IV and those who experience a PH-related hospitalization. Utility data for these health states are scarce since patients in FC IV are not often recruited in clinical trials due to the severity of their disease. Moreover, in randomized controlled trials with PAH and CTEPH patients, patient-reported outcome instruments have not previously been administered during hospitalization. The study also elicits utilities for BPA and PEA states for which there were no previous published data. For these procedures, the TTO approach was considered appropriate as recommended by Matza et al51 because these health states included descriptions of the overall recovery process following the intervention.
There are some limitations of this study to be considered. While extensive work was conducted to accurately portray the experience of patients with PH in the health states, interviews were conducted with a small sample of patients within each FC. A small number of patients were considered sufficient to obtain feedback because PAH and CTEPH are rare diseases. In addition, efforts were made to understand the patient experience by reviewing previous literature and conducting detailed interviews to minimise this limitation. Moreover, HCPs were interviewed in order to provide a broad understanding of the disease from experience of treating different patients; however, they may not fully understand the lived experience of patients and their families. Patients also did not review the final health states because it was considered unethical and inappropriate to ask patients to validate health states describing negative outcomes and events that they may have not experienced. To ensure robustness, health states were developed using a targeted literature review, concept elicitation interviews with patients and HCPs, and content validation interviews with HCPs. Overall, this study followed a similar approach to previous utility studies and recommendations for good practice51,52 in terms of health state development, qualitative data, and sample size.
Conclusion
This study reports societal utility values in PH in the UK. The results reflect the significant impact of PH symptoms on HRQL, and also provide new utility values in PH such as hospitalization, especially in CTEPH for PEA surgery and recovery and BPA procedures and recovery. These values may be applied to other sub-groups of PH in economic modelling and highlight the benefit of treatment to alleviate the HRQL burden associated with PH.
Abbreviations
6MWD, 6-Minute Walk Distance; AHF, Acute Heart Failure; BPA, Balloon Pulmonary Angioplasty; CTEPH, Chronic Thromboembolic Pulmonary Hypertension; CI, Confidence Interval; ERA, Endothelin Receptor Antagonist; EQ-5D-5L, EuroQol 5 Dimensions 5 Levels; FC, Functional Class; GPBM, Generic Preference-Based Measure; HTA, Health Technology Assessment; HCP, Healthcare Professional; HRQL, Health-Related Quality of Life; NICE, National Institute of Clinical Excellence; NYHA, New York Heart Association; ONS, Office for National Statistics; PDE5i, Phosphodiesterase Inhibitor; PAH, Pulmonary Arterial Hypertension; PEA, Pulmonary Endarterectomy; PH, Pulmonary Hypertension; SF-36, 36-Item Short Form Survey; SD, Standard Deviation; TTO, Time Trade-Off.
Acknowledgments
The authors would like to thank the patients who took part in the interviews and gave important insights into their experiences of PAH and CTEPH; and the clinicians and nurses who provided valuable expertise to support the development of the health states; Simone Stickel (SS), Professor David Kiely (DK), and Professor Sean Gaine (SG). SS, and DK took part in both rounds of expert review and SG took part in the first round of open-ended interviews.
Funding
The study was sponsored by Actelion Pharmaceuticals Ltd, a Janssen Pharmaceutical Company of Johnson & Johnson.
Disclosure
BN and HMdF were paid by Actelion Pharmaceuticals Ltd to conduct the research. AB is an employee of Actelion Pharmaceuticals Ltd, a Janssen Pharmaceutical Company of Johnson & Johnson. ET is an employee of Janssen Global Commercial Strategy Organization, High Wycombe, UK. WGS has received honoraria for speaking and consultation from Actelion Pharmaceuticals Ltd, a Janssen Pharmaceutical Company of Johnson and Johnson, Acceleron, Bayer, Gossamer Bio, and MSD. The authors report no other conflicts of interest in this work.
References
1. Galie N, Humbert M, Vachiery L, et al; 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. The joint task force for the diagnosis and treatment of pulmonary hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS). Eur Heart J. 2015. doi:10.1093/eurheartj/ehv317
2. Rose-Jones LJ, McLaughlin VV. Pulmonary hypertension: types and treatments. Curr Cardiol Rev. 2015;11(1):73–79. doi:10.2174/1573403X09666131117164122
3. Hoeper MM, Ghofrani HA, Grunig E, Klose H, Olschewski H, Rosenkranz S. Pulmonary hypertension. Dtsch Arztebl Int. 2017;114:73–84. doi:10.3238/arztebl.2017.0073
4. Leber L, Beaudet A, Muller A. Epidemiology of pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension: identification of the most accurate estimates from a systematic literature review. Pulm Circ. 2021;11(1):1–12. doi:10.1177/2045894020977300
5. Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43:3618–3731. doi:10.1093/eurheartj/ehac237
6. Galiè N, Channick RN, Frantz RP, et al. Risk stratification and medical therapy of pulmonary arterial hypertension. Eur Respir J. 2018. doi:10.1183/13993003.01889
7. Kim NH, Delcroix M, Jenkins DP, et al. Chronic thromboembolic pulmonary hypertension. J Am Coll Cardiol. 2013;62(25):D92–D99. doi:10.1016/j.jacc.2013.10.024
8. Mayer E, Jenkins D, Lindner J, et al. Surgical management and outcome of patients with chronic thromboembolic pulmonary hypertension: results from an international prospective registry. J Thorac Cardiovasc Surg. 2011;141(3):702–710. doi:10.1016/j.jtcvs.2010.11.024
9. Madani MM, Auger WR, Pretorius V, et al. Pulmonary endarterectomy: recent changes in a single institution’s experience of more than 2700 patients. Ann Thorac Surg. 2012;94(1):97–103. doi:10.1016/j.athoracsur.2012.04.004
10. NHS Royal Papworth Hospital. Pulmonary endarterectomy service. NHS Royal Papworth Hospital; 2021. Available from: https://royalpapworth.nhs.uk/our-services/surgery/pulmonary-endarterectomy-service.
11. Ishida K, Masuda M, Tanabe N, et al. Long-term outcome after pulmonary endarterectomy for chronic thromboembolic pulmonary hypertension. J Thorac Cardiovasc Surg. 2012;144(2):321–326. doi:10.1016/j.jtcvs.2011.09.004
12. Cannon JE, Su L, Kiely DG, et al. Dynamic risk stratification of patient long-term outcome after pulmonary endarterectomy: results from the United Kingdom National Cohort. Circulation. 2016;133(18):1761–1771. doi:10.1161/CIRCULATIONAHA.115.019470
13. Lang I, Meyer B, Ogo T, et al. Balloon pulmonary angioplasty in chronic thromboembolic pulmonary hypertension. Eur Respir Rev. 2017;26(143):160119. doi:10.1183/16000617.0119-2016
14. Digital, National Health Service (NHS). National audit of pulmonary hypertension. Eleventh annual report. United Kingdom: S.N.; 2021.
15. Fukui S, Ogo T, Morita Y, et al. Right ventricular reverse remodelling after balloon pulmonary angioplasty. Eur Respir J. 2014;43(5):1394–1402. doi:10.1183/09031936.00012914
16. Delcroix M, Howard L. Pulmonary arterial hypertension: the burden of disease and impact on quality of life. Eur Respir Rev. 2015;24(138):621–629. doi:10.1183/16000617.0063-2015
17. McCollister DH, Beutz M, McLaughlin V, et al. Depressive symptoms in pulmonary arterial hypertension: prevalence and association with functional status. Psychosomatics. 2010;51(4):339. doi:10.1176/appi.psy.51.4.339
18. Matura LA, McDonough A, Carroll DL. Health related quality of life and psychological states in patients with pulmonary arterial hypertension. J Cardiovasc Nurs. 2014;29(2):178–184. doi:10.1097/jcn.0b013e318275330d
19. Armstrong I, Billings C, Kiely DG, et al. The patient experience of pulmonary hypertension: a large cross-sectional study of UK patients. BMC Pulm Med. 2019;19:67. doi:10.1186/s12890-019-0827-5
20. Ivarsson B, Hesselstrand R, Radegran G, Kjellstrom B. Health-related quality of life, treatment adherence and psychosocial support in patients with pulmonary arterial hypertension or chronic thromboembolic pulmonary hypertension. Chron Respir Dis. 2018;16:1–8. doi:10.1177/1479972318787906
21. Reis A, Santos M, Vicente M, et al. Health-related quality of life in pulmonary hypertension and its clinical correlates: a Cross-Sectional Study. Biomed Res Int. 2018;3924517:10. doi:10.1155/2018/3924517
22. Kamenskaya O, Klinkova A, Chernyavskiy A, Lomivorotov VV, Edemskiy A, Shmyrev V. Long-term health-related quality of life after surgery in patients with chronic thromboembolic pulmonary hypertension. Qual Life Res. 2020;29(8):2111–2118. doi:10.1007/s11136-020-02471-z
23. National Institute of Health and Care Excellence. Guide to the Methods of Technolgy Appraisal. National Institute of Health and Care Excellence; 2013.
24. Davies E, Llewellyn S, Beaudet A, et al. Elicitation of health state utilities associated with the mode of administration of drugs acting on the prostacyclin pathway in pulmonary arterial hypertension. Patient Prefer Adherence. 2018;12:1079–1088. doi:10.2147/PPA.S160662
25. Hoeper M, Kramer T, Pan Z, et al. Mortality in pulmonary arterial hypertension: prediction by the 2015 European pulmonary hypertension guidelines risk stratification model. Eur Respir J. 2017;50(2):1700740. doi:10.1183/13993003.00740-2017
26. Darocha S, Pietura R, Pietrasik A, et al. Improvement in quality of life and hemodynamics in chronic thromboembolic pulmonary hypertension treated with balloon pulmonary angioplasty. Circ J. 2017;81(4):552–557. doi:10.1253/circj.CJ-16-1075
27. Benza RL, Lohmueller LC, Kraisangka J, Kanwar M. Risk assessment in pulmonary arterial hypertension patients: the long and short of it. Adv Pulm Hypertens. 2018;16(3):125–135. doi:10.21693/1933-088X-16.3.125
28. Benza RL, Miller DP, Gomberg-Maitland M, et al. Predicting survival in pulmonary arterial hypertension. Insights From the Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL). Circulation. 2010;122(2):164–172. doi:10.1161/CIRCULATIONAHA.109.898122
29. Boucly A, Weatherald J, Savale L, et al. Risk assessment, prognosis and guideline implementation in pulmonary arterial hypertension. Eur Respir J. 2017;50(2):1700889. doi:10.1183/13993003.00889-2017
30. Beaudet AF. Utility Values to be Used in the Selexipag Cost-Effectiveness Model: A Pragmatic Literature Review. Actelion; 2017.
31. Llewellyn S, Kosmas CE, Ballinger R, Doll H. Elicitation of Disutility Values Associated with the Mode of Administration of Drugs Acting on the Prostacyclin Pathway in Pulmonary Arterial Hypertension (PAH). Oxford, UK: ICON Plc.; 2018.
32. Lloyd A, Nafees B, Narewska J, et al. Health state utilities for metastatic breast cancer. Br J Cancer. 2006;95(6):683–690. doi:10.1038/sj.bjc.6603326
33. Worbes-Cerezo M, Nafees B, Lloyd A, Gallop K, Ladha I, Kerr C. Disutility study for adult patients with moderate to severe Crohn’s Disease. J Health Econ Outcomes Res. 2019;6(2):47–60. doi:10.36469/9685
34. Statistics, Office for National. UK Data Service. Census aggregate data; 2011.
35. Doyle S, Lloyd A, Walker M. Health state utility scores in advanced non-small cell lung cancer. Lung Cancer. 2008;62(3):374–380. doi:10.1016/j.lungcan.2008.03.019
36. Swinburn P, Lloyd A, Nathan P, Choueiri TK, Cella D, Neary MP. Elicitation of health state utilities in metastatic renal cell carcinoma. Curr Med Res Opin. 2010;26(5):1091–1096. doi:10.1185/03007991003712258
37. Janssen BMF, Oppe M, Versteegh MM, et al. Introducing the composite time trade-off: a test of feasibility and face validity. Eur J Health Econ. 2013;14(Suppl S1):S5–S13. doi:10.1007/s10198-013-0503-2
38. Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ. 1998;316(7133):736–741. doi:10.1136/bmj.316.7133.736
39. Boon G, van den Hout WB, Barco S, et al. A model for estimating the health economic impact of earlier diagnosis of chronic thromboembolic pulmonary hypertension. ERJ Open Res. 2021;7(3):00719–2020. doi:10.1183/23120541.00719-2020
40. Kamenskaya O, Klinkova A, Loginova I, et al. Determinants of health-related quality of life 1 year after pulmonary thromboendarterectomy. Ann Vasc Surg. 2018;51:254–261. doi:10.1016/j.avsg.2018.02.019
41. European Pulmonary Hypertension Association. The Impact of Pulmonary Arterial Hypertension (PAH) on the Lives of Patients and Carers: Results from an International Survey. European Pulmonary Hypertension Association; 2012.
42. Beaudet A, Davies EW, Di Scala L, et al. Association between health-related quality of life and pulmonary arterial hypertension (PAH) disease severity: a review of GRIPHON, SERAPHIN, COMPASS-2 and EARLY trials;
43. Keogh AM, McNeil K, Wlodarczyk J, et al. Quality of life in pulmonary arterial hypertension: improvement and maintenance with bosentan. J Heart Lung Transplant. 2007;26(2):181–187. doi:10.1016/j.healun.2006.11.009
44. Sitbon O, Channick R, Chin KM, et al. Selexipag for the treatment of pulmonary arterial hypertension. N Engl J Med. 2015;373(26):2522–2533. doi:10.1056/NEJMoa1503184
45. Pulido T, Adzerikho I, Channick R, et al. Macitentan and morbidity and mortality in pulmonary arterial hypertension. N Engl J Med. 2013;369(9):809–818. doi:10.1056/NEJMoa1213917
46. McLaughlin V, Channick RN, Ghofrani HA, et al. Bosentan added to sildenafil therapy in patients with pulmonary arterial hypertension. Eur Respir J. 2015;46:405–413.
47. Kirsch J, McGuire A. Establishing health state valuations for disease specific states: an example from heart disease. Health Econ. 2000;9(2):149–158. doi:10.1002/(SICI)1099-1050(200003)9:2<149::AID-HEC501>3.0.CO;2-N
48. Taichmann DB, Shin J, Hud L, et al. Health-related quality of life in patients with pulmonary arterial hypertension. Respir Res. 2005;6(1):92. doi:10.1186/1465-9921-6-92
49. Swinburn P, Shingler S, Ong SH, et al. Assessing the health-related quality of life in patients hospitalised for acute heart failure. Br J Cardiol. 2013;20:72–76.
50. Hong SH, Lee JY, Park SK, et al. The utility of 5 hypothetical health states in heart failure using Time Trade-Off (TTO) and EQ-5D-5L in Korea. Clin Drug Investig. 2018;38:727–736. doi:10.1007/s40261-018-0659-8
51. Matza LS, Stewart KD, Lloyd AJ, et al. Vignette-based utilities: usefulness, limitations, and methodological recommendations. Value Health. 2021;24(6):812–821. doi:10.1016/j.jval.2020.12.017
52. Hall F, de Freitas HM, Kerr C, et al. Estimating utilities/disutilities for high-risk metastatic hormone-sensitive prostate cancer (mHSPC) and treatment-related adverse events. Qual Life Res. 2019;28(5):1191–1199. doi:10.1007/s11136-019-02117-9
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
