Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
A Dermocosmetic Significantly Reduces the Frequency and Intensity of Facial Skin Intolerability and Sensitivity in Subjects with Skin Intolerant to Skin Care Products and Sensitive Skin
Authors Kerob D, Czermanska A, Karamon EM, Moga A, Lecerf G, Nioré M, Le Dantec G , Le Floc'h C , Tan J
Received 24 April 2023
Accepted for publication 4 July 2023
Published 11 July 2023 Volume 2023:16 Pages 1787—1794
DOI https://doi.org/10.2147/CCID.S418483
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Anne-Claire Fougerousse
Delphine Kerob,1 Anna Czermanska,2 Ewa M Karamon,3 Alain Moga,4 Guillaume Lecerf,4 Margot Nioré,1 Guénaëlle Le Dantec,1 Caroline Le Floc’h,1 Jerry Tan5
1Scientific Direction, La Roche-Posay Laboratoire Dermatologique, Levallois-Perret, France; 2Dermascan, Poland Sp. z o. o., Gdansk, Poland; 3Studio Dermatologia i Kosmetyka ul, Malbork, Poland; 4QIMA Bioalternatives - Prologue Biotech, Labège, France; 5Western University, Department of Medicine and Windsor Clinical Research Inc, Windsor, ON, Canada
Correspondence: Delphine Kerob, Scientific Direction, La Roche-Posay Laboratoire Dermatologique, International Scientific Affairs, Levallois-Perret, France, Email [email protected]
Introduction: Intolerance to dermocosmetics is frequent in subjects with allergic contact dermatitis (ACD). A dermocosmetic (DC) was developed to restore the natural skin barrier, to reduce skin inflammation and to improve sensitive skin in ACD.
Objective: To assess the benefit of a DC in subjects with an allergic background and intolerance to cosmetic care, or with sensitive skin.
Materials and Methods: In this open-label study, 107 subjects above 16 years of age applied DC on the face twice a day for 28 days. Assessments at Days 0, 14 and 28, included skin sensitivity, stinging test, local tolerance, transepidermal water loss (TEWL), skin hydration, inflammatory biomarkers (IL-1α, IL-1RA, PGE2) using tape stripping and subject satisfaction.
Results: 88% were women and mean age was 42.0± 15.0 years. Skin sensitivity at inclusion scored 5.9± 0.35; 46% had ACD, 95% skin irritation, 92% sensitive skin and 88% intolerance to cosmetics. A significant (p< 0.0001) 85% decrease of frequency and intensity of the composite score was observed at both endpoints. Stinging scores significantly (p< 0.0001) decreased from 3.9 at baseline to 2.4 at Day 14 and 1.4 at Day 28; 77% and 81% of subjects reported improved skin reactivity at Day 14 and Day 28, respectively. Similar improvements were noted in the frequency and intensity of irritation, erythema, stinging, burning and discomfort. TEWL, skin hydration and inflammatory biomarker levels significantly (p< 0.0001) improved. Overall subject satisfaction (85%) and tolerance (investigators: 99%, subjects: 97%) were high.
Conclusion: DC significantly reduced the frequency and intensity of facial skin intolerability and sensitivity in subjects with skin intolerant to skin care products.
Clinicaltrials.gov Identifier: NCT05487937.
Keywords: dermocosmetic, allergic prone skin, sensitive skin
Corrigendum for this paper has been published.
Introduction
Dermocosmetics are skincare solutions that use sophisticated active ingredients to directly support or care for the symptoms of various skin conditions, cosmetics are substances that clean, improve or change the complexion, skin, hair, nails or teeth. They include beauty preparations (make-up, perfume, skin cream, nail polish) and grooming aids (soap, shampoo, shaving cream, deodorant).1,2
Intolerance to cosmetics and dermocosmetics and sensitive skin is frequently observed in subjects with allergic contact dermatitis (ACD).3–5
All allergic conditions share a dysfunctional epithelial barrier. This altered barrier allows allergens and microbes to penetrate the skin, resulting in release of type 2 cytokines which drive the allergic inflammation. During epidermal differentiation, keratinocytes sequentially switch gene expression programs. As a result, terminal differentiation, and formation of a mature stratum corneum are observed. This process is to prevent allergen or microbial invasion of the skin. Any abnormalities in keratinocyte differentiation in skin prone to allergies triggers hyperproliferation of the basal layer of the epidermis, inhibition of terminal differentiation markers, and barrier lipid abnormalities alter the natural skin barrier, leading to inflammation and antimicrobial dysfunction.6,7
Sensitive skin is a subjective, perceived cutaneous hyper-reactivity to environmental factors.8,9 Subjects report exaggerated reactions when their skin is in contact with cosmetics, soaps and sunscreens. Moreover, they may report frequent itching, burning, stinging or a tight sensation, even if no clinical signs are present. The origins of sensitive skin are still not completely understood and may be caused by different mechanisms.10 Subjects with sensitive skin may have a thinner stratum corneum with a reduced corneocyte area, resulting in higher transcutaneous penetration of water-soluble chemicals.
The dermocosmetic tested herewith (DC, Toleriane® Dermallergo Cream, La Roche-Posay Laboratoire Dermatologique, France) has been specifically developed to restore the natural skin barrier and reduce skin inflammation to relieve signs and symptoms related to skin intolerance and sensitive skin. Key ingredients are Niacinamide, fractions of the probiotic Sphingomonas Ferment Extract, and Acetyl Dipeptide-1 Cetyl Ester, a soothing compound (Neurosensine®) that acts on skin sensitivity by decreasing erythema, irritation and pruritus, which have all been described in patients with ACD.11 Other compounds are water, isocetyl stearate, squalane, butyrospermum, shea butter, dimethicone, glycerin, corn starch, pentylene glycol, butylene glycol, glyceryl stearate, PEG-100 stearate, cetyl alcohol, salvia miltiorrhiza root extract, dimethiconol, sodium hydroxide, caprylyl glycol, citric acid and C10-30 alkyl acrylate cross polymer.
This exploratory study assessed the benefit of a DC in subjects with an allergic background and intolerance to facial cosmetic skin care products.
Materials and Methods
Methodology
This open-label study was conducted at one investigational site in Gdansk, Poland. According to local regulatory guidelines, this type of trial testing marketed cosmetics does not require approval from the local ethics committee of Gdansk, Poland. However, the local ethics committee was informed about this study and subjects and their care givers, if aged less than 18 years provided written informed consent prior to participation. The study followed the principles of the Declaration of Helsinki. The study is registered under the identifier number NCT05487937 in the Clinical trial PRS data base.
Subjects
Caucasian subjects above 16 years of age with a clinically confirmed allergic background and intolerance to cosmetics for at least 2 years prior to inclusion were suitable for participation and applied the DC on the entire face twice daily for 28 days. Upon their selection, subjects were asked not changed their cosmetic routine (hygiene and make-up) during the 15 days preceeding inclusion. During the study, subjects were not allowed to apply any other similar product on their face and not to modify their other usual skin hygiene and make-up products. Suitable subjects were asked to apply the DC on the face twice daily for 28 days.
Clinical and Instrumental Assessments
Dermatological assessments at Days 0, 14 and 28 included the composite skin sensitivity score (ranging from 0 to 12, and was the sum of pruritus, redness, burning sensation and tingling scores, each on a scale from 0=none to 4=severe) and symptoms (pruritus, redness, burning sensation and tingling) and stinging test using the global cutaneous reactivity score (from from 0=no stinging=3) using the lactic acid skin stinging test.12 A global score (Sensiscore®) assessed the subject-reported facial skin intolerance and reactivity on a scale from 0=never to 44=all the time, local tolerance, transepidermal water loss (TEWL) using a Tewameter® (Courage + Khazaka electronic GmbH, Cologne, Germany), and skin hydration was measured by corneometry using a Corneometer® (Courage + Khazaka electronic GmbH, Cologne, Germany).13
At the end of the study, subjects rated the soothing effect and their satisfaction with the DC.
Biomarker Quantification
Samples of the stratum corneum surface were taken to assess interleukin 1α, (IL-1α) and the interleukin-1-receptor antagonist IL-1RA levels, both playing a role in inflammation and innate immunity, as well as prostaglandin E2 (PGE2), which favours the regeneration of various organ systems following injury.14–17 Sampling was performed using the non-invasive skin tape stripping method at Day 0 and Day 14.18,19
Skin samples were analysed using an Enzyme immunoassay (EIA, R&D systems Inc., Minneapolis, MN, USA) and enzyme-linked immunosorbent assay (ELISA, R&D systems Inc., Minneapolis, MN, USA) and one replicate at QIMA Bioalternatives- Prologue Biotech, Labège, France.
Tubes containing the samples were thawed at ambient temperature. Samples were extracted from each tape with 500 µL of PBS using a thermomixer for 20 min of agitation at 40°C, followed by 10 min under ultrasonic agitation and then centrifuged for 3 min at 18,000 g at 4°C. The liquid obtained served for the assays.
The total protein assay was performed using the BCA method. This method is based on the colorimetric reaction of proteins which reduce the Cu2+ ion into Cu+ ion. The Cu+ ion is then complexed by the BCA reagent, which produces a blue-violet colour. The optical density was measured at 562 nm.
Assays were performed using ELISA kits. The IL-1α and IL1RA assays were performed in “sandwich” mode. The principle is to prepare a plate with a monoclonal antibody respectively specific for IL-1α and IL1RA. Then, the sample containing IL-1α and IL1RA respectively was added in order to bind to the antibody and to add a polyclonal antibody recognizing the antigen to be sandwiched. A secondary antibody bound to the enzyme was added to convert it into a detectable entity (450 nm), directly proportional to the amount of IL-1α or IL1RA.
The PGE2 assay, confirming the COX-2 activity, was carried out in a “competitive” mode. A plate was prepared to which anti-mouse IgG antibodies (by default) were attached. A mixture of labelled antigens (alkaline phosphatase conjugated-PGE2) and antigens to be assayed (sample) were added on the plate, to allow for a competition between the antigens during incubation. The prostaglandin E2 antibody and the substrate (pNpp) were added to the enzymatic reaction and converted to a detectable entity (450 nm) which was inversely proportional to the amount of PGE2.
Statistical analysis was performed using SAS® 9.4 software (SAS Institute, Cary, NC, USA). Quantitative variables were described by means, standard deviations, medians and interquartile ranges. Qualitative variables were described by the raw numbers of the different modalities and the corresponding percentages. The significance threshold was 5%; a significance level of p <0.05 was considered as statistically significant.
Results
Overall, 107 subjects participated in this study, 88% were women; mean age was 42.0±15.0 years. In total, 53% of the subjects had dry skin, 60% had allergic rhinitis, 46% ACD, and 15% allergic conjunctivitis. 95% reported skin prone to irritation, 92% facial sensitive skin and 74% reactive skin (with redness and/or burning, stinging, itching sensation); 88% of the subjects reported reactivity to several cosmetics. The mean skin sensitivity composite score was 5.9±0.35, and the mean global cutaneous reactivity score was 3.9±0.3 at baseline; the mean baseline Sensiscore was 15.3±0.6.
Stinging test scores significantly (p<0.0001) decreased from 3.9±0.3 at baseline to 2.4±0.4 at Day 14 (−39%) and 1.4±0.3 (−64%) at Day 28. Overall, 77% and 81% of subjects reported improved skin reactivity at Day 14 and Day 28, respectively.
The composite skin sensitivity score decreased from 5.9±0.35 to 0.05±0.1 after 28 days of daily use (p<0.0001; Figure 1).
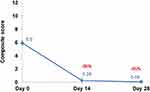 |
Figure 1 Composite skin sensitivity score at Day 0, Day 14 and Day 28. The composite skin sensitivity score significantly (p<0.0001) had decreased at Day 14 and Day 28 compared to Day 0. |
Significant (p<0.0001) improvements were observed for the intensity of symptoms: pruritus had improved by 98% after 14 and by 99% after 28 days, redness by 95% at Day 14 and by 100% after 28 days, burning sensation by 94% and 98% at Day 14 and Day 28 respectively, and tingling by 95% and 98% after 14 and 28 days of daily use (Figure 2).
 |
Figure 2 Subject-reported symptom scores at Day 0, Day 14 and Day 28. Subject-reported symptoms significantly (p<0.0001) improved as early as Day 14. |
In parallel, the frequency of the global differences compared to baseline were statistically significant (p<0.0001). The evolution of the intensity of the global Sensiscore was similar (p<0.0001), with a 92.0% decrease at Day 14 (1.3±0.3) and Day 28 (0.4±0.2), compared to baseline (16.7±0.2 at baseline).
Instrumental measures showed significant (p<0.0001) improvements of the TEWL (Figure 3) and skin hydration (Figure 4) at Day 14 and Day 28. The percentage of subjects with a reinforced cutaneous skin barrier confirmed by a decrease of TEWL was 82% after 14 and 99% after 28 days; 77% of subjects at Day 14 and 97% at Day 28 observed improved skin hydration.
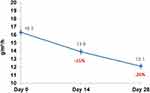 |
Figure 3 Evolution of transepidermal water loss over time. Transepidermal water loss was significantly (p<0.0001) reduced over time. |
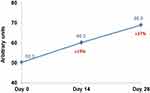 |
Figure 4 Evolution of skin hydration over time. Skin hydration had significantly (p<0.0001) improved as early as Day 14. |
The biomarker analysis showed that all three tested inflammatory biomarkers significantly (p<0.0001) decreased after 14 days of daily application of the DC.
Detailed results are given in Figure 5.
Overall, 93% of subjects reported that their skin felt soothed after 28 days of daily use. User satisfaction was high (85%). Tolerance was rated good to very good by 99% of the investigators and by 97% of subjects. Overall, 18 transient and mild AEs were considered related to the DC: 5 burning sensation, 5 erythema, 4 stinging, 3 itching and 1 tightness.
Discussion
Results from the present study demonstrate that a specifically developed DC significantly (p<0.0001) reduces clinical signs and symptoms of ACD on the face and improves sensitive skin after only 14 days of daily use. Particularly skin stinging, frequently reported in sensitive skin, had significantly (p<0.0001) improved after 14 days and continued to improve after 28 days, suggesting that further improvement is obtained with daily use of the DC.20
A similar evolution was observed for TEWL and skin hydration, which both favourably evolved indirectly, confirming that the DC significantly (p<0.0001) supports the restoration of the natural skin barrier.
Moreover, results from the inflammatory biomarker analyses confirmed that the DC was able to significantly (p<0.0001) reduce Il-1α, IL-1RA and PGE2 biomarkers, which aligned with the clinical improvement.
Allergies on the face and sensitive skin have been reported by subjects more and more frequently over the last few years.21 This may be because it is suspected that environmental factors, including unsuitable skin care products and airborne pollution, frequently impact the natural skin barrier.22–24 Providing specifically developed skin care for subjects with an intolerance to their usual facial skin care products, or who suffer from sensitive skin, may help to reduce clinical signs and relieve their symptoms without requiring pharmacological therapy. This is of importance, as the prolonged use of topical corticosteroids, for example, which may not always be indicated but are frequently used to manage ACD, may cause local side effects, requiring their withdrawal. Conversely, asking to avoid using any skin care may not be considered acceptable by subjects with ACD signs and symptoms.25,26 In parallel, the tested DC was very well tolerated, with no local side effects reported in addition to its significant benefit in improving signs and symptoms of skin intolerant to skin care products or sensitive skin, which may add to its benefit and is, therefore, another argument for using a specific DC in this type of subject profile.
One limitation is that the subjects were not asked to report the daily use of the tested DC. This would have allowed to assess compliance to the product regimen. Moreover, the results presented herewith would have been more powerful if the tested DC had been compared to its vehicle. Although a classic moisturizer would certainly have improved ACD signs and symptoms for a short period, it would not have obtained similar results over the test period. Niacinamide was shown to restore the cellular NAD+ pool and mitochondrial energetics, to reduce oxidative stress and the inflammatory response, to improve the extracellular matrix as well as the skin barrier, and to inhibit the pigmentation process in the skin. Moreover, when applied topically, alone or in combination with other active ingredients, it is able to reduce the progression of skin ageing and hyperpigmentation.11 The probiotic fraction of Sphingobioma which induces the syntheses of IL-10, providing a further anti-inflammatory effect.27,28
In conclusion, the tested DC reduces the frequency and intensity of skin intolerability and sensitivity in subjects with skin intolerant to skin care products. Further research may be necessary to confirm obtained results.
Data Sharing Statement
Delphine Kerob, the corresponding author, will share the study protocol and all data collected and statistically analysed in relationship with this study upon reasonable request for one year after publication of this manuscript, except identified participant data.
Ethical Statement
According to local regulations, this study did not require ethics committee approval from the independent ethics committee of Gdansk, Poland. However, subjects and their care givers, if aged less than 18 years provided written informed consent prior to participation and consented to the use of their photographs for publication purposes. The study followed the principles of the Declaration of Helsinki.
Acknowledgments
The authors acknowledge the staff members of Eurofins Gdansk, Poland, for having run the study and Karl Patrick Göritz, SMWS, France, for the writing support.
Funding
This study was financed by La Roche-Posay Laboratoire Dermatologique.
Disclosure
DK, GLD, MN and CLF are employees of La Roche-Posay Laboratoire Dermatologique. JT receives honoraria from La Roche-Posay Laboratoire Dermatologique. The authors report no other conflicts of interest in this work.
References
1. Gagliardi L, Dorato S. 1.1 - general concepts. Current legislation on cosmetics in different countries. In: Salvador A, Chisvert A, editors. Analysis of Cosmetic Products. Amsterdam: Elsevier; 2007:3–28.
2. Dreno B, Araviiskaia E, Berardesca E, et al. The science of dermocosmetics and its role in dermatology. J Eur Acad Dermatol Venereol. 2014;28(11):1409–1417. doi:10.1111/jdv.12497
3. Zirwas MJ. Contact dermatitis to cosmetics. Clin Rev Allergy Immunol. 2019;56(1):119–128. doi:10.1007/s12016-018-8717-9
4. Park ME, Zippin JH. Allergic contact dermatitis to cosmetics. Dermatol Clin. 2014;32(1):1–11. doi:10.1016/j.det.2013.09.006
5. Biebl KA, Warshaw EM. Allergic contact dermatitis to cosmetics. Dermatol Clin. 2006;24(2):215–32, vii. doi:10.1016/j.det.2006.01.006
6. Egawa G, Kabashima K. Barrier dysfunction in the skin allergy. Allergol Int. 2018;67(1):3–11. doi:10.1016/j.alit.2017.10.002
7. Goleva E, Berdyshev E, Leung DY. Epithelial barrier repair and prevention of allergy. J Clin Invest. 2019;129(4):1463–1474. doi:10.1172/JCI124608
8. Berardesca E, Farage M, Maibach H. Sensitive skin: an overview. Int J Cosmet Sci. 2013;35(1):2–8. doi:10.1111/j.1468-2494.2012.00754.x
9. Primavera G, Berardesca E. Sensitive skin: mechanisms and diagnosis. Int J Cosmet Sci. 2005;27(1):1–10. doi:10.1111/j.1467-2494.2004.00243.x
10. Misery L, Weisshaar E, Brenaut E, et al. Pathophysiology and management of sensitive skin: position paper from the special interest group on sensitive skin of the International Forum for the Study of Itch (IFSI). J Eur Acad Dermatol Venereol. 2020;34(2):222–229. doi:10.1111/jdv.16000
11. Boo YC. Mechanistic basis and clinical evidence for the applications of nicotinamide (niacinamide) to control skin aging and pigmentation. Antioxidants. 2021;10(8):1315. doi:10.3390/antiox10081315
12. Richters RJ, Hendriks JC, Uzunbajakava NE, et al. Responses to sodium dodecyl sulphate as an in vivo human model to study the pathomechanisms underlying sensitive skin. Exp Dermatol. 2016;25(5):407–409. doi:10.1111/exd.12973
13. Seite S, Rougier A, Benech F, Bayer Vanmoen M, Veyrat S. Clinical Usefulness of a Product Developed for Sensitive and Allergy Prone Skin. MOSBY-ELSEVIER; 2012;AB72–AB.
14. Cheng H, Huang H, Guo Z, Chang Y, Li Z. Role of prostaglandin E2 in tissue repair and regeneration. Theranostics. 2021;11(18):8836–8854. doi:10.7150/thno.63396
15. Dinarello CA. Overview of the IL-1 family in innate inflammation and acquired immunity. Immunol Rev. 2018;281(1):8–27. doi:10.1111/imr.12621
16. Dinarello CA, van der Meer JW. Treating inflammation by blocking interleukin-1 in humans. Semin Immunol. 2013;25(6):469–484. doi:10.1016/j.smim.2013.10.008
17. Macleod T, Berekmeri A, Bridgewood C, Stacey M, McGonagle D, Wittmann M. The immunological impact of IL-1 family cytokines on the epidermal barrier. Front Immunol. 2021;12:808012. doi:10.3389/fimmu.2021.808012
18. Bize C, Le Gélébart E, Moga A, Payré B, Garcia C. Barrier disruption, dehydration and inflammation: investigation of the vicious circle underlying dry skin. Int J Cosmet Sci. 2021;43(6):729–737. doi:10.1111/ics.12748
19. Barber C, Boiko S. Tape stripping: investigational, diagnostic, and therapeutic uses in dermatology. Clin Dermatol. 2022;40(4):355–362. doi:10.1016/j.clindermatol.2022.02.008
20. Inamadar AC, Palit A. Sensitive skin: an overview. Indian J Dermatol Venereol Leprol. 2013;79(1):9–16. doi:10.4103/0378-6323.104664
21. Geier J, Lessmann H, Schnuch A, Uter W. Recent increase in allergic reactions to methylchloroisothiazolinone/methylisothiazolinone: is methylisothiazolinone the culprit? Contact Dermatitis. 2012;67(6):334–341. doi:10.1111/j.1600-0536.2012.02157.x
22. Cecchi L, D’Amato G, Annesi-Maesano I. External exposome and allergic respiratory and skin diseases. J Allergy Clin Immunol. 2018;141(3):846–857. doi:10.1016/j.jaci.2018.01.016
23. Passeron T, Krutmann J, Andersen ML, Katta R, Zouboulis CC. Clinical and biological impact of the exposome on the skin. J Eur Acad Dermatol Venereol. 2020;34(Suppl 4):4–25. doi:10.1111/jdv.16614
24. Passeron T, Zouboulis CC, Tan J, et al. Adult skin acute stress responses to short-term environmental and internal aggression from exposome factors. J Eur Acad Dermatol Venereol. 2021;35(10):1963–1975. doi:10.1111/jdv.17432
25. Hajar T, Leshem YA, Hanifin JM, et al. A systematic review of topical corticosteroid withdrawal (“steroid addiction”) in patients with atopic dermatitis and other dermatoses. J Am Acad Dermatol. 2015;72(3):541–9.e2. doi:10.1016/j.jaad.2014.11.024
26. Ehmann L, Reinholz M, Maier T, Lang M, Wollenberg A. Efficacy and safety results of a drug-free cosmetic fluid for perioral dermatitis: the toleriane fluide efficacy in perioral dermatitis (TOLPOD) study. Ann Dermatol. 2014;26(4):462–468. doi:10.5021/ad.2014.26.4.462
27. Chen AC, Damian DL. Nicotinamide and the skin. Australas J Dermatol. 2014;55(3):169–175. doi:10.1111/ajd.12163
28. Madaan P, Sikka P, Malik DS. Cosmeceutical aptitudes of niacinamide: a review. Recent Adv Anti Infect Drug Discov. 2021;16(3):196–208. doi:10.2174/2772434416666211129105629
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

